Abstract
Purpose
The study aimed to examine the relationship between cardiovascular disease (CVD) and physical activity (PA) levels in cancer survivors (CS).
Methods
Using a nested, retrospective follow-up design, this study presents the self-reported prevalence of CVD in an Atlantic Canadian population-based cohort of 1526 CS and 6034 age-sex matched, non-cancer controls ranging from 35 to 69 years of age. Univariate and multiple logistic regression models were used to explore the association between CVD and PA.
Results
Overall, CS were 30% more likely to have ever experienced a CVD event than controls (OR = 1.3; 95% CI 1–1.7, p = .07). Survivors were also significantly more likely to report having hypertension (OR = 1.60; 95% CI 1.03–1.3, p = .02) and diabetes (OR = 1.27; 95% CI 1.03–1.16, p = .02). Compared to controls, CS were significantly less likely to engage in high levels of PA. For survivors, compared to those who were least physically active, the odds of having a CVD risk factor was 35% lower for those who were moderately active (OR = 0.65; 95% CI 0.48–0.88) and 45% lower in the most highly active group (OR = 0.55; 95% CI 0.4–0.73). For controls, the odds of having a CVD risk factor was 25% lower for those in the moderately active group (OR = 0.75; 95% CI 0.64–0.88) and 30% lower for those in the high active group (OR = 0.70; 95% CI 0.6–0.81).
Conclusion
Low active survivors appear to be at a high risk of CVD-related comorbidity.
Implications for cancer survivors
PA is associated with lower CVD-related comorbidity in CS, suggesting that interventions directed at increasing PA should be implemented to improve long-term health outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While the war against cancer wages on, since the passing of the National Cancer Act in 1971, the number of cancer survivors has grown from three million to approximately 14.5 million in the USA alone. As our population continues to age, the number of new cancer diagnoses will likewise rise dramatically over the next several decades. However, with continued advances in early detection and treatment, improved survival rates are resulting in a rapidly growing population of cancer survivors. With an average projected annual growth of 450,000 survivors, over the course of the next 10 years as many as 19 million cancer survivors will be living in the USA by 2024 [1].
Although the achievements in cancer care which have led to the growing number of cancer survivors should be celebrated, it is becoming increasingly apparent that these successes have not come without a cost. Not only are cancer survivors at risk of progressive and/or recurrent disease and secondary cancer, they are also at risk of functional decline, psychosocial distress, and multiple chronic co-morbid conditions [2–4]. Notably, several reports have indicated that cardiovascular disease (CVD) is a significant health issue among many cancer survivors contributing to disease burden and as many as half of non-cancer related deaths [5–13]. While seemingly distinct, several coinciding risk factors for cancer and CVD, including advancing age and modifiable risk factors (e.g., smoking, obesity, physical inactivity), suggest a common underlying biological pathway [14]. Moreover, the well-established cardiotoxic effects of several antineoplastic therapies [15, 16] as well as the lifestyle changes associated with treatment (e.g., weight gain, deconditioning) function to intensify CVD risk [17]. In light of significant disease burden associated with cancer survivorship, intervention strategies aimed at improving the overall health status of a population at risk of excess morbidity is needed.
Physical activity (PA) has long been established as a powerful tool in the prevention and treatment of chronic disease, including some cancers and CVD [18, 19]. PA has also been shown to reduce all-cause mortality, including both cancer [20] and cardiovascular-related mortality [21]. Although it has been well documented that PA can modify traditional CVD risk factors [19], emerging evidence suggests that PA may also play an important role in mediating the cardiotoxic effects of several antineoplastic therapies [22–24]. However, limited data exists on the prevalence of CVD risk factors among adult cancer survivors. Likewise, the relationship between PA, CVD risk, and events among adult cancer survivors has not been well described. Accordingly, this study explored the relative CVD burden among a population-based sample of adult cancer survivors from Atlantic Canada. We also examined the relationship between CVD risk and PA among survivors and compared with age-sex matched controls. Specifically, using a nested, retrospective design, the present analyses aimed to:
-
1.
