Abstract
Cerebral Oximetry by Near-infrared Spectroscopy (NIRS) has been used in cardiovascular anesthesia, but there was no guideline of regional cerebral oxygen saturation measured by cerebral oximetry by NIRS. This guideline provides recommendations applicable to patients at a risk of developing cerebral ischemia in cardiovascular surgery. Guidelines are intended to define practices meeting the needs of patients in most, but not all, circumstances, and should not replace clinical judgment. The Japanese Society of Cardiovascular Anesthesiologists (JSCVA) Task Force on Guidelines make an effort to ensure that the guideline writing committee contains broad views in using cerebral oximetry. Adherence to recommendations could be enhanced by shared decision making between healthcare providers and patients. This guideline was focused on cerebral oximetry of pediatric and adult cardiovascular disease. We hope this guideline would play an important role in using cerebral oximetry by measured NIRS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Perioperative brain injuries such as intraoperative cerebral infarction and postoperative cognitive dysfunction (POCD) have an immense impact on a variety of patient outcomes. These injuries prolong patients’ hospital stays, increase their mortality rates, and compromise their functional status, thereby increasing family burdens and medical costs. Given the increasing annual number of elderly patients undergoing cardiovascular surgeries, the importance of preventing perioperative brain injuries cannot be underestimated. The etiology of these conditions is multifactorial. Their prevention requires multidisciplinary strategies involving respiratory and cardiovascular management, body temperature management, monitoring of cerebral blood flow and metabolism (e.g., measurement of cerebral cortex energy metabolism), neurophysiologic monitoring, and drug control.
In particular, near-infrared spectroscopy (NIRS) monitoring of brain oxygenation (NIRS oxygenation monitoring) is frequently employed in cardiovascular surgeries because it can noninvasively provide continuous data on the balance between oxygen supply and demand in brain tissues. Early detection and timely management of cerebral hypoperfusion could help reduce the risk of preventable cerebral injury. Correct knowledge and proper implementation of NIRS oxygenation monitoring are indispensable for the prevention of perioperative neurological damage in patients undergoing cardiovascular surgery.
The Cerebrospinal Division of the Academic Committee of the Japanese Society of Cardiovascular Anesthesiologists (JSCVA) undertook a literature search and review to identify the mechanisms and incidence of perioperative cerebral injuries in patients undergoing cardiovascular surgery. The Cerebrospinal Division also discussed the proper use of NIRS oxygenation monitoring systems. Summarizing and consolidating the latest evidence-based information, the Cerebrospinal Division published these Use Guidelines to help minimize the risk of perioperative cerebral injury in cardiovascular surgery. In this guideline, each section is comprised with several summary statements and is followed by commentary section. This guide line was translated from “The guideline of cerebral oximetry of near-infrared spectroscopy in cardiac anesthesia” written in Japanese (URL: http://www.jscva.org/news/detail/id/114).
Perioperative cerebral injury in adult cardiovascular surgery
Incidence of perioperative cerebral injury
Summary statements
-
There are three major categories of perioperative cerebral injuries: stroke, encephalopathy, and postoperative cognitive dysfunction (POCD). The pathologies range from mild, focal neurologic disorders to coma resulting from hypoxic encephalopathy.
-
Perioperative stroke develops in 0.1% of patients undergoing noncardiac, nonneurologic surgery. By contrast, perioperative stroke develops in 0.25–3.0% of patients undergoing carotid surgery, 0.8–3.2% of patients undergoing coronary artery bypass grafting (CABG), and 4.7–11.2% of patients undergoing aortic artery surgery. Thus, perioperative stroke occurs more frequently in cardiovascular surgeries than in noncardiovascular surgeries.
-
In patients undergoing cardiovascular surgery, postoperative delirium occurs at a rate of 25–45%, which is higher than the rate in patients undergoing noncardiovascular surgery. In the same group of patients, POCD is observed at a rate of 30–80% at discharge and 20–40% at 6–12 months after discharge.
Commentary
The manifestations of perioperative cerebral injury are diverse, ranging from mild, focal neurologic deficits to memory loss, hypoxic encephalopathy–induced coma, and apallic syndrome. The major clinical categories of perioperative cerebral injuries are stroke, encephalopathy (including delirium), and POCD.
Perioperative stroke develops at a rate of 0.1% in patients undergoing noncardiovascular surgery, but the rate is much higher in those undergoing cardiovascular surgery (Table 1). The rate of perioperative stroke is 0.25–3.0% in carotid surgery, 0.8–3.2% in CABG, 4.7–11.2% in aortic artery surgery with cardiopulmonary bypass, and 2.0–4.0% in transcatheter aortic valve replacement (TAVR). In addition, the rate of perioperative stroke is 3.9–6.3% in thoracic endovascular aortic repair (TEVAR), where the device-landing zone is close to the aortic arch branch vessels.
Cerebral injury outcomes may be classified as Type I (e.g., stroke and hypoxic encephalopathy) and Type II (e.g., new deterioration in intellectual function, confusion, agitation, disorientation, memory deficit, and seizure without evidence of focal injury). Type I and Type II cerebral injuries were reported at a rate of 3.1% and 3.0%, respectively, and resulted in death in 21% and 10% of cases, respectively [16]. Elderly patients are at higher risk of both Type I and Type II cerebral injuries.
Postoperative delirium is associated with an increased long-term risk of death [17, 18] and POCD [19]. The incidence of postoperative delirium was shown to be high, at 25–45% after cardiovascular surgery [20, 21] (Table 2).
In broad terms, POCD is defined as cortical dysfunction characterized by impairments in speech, memory, attention, concentration, and executive function, and is detected by neuropsychological testing after surgery. In noncardiac surgeries, POCD was reported at a rate of 6.8–19.2% [31, 32] from 7 days to 3 months after the surgery. In patients who underwent cardiovascular surgery, POCD was documented at a rate of 30–80% at discharge and 20–40% at 6–12 months after discharge [33, 34]. Given the absence of an international consensus on the diagnostic criteria for POCD, published POCD incidence rates may depend on the testing protocols, assessment criteria, and other variables employed in specific studies [35, 36].
Socioeconomic impact of perioperative cerebral injury
Summary statements
-
The onset of stroke after cardiovascular surgery increases the risk of perioperative death by six- to eight-fold, and the 10-year mortality risk by threefold.
-
In patients undergoing cardiovascular surgery, postoperative delirium is associated with elevated mortality.
-
Patients with documented POCD have worse general health after discharge and are less productive at work than those without documented POCD.
-
Perioperative cerebral injuries compromise the quality of life and inflict considerable social and economic losses. These adverse effects underline the importance of properly evaluating the burden of perioperative cerebral injuries and providing appropriate medical interventions.
Commentary
The onset of stroke in patients who undergo cardiovascular surgery increases the perioperative mortality rate by six- to eight-fold [37, 38]. In addition, perioperative stroke strongly influences long-term outcomes. In a study of 35,733 consecutive patients who underwent isolated CABG surgery [39], 575 (1.6%) developed perioperative stroke. Survival rates in patients with and without perioperative stroke were 83% and 94.1%, respectively, at 1 year; 58.7% and 83.3%, respectively, at 5 years; and 26.9% and 61.9%, respectively, at 10 years. Thus, perioperative stroke resulted in a threefold increase in the 10-year mortality rate. In addition, the majority of patients with perioperative stroke required rehabilitation services to improve their limitations in activities of daily living [40].
Like postoperative stroke, postoperative delirium is associated with elevated mortality in patients who undergo cardiovascular surgery. In a 10-year follow-up study of 5,034 CABG surgery patients, those who developed perioperative delirium (n = 304, 6%) had an increased hazard of death (adjusted hazard ratio 1.65, 95% confidence interval 1.38–1.97). Postoperative delirium is also associated with an increased risk of developing POCD. One study showed that compared with patients without delirium, a significantly higher proportion of patients with delirium did not return to their preoperative baseline Mini-Mental State Examination score at 6 months [19]. It has been shown that POCD impairs patients’ activities of daily living after discharge, thereby decreasing their quality of life. In a 5-year follow-up study of 261 patients who underwent cardiac surgery with cardiopulmonary bypass, POCD was correlated with worse general health and reduced productivity at work [41]. The development of postoperative cerebral injury results in higher mortality and worse quality of life and entails a considerable social and financial burden. These facts emphasize the importance of adequate perioperative evaluation of and medical care for cerebral injuries.
Mechanisms and prevention of perioperative cerebral injury
Although the human brain accounts for 2% of body weight in average adults, it has high energy demands. It receives 15% of the cardiac output and requires 20% of the oxygen and 25% of the glucose consumed by the entire body. The typical normal rate of cerebral blood flow is 50 mL/100 g brain/min, which means that every minute, 3–4 mL of oxygen and 6 mg of glucose is delivered per 100 g of human brain. The brain has poor oxygen and energy stores. It is, therefore, highly susceptible to ischemia, requiring an adequate blood supply.
Carotid artery surgery
Summary statements
-
Carotid endarterectomy (CEA) is an established surgical procedure for carotid stenosis. This technique involves temporarily cross-clamping the diseased carotid artery, which increases the risk of an ischemic event.
-
The risk of cerebral ischemia during carotid cross-clamping must be evaluated using multiple monitoring tools.
-
As a preventive measure against intraoperative ischemic events, a shunt to maintain cerebral blood flow is often inserted into the carotid artery being operated on.
-
Cerebral hyperperfusion syndrome (CHS) is a serious brain injury that occurs at a rate of 1.9% after CEA. In CHS patients with associated intracranial hemorrhage, the mortality rate was reported to be 26%, and sequelae were noted in 80% of survivors.
Commentary
CEA is an established surgical procedure for the treatment of carotid stenosis. CEA combined with medical therapy reduces the risk of stroke in symptomatic severe and moderate carotid stenosis (defined, respectively, as ≥ 70% and 50–69% narrowing of the luminal diameter) [42,43,44,45,46,47,48,49]. The Japanese stroke guidelines (Japanese Guidelines for the Management of Stroke [50]) recommend CEA in addition to antiplatelet, antidyslipidemic, and other pharmacological therapies. Because CEA requires temporary cross-clamping of the carotid artery under repair, it increases the risk of intraoperative cerebral ischemia.
Cerebral ischemia during CEA
The causes of cerebral infarction during CEA include the following: (1) hypoperfusion resulting from carotid cross-clamping, (2) inadvertent dislodging of arterial wall plaques, and (3) embolization resulting from carotid revascularization. To prevent intraoperative ischemic events, a shunt to maintain cerebral blood flow may be inserted into the carotid artery during surgery. Older age, female sex, hypertension, occlusion of the contralateral carotid artery, and a history of contralateral carotid surgery were associated with a greater need for carotid shunt placement [51]. However, experts are divided on the use of shunt placement because it is associated with an increased risk of cerebral ischemia resulting from embolization or carotid dissection. A recent review reported that the mean perioperative cerebral infarction rate for CEA was 1.4% for routine shunting and 2.0% for routine nonshunting. In addition, the mean perioperative cerebral infarction rates for selective shunting were 1.6% using electroencephalogram (EEG) monitoring, 4.8% using transcranial Doppler (TCD), 1.6% using stump pressure, and 1.8% using somatosensory evoked potential (SEP) [52]. Shunt placement should be determined based on a variety of variables, including the patient risk factors, the policies of the surgical institution, EEG, stump pressure, SEP, TCD, motor evoked potential, NIRS hemoglobin oxygen saturation, and other monitoring data.
CHS
Serious perioperative cerebral injuries in patients undergoing CEA include CHS, which manifests as headache, seizures, and focal neurologic symptoms, among other symptoms. Postoperative hyperperfusion may develop when acute changes in regional cerebral blood flow such as ischemia or reperfusion are combined with dysfunction of cerebrovascular autoregulation, which underlies chronic cerebral ischemia. In a cohort of Japanese patients treated with CEA, the onset of CHS peaked on the sixth postoperative day, with an overall incidence rate of 1.9% [53]. In these patients, intracranial hemorrhage developed at a rate of 0.4%. In CHS patients with associated intracranial hemorrhage, the mortality rate was 26%, and sequelae were noted in 80% of survivors.
Aortic surgery
Summary statements
-
Aortic arch surgery is associated with a high risk of cerebral hypoperfusion during reconstruction of the arch branches.
-
Brain protection techniques include deep hypothermic circulatory arrest (DHCA), antegrade cerebral perfusion (ACP), and retrograde cerebral perfusion (RCP).
-
In ACP the surgeon inserts the inflow cannula into the arch branch of interest for cerebral perfusion. ACP may cause atheromatous plaques to be inadvertently released from the vessel wall during cannula manipulation. In addition, ACP may result in cerebral ischemia if the inflow cannula is malpositioned.
-
Acute aortic dissection is associated with pathophysiologic risk factors for cerebral ischemia, including stenosis and occlusion of the arch branch arteries due to enlargement of the false lumen.
Commentary
Aortic arch surgery typically involves resecting and reconstructing the brachiocephalic, left common carotid, and left subclavian arteries. These arteries supply blood to the brain (the subclavian arteries branch to the vertebral arteries that enter the brain). It is, therefore, critical to prevent cerebral ischemia during reconstruction of these arteries.
