Abstract
Objective
Currently, several near-infrared spectroscopy oximetry devices are used for detecting cerebral ischemia during cardiopulmonary bypass (CPB) surgery. We investigated whether two different models of near-infrared spectroscopy oximetry devices affect the assessment of cerebral ischemia and its management during CPB.
Methods
From January 2017 to August 2017, 70 adult cardiovascular surgery cases were randomly assigned to 1 of 2 different near-infrared spectroscopy oximetry devices. The devices were INVOS 5100C (Medtronic, Minneapolis, MN, USA) (group I; n = 35) and FORE-SIGHT ELITE (CAS Medical Systems, Branford, CT, USA) (group F; n = 35).
Results
There were no significant differences in patient characteristics. The rSO2 values were significantly higher for patients in group F than for patients in group I. Scalp–Cortex distance showed negative correlations with the mean rSO2 values in group I (P = 0.01). Interventions for low rSO2 during CPB for groups I and F were increase perfusion flow (13:5; P = 0.03), blood transfusion (7:1; P = 0.02), and both (6:1; P = 0.04), respectively. The Scalp–Cortex distance in group I was significantly longer in patients who required intervention than in patients who did not (17.1 ± 2.5 vs 15.1 ± 1.6 mm; P = 0.007).
Conclusions
It is inappropriate to use the same intervention criteria for different near-infrared spectroscopy oximetry devices. Moreover, brain atrophy influence rSO2 values depending on device selection. It is important to note that inappropriate device selection may misguide perfusionists into performing unnecessary or excessive intervention during CPB.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There are currently several near-infrared spectroscopy (NIRS) oximetry devices commercially available and used for detecting cerebral ischemia during cardiopulmonary bypass (CPB). These devices may help surgeons and anesthesiologists avoid poor cerebral perfusion, which can result in perioperative neurological adverse events. These devices operate on the same measurement principles; however, their algorithms of detection and calculation of regional cerebral oxygen saturation (rSO2) value are different, and it is inappropriate to compare values measured by such different devices directly. Thus, measured values and trends fluctuate depending on devices.
Our previous retrospective evaluation of 223 adult patients undergoing cardiac surgery has revealed that brain atrophy, poor left ventricular ejection function, anemia, and hemodialysis had significant correlations with low initial cerebral rSO2 values measured by INVOS 5100C (Medtronic, Minneapolis, MN, USA) [1]. In clinical settings, these fluctuations of measured values affect the decision making for intervention during CPB.
In this study, 70 patients were randomly assigned to 1 of 2 groups in which surgery was performed using 2 different devices: the INVOS 5100C and the FORE-SIGHT ELITE (CAS Medical Systems, Branford, CT, USA). We prospectively evaluated intraoperative rSO2 values in each group and the presence or absence of intervention for low rSO2 value during CPB.
Subjects
From January 2017 to August 2017, 96 patients underwent elective cardiac surgery at Kitasato University Hospital. Patients ≤ 12 years of age; patients who did not undergo preoperative brain magnetic resonance imaging; and patients with a medical history of acute cerebral infarction, intracranial hemorrhage or neurosurgery, surgery performed in a nonsupine position, off-pump coronary artery bypass surgery, and/or with left ventricular assist devices were excluded from the study. Finally, 70 patients were enrolled.
Methods
Each patient was randomly assigned to 1 of 2 groups utilizing either the INVOS 5100C (group I; n = 35) or the FORE-SIGHT ELITE (group F; n = 35). This research was conducted with the approval of the Kitasato University Medical Ethics Organization (approval number: KMEO B16-96). All patients gave informed consent before inclusion in the study.
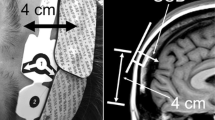
Scalp–Cortex distance
Preoperative brain magnetic resonance imaging was routinely evaluated for detection of cerebrovascular disease. Scalp–Cortex distance (SCD) was measured on a T1-weighted image of the mid-sagittal plane as the distance from the surface of the scalp on the upper forehead, at 4 cm from the superciliary arch, to the frontal cerebral cortex (Fig. 1).
Cerebral rSO2 monitoring
From anesthetic induction to the end of surgery, continuous monitoring of cerebral rSO2 was carried out in each group. Optodes of each device were placed on the patient’s forehead, at 4 cm from the superciliary arch, to avoid the frontal sinus [2]. The values were recorded at anesthetic induction, CPB start, aortic cross clamp, and CPB end.