Describe the prevalence of major CVD risk factors (defined as hypertension and/or diabetes) and major CVD events (defined as myocardial infarction and/or stroke) among adult cancer survivors and age-sex matched non-cancer controls;
-
2.
Explore the association between the rate of major CVD events among cancer survivors and compare to age-sex matched controls using a simplified prediction model;
-
3.
Examine the relationship between PA and major CVD risk factors among cancer survivors and matched non-cancer controls and to determine whether these associations differed between survivors and controls; and
-
4.
Assess if the relationship between PA and major CVD risk changed when adjusting for common CVD risk factors.
Methods
Population
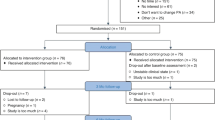
This retrospective nested case-control study drew participants from the population-based Atlantic Partnership for Tomorrow’s Health (PATH) cohort. Atlantic PATH is part of the Canadian Partnership for Tomorrow Project, a national study examining the influence of genetic, environmental, and lifestyle factors in the development of cancer and chronic disease [25]. In brief, 33,587 Atlantic PATH participants, ages 35–69 years, were recruited between 2009 and 2014 from the general population of the four Atlantic Canadian provinces (Nova Scotia, New Brunswick, Newfoundland and Labrador, and Prince Edward Island). The study protocol was approved by the appropriate provincial and regional ethics boards and all participants gave written informed consent prior to participation. For the current analysis, we identified 1526 cancer survivor participants between the ages of 35–69 years with complete cardiovascular health data. Each survivor was then matched to four non-cancer participants (n = 6034) of the same gender and born within 2 years of the survivor.
Data collection
Study participants were recruited through invitation, wide-spread provincial advertising campaigns, and community and workplace outreach activities. Baseline sociodemographic, health events (i.e., cancer, diabetes, hypertension), risk factors thought to influence CVD risk, CVD major events (defined as myocardial infarction or stroke), and age of diagnosis of health events were captured through self-report. The presence/absence of cancer, CVD risk factors and major cardiovascular events were dichotomized as yes/no. PA was assessed using both the short and long form of the International Physical Activity Questionnaire (IPAQ) [26]. In accordance with the IPAQ scoring protocol (https://sites.google.com/site/theipaq/scoring-protocol), data from both forms were used to calculate categorical (low, moderate, high) PA scores. Self-reported time spent sitting (sedentary behaviors) was also assessed by the IPAQ by calculating the sum of the time spent sitting (e.g., at a desk, watching television, reading, and time spent sitting in a vehicle for the purpose of transportation) in accordance with the IPAQ scoring protocol. Total daily time spent sitting was dichotomized into <4 h to ≥4 h based on the increased association with cardiometabolic disease and all-cause mortality in individuals spending ≥4 h each day sitting [27]. Self-reported health status was recorded into two levels; excellent/very good/good and fair/poor. For tobacco use, participants who reported never having smoked 100 cigarettes in their life or had not used other types of tobacco on a regular basis for at least 6 months were defined as never smokers. Former smokers were defined as those who reported having smoked at least 100 cigarettes in their lifetime but did not use any type of tobacco within the previous 30 days. Current smokers were defined as those who reported smoking at least 100 cigarettes in their lifetime and smoked during the past 30 days. Participant responses were reclassified as never smoked or ever smoked (former and current smokers). For alcohol consumption, participants were classified as an abstainer if they reported never drinking alcohol, occasional drinker if they reported drinking alcohol two to three times per month or less, regular drinker if they reported drinking alcohol more than once a week but no more than three times per week, and habitual drinker if they reported drinking four or more times per week. Participants were asked to report how many daily servings of fruit, fruit juices, and vegetables they eat on a typical day. Responses were coded as not meeting Health Canada Food Guidelines (≤6 daily servings) or meeting guidelines (≥7 daily servings) [28]. Physical measurements including height, weight, and waist circumference were measured by research nurses at a study assessment center. Body weight and height were measured by a Seca stadiometer and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Waist circumference was measured at the top of iliac crest using a Lufin steel tape. Overweight was defined as a BMI between 25.0–29.9 kg/m2 and obesity was defined as a BMI greater than 30.0 kg/m2. Abdominal adiposity was defined as a waist circumference ≥102 cm for men and ≥88 cm for women [29].