The major causes of cerebral ischemia are extensive hypoxic encephalopathy resulting from insufficient oxygen supply during arch branch reconstruction (cerebral hypoperfusion), and embolization resulting from atheromas dislodged from the atherosclerotic vessel wall. Techniques to protect the brain and thereby prevent intraoperative cerebral ischemia include DHCA, ACP, and RCP; the specific method used generally depends on the patient’s background factors and the policies of the surgical institution. The goal of DHCA is to protect the brain tissue by increasing its ischemic tolerance via hypothermia. However, since deep hypothermia (a nasopharyngeal temperature of 14–20 °C) allows for a cerebral ischemic time of 20–30 min [54, 55], DHCA alone is insufficient to ensure satisfactory cerebral protection during long surgeries. Therefore, ACP has emerged as an adjunct technique for brain protection, where an inflow cannula is inserted into the arch branch of interest. However, ACP carries a risk of releasing atheromas from the vessel wall during cannula manipulation. ACP may also cause cerebral ischemia if the cannula is malpositioned [56] (Fig. 1). By contrast, RCP provides brain perfusion via a superior vena cava cannula, i.e., in the reverse direction of normal blood flow. In a retrospective analysis of 1193 patients who underwent DHCA for the treatment of aneurysms involving the ascending aorta and arch, the rate of cerebral infarction was 1.7% with RCP and 30% without RCP in patients whose circulatory arrest time exceeded 40 min [57]. These results showed that RCP extended the cerebral ischemic time. However, retrograde perfusion is not a physiologically normal method of circulation, and it may cause brain edema [58]. It is often recommended that the retrograde superior vena cava perfusion flow rate be set below 400 mL/min and that venous pressure be maintained between 15 and 25 mmHg [59].
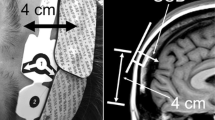
Catheter malposition was detected in 4 (11.4%) of 35 consecutive patients with aortic arch aneurysm undergoing total arch replacement (n = 13) or transaortic stent graft implantation (n = 22) [56]. Catheter malposition can prevent blood flow to the right common carotid artery (arranged form the figure in the article [56])
In a Japanese retrospective analysis of brain protection in 8169 patients with total arch replacement (excluding those with acute aortic dissection and ruptured aneurysms), the rate of postoperative cerebral infarction was comparable between ACP (7.0%) and RCP (8.5%) [60]. A separate analysis conducted in Japan investigated brain protection during ascending aortic repair surgery for Stanford Type A acute aortic dissection [11]. In this study, the rate of postoperative cerebral infarction was 11.2% for ACP and 9.7% for RCP. These rates increased to 18.6% and 18.2%, respectively, when the development of other neurologic complications (transient neurologic dysfunction, continuous coma > 24 h, and paraparesis/paraplegia) were included. These results showed that brain injuries occurred frequently and the rates were comparable between ACP and RCP.
Patients with acute aortic dissection and thoracic aneurysm rupture are at extremely high risk of cerebral ischemia. In a 2013 annual report of thoracic and cardiovascular surgeries in Japan, the hospital mortality rate was 9.1% for Stanford Type A acute aortic dissection and 22.2% for ruptured aneurysms [61]. These high rates may be attributable to the following: (1) stenosis or occlusion of the arch branch by the thrombosed false lumen, and (2) cardiac tamponade, myocardial ischemia, or heavy bleeding causing circulatory failure and subsequent cerebral ischemia [62] (Fig. 2). Notably, patients with acute aortic dissection can present with preoperative neurologic symptoms because of cerebral hypoperfusion. In a small study of 53 patients with new-onset neurologic deficits who received surgical repair for Stanford Type A acute aortic dissection, 45% of patients had persistent neurologic symptoms [63].
Mechanisms of cerebral malperfusion in patients with Stanford Type A acute aortic dissection. Progressive enlargement of the false lumen ultimately occludes the brachiocephalic artery, blocking blood flow into the R-CCA and R-SCA (R-VA). In addition, cardiac tamponade or myocardial ischemia reduces cardiac output, thereby exacerbating right hemisphere ischemia [62]. (arranged form the figure in the article [62]). PCA posterior cerebral artery, MCA middle cerebral artery, CCA common carotid artery, SCA subclavian artery, VA vertebral artery
Cardiac surgery
Summary statements
-
In cardiac surgery with cardiopulmonary bypass, the risk factors for cerebral ischemia include catheter insertion, cross-clamping and unclamping of the aorta, and other mechanical operations that may cause aortic dissection or embolus formation.
-
In patients with cerebral hypoperfusion resulting from hypotension or decreased cardiac output, embolism may cause serious cerebral injury.
Commentary
Cardiac surgery with cardiopulmonary bypass involves insertion of an inflow catheter, cross-clamping and unclamping of the aorta, and other mechanical manipulations that may cause cerebral ischemia. Improper catheter placement may result in aortic dissection. In an international registry-based study, the incidence rate of this iatrogenic complication was 0.23%, although the postoperative mortality rate was as high as 43% in patients with this complication [64]. Cardiopulmonary bypass operations, cross-clamping and unclamping of the aorta, and other mechanical maneuvers may result in the formation of emboli, including air, atherosclerotic plaques, fat, and platelet aggregates, which cause embolism as they enter into the cerebral circulation [65, 66]. Reduced perfusion due to intraoperative hypotension or decreased cardiac output restricts the ability of the bloodstream to clear emboli and microemboli from the watershed area that is susceptible to ischemia [67, 68]. This restriction probably plays a key role in the pathogenesis of cerebral ischemia. During cardiopulmonary bypass, the mean arterial pressure is typically maintained at 50–70 mmHg because physiologic blood flow to the brain is normally 50 mmHg or higher. In a study of 248 patients undergoing CABG with cardiopulmonary bypass, patients were randomized to a low mean arterial pressure of 50–60 mmHg (n = 124) or a high mean arterial pressure of 80–100 mmHg (n = 124) [69]. At 6 months after coronary bypass for the low and high pressure groups, the total mortality rate was 4.0% and 1.6%, respectively, and the stroke rate was 7.2% and 2.4%, respectively. Higher mean arterial pressure resulted in better outcomes. However, higher perfusion pressure during cardiopulmonary bypass was associated with a greater number of emboli [70], and increased the risk of diffuse capillary leakage and edema formation [71]. Older patients and those with hypertension, diabetes mellitus, or other high-risk factors were found to exhibit considerable variation in the lower cerebral blood flow autoregulatory threshold [72], thus preventing definitive determination of the optimal perfusion pressure during cardiopulmonary bypass.
Cerebral injury in pediatric cardiac surgery
Congenital cardiovascular disease and brain dysfunction resulting from genetic abnormalities
Summary statements
-
Pediatric patients undergoing cardiac surgery include children with developmental brain problems resulting from genetic abnormalities (organic mental and functional disorders).
-
Corpus callosum hypoplasia, Dandy–Walker syndrome, aqueductal stenosis, and 22q11.2 deletion syndrome involve organic damage, whereas trisomy 21 and trisomy 18 are associated with functional disorders (mental retardation) that are not necessarily organic in nature.
-
It is not well examined whether cardiac surgery aggravates the developmental disabilities of children with congenital brain defects.
Commentary
A proportion of pediatric patients undergoing cardiac surgery have congenital brain damage (organic or functional) resulting from genetic abnormalities. Corpus callosum hypoplasia, Dandy–Walker syndrome (a congenital brain malformation characterized by the presence of a posterior fossa midline cyst that communicates with the fourth ventricle, and agenesis or hypoplasia of the cerebellar vermis), aqueductal stenosis [73], and 22q11.2 deletion syndrome (characterized by deletion of the 11.2 region of the long arm [q] of chromosome 22, including DiGeorge syndrome) involve organic impairments. These disorders occur in 5–10% of pediatric patients with cardiac diseases [74]. In particular, patients with 22q11.2 deletion syndrome often exhibit a variety of brain malformations (cerebral cortical hypoplasia, cyst-like white matter lesions, underdevelopment of the frontal operculum, and meningomyelocele) and cardiac diseases (tetralogy of Fallot, ventricular septal defect, interrupted aortic arch, and truncus arteriosus). In addition, 40% of trisomy 21 patients with functional brain injury (mental retardation) have a ventricular septal defect, common atrioventricular valve, or other malformations of the heart. Similarly, patients with trisomy 18 often present with a ventricular septal defect, atrial septal defect, patent ductus arteriosus, and other forms of simple left-to-right shunt lesions, as well as aortic stenosis, double-outlet right ventricle, and other complex cardiac disorders. Patients with genetic abnormalities often have developmental disorders irrespective of their cardiac surgery history. When brain function is not evaluated preoperatively, it is difficult to differentiate between congenital and surgically induced brain injury. It is not well examined whether cardiac surgery aggravates the developmental disabilities of children with congenital brain defects.
Brain injury in patients with congenital cardiovascular disease
Summary statements
-
Neonates without genetic abnormalities may have immature brains due to preterm births or brain damage resulting from postpartum hypoxemia, low cardiac output, or hypotension.
-
In patients with congenital heart diseases, hypoplastic left heart syndrome, aortic coarctation, and transposition of the great arteries are common underlying causes of brain injury.
-
No consensus has emerged regarding whether preoperative brain abnormalities are associated with new-onset injuries noted after cardiovascular surgery.
Commentary
Regardless of whether or not they harbor genetic abnormalities, neonates who require surgical treatment for their cardiovascular problems are susceptible to brain injuries under two scenarios. First, many babies with cardiac failure are delivered preterm (usually before 35 weeks of gestation). In such cases, they are born with immature brains. Another scenario is that their cardiovascular diseases result in hypoxemia, low cardiac output, or hypotension, and these conditions increase the risk of brain injuries.
In a study of 67 neonatal patients who underwent cardiac surgery with cardiopulmonary bypass, brain magnetic resonance imaging (MRI) was performed pre- and postoperatively (up to 6 months). The developmental maturity of their brains was evaluated in terms of myelination, cortical infolding, involution of the geminal matrix, and the presence of bands of migrating glial cells. The results of MRI scans were used to classify abnormalities into nine categories: white matter injury, infarction or ischemic stroke, intraparenchymal hemorrhage or hemorrhagic stroke, punctate lesions, elevated lactate, subdural hemorrhage, dural sinovenous thrombosis, intraventricular hemorrhage, and congenital malformations. Postoperative brain abnormalities, particularly white matter injury, were strongly associated with preoperative brain immaturity. Twenty-four (36%) of the 67 patients had new postoperative white matter injury, infarction, or hemorrhage, indicating poor neurologic outcomes [75]. Preterm infants commonly have a thick subependymal germinal layer that surrounds the lateral ventricles. The germinal matrix is susceptible to bleeding (subependymal hemorrhage) caused by changes in hemodynamics. The blood in the subependymal layer often extends into the lateral ventricles and causes an intraventricular hemorrhage [76].
Among 50 neonates who had major congenital heart disease in the absence of other congenital or chromosomal aberrations (gestational age > 35 weeks), 42% showed cerebral abnormalities on preoperative cranial ultrasound [77]. Brain injury is commonly seen (frequency 30%) in patients with hypoplastic left heart syndrome. In addition, brain injury is often noted in cases of aortic coarctation. In such cases, postpartum brain injury may occur because of cerebral hypoxia or hypoperfusion resulting from (1) decreased cardiac function, (2) increased central venous pressure due to intracardiac shunting, or (3) cyanosis. In the absence of antenatal evidence of congenital heart defects, which would indicate a high likelihood of postnatal hypoxia or hypoperfusion, brain injury may worsen after delivery because of delayed delivery of oxygen and other supportive measures. Apgar scores measured at birth can provide useful prognostic data on neurologic outcomes [78].
In healthy neonates, the watershed area that is susceptible to hypoperfusion is the parasagittal cerebral cortex, whereas in preterm babies it is the periventricular white matter. In a study of 24 neonates with congenital heart disease (including eight with hypoplastic left heart syndrome), preoperative MRI examinations showed periventricular leukomalacia in four patients (16%) and infarct in two (8%). Early postoperative MRI (n = 21) identified periventricular leukomalacia in 48%, new infarct in 19%, and new parenchymal hemorrhage in 33%. Altogether, new lesions or worsening of preoperative lesions occurred in 67% of subjects [79]. In another study of 62 neonates with congenital heart disease, white matter injury was noted preoperatively in 11 subjects (18%), with the rate rising to 26% postoperatively [80]. In addition, infarcts were observed in the middle cerebral artery territory. In a study of 22 subjects who underwent the Norwood procedure for the treatment of hypoplastic left heart syndrome [81], five (23%) showed abnormal MRI findings preoperatively (multifocal periventricular leukomalacia, focal infarctions in the right frontal lobe, and hemorrhage). Postoperatively, 73% of the subjects showed new MRI abnormalities (periventricular leukomalacia, focal ischemia, and hemorrhagic infarction). Subjects with transposition of the great arteries also reported a high incidence of postoperative brain injury, including cortical lamilar necrosis, periventricular and other white matter injury, and injuries to the cerebellum and basal nuclei. Preoperative brain injury was significantly associated with balloon atrial septostomy [81], a procedure that aims to enhance atrial mixing and improve pulmonary blood flow by enlarging the interatrial communication. This procedure is most often performed on patients with serious preexisting cerebral hypoxia.