Interventions during CPB
Interventions for low rSO2 during CPB were defined as approaches to improve rSO2 values such as increasing perfusion flow rate, increasing inspired oxygen fraction, and blood transfusion. Increasing perfusion flow should be considered as primary intervention method, and the others as supplemental. Since there is no established value of rSO2 that should be maintained during CPB to avoid postoperative cognitive disorder, the thresholds for intervention were set as an absolute drop to below 40% or a 10% relative decrease from the initial baseline value. These thresholds were based on the recommendation by the manufacturer of INVOS 5100C, Medtronic, with clinical modifications.
Data collection
Patient medical records were reviewed for preoperative clinical and demographic characteristics according to the hospital information system.
Data analysis
Continuous variables were presented as mean ± standard deviation. For each group, odds ratios for the presence of intervention and correlations between rSO2 value and SCD were evaluated.
Differences with P < 0.05 were considered statistically significant. Statistical analyses were performed using JMP Software, version 12.0 (SAS Institute, Carey, NC, USA).
Results
Patient characteristics
Patient characteristics including age; sex; body surface area; medical history (stroke, hypertension, diabetes mellites, and hemodialysis); preoperative left ventricular ejection fraction; hemoglobin concentration (Hb); and SCD are shown in Table 1. There were no significant differences between the 2 groups.
Operative outcomes
Surgical procedures, CPB time, perfusion index, minimum core temperature, blood transfusion during CPB, and postoperative neurological adverse events are shown in Table 2. In group I, 1 patient of aortic valve replacement experienced convulsions and 1 patient of aortic valve replacement, tricuspid valve annuloplasty, coronary artery bypass and maze procedure experienced delayed emergence. However, there were no significant differences between the 2 groups.
Intraoperative rSO2 values
The rSO2 values were recorded at anesthetic induction, CPB start, aortic cross clamp, and CPB end. The values for group F are significantly higher than those for group I. However, there were no significant differences in mean mixed venous oxygen saturation value in the 2 groups (Table 3).
Interventions for low rSO2 value
Interventions for low rSO2 during CPB for group I and group F were increase perfusion flow (13:5; P = 0.03), blood transfusion (7:1; P = 0.02), and both (6:1; P = 0.04), respectively. Interventions were significantly more frequent in group I, despite similar patient backgrounds (Table 4). The cases of high perfusion pressure of > 400 mmHg at the inlet of the artificial lung were managed only with blood transfusion without increasing perfusion flow.
SCD and rSO2 values
In group F, there was no correlation between the mean rSO2 value and SCD. In contrast, the mean rSO2 value in group I had a significant negative correlation with SCD (Fig. 2). In group I, in which mean rSO2 and SCD were significantly correlated, the relationship between SCD and the presence or absence of intervention was examined. The mean SCD of interventions were significantly longer than that of noninterventions (17.1 ± 2.5 vs 15.1 ± 1.6 mm; P = 0.007). A cutoff value of SCD for group I was determined by ROC analysis. The area under the curve was 0.75, and a cutoff value for intervention was SCD > 17.6 mm (Table 5) (Fig. 3).
Discussion
Since CPB surgery was first introduced, perioperative stroke emerged as a serious adverse event. In 1965, Pillsbury et al. reported their 450 consecutive open-heart surgeries. The incidence of stroke was 2.0% (n = 9), and the mortality rate was 55.6% (n = 5) [3]. Recent meta-analysis revealed that the incidence of perioperative stroke after cardiac surgery was 2.03%. The operative and late mortality were 21.3 and 10.9%, respectively [4]. It is inappropriate to compare these studies with studies reported by clinicians with different historical and clinical backgrounds. However, despite much innovative progress, perioperative stroke remains a complication that concerns surgeons.
Real-time, noninvasive monitoring of tissue oxygenation using an NIRS oximetry device was first reported in 1977 [5]. Today, clinical utility of such devices has been established and commonly applied to detect cerebral ischemia during CPB surgery. In 184 Japanese medical centers in which cardiac surgery was performed, 155 (84%) used intraoperative NIRS oximetry monitoring, and 70 (38%) used it routinely [6]. Although several NIRS oximetry devices are commercially available, their algorithms of detection and calculation of rSO2 value are different. Thus, measurement results may vary, and factors that influence measurements must be weighed differently [6].
Fluctuations in measured rSO2 values with the INVOS 5100C during cerebral desaturation are reportedly significantly wider than those with the EQUANOX 7600 (Nonin Medical Inc, Plymouth, MN, USA), and a similar but nonsignificant trend was observed for the INVOS 5100C compared with the FORE-SIGHT ELITE [7]. Greenberg et al. reported that the FORE-SIGHT ELITE was significantly less affected by extracranial contamination such as dermal ischemia than the INVOS 5100C [8]. These reports suggest that vulnerability of noise-tolerance specifications of INVOS 5100C. In addition, recent report suggests that rSO2 alone is insufficient in describing cerebral metabolism and predicting neurological outcome [9].