Statistical analyses
Data management and analyses were performed with SAS statistical package version 9.4 (SAS Institute, Cary, North Carolina). In brief, we calculated frequencies and relative frequencies of cancer survivor participants and sex-age matched non-cancer controls for categorical characteristics on education, employment, household income, marital status, and ethnicity. Associations between these characteristics were examined using Chi-square test (Table 1).
We employed univariable logistic regression models to compute odds ratios (OR) and 95% confidence intervals (CI) of cancer for individuals with different levels of each selected CVD risk factors, including PA, sedentary behavior, smoking status, alcohol consumption, daily fruit/vegetable intake, body mass index, and abdominal adiposity (Table 2). Multiple logistic regression models were employed to compute OR and 95% CI (with Bonferroni adjustment) of two major cardiovascular risk factors (i.e., hypertension and diabetes) for individuals with different levels of PA with adjustment for sex, age, and cancer status if applicable. Further analyses were performed by adding additional risk factors into the basic model separately and stratified within each specific level of the additional risk factors correspondingly. All analyses were performed for cancer survivor participants and non-cancer controls. None of the interactions between PA and CVD risk factors that we tested achieved significance. Trend tests were performed by using PA in the model as a continuous variable (Table 3). A simplified CVD risk score was calculated using a simple risk prediction model that utilized sex, age, body mass index, systolic blood pressure, antihypertensive medication usage, current smoking, and diabetic status. Participants were grouped into four CVD risk quartiles using three percentile (P) cut points (P25 = .01, P50 = .05, P75 = .43) and the relationship between risk score and major CVD events was explored using univariable logistic regression models. Statistical significance was defined as p value <.05 (two-sided).
Results
Descriptive statistics were generated for sociodemographic and selected lifestyle characteristics using overall and age-sex matched data and are presented in Tables 1 and 2. The mean age of cancer diagnosis was 48 years (SD = 12 years). Mean time since cancer diagnosis was 9.7 years (SD = 9.4 years). Overall, compared to controls, cancer survivor participants were 84% more likely to self-report worse (i.e., fair or poor) overall health status than controls (OR = 1.84; 95% CI 1.5–2.2, p < .0001).
CVD risk and major events
No significant differences between cancer survivors and non-cancer controls were found for smoking status, obesity status (BMI category), abdominal adiposity (waist circumference), time spent sitting (i.e., sedentary behaviors), or fruit and vegetable consumption (i.e., meeting guidelines vs. not meeting guidelines). Cancer survivors were significantly less likely to consume alcohol and were less physically active than those without a history of cancer. Cancer survivors were significantly more likely to report having hypertension (OR = 1.60; 95% CI 1.03–1.3, p = .02) and diabetes (OR = 1.27; 95% CI 1.03–1.16, p = .02). Of those survivors reporting CVD risk factors, 63% reported a diagnosis of hypertension and 61% reported a diagnosis of diabetes prior to their cancer diagnosis. While not significant, cancer survivors were 41% more likely to have suffered a stroke (OR = 1.41; 95% CI 0.91–2.2, p = .12) and 24% more likely to have suffered a myocardial infarction (OR = 1.24; 95% CI 0.87–1.76, p = .32) (Table 2). Of the 69 major CVD events self-reported by cancer survivors, 74% occurred prior to the first cancer diagnosis.