While some data indicate a significant correlation between preoperative brain injuries and new postoperative abnormalities [82], other results are inconclusive [83].
Brain injury and its risk factors in pediatric patients undergoing cardiovascular surgery
Summary statements
-
Brain injury occurs at a rate of 2–25% in pediatric patients receiving cardiac surgery.
-
A DHCA time longer than 40 min places pediatric patients at increased risk of brain injury.
-
The adjunctive use of regional low-flow cerebral perfusion or pH-stat helps reduce the risk of brain injury.
-
Hypotension, low cardiac output, and hypoxia during the postoperative period are important risk factors for cerebral injury.
Commentary
Symptomatic brain injuries develop at a rate of 2–25% in infants who undergo cardiac surgery [73]. To achieve a bloodless operative field, DHCA is frequently adopted in surgery for infants with complex cardiac anomalies. However, a DHCA time extending beyond 40 min increases the risk of periventricular leukomalacia and stroke. To lower this risk, regional low-flow cerebral perfusion has been devised, in which unilateral perfusion is delivered via the brachiocephalic artery. This technique is associated with a lower incidence of neurologic complications than DHCA [82]. The pH-stat method is commonly employed in pediatric cardiopulmonary bypass surgery. This technique reduces the incidence of brain injury through cerebral vasodilation and resulting homogenous cooling [83]. During cardiopulmonary bypass, a larger amount of circulatory blood is exposed to the synthetic surface of the bypass circuit in infants than adults. This may give rise to an inflammatory response and reactive oxygen species, placing the neonatal brain at a greater risk of injury.
Pre- and postoperative circulatory insufficiency (hypotension and low cardiac output) and hypoxemia are known causes of white matter injury in pediatric patients [80].
The basics of NIRS oxygenation monitoring
Principles of measurement
Summary statements
-
The NIRS oxygenation monitoring system utilizes the high tissue permeability of near-infrared light.
-
Near-infrared light that enters body tissues is absorbed by oxygenated and deoxygenated hemoglobin molecules, which have different absorption spectra for near-infrared light. The spectral difference is used to determine the tissue oxygen saturation.
-
The modified Beer–Lambert (MBL) law, spatially resolved spectroscopy (SRS), and time-resolved spectroscopy (TRS) are key NIRS concepts used to measure the degree of oxygenation.
Commentary
The absorption spectra of hemoglobin and available measurement systems
The NIRS oxygenation monitoring system is based on the high tissue permeability of near-infrared light. This light has a wavelength ranging from 700 to 1000 nm, and its biopermeability is greater than that of visible light (wavelength approximately 350–700 nm). Oxygenated and deoxygenated hemoglobin molecules absorb near-infrared light that enters body tissues. Because these molecules have different absorption spectra for near-infrared light, the spectral difference can be used to determine the degree of tissue oxygen saturation.
Unlike pulse oximetry, which focuses on the pulsatile arterial component, the NIRS oxygenation monitoring system detects both arterial and venous blood hemoglobin oxygenation.
Table 3 lists the latest major NIRS oxygenation monitoring systems that are available on the market.
Theory and methods of measurement
Beer–Lambert law
The NIRS measurement of cerebral tissue oxygen saturation is based on the Beer–Lambert law. In the simplest case, the relationship between the optical density at the wavelength of λ [OD (λ)] on the one hand, and the incident intensity [I0] and the light intensity after it passes through the sample [I] on the other, are calculated by the following equation:
where ε (λ) is the molar extinction coefficient, c is the analyte concentration, and d is the path length.
This equation shows that the hemoglobin concentration c can be determined if the value of the variable d is known. Because biological tissue samples scatter light, the MBL equation is applied, as follows:
where B is the differential path length factor and OD (λ)R represents the amount of light lost by scattering. In most cases, the value of d × B is defined as being equal to the mean path length.
Emitter–detector distance, elimination of interference by scalp blood flow, and path length
The distance between the emitter and detector of the NIRS oxygenation monitor is typically set in the range of 30–50 mm. The emitter–detector distance should preferably be set at 40 mm in adults based on the results of experiments using isocyanine green (ICG) dye (peak absorption at 803 nm). After injecting the ICG dye into the internal or external carotid artery, the difference in the emitter–detector distance on NIRS measurement is evaluated. When the dye is injected into the external carotid artery, NIRS measurements show no meaningful difference for an emitter–detector distance range of 10–40 mm. This indicates that NIRS measurements are independent of the tested emitter–detector distance range with regard to the blood flow of the external carotid artery. On the other hand, when the dye is injected into the internal carotid artery, NIRS measurements increase with increasing emitter–detector distances and reach a plateau at a distance of 40 mm. This means that cerebral blood flow has a significant impact on NIRS measurements up to emitter–detector distances of 40 mm [84].
As the near-infrared light produced by the NIRS oxygenation monitor passes through the scalp and other superficial tissues, its effect on the blood flow in these tissues is detected by the NIRS system. To eliminate the confounding effect of superficial blood flow, a variety of strategies have been devised. The INVOS™ 5100C system (Covidien) and O3™ Regional Oximetry system (Masimo) are equipped with two detectors, placed at 30 mm and 40 mm from the emitter, respectively. Regional cerebral oxygen saturation (rSO2) is determined by subtracting the data obtained by the detector at 30 mm from the data obtained at 40 mm. In the TOS-OR system (Fujita Medical Instruments), light that is detected earlier is filtered out and only that which arrives later is used. The SenSmart™ X-100 device (Terumo) has two emitter–detector pairs to cancel out the influence of the superficial blood flow.
When the emitter–detector distance is set at 40 mm, this does not necessarily mean that the path length is also 40 mm. For example, when the near-infrared light that enters the brain is detected after 1.1 nanosecond by the detector located 40 mm from the emitter, the path length is calculated to be 24 cm [85].
NIRS oxygenation monitoring using the MBL algorithm
Most commercially available NIRS oxygenation monitoring systems employ MBL algorithms for rSO2 measurements. The NIRO®-200NX system (Hamamatsu Photonics) features a proprietary MBL algorithm to determine oxygenated, deoxygenated, and total hemoglobin concentrations from measurements of three near-infrared lights of different wavelengths. The FORE-SIGHT ELITE™ system (CAS Medical System) is equipped with a sophisticated MBL algorithm and utilizes five different wavelengths of near-infrared light to cancel out the impact of path length differences. The FORE-SIGHT ELITE™ system provides rSO2 measurements with a very high level of accuracy and precision (see Table 3).
SRS
While the photons from the incident light travel through the sample, they are scattered, reflected, and attenuated until they exit the sample at different locations (Fig. 3). In SRS, the reflected photons are measured at different distances from the light source. Measurements of the beam attenuation at multiple locations can provide estimates of oxygenated and deoxygenated hemoglobin concentrations without taking path lengths into consideration, as shown in the following formula [86]:
A schematic illustrating the principles of spatial resolved spectroscopy (SRS) measurement (arranged from the figure in [86])
The NIRO®-200NX instrument uses the SRS approach and provides the tissue oxygenation index (TOI) in addition to MBL.
Additional measurement approach
Another measurement method used in NIRS is TRS. Short pulsed beams (duration on the order of 10− 10 s, or 100 ps) are emitted from the light source, and the measured time difference between emission and detection can help determine the precise path length of the beam because the velocity of light is constant. The TRS-20 [85] and tNIRS-1 instruments (Hamamatsu Photonics) employ this approach. Because TRS yields a precise path length estimate, the resulting tissue oxygen saturation measurements are close to the actual values.
Tips for successful measurements
Summary statements
-
Disposable probes (or sensors, integrated with a near-infrared light source and photodetector) should not be used more than once.
-
Entrance of ambient light into the emitter–tissue–detector pathway should be prevented to increase measurement accuracy.
-
Probes should not be fixed firmly to the body by means of tape, a headband, or bandage.
-
NIRS oxygenation monitoring should be started before oxygen delivery in anesthesia, and the data obtained should be treated as the baseline reference value.
-
NIRS oxygenation monitoring may be stopped at the end of surgery. However, 60% of cerebral injuries occur postoperatively in adult patients undergoing cardiac surgery. In addition, a possible association between the postoperative oxygen saturation level and the development of new brain injuries and surgical complications has been indicated in pediatric cardiac surgery. Thus, postoperative NIRS oxygenation monitoring should be considered.
Commentary
Most marketed NIRS oxygenation monitoring systems employ disposable probes, with the exception of the TOS-OR system. Disposable probes should be used only once. Long-term or frequent use of disposable probes leads to inaccurate measurements due to insufficient probe adhesion or light emitting diode (LED) deterioration. In addition, because NIRS measurements are influenced by fluorescent lamp light or other ambient lights, the operator should take appropriate measures to protect the probes from ambient lights after they have been placed for measurement.
NIRS oxygenation monitoring is essentially noninvasive and harmless, although it may occasionally cause temporary reddening at the site of the application. It is, therefore, recommended not to fix the sensors firmly to the body by means of tape, a headband, or bandage. In addition, sensors should not be placed on unhealed or edematous skin lesions.
NIRS oxygenation monitoring should be started before the initiation of oxygen delivery in anesthesia, and the data obtained before oxygen administration should be handled as the baseline reference level. NIRS oxygenation monitoring may be stopped at the end of the surgery. However, 60% of adult patients undergoing cardiac surgery experience cerebral injuries postoperatively [6]. In addition, a possible association between postoperative rSO2 on the one hand and newly acquired brain injuries and surgical complications on the other has been indicated in pediatric cardiac surgery [81, 87]. These findings suggest that postoperative NIRS oxygenation monitoring will increase the possibility of detecting and preventing cerebral injury. No probe-induced injury has been reported with 3-week continuous use of the TOS-OR system. However, new-onset skin lesions were reported with 26-h use of another oximetry instrument [88]. The surgeon should carefully monitor the patient for possible adverse changes during extended use of NIRS oxygenation monitoring devices.
Generally, NIRS oxygenation monitoring probes should be placed on the subject’s forehead. Probes should not be attached over nevi, the paranasal cavities, the superior sagittal sinus, any epidural hematoma, or malformed vessels, because the resulting measurements may be suboptimal.
Up to four emitter–detector probes can be used with the INVOS™ 5100C and NIRO®-200NX systems, as well as with the FORE-SIGHT ELITE™ system (optional device is required). The application of a second probe to the occipital region may possibly expand the region of oxygen saturation measurement. However, attention should be paid when interpreting the results obtained from a second probe on occipital region, because the measurements are influenced by scalp hair and the difference in thickness between the frontal and occipital bones. In addition, the probe location in the forehead influences rSO2 measurements. The mean (± standard deviation) rSO2 values obtained from two probes located with their medial aspects at the midline of the forehead (left 61% [± 11%], right 61% [± 10%]) were greater than the mean values obtained from two probes with their medial aspects placed 1 cm lateral to the midline (left 59% [± 10%], right 58% [± 11%]). When the probe was located over the forehead midline, the mean (± standard deviation) value was 64% (± 12%) [89]. In addition, the mean rSO2 value was significantly lower at the upper than lower forehead during cardiac surgery (60% versus 66%, respectively) [90]. The location of the probe influences measurements because of differences in the cranial and subcranial structures and the hemodynamics underneath.
Practical considerations in data interpretation
Summary statements
-
Because different NIRS oxygenation monitoring devices employ different algorithms, measurement results may vary from one device to another, and factors influencing the measurements must be weighed differently.
-
The results of NIRS oxygenation monitoring are strongly influenced by anemia, cranial bone thickness, the cerebrospinal fluid layer, extracranial blood flow, and the subject’s body position.
Commentary
Several points should be considered when interpreting NIRS oxygenation monitoring data. Because this technique provides local cerebral oxygen saturation data, many healthcare professionals tend to assume that its measurement accuracy is as high as that of pulse oximetry, which provides data on arterial oxygen saturation. However, it should be noted that the two systems are completely different in measurement accuracy and precision. Pulse oximetry data are highly reliable, and a value below 90% suggests an imminent risk of hypoxemia. On the other hand, NIRS oxygenation monitoring data are of moderate reliability, and a decrease of 20–30% from the reference level suggests a possible risk of ischemia.
A key point to consider in this context is that measurements in NIRS oxygen monitoring may deviate considerably from the true value because of differences in measurement methodology and conditions, as well as individual anatomical characteristics. Some of the major factors will be discussed in detail below. Healthcare professionals should have a good understanding of the factors that influence NIRS oxygenation measurements so that they interpret the data correctly.
Differences in measurement algorithms
At present, several NIRS systems measure rSO2 values, but they use different MBL algorithms. In addition, the number of wavelengths used for measurements varies from two to five depending on the model. These differences indicate that oxygen saturation measurement results may vary from one device to another.