In our study, intraoperative interventions for lower rSO2 value were performed more frequently in group I than in group F. Measured decreasing rSO2 values in group I were significantly affected by longer SCD, which means that brain atrophy may influence rSO2 values, depending on device selection. Inappropriate intervention for pseudo-lower rSO2 values may have been performed without the presence of actual ischemia. In particular, SCD of longer than 17.6 mm in group I may misguide perfusionists to perform unnecessary or excessive interventions. In such cases, INVOS 5100C should not be used. An appropriate application of the intervention threshold such as decreasing rSO2 value of 40% assumes that the value is less affected by non-ischemic parameters. It is unlikely that there were more cases of cerebral ischemia in group I than in group F in a similar clinical populations. Moreover, it is inappropriate to use the same intervention criteria for different NIRS oximetry devices during CPB. Further study will be required to determine optimal value of rSO2 to be maintained for each NIRS device.
Study limitations
The limitation of this study is small sample size (≤ 100 patients) in a single-center design. Moreover, thresholds for intervention against desaturation may vary depending on each clinical team. Additional multicenter studies should be carried out in larger patient populations to investigate device selection and measured cerebral rSO2 values during CPB surgery and the impact on the need for interventions.
Conclusion
We report a prospective study to investigate the relationship between NIRS oximetry device selection and measured cerebral rSO2 values during CPB and its influence on whether interventions to improve desaturation should be performed. In the INVOS 5100C group (group I) in our study, SCD longer than 17.6 mm may compel clinicians to perform excessive interventions. In such cases, INVOS 5100C should not be used. Moreover, it is inappropriate to use the same intervention criteria for different NIRS oximetry devices during CPB. Device selection affect intervention for desaturation during CPB. Appropriate device selection should be considered for safe and minimally invasive cardiac surgery.
References
Kobayashi K, Kitamura T, Kohira S, Torii S, Horai T, Hirata M, et al. Factors associated with a low initial cerebral oxygen saturation value in patients undergoing cardiac surgery. J Artif Organs. 2017;20:110–6.
Gregory AJ, Hatem MA, Yee K, Grocott HP. Optimal placement of cerebral oximeter monitors to avoid the frontal sinus as determined by computed tomography. J Cardiothorac Vasc Anesth. 2016;30:127–33.
Pillsbury RC, Lower RR, Hurley EJ, Dong E Jr, Shumway NE. Four hundred and fifty consecutive open heart operations. Calif Med. 1965;102:181–4.
Gaudino M, Rahouma M, Di Mauro M, Yanagawa B, Abouarab A, Demetres M, et al. Early versus delayed stroke after cardiac surgery: a systematic review and meta-analysis. J Am Heart Assoc. 2019;8:e012447.
Jöbsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science. 1977;198:1264–7.
Yoshitani K, Kawaguchi M, Ishida K, Maekawa K, Miyawaki H, Tanaka S, et al. Guidelines for the use of cerebral oximetry by near-infrared spectroscopy in cardiovascular anesthesia: a report by the cerebrospinal Division of the Academic Committee of the Japanese Society of Cardiovascular Anesthesiologists (JSCVA). J Anesth. 2019;33:167–96.
Tomlin KL, Neitenbach AM, Borg U. Detection of critical cerebral desaturation thresholds by three regional oximeters during hypoxia: a pilot study in healthy volunteers. BMC Anesthesiol. 2017. https://doi.org/10.1186/s12871-016-0298-7.
Greenberg S, Murphy G, Shear T, Patel A, Simpson A, Szokol J, et al. Extracranial contamination in the INVOS 5100C vs the FORE-SIGHT ELITE cerebral oximeter: a prospective observational crossover study in volunteers. Can J Anaesth. 2016;63:24–30.
Rajaram A, Milej D, Suwalski M, Yip LCM, Guo LR, Chu MWA, et al. Optical monitoring of cerebral perfusion and metabolism in adults during cardiac surgery with cardiopulmonary bypass. Biomed Opt Express. 2020;11:5967–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kobayashi, K., Kitamura, T., Kohira, S. et al. Near-infrared spectroscopy device selection affects intervention management for cerebral desaturation during cardiopulmonary bypass surgery. Gen Thorac Cardiovasc Surg 70, 11–15 (2022). https://doi.org/10.1007/s11748-021-01659-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01659-5