Employing a simple risk prediction model that utilized age, sex, BMI, systolic blood pressure, antihypertensive medication usage, current smoking, and diabetic status [30], it was found that cancer survivors had a 30% higher absolute risk of having ever experienced a major CVD event in comparison to controls (OR = 1.3; 95% CI 1–1.7, p = .07). Combined, those in second, third, and fourth quartile had 1.8 times (95% CI 1.1–2.9), 2.5 times (95% CI 1.6–3.8), and 4.6 times (95% CI 3.1–7.0) the risk of a major CVD event as compared to those in the first quartile. For survivors, those in the second, third, and fourth quartiles had 1.3 times (95% CI 0.6–3.0), 1 times (95% CI 0.4–2.3), and 2.9 times (95% CI 1.4–5.8) the risk for a major CVD event as compared to those in the first quartile. For non-cancer controls, those in the second, third, and fourth quartiles had 2.1 times (95% CI 1.2–3.8), 3.4 times (95% CI 2.0–5.9), and 5.8 times (95% CI 3.4–9.8) the risk for a major CVD event as compared to those in the first quartile. With the exception of the third quartile, compared to controls, cancer survivors in the first, second, and fourth quartiles had a 2.6 (95% CI 1.2–5.6, p = .015), 1.6 (95% CI 0.9–3.0, p = .130), and 1.3 (95% CI 0.8–2.0, p = .270) times greater risk for a major CVD event, respectively.
PA and CVD risk
Using multiple logistic regression, overall compared to those in the low PA group, those in the moderate (OR = 0.73; 95% CI 0.64–0.84) and high (OR = 0.66; 95% CI 0.58–0.76) PA groups were significantly less likely to report major CVD risk factors (i.e., hypertension and/or diabetes). For cancer survivors, the odds of having a major CVD risk factor was about 35% lower for those in the moderately active group (OR = 0.65; 95% CI 0.48–0.88) and 45% lower in the highly physically active group (OR = 0.55; 95% CI 0.4–0.73). For no cancer controls, the odds of having a major CVD risk factors was about 25% lower for those in the moderately active group (OR = 0.75; 95% CI 0.64–0.88) and 30% lower for those in the highly physically active group (OR = 0.70; 95% CI 0.60–0.81). To assess whether the effect of PA differed when controlling for additional CVD risk factors, additional analyses were run to adjust for alcohol consumption, body mass index, daily fruit and vegetable consumption, sedentary behavior, smoking status, and waist circumference/abdominal adiposity. With the exception of body mass index (low/normal weight) for controls and normal abdominal adiposity for controls and cancer survivors, the positive relationship between PA and lowered risk of major CVD risk factors remained unchanged (Table 3).
Discussion
In this population-based study of cancer survivors and age-sex matched controls, we found that both cancer survivors and non-cancer controls had multiple modifiable lifestyle CVD risk factors suggesting the need for intervention in both groups (Table 2). For example, relative to Canadian population data which indicates that about 22% of Canadian adults (20–79 years) suffer from hypertension [31], the present study shows a higher prevalence of hypertension among both non-cancer controls (29%) and cancer survivors (32%) which may reflect both the age structure of the cohort and the high disease prevalence rate in Atlantic Canadians. While the prevalence of several lifestyle risk factors (i.e., sedentary behavior, smoking status, diet, BMI, abdominal adiposity) were similar among the groups, survivors reported a higher prevalence of diabetes (8.3%) compared to both the non-cancer controls (6.7%) and the Canadian average (6.8%) [32]. These findings are consistent with those of other cohort studies which have found that the prevalence of major CVD risk factors (i.e., hypertension, diabetes) and CVD was higher in cancer survivors when compared to non-cancer controls [10, 11, 33, 34].
The manifestation of CVD in cancer survivors has been presented as being multifactorial, including overlapping risk factors (e.g., obesity, diabetes), shared biological pathways (e.g., inflammation) [14], and exposure to cardiotoxic antineoplastic therapies [17]. Notably, survivors in the current study had a 30% absolute higher risk of having ever experienced a major CVD event compared to age-sex matched controls. While the cardiotoxic impact of several commonly used cancer therapies has been well documented [35], as the majority (%) of the CVD events preceded the cancer diagnosis, it appears that pre-existing cardiovascular morbidity is a significant concern for many newly diagnosed patients and highlights the need for pre-treatment risk assessment and optimizing cardiovascular health for all cancer survivors [36]. As comorbidities may influence treatment decisions and have been shown to impact overall survival and all-cause mortality, there is a need for the ongoing management of pre-existing conditions without interfering with effective antineoplastic regimes [13, 37].