Mean path length
The MBL algorithm for rSO2 measurement involves the determination of the mean path length (Fig. 4). As shown in the above equation for the determination of the oxy and deoxy hemoglobin concentration (“Beer–Lambert Law”), the mean path length, which refers to the distance the photon travels from the emitter to the detector, influences the rSO2 estimation. Although the mean path length varies depending on the actual measurement conditions, it is included as a constant in the equation. A change in the mean path length may result in rSO2 over- or underestimation. For this reason, it is important to know whether the mean path length is included in the calculation algorithm of the NIRS oxygenation monitoring device in use. Major factors that can affect the mean path length include the following:
A schematic illustrating the near-infrared light path length from the emitter to the detector (arragened from the figure in [99])
Anemia
Anemia is characterized by low hemoglobin levels, and the NIRS beams emitted to measure rSO2 are specifically absorbed by hemoglobin molecules. Therefore, a reduction in the hemoglobin level results in elongation of the mean path length because it causes less photon energy loss, thereby allowing photons to travel a longer distance. In a study of nine patients undergoing cardiac surgery, the mean path length was elongated 1.3-fold due to decreased hemoglobin concentrations [91]. On the other hand, in the formula of modified Beer Lambert law, optical path length is constant value, but changed during CPB. Therefore, the change of rSO2 values are overestimated 1.3 times as much as the real change of rSO2.
Cranial Bone Thickness and Cerebrospinal Fluid Layer
Cranial bone thickness varies between individuals. In NIRS the path length of the photon tends to be longer with a greater bone thickness. The volume of the cerebrospinal fluid layer is determined by the size of the space between the brain parenchyma and the cranial bone, as shown on the head CT scan in Fig. 5. A larger cerebrospinal fluid volume is associated with a smaller number of photons reaching the brain parenchyma and, therefore, an underestimation of rSO2 [92].
Impact of skull thickness and the cerebrospinal fluid layer on NIRS oxygenation monitoring measurements (arranged from the figure in [91])
It is important to understand that rSO2 measurements of MBL-based NIRS oxygenation monitoring devices depend on the factors that influence the mean path length.
Extracranial blood flow
NIRS sensors are typically attached to the forehead for rSO2 measurement, and rSO2 values are impacted by the scalp blood flow beneath the sensor. In a study using three NIRS oxygenation monitoring devices (FORE-SIGH, INVOS 5100C-PB, and EQUANOX Classic 7600), Davie and Grocott reported that scalp tissue hypoxia and ischemia resulted in decreases in rSO2 values of 6–15% from baseline [93]. Further, rSO2 values are decreased during infusion of phenylephrine or other vasoconstrictors, but not during infusion of ephedrine or other β1 receptor agonists. Given that cerebral blood flow remains almost unaffected following administration of a vasoconstrictor, phenylephrine-induced decreases in rSO2 reflect extracranial vasoconstriction [94].
Subject’s body position
In a NIRS study of healthy volunteers, rSO2 values measured on the forehead were lower when the subject was in the upright position than in the supine (Tredelenburg) position [95]. In a study of patients who underwent shoulder surgery, those in the beach chair position had a lower rSO2 value than those in the supine position [96]. Several studies on gynecological laparoscopic surgery and robot-assisted prostatectomy reported contradictory findings on the impact of the steep Trendelenburg position on rSO2 values, with some reporting an increase and others reporting a decrease [97,98,99,100]. Despite the reports of decreased rSO2 associated with the patient’s surgical position, it is unknown whether such decreases are a direct cause of postoperative brain injury. In the cardiovascular field, the Trendelenburg position is commonly used during off-pump CABG surgery. However, the impact of this position on rSO2 measurement during CABG surgery has not been fully investigated.
The sections in this chapter have discussed the major factors that influence NIRS-based rSO2 measurements. Individual NIRS oxygenation monitoring devices use proprietary calculation algorithms with different evaluation schemes. The surgeon and anesthesiologist should be aware of the advantages and disadvantages of the NIRS oxygenation monitoring devices they use.
Use of and interventions based on NIRS oxygenation monitoring in adult cardiovascular surgery
CEA
Use of NIRS oxygenation monitoring
Summary statements
-
The utility of NIRS oxygenation monitoring in CEA has been established.
-
The majority of studies of NIRS oxygenation monitoring in CEA relate to the evaluation of hypoperfusion. This technique is also useful for the clinical assessment of the risk of CHS.
-
To determine the alarm threshold for hypoperfusion during CEA, the relation between intraoperative NIRS values and the onset of neurologic complications has been assessed in patients with local anesthesia. In patients undergoing general anesthesia, SEP, EEG, or TCD criteria for intervention are defined before the study, and their association with intraoperative NIRS values is evaluated.
-
The onset of CHS is evaluated based on the emergence of postoperative symptoms and changes in TCD and SPECT blood flow. Intraoperative NIRS oxygen saturation values are retrospectively analyzed for correlation with TCD or SPECT data in patients who develop CHS.
Commentary
NIRS oxygenation monitoring is performed in CEA patients to detect the risk of cerebral hypoperfusion during carotid cross-clamping or the risk of postoperative CHS [101]. While most studies of NIRS oxygenation monitoring in CEA relate to the intraoperative evaluation of hypoperfusion risk, it is also useful for monitoring the CHS risk. The alarm threshold in patients with local anesthesia may be appropriately determined based on the NIRS oxygen saturation values obtained when neurologic symptoms develop during surgery. The alarm threshold in patients with general anesthesia is frequently determined by comparing the lowest NIRS values during carotid cross-clamping in patients with and without neurologic complications postoperatively. In addition, these patient groups are compared in terms of the relation between NIRS data on the one hand and intraoperative SEP and EEG changes, TCD abnormalities, and stump pressure decreases on the other. The diagnosis of CHS is based on the appearance of postoperative symptoms and changes in TCD and SPECT blood flow, and intraoperative NIRS values are retrospectively analyzed regarding potential associations with TCD and SPECT data at the onset of CHS.
Alarm threshold and clinical interventions
Summary statements
-
In CEA, a 20% or greater relative drop in rSO2 from baseline or a decrease to ≤ 50% of the value measured during carotid cross-clamping indicates that shunt insertion or other appropriate measures should be considered.
-
In patients undergoing CEA, an association has been reported between CHS development and at least a 5–10% absolute postoperative increase from baseline rSO2 values.
-
Early detection of the CHS risk based on NIRS oxygenation monitoring will facilitate appropriate postoperative blood pressure management and other interventions to prevent CHS.
Commentary
Table 4 summarizes the major publications that evaluated the association between NIRS oxygen saturation data and the onset of intraoperative hypoperfusion or postoperative CHS in patients with CEA [102,103,104,105,106,107,108,109,110,111,112].
The lowest intraoperative NIRS values from the side being operated on can be a reliable predictor of imminent hypoperfusion risk. For this purpose, the association between NIRS data and decreases in TCD middle artery flow, changes in EEG or SEP, or the onset of postoperative neurologic complications is evaluated in patients undergoing local anesthesia. In Table 4, data on rSO2 values were obtained using the INVOS™ system in all studies except two (OM-220, Shimadzu Corp., Kyoto, Japan and NIRO® 500, Hamamatsu Photonics K.K., Shizuoka, Japan) [106, 109]. In one study, a decrease in oxygenated hemoglobin concentration was also reported as an indicator for hypoperfusion risk [106].
Moritz et al. showed that a 20% relative rSO2 decrease from baseline maximized both the sensitivity (83%) and specificity (83%) for the risk of hypoperfusion under local anesthesia [110]. The absolute rSO2 value that maximized both sensitivity and specificity was 59%. Samra et al. also reported that a 20% reduction in rSO2 from baseline was an excellent cutoff threshold for the risk of subsequent complications [107]. In studies that evaluated the association between rSO2 values and the onset of postoperative neurologic complications, absolute values of 54–56% [103], an 11.7–18% absolute decrease from baseline [103, 108], and a 20% relative decrease from baseline [108] have been documented as warning thresholds. In studies that assessed the relationship between rSO2 and other monitoring data, decreased SEP amplitude, loss of SEP signals, EEG asymmetry, decreased TCD middle artery flow (a 50–80% relative decrease from baseline), and decreased stump pressure (< 40 mmHg) were considered to indicate a risk of hypoperfusion. Specifically, rSO2 values of 50–56% [105, 106], a 5–25% absolute decrease from baseline [109, 111], and a 10–15% relative decrease from baseline [105, 106] have been reported as warning thresholds. In light of the above studies, an absolute rSO2 value of 50% and a 20% relative decrease from baseline are plausible warning thresholds for the risk of hypoperfusion in CEA surgeries.
Shunt placement is probably the most effective intervention to prevent hypoperfusion, although the benefit of increased oxygen ventilation and the administration of ephedrine to elevate blood pressure has also been documented in the literature. Figure 6 shows a flow chart that the JSCVA proposes for hemodynamic management in CEA surgery, with a minor modification of the algorithm developed by Zogogiannis and colleagues [113]. In essence, the surgeon should immediately consider inserting a shunt if patients with a mean arterial pressure of 60 mmHg or above experience a 20% relative decrease of rSO2 from baseline or an absolute rSO2 value equal to or below 50%. When the mean arterial pressure is below 50 mmHg, the surgeon should increase it to above 60 mmHg, and if the aforementioned rSO2 criteria are still applicable 3 min after the blood pressure elevation, shunt insertion should be considered.
Potentially critical events and interventions during CEA surgery (arranged from the figure in [130]). BP blood pressure, MAP mean arterial pressure, CVP central venous pressure, SaO2 arterial oxygen saturation, PaCO2 arterial partial pressure of carbon dioxide, Hb hemoglobin, CMRO2 cerebral metabolic rate of oxygen
NIRS oxygenation monitoring is useful for the early detection of CHS risk. In a report by the Japanese Society for Treatments at Neck in Cerebrovascular Disease, CHS occurred in 30 of 1596 patients treated with CEA (1.9%), with a peak on postoperative days 3–6 [53]. The diagnosis of CHS is based on postoperative symptoms, increased TCD flow velocity (a twofold increase is a common criterion), and SPECT findings. In most studies, the relationship between intraoperative NIRS data after unclamping and the onset of CHS has been retrospectively evaluated. No studies to date have assessed the NIRS data obtained at the time of CHS onset, because patients who undergo CEA are generally weaned off of NIRS oxygenation monitoring by postoperative days 3–6, when CHS is most likely to develop. It is neither practical nor beneficial to continue NIRS oxygenation monitoring for several days after surgery. However, the surgeon may consider maintaining NIRS oxygenation monitoring until the patient leaves the intensive care unit.
An absolute increase of 5–10% in the rSO2 value after unclamping was associated with an elevated risk of postoperative CHS in patients who underwent CEA under local anesthesia [111]. In a study of 151 patients who underwent CEA under general anesthesia, CHS developed in 7 patients (4.6%) [112]. Whereas the non-CHS patient group showed little change in rSO2, the CHS patient group exhibited a mean 7% absolute increase from baseline 1 h after the surgery.
These findings suggest the need for stringent pharmacological blood pressure control to prevent cerebral hemorrhage, a potentially fatal complication of CHS, in patients with an absolute rise of 5–10% on postoperative rSO2 readings. The primary goal in managing CEA patients is to maintain blood pressure within the normal range. If the patient becomes symptomatic, the surgeon should intensify the hypotensive therapy and contemplate the use of propofol or other sedatives to suppress the cerebral metabolism. A group of surgeons demonstrated that the administration of edaravone immediately before unclamping attenuated cerebral hyperperfusion in patients undergoing CEA [114]. Data from NIRS oxygenation monitoring may help identify patients at high risk of CHS and those who are candidates for pharmacotherapy.
Aortic surgery
Use of NIRS oxygenation monitoring
Summary statements
-
Aortic surgery is associated with a higher incidence of serious cerebral infarction than most other surgical procedures.
-
NIRS oxygenation monitoring can be a useful tool for detecting cerebral perfusion abnormalities in patients undergoing aortic surgery.
-
NIRS oxygenation monitoring is effective for detecting unilateral perfusion abnormalities during aortic surgery.
Commentary
Compared with most other surgeries, aortic surgery has a higher incidence of postoperative stroke (4.7–11.2%), and the cases are frequently serious [10]. When the procedure involves aortic arch manipulation or an open distal anastomosis of the graft, deep hypothermia and circulatory arrest are necessary while maintaining cerebral blood flow via RCP or ACP. Since cerebral protection plays a critical role in aortic surgery, the application of NIRS oxygenation monitoring is, therefore, beneficial. Studies using NIRS oxygenation monitoring in aortic surgery patients demonstrated an association between a sustained decrease in rSO2 and the occurrence of neurologic events [115,116,117]. In addition, NIRS oxygenation monitoring was used to successfully identify malperfusion and take remedial actions during aortic surgery. In a study of 35 consecutive patients with aortic aneurysm, the authors reported several cases in which the ACP brachiocephalic catheter was inadvertently advanced into the right subclavian artery intraoperatively, reducing the blood supply to the right internal carotid artery. In these cases, the changes in rSO2 measurement contributed to discovering the malpositioning [56]. Another study reported a patient with acute Stanford Type A aortic dissection who underwent total arch replacement with cardiopulmonary bypass [118]. In this case, the dissection extending into the right carotid artery caused narrowing of its true lumen, and the difference in rSO2 between the right and left sides of the forehead contributed to restoring the perfusion of the right hemisphere.
Alarm threshold and clinical interventions
Summary statements
-
The subsequent occurrence of neurologic events is closely associated with a relative rSO2 decrease to 64–80% of baseline or the duration for which rSO2 drops to below 60% or 55%.