Given the relatively small sample size and lack of treatment data, it was not possible to examine the impact of various diagnoses and therapeutic exposures on CVD risk or major cardiac events. Despite this limitation, the higher overall risk of major CVD events in cancer survivors provides additional rationale for the need for greater attention to CVD management and prevention in this growing segment of the population. Moreover, although mortality data was not available for the current analyses, the relationship between CVD morbidity and premature mortality in cancer survivors has been previously reported [6, 11, 38] again highlighting the need for improved efforts to identify risk factors and interventions that reduce the burden of CVD morbidity and mortality.
While the distribution of characteristics in the PATH cohort is generally representative of the Atlantic Canadian population, there is an overrepresentation of women and individuals with higher socioeconomic status and post-secondary education. Thus, although we acknowledge that our cancer survivor cohort may not be entirely a representative of the broader cancer survivor population, this study is one of only a few that have examined the prevalence of CVD risk factors and the relationship between PA and CVD in adult cancer survivors [17]. The results of the current study indicate that, with the exception of PA levels, hypertension, and diabetes, all CVD risk factors examined were common among the non-cancer controls and cancer survivors. Of note, as compared to age-sex matched controls, cancer survivors were significantly more likely to engage in low levels of activity and less likely to engage in moderate to high levels of PA. As PA data was collected cross-sectionally, a temporal pattern between PA level, cancer diagnosis, and CVD risk cannot be established. However, while the potential for reverse causation bias cannot be overlooked, the results suggest that PA level appears to be an important predictor of CVD risk with those in the highest PA category showing the greatest risk reduction (45%) for two prevalent CVD risk factors, hypertension and diabetes. Importantly, the inclusion of additional CVD risk factors into the model did not attenuate this finding.
While not significant, data from the present study suggest that those with a history of cancer have a 30% absolute higher risk of ever having experienced a major CVD event. Moreover, as recent data suggests that <10% of cancer patients will be active during treatment and only 20–30% will be active post-treatment [39], it is reasonable to assume that PA levels of the present survivor cohort have likewise decreased since the time of cancer diagnosis, thereby contributing to a potentially higher CVD risk profile. Overall, these data support the current emphasis on promoting PA for cancer survivors specifically for the potential cardioprotective benefits [40].
A considerable strength of the present study was the population-based study design which included survivors and non-cancer controls that were representative of the same source population. Notwithstanding, the data provides only a cross-sectional representation of the population and does not permit for an assessment of cardiac risk/events that may change as a result of a cancer diagnosis and/or changes in PA levels over time. In addition, given the relatively small number of cancer survivors, we were not able to explore CVD risk and morbidity among survivors of different cancer diagnoses. Moreover, detailed treatment information was not available, thereby precluding additional analyses examining the long-term implications of anti-cancer therapies and the identification of survivors at the greatest risk of future cardiac morbidity. Future research would benefit from a larger sample size and detailed treatment data. Likewise, long-term follow-up and data linkage are needed to explore the underlying factors contributing to CVD in cancer survivors and the extent of disease burden across survivor sub-groups over time. Finally, as the bulk of the lifestyle and health events were captured by self-report, this data is subject to response bias resulting in an under or over-reporting of a behavior or events [41, 42].
Overall, this study shows that while CVD morbidity is prevalent among the cohort, cancer survivors appear to be at risk of greater CVD comorbidity and burden than non-cancer controls. Of note, it appears that PA may confer an important cardioprotective benefit reducing CVD risk by as much as 50%. This study contributes to a growing body of evidence highlighting the need for the identification and management of CVD risk factors, including PA, in cancer survivors.
In brief, PA has been demonstrated to be a feasible and effective means to improve quality of life and reduce morbidity and mortality in cancer survivors. Regrettably, despite the development of evidence-based guidelines [43], PA has not yet been widely implemented as a standard of care in the oncology setting largely due to a lack of resources, PA expertise, and awareness of benefits [44, 45]. While much is left to be understood, clinicians and survivors alike need to be made aware of the evidence regarding the benefits and safety of PA to promote widespread adoption, ultimately improving survivorship.