-
The new onset of side-to-side asymmetry in rSO2 during aortic surgery indicates a high probability of unilateral perfusion abnormalities, and the surgeon should perform appropriate interventions immediately.
-
NIRS oxygenation monitoring helps the surgeon make an informed decision about switching from unilateral to bilateral ACP during aortic arch surgery.
Commentary
Table 5 summarizes the major studies that investigated the association between rSO2 and the onset of stroke in aortic surgery [115,116,117]. In a study by Orihashi et al. [115], 59 consecutive patients underwent aortic surgery with ACP under moderately hypothermic circulatory arrest (25 °C). Measurements of rSO2 were conducted using the TOS-96 oximeter (Tostec Co., Tokyo, Japan). Type I or II neurologic deficits were observed in 16 patients (27.1%), and Type I neurologic deficits (i.e., new onset of cerebral infarction) were observed in six. The duration for which rSO2 values remained below 60% or 55% was significantly longer for the 16 patients with neurologic events than for the 43 patients without neurologic events. The six patients with newly acquired cerebral infarction were characterized by diffuse hypoperfusion in the carotid or basilar artery region and an extended period in which rSO2 was below 60%. In a study of 46 consecutive patients who underwent aortic surgery with ACP [116], six (13%) developed Type I neurologic deficits, and their rSO2 values decreased to 65–80% of baseline (no meaningful change in rSO2 was observed in patients without Type I deficits). It is noteworthy that the difference between the left and right hemispheric rSO2 measurements provided insight into the detection of cerebral injury in this study. In the study using the FORE-SIGHT ELITE™ system, Fischer et al. showed that the area under the curve (AUC) below the 60% or 65% threshold was significantly associated with postoperative organ dysfunction, and the authors proposed that these values could represent the lowest target rSO2 threshold that can be used in thoracic aortic surgery [117].
The studies cited above indicate that NIRS oxygenation monitoring is effective for detecting the risk of cerebral injury in patients undergoing aortic surgery. Changes in NIRS oxygenation data, such as a decrease to 65–80% of baseline and the onset of a difference between the left and right hemispheric values, should prompt the surgeon to examine the cause for the change and take appropriate remedial actions where necessary. The surgeon should review the adequacy of the catheter position, perfusion rate, patient body temperature, and other clinical parameters (Table 6).
There have been case reports of aortic surgery patients in whom left-to-right differences in rSO2 readings provided key insights into the successful detection and correction of unilateral perfusion abnormalities. One of these cases involved the accidental intraoperative advancement of the ACP brachiocephalic catheter into the right subclavian artery, which reduced the blood supply to the right internal carotid artery [56]. In addition, a patient with acute Stanford Type A aortic dissection suffered from right-sided hemispheric hypoperfusion because the dissection extending into the right carotid artery caused narrowing of its true lumen [118]. In these cases, catheter repositioning or other appropriate and timely actions helped prevent brain injury.
Moreover, Harrer et al. showed that NIRS oxygenation data guided the surgeon in switching from unilateral ACP to bilateral ACP in aortic arch surgery [119]. In their study, unilateral ACP via the right axillary artery was established at the start of the surgery, which continued as long as there was no significant left-to-right imbalance in NIRS oxygen saturation data. When the NIRS oxygenation measurements over the right frontal cortex showed a significant drop (rSO2 < 55% or a relative drop in TOI of 15–20% below baseline), an additional cannula was placed in the left carotid artery for bilateral ACP. Most patients in the Harrer et al. study (92%) required switching from unilateral to bilateral ACP.
Cardiac surgery
Use of NIRS oxygenation monitoring
Summary statements
-
The use of NIRS oxygenation monitoring during cardiac surgery with cardiopulmonary bypass can contribute to a decreased incidence of Type I and Type II neurologic deficits.
-
A decrease in NIRS oxygenation measurements during cardiac surgery with cardiopulmonary bypass can indicate a risk of POCD or delirium.
Commentary
The risk of Type I and Type II neurologic deficits can be minimized by NIRS oxygenation monitoring in cardiac surgery [120, 121]. A decrease in NIRS oxygen saturation data during cardiac surgery can be a predictor of subsequent POCD or delirium [122,123,124,125,126,127,128,129,130,131]. Proactive intraoperative management to prevent cerebral oxygen desaturation reduces the incidence of complications involving the brain and other major organs [130] and postoperative neurocognitive decline [131].
Alarm threshold and clinical interventions
Summary statements
-
Patient management based on an alarm threshold of a 20% relative decrease from baseline in NIRS oxygenation reading can reduce the risk of Type II neurologic injuries in cardiac surgery.
-
In patients undergoing cardiac surgery, a relative decrease of 20–30% in rSO2 from baseline or an absolute drop to below 35–65% can be an alarm threshold that triggers actions to prevent POCD and postoperative delirium. The AUC below the saturation threshold is also a reliable indicator of the postoperative injury risk.
-
Several patient management algorithms that incorporate specific trigger thresholds have been proposed, such as a 20–30% relative decrease in rSO2 from baseline or a drop to below 50%.
-
When abnormal rSO2 data are obtained, the catheter placement, head position, arterial oxygen saturation, mean arterial pressure, central venous pressure, cardiac index, mixed venous oxygen saturation, hemoglobin concentration, and other variables should be reexamined to reduce the risk of major organ dysfunction.
Commentary
Physicians have reported that NIRS oxygenation monitoring contributes to a decrease in the occurrence of Type I and Type II neurologic injuries in cardiac surgery. In a retrospective study that compared the benefit of cerebral oximetry in CABG and valve replacement surgeries between 1,034 patients with and 1,245 patients without rSO2 monitoring, Goldman et al. showed that Type I neurologic injuries occurred at a rate of 0.97% (n = 10) with oximetry and at a rate of 2.01% (n = 25) without oximetry [120]. In a retrospective review, Edmonds compared the outcomes in 332 cases of CABG surgery with a battery of cerebral oximetry, EEG, and TCD monitoring, and the outcomes in 286 cases of CABG surgery before the incorporation of cerebral oximetry [121]. Abnormal changes in rSO2 were defined as a 20% or greater relative decrease from baseline, and were corrected to the greatest extent possible by raising the perfusion pressure and pump flow rate while maintaining the arterial partial pressure of carbon dioxide. The incidence of Type II neurologic injuries was 3% before and 0.3% after the introduction of cerebral oximetry.
Many studies have investigated the utility of NIRS oxygenation monitoring in predicting and preventing the onset of POCD and postoperative delirium (Table 7). Most employed the INVOS™ or NIRO® systems, and rSO2 or TOI was the oximetry parameter used in clinical evaluation. An absolute decrease in rSO2 or TOI to 35–65%, a 20–30% relative decrease in rSO2 or TOI from baseline, or an AUC below the oxygen saturation threshold was used to prompt remedial interventions. Among the seven studies of POCD listed in Table 7, five demonstrated a positive association between intraoperative NIRS measurements and the onset of POCD [125,126,127,128, 138], whereas the other two showed no positive association [122, 124]. Although the reasons for these contradictory results remain largely speculative, the timing of clinical evaluation or differences in the neurocognitive test battery or POCD diagnosis criteria may possibly have contributed to the varied outcomes. In addition, a positive association between an intraoperative decrease in rSO2 and the onset of postoperative delirium has been demonstrated [129]. The body of available evidence highlights the utility of intraoperative NIRS oxygenation monitoring in predicting the subsequent development of POCD and delirium. Furthermore, proactive intervention strategies to maintain the NIRS cerebral oxygen saturation at or above 80% or 85% of baseline have been shown to prevent postoperative delirium [130] and neurocognitive decline [131].
In a prospective, randomized study of patients undergoing CABG surgery, Murkin et al. showed that active interventions to maintain rSO2 values at or above 75% of baseline were associated with a significant decrease in mortality, major organ morbidity (ventilation > 48 h, stroke, myocardial infarction, return for reexploration), and stay in the intensive care unit, compared with no interventions [132]. In the study by Murkin et al., cerebral desaturation was defined as a decrease in saturation values below 70% of baseline for 1 min or longer. However, to minimize the probability of patients reaching these levels, interventions to improve cerebral oxygenation were initiated when rSO2 reached 75% of baseline for > 15 s. Denault et al. proposed an eight-step algorithm that incorporated a trigger rSO2 threshold defined by a 20% bilateral or unilateral relative reduction from baseline or an absolute decrease below 50% [133]. Figure 7 shows an algorithm proposed for hemodynamic management in cardiac surgery with cardiopulmonary bypass, with a minor modification based on the Murkin et al. and Denault et al. studies [132, 133].
A proposed algorithm for cardiac surgery with cardiopulmonary bypass (arranged from the figure in [116, 117] with a minor modification). MAP mean arterial pressure, CVP central venous pressure, SaO2 arterial oxygen saturation, PaCO2 arterial partial pressure of carbon dioxide, Hb hemoglobin, SvO2 venous oxygen saturation, TEE transesophageal echocardiography, CPB cardiopulmonary bypass, CMRO2 cerebral metabolic rate of oxygen, ICP intracranial pressure
When abnormal rSO2 data are obtained (i.e., 20–30% relative decrease from baseline), the surgeon should review the catheter placement, head position, arterial oxygen saturation, mean arterial pressure, central venous pressure, cardiac index, mixed venous oxygen saturation, hemoglobin concentration, and other variables. Appropriate and timely interventions should be implemented to reduce the risk of major organ dysfunction.
Scientists recently discovered a NIRS method to assess cerebral blood flow autoregulation based on spontaneous variations in blood pressure. When the mean arterial blood pressure is within the autoregulatory range, NIRS oxygenation saturation is less dependent on fluctuations in blood pressure. By contrast, when the mean arterial blood pressure falls below the lower autoregulatory limit, the dependence of NIRS oxygenation saturation on arterial blood pressure becomes more pronounced. On the basis of the lower limit of autoregulation, the acceptable lower limit of cerebral perfusion pressure during cardiopulmonary bypass should be 50 mmHg [72]. However, based on data from 225 patients, a clinical study reported a wide 95% prediction interval of 43–90 mmHg for mean arterial pressure at the lower limit of autoregulation [134].
Pediatric cardiac surgery
Points to consider in pediatric patients
Summary statement
-
In pediatric patients undergoing cardiac surgery, NIRS oxygen saturation data vary significantly depending on the medical condition.
Commentary
The anatomical and physiological properties that affect NIRS oxygen saturation measurements differ considerably between children and adults. For example, the skull and scalp are still developing in infants and are often thinner than in adults. These characteristics suggest that extracranial blood flow has a smaller impact on NIRS measurements in children than in adults. In pediatric patients undergoing cardiac surgery, NIRS oxygen saturation data vary significantly dependent on the medical conditions involved. In patients who underwent palliative surgery on cardiopulmonary bypass for single-ventricle congenital heart defects, the mean baseline rSO2 value measured before the induction of anesthesia was approximately 70% of that in patients without left-to-right shunt or cyanosis, and 40–60% of that in patients with cyanosis [135]. The mean (standard deviation) rSO2 value measured after anesthesia induction was 61% (11%) in infants with D-transposition of the great arteries, 71% (14%) in those with tetralogy of Fallot, 62% (9%) in those with ventricular septal defect [136], and 60% (11%) in those with hypoplastic left heart syndrome [137].
Use of NIRS oxygenation monitoring and alarm thresholds in pediatric cardiac surgery
Summary statements
-
In pediatric cardiac surgery, NIRS oxygen monitoring is used to identify the safe duration of DHCA and the risk of hypoperfusion of the left hemisphere, which tends to be less oxygenated than the right hemisphere during regional low-flow cerebral perfusion.
-
A decrease in perioperative NIRS oxygen saturation has been associated with the development of postoperative neurologic and other complications.
Commentary
In pediatric cardiac surgery, NIRS oxygen monitoring is used to identify the safe duration of DHCA and the risk of hypoperfusion of the left hemisphere, which tends to be less oxygenated than the right hemisphere during regional low-flow cerebral perfusion. In children undergoing cardiac surgery, rSO2 values decreased to 60–70% of baseline over the duration of DHCA, reaching the nadir in 20–40 min [136]. The half-life of change in NIRS oxygenation saturation during DHCA was inversely related to age: 9 min in neonates (age < 1 month), 6 min in infants (age 1–12 months), and 4 min in children (age 1–4 years) [137]. These results indicate that cerebral oxygen consumption increases with age. In a study of 19 neonates undergoing regional low-flow cerebral perfusion via the brachiocephalic artery, a mean rSO2 difference of 6.3% between the hemispheres was observed, with the left hemisphere showing lower values, and nearly half of the patients had sustained differences of > 10% [82]. However, the impact of left-to-right rSO2 differences on the onset of postoperative neurologic complications was not evaluated in this study.
Table 8 summarizes major pediatric cardiac surgery studies that investigated the association between NIRS oxygenation data and neurologic complications or other outcomes.