References
DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics. CA Cancer J Clin. 2014;64(4):252–71.
Demark-Wahnefried W, Aziz NM, Rowland JH, et al. Riding the crest of the teachable moment: promoting long-term health after the diagnosis of cancer. J Clin Oncol. 2005;23(24):5814–30.
Eakin EG, Youlden DR, Baade PD, et al. Health status of long-term cancer survivors: results from an Australian population-based sample. Cancer Epidemiol Biomark Prev. 2006;15(10):1969–76.
Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci 2003;58(1):82–91.
Baade PD, Fritschi L, Eakin EG. Non-cancer mortality among people diagnosed with cancer (Australia). Cancer Causes Control. 2006;17(3):287–97.
Bradshaw PT, Stevens J, Khankari N, et al. Cardiovascular disease mortality among breast cancer survivors. Epidemiology. 2016;27(1):6–13.
Patnaik JL, Byers T, DiGuiseppi C, et al. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. 2011;13(3):R64.
Chow EJ, Mueller BA, Baker KS, et al. Cardiovascular hospitalizations and mortality among recipients of hematopoietic stem cell transplantation. Ann Intern Med. 2011;155(1):21–32.
Al-Kindi SG, Abu-Zeinah GF, Kim CH, et al. Trends and disparities in cardiovascular mortality among survivors of Hodgkin lymphoma. Clin Lymphoma Myeloma Leuk. 2015;15(12):748–52.
Armenian SH, Chow EJ. Cardiovascular disease in survivors of hematopoietic cell transplantation. Cancer. 2014;120(4):469–79.
Armenian SH, Xu L, Ky B, et al. Cardiovascular disease among survivors of adult-onset cancer: a community-based retrospective cohort study. J Clin Oncol. 2015; doi:10.1200/JCO.2015.64.0409.
Kreatsoulas C, Subramanian SV. An emerging double burden of disease: the prevalence of individuals with cardiovascular disease and cancer. J Intern Med. 2013;275:494–504.
Janssen-Heijnen MLG, Szerensci K, van de Schans SAM, Maas HAAM, Widdershoven JW, Coebergh JWW. Cancer patients with cardiovascular disease have survival rates to cancer patients within the age-cohort of 10 years older without cardiovascular morbidity. Crit Rev Oncol Hematol. 2010;76:196–207.
Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133:1104–14.
O'Hare M, Sharma A, Murphy K, et al. Cardio-oncology part I: chemotherapy and cardiovascular toxicity. Expert Rev Cardiovasc Ther. 2015;13(5):511–8.
Rosa GM, Gigli L, Tagliasacchi MI, et al. Update on cardiotoxicity of anti-cancer treatments. Eur J Clin Investig. 2016;46(3):264–84.
Jones LW, Haykowsky MJ, Swartz JJ. Early breast cancer therapy and cardiovascular injury. J Am Coll Cardiol. 2007;50(15):1435–41.
Sallis R. Exercise is medicine: a call to action for physicians to assess and prescribe exercise. Phys Sportsmed. 2015;43(1):22–6.
Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–9.
Li T, Wei S, Shi Y, et al. The dose-response effect of physical activity on cancer mortality: findings from 71 prospective cohort studies. Br J Sports Med. 2016;50(6):339–45.
Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–34.
Scott JM, Armenian S, Giralt S, et al. Cardiovascular disease following hematopoietic stem cell transplantation: pathogenesis, detection, and the cardioprotective role of aerobic training. Crit Rev Oncol Hematol. 2016;98:222–34.
Scott JM, Lakoski S, Mackey JR, et al. The potential role of aerobic exercise to modulate cardiotoxicity of molecularly targeted cancer therapeutics. Oncologist. 2013;18(2):221–31.
Kirkham AA, Davis MK. Exercise prevention of cardiovascular disease in breast cancer survivors. J Oncol. 2015; doi:10.1155/2015/917606.