In a study of 26 pediatric patients who underwent cardiac surgery, three had an abnormal postoperative neurologic status; these patients had a smaller rSO2 increase during DHCA than other patients, with a shorter time to DHCA [137]. The smaller rSO2 changes during DHCA may have reflected insufficient cooling of the brain [137]. In a retrospective study of 250 pediatric patients with congenital heart disease, Austin et al. employed TCD and NIRS for neurophysiologic monitoring. They showed that interventions based on a 50% reduction from baseline in the peak flow velocity or a 20% relative decrease from baseline in rSO2 decreased the incidence of postoperative neurologic sequelae and the length of hospital stay [138]. In a study of 22 neonates who underwent the Norwood procedure for hypoplastic left heart syndrome, a prolonged duration of low postoperative rSO2 values (< 45% for > 180 min) was associated with abnormal findings on postoperative MRI scans [81]. In a prospective cohort study of 66 term newborns requiring surgery for congenital heart disease, 16 underwent intraoperative NIRS monitoring (n = 11 with transposition of the great arteries, n = 4 with hypoplastic left heart syndrome, and n = 1 with aortic arch obstruction) [80]. Six of them showed brain injury on postoperative MRI scans, and their mean total oxygen index during aortic clamping was significantly lower than in non-injured patients. Moreover, in a retrospective analysis of 50 consecutive newborns who received surgery for hypoplastic left heart syndrome, 18 adverse events occurred in 11 patients [87]. The mean rSO2 over the first 48 postoperative hours was smaller in these patients than in other patients. Of note, in a study of 68 neonates undergoing cardiac surgery with cardiopulmonary bypass, no association was found between prolonged low rSO2 < 45% in the intra- and postoperative periods and any measure of postoperative MRI brain injury [75].
Use of NIRS oxygenation monitoring in cardiovascular surgery in Japan
Summary statements
-
NIRS oxygenation monitoring is used at 84% of departments that perform cardiac and aortic surgery in Japan. More than 90% of the cardiac and aortic surgery facilities that employ this monitoring modality consider it useful.
-
NIRS oxygenation monitoring is used at 64% of facilities in Japan that perform CEA. Most of the CEA facilities that employ this monitoring modality consider it useful.
Commentary
In a 2015 survey on the use of NIRS oxygenation monitoring in cardiovascular anesthesia, the JSCVA mailed a questionnaire to 487 Japanese medical centers that had an anesthesia department, of which 184 (38%) responded [139]. All 184 stated that they provided cardiac and aortic surgery services, and 155 (84%) used intraoperative NIRS oxygenation monitoring. At 70 centers (38%), this monitoring method was routinely implemented. NIRS oxygenation monitoring was not adopted at 29 centers (16%). The most frequent reasons for not using NIRS oxygenation monitoring included the following: (1) the center did not possess a NIRS device, (2) the monitoring procedure was not covered by the national health insurance policy, and (3) the costs of the purchase and application of the device were high. These reasons related to hospital financial management. More than 90% of the centers that implemented NIRS oxygenation monitoring considered it to be useful for cerebral circulation management during cardiac surgery and cardiopulmonary bypass. Questions regarding CEA showed that 47% of the responding centers routinely used NIRS oxygenation monitoring whereas 36% did not. Most of the centers that employed this modality in CEA mentioned that it was useful for the detection and management of cerebral hypoperfusion and hyperperfusion. Apart from cardiac, aortic, and CEA surgery, NIRS oxygenation monitoring was utilized in the surgical management of patients with a history of cerebral infarction, carotid stenosis, Moyamoya disease, and intracranial aneurysm that required vascular reconstruction. Fifty-eight centers mentioned its use in surgery for patients with carotid stenosis.
Concluding remarks
This document provides an overview of the current epidemiology and pathogenetic mechanisms of perioperative brain injury in cardiovascular surgery. It also summarizes the principles and application of NIRS oxygenation monitoring as a tool to prevent surgically induced brain injury. Moreover, this document presents practical considerations in the use of this monitoring method and discusses approaches to abnormal findings. The available clinical evidence is insufficient to establish a comprehensive intervention program to prevent perioperative brain injury based on NIRS oxygenation monitoring. However, this noninvasive and continuous monitoring technique has been shown to detect perfusion abnormalities that occur during surgery. Further research is warranted to establish the utility of NIRS oxygenation monitoring in improving neurologic and other outcomes. In particular, more attention should be paid to the accuracy and precision of commercially available NIRS oxygenation monitoring devices. Appropriately using this monitoring modality to detect changes in cerebral metabolism and other physiological conditions in patients undergoing cardiovascular surgery, and implementing timely interventions in response to abnormal findings, will help improve functional outcomes. The JSCVA should make efforts to expand the use of NIRS oxygenation monitoring in clinical practice, and the future coverage of this modality under the national health insurance policy will be a key to this expansion.
Abbreviations
- ACP:
-
Antegrade cerebral perfusion
- AUC:
-
Area under the curve
- CABG:
-
Coronary artery bypass grafting
- CEA:
-
Carotid endarterectomy
- CHS:
-
Cerebral hyperperfusion syndrome
- DHCA:
-
Deep hypothermic circulatory arrest
- ICG:
-
Indocyanine green
- JSCVA:
-
Japanese Society of Cardiovascular Anesthesiologists
- LED:
-
Light emitting diode
- MBL:
-
Modified Beer–Lambert
- MRI:
-
Magnetic resonance imaging
- NIRS:
-
Near-infrared spectroscopy
- POCD:
-
Postoperative cognitive dysfunction
- RCP:
-
Retrograde cerebral perfusion
- rSO2 :
-
Regional cerebral oxygen saturation
- SCP:
-
Selective cerebral perfusion
- SEP:
-
Somatosensory evoked potential
- SPECT:
-
Single photon emission computed tomography
- SRS:
-
Spatially resolved spectroscopy
- SSEP:
-
Somatosensory evoked potential
- TAVR:
-
Transcatheter aortic valve replacement
- TCD:
-
Transcranial Doppler
- TEVAR:
-
Thoracic endovascular aortic repair
- TOI:
-
Tissue oxygenation index
- TRS:
-
Time-resolved spectroscopy
References
Mashour GA, Shanks AM, Kheterpal S. Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology. 2011;114:1289–96.
Hill MD, Brooks W, Mackey A, Clark WM, Meschia JF, Morrish WF, Mohr JP, Rhodes JD, Popma JJ, Lal BK, Longbottom ME, Voeks JH, Howard G, Brott TG, CREST Investigators. Stroke after carotid stenting and endarterectomy in the carotid revascularization endarterectomy versus stenting trial (CREST). Circulation. 2012;126:3054–61.
Heyer EJ, Mergeche JL, Bruce SS, Ward JT, Stern Y, Anastasian ZH, Quest DO, Solomon RA, Todd GJ, Benvenisty AI, McKinsey JF, Nowygrod R, Morrissey NJ, Connolly ES. Statins reduce neurologic injury in asymptomatic carotid endarterectomy patients. Stroke. 2013;44:1150–2.
Barbetta I, Carmo M, Mercandalli G, Lattuada P, Mazzaccaro D, Settembrini AM, Dallatana R, Settembrini PG. Outcomes of urgent carotid endarterectomy for stable and unstable acute neurologic deficits. J Vasc Surg. 2014;59:440–6.
Takase S, Yokoyama H. Future role of CABG surgery in coronary artery heart disease: fighting stroke, less invasiveness, and data disclosure (in Japanese). J Jpn Coron Assoc. 2013;19:301–5.
Tarakji KG, Sabik JF III, Bhudia SK, Batizy LH, Blackstone EH. Temporal onset, risk factors, and outcomes associated with stroke after coronary artery bypass grafting. JAMA. 2011;305:381–90.
Mérie C, Køber L, Olsen PS, Andersson C, Jensen JS, Torp-Pedersen C. Risk of stroke after coronary artery bypass grafting: effect of age and comorbidities. Stroke. 2012;43:38–43.
Shahian DM, O’Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP, Society of Thoracic Surgeons Quality Measurement Task Force. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 3–valve plus coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88:43–62.
O’Brien SM, Shahian DM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP. Society of Thoracic Surgeons Quality Measurement Task Force. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 2–isolated valve surgery. Ann Thorac Surg. 2009;88:23–42.
Hu Z, Wang Z, Ren Z, Wu H, Zhang M, Zhang H, Hu X. Similar cerebral protective effectiveness of antegrade and retrograde cerebral perfusion combined with deep hypothermia circulatory arrest in aortic arch surgery: a meta-analysis and systematic review of 5060 patients. J Thorac Cardiovasc Surg. 2014;148:544–60.
Tokuda Y, Miyata H, Motomura N, Oshima H, Usui A, Takamoto S, Japan Adult Cardiovascular Database Organization. Brain protection during ascending aortic repair for Stanford type A acute aortic dissection surgery. Nationwide analysis in Japan. Circ J. 2014;78:2431–8.
Knowles M, Murphy EH, Dimaio JM, Modrall JG, Timaran CH, Jessen ME, Arko FR III. The effects of operative indication and urgency of intervention on patient outcomes after thoracic aortic endografting. J Vasc Surg. 2011;53:926–34.
Patterson BO, Holt PJ, Nienaber C, Fairman RM, Heijmen RH, Thompson MM. Management of the left subclavian artery and neurologic complications after thoracic endovascular aortic repair. J Vasc Surg. 2014;60:1491–7.
Zahn R, Erbel R, Nienaber CA, Neumann FJ, Nef H, Eggebrecht H, Senges J. Endovascular aortic repair of thoracic aortic disease: early and 1-year results from a German multicenter registry. J Endovasc Ther. 2013;20:265–72.
Daneault B, Kirtane AJ, Kodali SK, Williams MR, Genereux P, Reiss GR, Smith CR, Moses JW, Leon MB. Stroke associated with surgical and transcatheter treatment of aortic stenosis: a comprehensive review. J Am Coll Cardiol. 2011;58:2143–50.
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K, Graham SH, Ley C. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med. 1996;335:1857–63.
Martin BJ, Buth KJ, Arora RC, Baskett RJ. Delirium: a cause for concern beyond the immediate postoperative period. Ann Thorac Surg. 2012;93:1114–20.
Gottesman RF, Grega MA, Bailey MM, Pham LD, Zeger SL, Baumgartner WA, Selnes OA, McKhann GM. Delirium after coronary artery bypass graft surgery and late mortality. Ann Neurol. 2010;67:338–44.
Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, Jones RN. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367:30–9.
Kazmierski J, Kowman M, Banach M, Fendler W, Okonski P, Banys A, Jaszewski R, Rysz J, Mikhailidis DP, Sobow T, Kloszewska I, IPDACS Study. Incidence and predictors of delirium after cardiac surgery: results from The IPDACS Study. J Psychosom Res. 2010;69:179–85.
Rudolph JL, Inouye SK, Jones RN, Yang FM, Fong TG, Levkoff SE, Marcantonio ER. Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc. 2010;58:643–9.
Milstein A, Pollack A, Kleinman G, Barak Y. Confusion/delirium following cataract surgery: an incidence study of 1-year duration. Int Psychogeriatr. 2002;14:301–6.
Mann C, Pouzeratte Y, Boccara G, Peccoux C, Vergne C, Brunat G, Domergue J, Millat B, Colson P. Comparison of intravenous or epidural patient-controlled analgesia in the elderly after major abdominal surgery. Anesthesiology. 2000;92:433–41.
Kaneko T, Takahashi S, Naka T, Hirooka Y, Inoue Y, Kaibara N. Postoperative delirium following gastrointestinal surgery in elderly patients. Surg Today. 1997;27:107–11.
Fisher BW, Flowerdew G. A simple model for predicting postoperative delirium in older patients undergoing elective orthopedic surgery. J Am Geriatr Soc. 1995;43:175–8.
Weed HG, Lutman CV, Young DC, Schuller DE. Preoperative identification of patients at risk for delirium after major head and neck cancer surgery. Laryngoscope. 1995;105:1066–8.
Marcantonio ER, Goldman L, Mangione CM, Ludwig LE, Muraca B, Haslauer CM, Donaldson MC, Whittemore AD, Sugarbaker DJ, Poss R, Haas S, Cook EF, Orav EJ, Lee TH. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994;271:134–9.
Schneider F, Böhner H, Habel U, Salloum JB, Stierstorfer A, Hummel TC, Miller C, Friedrichs R, Müller EE, Sandmann W. Risk factors for postoperative delirium in vascular surgery. Gen Hosp Psychiatry. 2002;24:28–34.
Böhner H, Hummel TC, Habel U, Miller C, Reinbott S, Yang Q, Gabriel A, Friedrichs R, Müller EE, Ohmann C, Sandmann W, Schneider F. Predicting delirium after vascular surgery: a model based on pre- and intraoperative data. Ann Surg. 2003;238:149–56.
Benoit AG, Campbell BI, Tanner JR, Staley JD, Wallbridge HR, Biehl DR, Bradley BD, Louridas G, Guzman RP, Fromm RA. Risk factors and prevalence of perioperative cognitive dysfunction in abdominal aneurysm patients. J Vasc Surg. 2005;42:884–90.
Johnson T, Monk T, Rasmussen LS, Abildstrom H, Houx P, Korttila K, Kuipers HM, Hanning CD, Siersma VD, Kristensen D, Canet J, Ibañaz MT, Moller JT, ISPOCD2 Investigators. Postoperative cognitive dysfunction in middle-aged patients. Anesthesiology. 2002;96:1351–7.
Canet J, Raeder J, Rasmussen LS, Enlund M, Kuipers HM, Hanning CD, Jolles J, Korttila K, Siersma VD, Dodds C, Abildstrom H, Sneyd JR, Vila P, Johnson T, Muñoz Corsini L, Silverstein JH, Nielsen IK, Moller JT, ISPOCD2 investigators. Cognitive dysfunction after minor surgery in the elderly. Acta Anaesthesiol Scand. 2003;47:1204–10.
van Dijk D, Keizer AM, Diephuis JC, Durand C, Vos LJ, Hijman R. Neurocognitive dysfunction after coronary artery bypass surgery: a systematic review. J Thorac Cardiovasc Surg. 2000;120:632–9.
Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA, Neurological Outcome Research Group and the Cardiothoracic Anesthesiology Research Endeavors Investigators. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344:395–402.
Rasmussen LS, Larsen K, Houx P, Skovgaard LT, Hanning CD, Moller JT, ISPOCD group. The International Study of Postoperative Cognitive Dysfunction. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand. 2001;45:275–89.
Rudolph JL, Schreiber KA, Culley DJ, McGlinchey RE, Crosby G, Levitsky S, Marcantonio ER. Measurement of post-operative cognitive dysfunction after cardiac surgery: a systematic review. Acta Anaesthesiol Scand. 2010;54:663–77.
Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Onnasch JF, Metz S, Falk V, Mohr FW. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003;75:472–8.
Anyanwu AC, Filsoufi F, Salzberg SP, Bronster DJ, Adams DH. Epidemiology of stroke after cardiac surgery in the currentera. J Thorac Cardiovasc Surg. 2007;134:1121–7.
Dacey LJ, Likosky DS, Leavitt BJ, Lahey SJ, Quinn RD, Hernandez F Jr, Quinton HB, Desimone JP, Ross CS, O’Connor GT, Northern New England Cardiovascular Disease Study Group. Perioperative stroke and long-term survival after coronary bypass graft surgery. Ann Thorac Surg. 2005;79:532–6.
McKhann GM, Grega MA, Borowicz LM Jr, Baumgartner WA, Selnes OA. Stroke and encephalopathy after cardiac surgery: an update. Stroke. 2006;37:562–71.
Newman MF, Grocott HP, Mathew JP, White WD, Landolfo K, Reves JG, Laskowitz DT, Mark DB, Blumenthal JA, Neurologic Outcome Research Group and the Cardiothoracic Anesthesia Research Endeavors (CARE) Investigators of the Duke Heart Center. Report of the substudy assessing the impact of neurocognitive function on quality of life 5 years after cardiac surgery. Stroke. 2001;32:2874–81.
Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, Rankin RN, Clagett GP, Hachinski VC, Sackett DL, Thorpe KE, Meldrum HE, Spence JD. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339:1415–25.
Risk of stroke in the distribution of an asymptomatic carotid artery. The European Carotid Surgery Trialists Collaborative Group. Lancet. 1995;345:209–12.
Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998;351:1379–87.
Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA. 1995;273:1421–8.
Hobson RW II, Weiss DG, Fields WS, Goldstone J, Moore WS, Towne JB, Wright CB. Efficacy of carotid endarterectomy for asymptomatic carotid stenosis. The Veterans Affairs Cooperative Study Group. N Engl J Med. 1993;328:221–7.
Mayberg MR, Wilson SE, Yatsu F, Weiss DG, Messina L, Hershey LA, Colling C, Eskridge J, Deykin D, Winn HR. Carotid endarterectomy and prevention of cerebral ischemia in symptomatic carotid stenosis. Veterans Affairs Cooperative Studies Program 309 Trialist Group. JAMA. 1991;266:3289–94.
North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445–53.
Rothwell PM, Gibson RJ, Slattery J, Sellar RJ, Warlow CP. Prognostic value and reproducibility of measurements of carotid stenosis. A comparison of three methods on 1001 angiograms. European Carotid Surgery Trialists’ Collaborative Group. Stroke. 1994;25:2440–4.
Japan Stroke Society Committee on the Japanese Guidelines for the Management of Stroke. In. Japanese guidelines for the management of stroke 2015, First Edition. Tokyo: Kyowa Kikaku; 2015 (in Japanese).
Kretz B, Abello N, Bouchot O, Kazandjian C, Beaumont M, Terriat B, Bernard A, Brenot R, Steinmetz E. Risk index for predicting shunt in carotid endarterectomy. Ann Vasc Surg. 2014;28:1204–12.
Aburahma AF, Mousa AY, Stone PA. Shunting during carotid endarterectomy. J Vasc Surg. 2011;54:1502–10.
Ogasawara K, Sakai N, Kuroiwa T, Hosoda K, Iihara K, Toyoda K, Sakai C, Nagata I, Ogawa A, Japanese Society for Treatment at Neck in Cerebrovascular Disease Study Group. Intracranial hemorrhage associated with cerebral hyperperfusion syndrome following carotid endarterectomy and carotid artery stenting: retrospective review of 4494 patients. J Neurosurg. 2007;107:1130–6.
Stecker MM, Cheung AT, Pochettino A, Kent GP, Patterson T, Weiss SJ, Bavaria JE. Deep hypothermic circulatory arrest: I. Effects of cooling on electroencephalogram and evoked potentials. Ann Thorac Surg. 2001;71:14–21.
James ML, Andersen ND, Swaminathan M, Phillips-Bute B, Hanna JM, Smigla GR, Barfield ME, Bhattacharya SD, Williams JB, Gaca JG, Husain AM, Hughes GC. Predictors of electrocerebral inactivity with deep hypothermia. J Thorac Cardiovasc Surg. 2014;147:1002–7.
Orihashi K, Sueda T, Okada K, Imai K. Malposition of selective cerebral perfusion catheter is not a rare event. Eur J Cardiothorac Surg. 2005;27:644–8.
Safi HJ, Miller CC III, Lee TY, Estrera AL. Repair of ascending and transverse aortic arch. J Thorac Cardiovasc Surg. 2011;142:630–3.
Harris DN, Bailey SM, Smith PL, Taylor KM, Oatridge A, Bydder GM. Brain swelling in first hour after coronary artery bypass surgery. Lancet. 1993;342:586–7.
Usui A, Oohara K, Liu TL, Murase M, Tanaka M, Takeuchi E, Abe T. Determination of optimum retrograde cerebral perfusion conditions. J Thorac Cardiovasc Surg. 1994;107:300–8.
Okita Y, Miyata H, Motomura N, Takamoto S, Japan Cardiovascular Surgery Database Organization. A study of brain protection during total arch replacement comparing antegrade cerebral perfusion versus hypothermic circulatory arrest, with or without retrograde cerebral perfusion: analysis based on the Japan Adult Cardiovascular Surgery Database. J Thorac Cardiovasc Surg. 2015;149:65–73.
Committee for Scientific Affairs, The Japanese Association for Thoracic Surgery. Masuda M, Kuwano H, Okumura M, Arai H, Endo S, Doki Y, Kobayashi J, Motomura N, Nishida H, Saiki Y, Tanaka F, Tanemoto K, Toh Y, Yokomise H. Thoracic and cardiovascular surgery in Japan during 2013: Annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2015;63:670–701.
Orihashi K. Cerebral malperfusion in acute aortic dissection. Surg Today. 2016;46:1353–61.
Most H, Reinhard B, Gahl B, Englberger L, Kadner A, Weber A, Schmidli J, Carrel TP, Huber C. Is surgery in acute aortic dissection type A still contraindicated in the presence of preoperative neurological symptoms? Eur J Cardiothorac Surg. 2015;48:945–50.
Fleck T, Ehrlich M, Czerny M, Wolner E, Grabenwoger M, Grimm M. Intraoperative iatrogenic type A aortic dissection and perioperative outcome. Interact Cardiovasc Thorac Surg. 2006;5:11–4.
Ura M, Sakata R, Nakayama Y, Goto T. Ultrasonographic demonstration of manipulation-related aortic injuries after cardiac surgery. J Am Coll Cardiol. 2000;35:1303–10.
Kapetanakis EI, Stamou SC, Dullum MK, Hill PC, Haile E, Boyce SW, Bafi AS, Petro KR, Corso PJ. The impact of aortic manipulation on neurologic outcomes after coronary artery bypass surgery: a risk-adjusted study. Ann Thorac Surg. 2004;78:1564–71.
Caplan LR, Hennerici M. Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol. 1998;55:1475–82.
Gottesman RF, Sherman PM, Grega MA, Yousem DM, Borowicz LM Jr, Selnes OA, Baumgartner WA, McKhann GM. Watershed strokes after cardiac surgery: diagnosis, etiology, and outcome. Stroke. 2006;37:2306–11.
Gold JP, Charlson ME, Williams-Russo P, Szatrowski TP, Peterson JC, Pirraglia PA, Hartman GS, Yao FS, Hollenberg JP, Barbut D, Hayes JG, Thomas SJ, Purcell MH, Mattis S, Gorkin L, Post M, Krieger KH, Isom OW. Improvement of outcomes after coronary artery bypass. A randomized trial comparing intraoperative high versus low mean arterial pressure. J Thorac Cardiovasc Surg. 1995;110:1302–11.
Hogue CW Jr, Palin CA, Arrowsmith JE. Cardiopulmonary bypass management and neurologic outcomes: an evidence-based appraisal of current practices. Anesth Analg. 2006;103:21–37.
Laffey JG, Boylan JF, Cheng DC. The systemic inflammatory response to cardiac surgery: implications for the anesthesiologist. Anesthesiology. 2002;97:215–52.
Brady K, Joshi B, Zweifel C, Smielewski P, Czosnyka M, Easley RB, Hogue CW Jr. Real-time continuous monitoring of cerebral blood flow autoregulation using near-infrared spectroscopy in patients undergoing cardiopulmonary bypass. Stroke. 2010;41:1951–6.
du Plessis AJ. Mechanisms of brain injury during infant cardiac surgery. Semin Pediatr Neurol. 1999;6:32–47.
Strauss AW, Johnson MC. The genetic basis of pediatric cardiovascular disease. Semin Perinatol. 1996;20:564–76.
Andropoulos DB, Hunter JV, Nelson DP, Stayer SA, Stark AR, McKenzie ED, Heinle JS, Graves DE, Fraser CD Jr. Brain-immaturity is associated with brain injury before and after neonatal cardiac surgery with high-flow bypass and cerebral oxygenation monitoring. J Thorac Cardiovasc Surg. 2010;139:543–56.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weight less than 1500 gm. J Pediatr. 1978;92:529–34.
Te Pas AB, van Wezel-Meijler G, Bokenkamp-Gramann R, Walther FJ. Preoperative cranial ultrasound findings in infants with major congenital heart disease. Acta Paediatr. 2005;94:1597–603.
Laptook AR, Shankaran S, Ambalavanan N, Carlo WA, McDonald SA, Higgins RD, Das A, The Hyothermia Subcommitte of the NICD Neonatal Research Network. Outcome of term infants using apgar scores at 10 minutes following hypoxic-ischemic encephalopathy. Pediatrics. 2009;124:1619.
Mahle WT, Tavani F, Zimmerman RA, Nicolson SC, Galli KK, Gaynor JW, Clancy RR, Montenegro LM, Spray TL, Chiavacci RM, Wernovsky G, Kurth CD. An MRI study of neurological injury before and after congenital heart surgery. Circulation. 2002;106:1109–14.
McQuillen PS, Barkovich AJ, Hamrick SE, Perez M, Ward P, Glidden DV, Azakie A, Karl T, Miller SP. Temporal and anatomic risk profile of brain injury with neonatal repair of congenital heart defects. Stroke. 2007;38:736–41.
Dent CL, Spaeth JP, Jones BV, Schwartz SM, Glauser TA, Hallinan B, Pearl JM, Khoury PR, Kurth CD. Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg. 2006;131:190–7.
Andropoulos DB, Diaz LK, Fraser CD Jr, McKenzie ED, Stayer SA. Is bilateral monitoring of cerebral oxygen saturation necessary during neonatal aortic arch reconstruction? Anesth Analg. 2004;98:1267–72.
Abdul Aziz KA, Meduoye A. Is pH-stat or alpha-stat the best technique to follow in patients undergoing deep hypothermic circulatory arrest? Interact Cardiovasc Thorac Surg. 2010;10:271–82.
Hongo K, Kobayashi S, Okudera H, Hokama M, Nakagawa F. Noninvasive cerebral optical spectroscopy: depth-resolved measurements of cerebral haemodynamics using indocyanine green. Neurol Res. 1995;17:89–93.
Yamashita Y. The measurement principles of time-resolved spectroscopy (in Japanese). In: Okada E, Hoshi Y, Miyai I, Watanabe E, editors. NIRS: its basics and clinical application. Tokyo: Shinkoh Igaku Shuppansha; 2012. pp. 19–22.
Sakatani K. Basic principles (in Japanese). In: Japan Cerebral Metabolism Monitoring Research Group, editor. Near-infrared spectroscopy made easy for clinicians. Tokyo: Shinkoh Igaku Shuppansha; 2002: pp. 1–9.
Phelps HM, Mahle WT, Kim D, Simsic JM, Kirshbom PM, Kanter KR, Maher KO. Postoperative cerebral oxygenation in hypoplastic left heart syndrome after the Norwood procedure. Ann Thorac Surg. 2009;87:1490–4.