Borugian MJ, Robson P, Fortier I, et al. The Canadian Partnership for Tomorrow Project: building a pan-Canadian research platform for disease prevention. CMAJ. 2010;182(11):1197–201.
Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Chau JY, Grunseit A, Midthjell K, et al. Sedentary behaviour and risk of mortality from all-causes and cardiometabolic diseases in adults: evidence from the HUNT3 population cohort. Br J Sports Med. 2015;49(11):737–42.
Health Canada. Eating well with Canada's Food Guide. Health Canada, Ottawa, Ont., Canada. http://www.hc-sc.gc.ca/fn-an/food-guide-aliment/index-eng.php. 2011.
Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–52.
D'Agostino Sr RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743–53.
Wilkins K, Campbell NR, Joffres MR, et al. Blood pressure in Canadian adults. Health Rep. 2010;21(1):37–46.
Public Health Agency of Canada. Diabetes in Canada: facts and figures from a public health perspective. Ottawa, Ont: Public Health Agency of Canada ; 2011.http://www.phac-aspc.gc.ca/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/index-eng.php
Daher IN, Daigle TR, Bhatia N, et al. The prevention of cardiovascular disease in cancer survivors. Tex Heart Inst J. 2012;39(2):190–8.
Weaver KE, Foraker RE, Alfano CM, et al. Cardiovascular risk factors among long-term survivors of breast, prostate, colorectal, and gynecologic cancers: a gap in survivorship care? J Cancer Surviv. 2013;7(2):253–61.
Curigliano G, Cardinale D, Dent S, et al. Cardiotoxicity of anticancer treatments: epidemiology, detection, and management. CA Cancer J Clin. 2016; doi:10.3322/caac.21341.
Knobf MT, Coviello J. Lifestyle interventions for cardiovascular risk reduction in women with breast cancer. Curr Cardiol Rev. 2011;7(4):250–7.
Søgaard M, Thomsen RW, Bossen KS, et al. The impact of comorbidity on cancer survival: a review. Clin Epidemiol. 2014;5(Suppl 1):3–29.
Patnaik JL, Byers T, Diguiseppi C, et al. The influence of comorbidities on overall survival among older women diagnosed with breast cancer. J Natl Cancer Inst. 2011;103(14):1101–11.
Garcia DO, Thomson CA. Physical activity and cancer survivorship. Nutr Clin Pract. 2014;29(6):768–79.
Kirkham AA, Bland KA, Sayyari S, et al. Clinically relevant physical benefits of exercise interventions in breast cancer survivors. Curr Oncol Rep. 2016;18(2):12.
Adams SA, Matthews CE, Ebbeling CB, et al. The effect of social desirability and social approval on self-reports of physical activity. Am J Epidemiol. 2005;161(4):389–98.
Prince SA, Adamo KB, Hamel ME, et al. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56.
Schmitz KH, Courneya KS, Matthews C, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42(7):1409–26.
Keogh J, Olsen A, Climstein M, Sargeant S, Jones L. Benefits and barriers of cancer practitioners discussing physical activity with their cancer patients. J Canc Educ. 2015.
Santa Mina D, Alibhai SM, Matthew AG, et al. Exercise in clinical cancer care: a call to action and program development description. Curr Oncol. 2012;19(3):e136–44.
Acknowledgements
The authors gratefully acknowledge the funding from the Canadian Partnership Against Cancer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Atlantic PATH is part of the Canadian Partnership for the Tomorrow Project funded by the Canadian Partnership Against Cancer. The opinions, results, and conclusions reported in this paper are those of the authors.
Conflict of interest
Melanie Keats, Yunsong Cui, Scott Grandy, and Louise Parker all declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from participants at the time of original study enrollment.
Rights and permissions
About this article
Cite this article
Keats, M.R., Cui, Y., Grandy, S.A. et al. Cardiovascular disease and physical activity in adult cancer survivors: a nested, retrospective study from the Atlantic PATH cohort. J Cancer Surviv 11, 264–273 (2017). https://doi.org/10.1007/s11764-016-0584-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0584-x