Shiraishi Y, Yokoyama J, Atsumi K, Satou N, Momose K, Yamaguchi N. Hazard induced by sensor probe of near infrared spectroscopy (Invos 3100A) (in Japanese with English abstract). J Jpn Soc Clin Anesth. 2001;21:430–3.
Kishi K, Kawaguchi M, Yoshitani K, Nagahata T, Furuya H. Influence of patient variables and sensor location on regional cerebral oxygen saturation measured by INVOS 4100 near-infrared spectrophotometers. J Neurosurg Anesthesiol. 2003;15:302–6.
Cho AR, Kwon JY, Kim C, Hong JM, Kang C. Effect of sensor location on regional cerebral oxygen saturation measured by INVOS 5100 in on-pump cardiac surgery. J Anesth. 2017;31:178–84.
Yoshitani K, Kawaguchi M, Okuno T, Kanda T, Ohnishi Y, Kuro M, Nishizawa M. Measurements of optical pathlength using phase-resolved spectroscopy in patients undergoing cardiopulmonary bypass. Anesth Analg. 2007;104:341–6.
Yoshitani K, Kawaguchi M, Miura N, Okuno T, Kanda T, Ohnishi Y, Kuro M. Effects of hemoglobin concentration, skull thickness, and the area of the cerebrospinal fluid layer on near-infrared spectroscopy measurements. Anesthesiology. 2007;106:458–62.
Davie SN, Grocott HP. Impact of extracranial contamination on regional cerebral oxygen saturation: a comparison of three cerebral oximetry technologies. Anesthesiology. 2012;116:834–40.
Ogoh S, Sato K, Okazaki K, Miyamoto T, Secher F, Sørensen H, Rasmussen P, Secher NH. A decrease in spatially resolved near-infrared spectroscopy-determined frontal lobe tissue oxygenation by phenylephrine reflects reduced skin blood flow. Anesth Analg. 2014;118:823–9.
Kato S, Yoshitani K, Kubota Y, Inatomi Y, Ohnishi Y. Effect of posture and extracranial contamination on results of cerebral oximetry by near-infrared spectroscopy. J Anesth. 2017;31:103–10.
Closhen D, Berres M, Werner C, Engelhard K, Schramm P. Influence of beach chair position on cerebral oxygen saturation: a comparison of INVOS and FORE-SIGHT cerebral oximeter. J Neurosurg Anesthesiol. 2013;25:414–9.
Lee JR, Lee PB, Do SH, Jeon YT, Lee JM, Hwang JY, Han SH. The effect of gynaecological laparoscopic surgery on cerebral oxygenation. J Int Med Res. 2006;34:531–6.
Park EY, Koo BN, Min KT, Nam SH. The effect of pneumoperitoneum in the steep Trendelenburg position on cerebral oxygenation. Acta Anaesthesiol Scand. 2009;53:895–9.
Kalmar AF, Foubert L, Hendrickx JF, Mottrie A, Absalom A, Mortier EP, Struys MM. Influence of steep Trendelenburg position and CO2 pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth. 2010;104:433–9.
Closhen D, Treiber AH, Berres M, Sebastiani A, Werner C, Engelhard K, Schramm P. Robotic assisted prostatic surgery in the Trendelenburg position does not impair cerebral oxygenation measured using two different monitors: a clinical observational study. Eur J Anaesthesiol. 2014;31:104–9.
Nielsen HB. Systematic review of near-infrared spectroscopy determined cerebral oxygenation during non-cardiac surgery. Front Physiol. 2014;5:93.
Kirkpatrick PJ, Lam J, Al-Rawi P, Smielewski P, Czosnyka M. Defining thresholds for critical ischemia by using near-infrared spectroscopy in the adult brain. J Neurosurg. 1998;89:389–94.
Oyama H, Endoh O, Iizuka H, Ikeda S, Inoue S, Nakashima Y, Shibuya S. The effectiveness of regional cerebral oxygen saturation monitoring using near-infrared spectroscopy in carotid endarterectomy. J Clin Neurosci. 2003;10:79–83.
Carlin RE, McGraw DJ, Calimlim JR, Mascia MF. The use of near-infrared cerebral oximetry in awake carotid endarterectomy. J Clin Anesth. 1998;10:109–13.
Beese U, Langer H, Lang W, Dinkel M. Comparison of near-infrared spectroscopy and somatosensory evoked potentials for the detection of cerebral ischemia during carotid endarterectomy. Stroke. 1998;29:2032–7.
Cho H, Nemoto EM, Yonas H, Balzer J, Sclabassi RJ. Cerebral monitoring by means of oximetry and somato sensory evoked potentials during carotid endarterectomy. J Neurosurg. 1998;89:533–8.
Samra SK, Dy EA, Welch K, Dorje P, Zelenock GB, Stanley JC. Evaluation of a cerebral oximeter as a monitor of cerebralischemia during carotid endarterectomy. Anesthesiology. 2000;93:964–70.
Mille T, Tachimiri ME, Klersy C, Ticozzelli G, Bellinzona G, Blangetti I, Pirrelli S, Lovotti M, Odero A. Near infrared spectroscopy monitoring during carotid endarterectomy: which threshold value is critical? Eur J Vasc Endovasc Surg. 2004;27:646–50.
Yamamoto K, Miyata T, Nagawa H. Good correlation between cerebral oxygenation measured using near infrared spectroscopy and stump pressure during carotid clamping. Int Angiol. 2007;26:262–5.
Moritz S, Kasprzak P, Arlt M, Taeger K, Metz C. Accuracy of cerebral monitoring in detecting cerebral ischemia during carotid endarterectomy: a comparison of transcranial Doppler sonography, near-infrared spectroscopy, stump pressure, and somatosensory evoked potentials. Anesthesiology. 2007;107:563–9.
Pennekamp CW, Bots ML, Kappelle LJ, Moll FL, de Borst GJ. The value of near-infrared spectroscopy measured cerebraloximetry during carotid endarterectomy in perioperative stroke prevention. A review. Eur J Vasc Endovasc Surg. 2009;38:539–45.
Pennekamp CW, Immink RV, den Ruijter HM, Kappelle LJ, Ferrier CM, Bots ML, Buhre WF, Moll FL, de Borst GJ. Nearinfrared spectroscopy can predict the onset of cerebral hyperperfusion syndrome after carotid endarterectomy. Cerebrovasc Dis. 2012;34:314–21.
Zogogiannis ID, Iatrou CA, Lazarides MK, Vogiatzaki TD, Wachtel MS, Chatzigakis PK, Dimitriou VK. Evaluation of an intraoperative algorithm based on near-infrared refracted spectroscopy monitoring, in the intraoperative decision for shunt placement, in patients undergoing carotid endarterectomy. Middle East J Anaesthesiol. 2011;21:367–73.
Ogasawara K, Inoue T, Kobayashi M, Endo H, Fukuda T, Ogawa A. Pretreatment with the free radical scavenger edaravone prevents cerebral hyperperfusion after carotid endarterectomy. Neurosurgery. 2004;55:1060–7.
Orihashi K, Sueda T, Okada K, Imai K. Near-infrared spectroscopy for monitoring cerebral ischemia during selective cerebral perfusion. Eur J Cardiothorac Surg. 2004;26:907–11.
Olsson C, Thelin S. Regional cerebral saturation monitoring with near-infrared spectroscopy during selective antegradecerebral perfusion: diagnostic performance and relationship to postoperative stroke. J Thorac Cardiovasc Surg. 2006;131:371–9.
Fischer GW, Lin HM, Krol M, Galati MF, Di Luozzo G, Griepp RB, Reich DL. Noninvasive cerebral oxygenation may predict outcome in patients undergoing aortic arch surgery. J Thorac Cardiovasc Surg. 2011;141:815–21.
Sakaguchi G, Komiya T, Tamura N, Obata S, Masuyama S, Kimura C, Kobayashi T. Cerebral malperfusion in acute type Adissection: direct innominate artery cannulation. J Thorac Cardiovasc Surg. 2005;129:1190–1.
Harrer M, Waldenberger PR, Weiss G, Folkmann S, Gorlitzer M, Moidl R, Grabenwoeger M. Aortic arch surgery using bilateral antegrade selective cerebral perfusion in combination with near-infrared spectrpscopy. Eur J Cardiothorac Surg. 2010;38:561–7.
Goldman S, Sulter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7:E376–81.
Edmonds HL Jr. Protective effect of neuromonitoring during cardiac surgery. Ann N Y Acad Sci. 2005;1053:12–9.
Reents W, Muellges W, Franke D, Babin-Ebell J, Elert O. Cerebral oxygen saturation assessed by near-infrared spectroscopy during coronary artery bypass grafting and early postoperative cognitive function. Ann Thorac Surg. 2002;74:109–14.
Yao FS, Tseng CC, Ho CY, Levin SK, Illner P. Cerebral oxygen desaturation is associated with early postoperative neuropsychological dysfunction in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18:552–8.
Hong SW, Shim JK, Choi YS, Kim DH, Chang BC, Kwak YL. Prediction of cognitive dysfunction and patients’ outcome following valvular heart surgery and the role of cerebral oximetry. Eur J Cardiothorac Surg. 2008;33:560–5.
Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM III, Rodriguez AL, Magovern CJ, Zaubler T, Freundlich K, Parr GV. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg. 2009;87:36–44.
Schoen J, Husemann L, Tiemeyer C, Lueloh A, Sedemund-Adib B, Berger KU, Hueppe M, Heringlake M. Cognitive function after sevoflurane- vs propofol-based anaesthesia for on-pump cardiac surgery: a randomized controlled trial. Br J Anaesth. 2011;106:840–50.
Fudickar A, Peters S, Stapelfeldt C, Serocki G, Leiendecker J, Meybohm P, Steinfath M, Bein B. Postoperative cognitive deficit after cardiopulmonary bypass with preserved cerebral oxygenation: a prospective observational pilot study. BMC Anesthesiol. 2011;11:7.
de Tournay-Jette E, Dupuis G, Bherer L, Deschamps A, Cartier R, Denault A. The relationship between cerebral oxygen saturation changes and postoperative cognitive dysfunction in elderly patients after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2011;25:95–104.
Schoen J, Meyerrose J, Paarmann H, Heringlake M, Hueppe M, Berger KU. Preoperative regional cerebral oxygen saturation is a predictor of postoperative delirium in on-pump cardiac surgery patients: a prospective observational trial. CritCare. 2011;15:R218.
Palmbergen WA, van Sonderen A, Keyhan-Falsafi AM, Keunen RW, Wolterbeek R. Improved perioperative neurological monitoring of coronary artery bypass graft patients reduces the incidence of postoperative delirium: the Haga Brain CareStrategy. Interact Cardiovasc Thorac Surg. 2012;15:671–7.
Mohandas BS, Jagadeesh AM, Vikram SB. Impact of monitoring cerebral oxygen saturation on the outcome of patients undergoing open heart surgery. Ann Card Anaesth. 2013;16:102–6.
Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, Cleland A, Schaefer B, Irwin B, Fox S. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51–8.
Denault A, Deschamps A, Murkin JM. A proposed algorithm for the intraoperative use of cerebral near-infrared spectroscopy. Semin Cardiothorac Vasc Anesth. 2007;11:274–81.
Joshi B, Ono M, Brown C, Brady K, Easley RB, Yenokyan G, Gottesman RF, Hogue CW. Predicting the limits of cerebralautoregulation during cardiopulmonary bypass. Anesth Analg. 2012;114:503–10.
Fenton KN, Lessman K, Glogowski K, Fogg S, Duncan KF. Cerebral oxygen saturation does not normalize until after stage 2 single ventricle palliation. Ann Thorac Surg. 2007;83:1431–6.
Kussman BD, Wypij D, DiNardo JA, Newburger JW, Mayer JE Jr, del Nido PJ, Bacha EA, Pigula F, McGrath E, Laussen PC. Cerebral oximetry during infant cardiac surgery: evaluation and relationship to early postoperative outcome. Anesth Analg. 2009;108:1122–31.
Kurth CD, Steven JM, Nicolson SC. Cerebral oxygenation during pediatric cardiac surgery using deep hypothermic circulatory arrest. Anesthesiology. 1995;82:74–82.
Austin EH III, Edmonds HL Jr, Auden SM, Seremet V, Niznik G, Sehic A, Sowell MK, Cheppo CD, Corlett KM. Benefit of neurophysiologic monitoring for pediatric cardiac surgery. J Thorac Cardiovasc Surg. 1997;114:707–17.
Kawaguchi M, Yoshitani K, Ishida K, Yokota M, Uezono S, Nomura M. Survey on perioperative use of cerebral near-infrared spectroscopy monitoring in Japan (in Japanese with English abstract). J Jpn Soc Clin Anesth. 2015;35:651–59.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Yoshitani, K., Kawaguchi, M., Ishida, K. et al. Guidelines for the use of cerebral oximetry by near-infrared spectroscopy in cardiovascular anesthesia: a report by the cerebrospinal Division of the Academic Committee of the Japanese Society of Cardiovascular Anesthesiologists (JSCVA). J Anesth 33, 167–196 (2019). https://doi.org/10.1007/s00540-019-02610-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02610-y