Abstract
Regional cerebral oximetry using near-infrared spectroscopy devices is commonly used for detecting cerebral ischemia during cardiopulmonary bypass, and aim to avoid poor cerebral perfusion which may result in perioperative neurological impairment. Today, several devices that can detect cerebral ischemia are commercially available. Although these devices operate on the same measurement principles, their algorithms for detecting and calculating cerebral ischemia are different and no criteria for directly comparing values measured by such different devices exist. From January 2017 to August 2017, 80 adult cardiovascular surgery patients were enrolled in the prospective study. In each patient, preoperative regional cerebral oxygen saturation values were measured by two different devices and their correlations with various preoperative factors were evaluated. Regional cerebral oxygen saturation levels were significantly higher for values of FORE-SIGHT ELITE (CAS Medical Systems, Branford, CT, USA) (F value) than those of the INVOS 5100C (Medtronic, Minneapolis, MN, USA) (I value). Scalp–cortex distance, hemoglobin concentration, and the presence or absence of hemodialysis showed significant correlations with ratios of measured values specific to each device (F/I). An appropriate device should be selected according to preoperative patient characteristics, and factors influencing regional cerebral oxygen saturation values should be considered to ensure the correct interpretation of measured values. This research was conducted with the approval of the ethics committee of our university (approval number: B16–96).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Regional cerebral oximetry using near-infrared spectroscopy (NIRS) devices is commonly used for detecting cerebral ischemia during cardiopulmonary bypass (CPB). These easy-to-use, non-invasive, real-time detection devices could serve as early warning systems for intraoperative hemodynamic compromise or as predictors for postoperative cognitive dysfunction [1] and could be used with an aim to avoid poor cerebral perfusion due to inappropriate cannulation, low perfusion pressure, anemia, and other adverse events that may result in perioperative neurological impairment during CPB [2,3,4,5].
However, it is common to encounter cases of critically low regional cerebral oxygen saturation (rSO2) during the induction of anesthesia, or low rSO2 values unresponsive to any intervention.
A previous retrospective evaluation of 223 cases of adult cardiac surgery with preoperative brain magnetic resonance imaging (MRI) has revealed that brain atrophy, poor left ventricular function, anemia, and hemodialysis were associated with low initial cerebral rSO2 values [6].
In this study, we prospectively evaluated differences in preoperative rSO2 values and other preoperative characteristics between two NIRS devices, including the INVOS 5100C (Medtronic, Minneapolis, MN, USA) and the FORE-SIGHT ELITE (CAS Medical Systems, Branford, CT, USA).
Materials and methods
From January 2017 to August 2017, a total of 96 consecutive patients underwent elective cardiac surgery at Kitasato University Hospital. Patients without preoperative brain MRI; and with a past medical history of acute cerebral infarction, previous intracranial hemorrhage or neurosurgery, off-pump coronary artery bypass surgery, and/or left ventricular assist devices were excluded. Finally, 80 patients were enrolled and analyzed in the study. In each patient, preoperative cerebral rSO2 values were consecutively recorded with two different devices: the INVOS 5100C, defined as “I value”, and the FORE-SIGHT ELITE, defined as “F value”. This research was conducted with the approval of the ethics committee of our university (approval number: B16–96). All patients gave their informed consent prior to their inclusion in the study.
Cerebral rSO2 monitoring
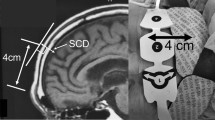
Under supine position, the arithmetic mean within 1 min at room air was recorded as cerebral rSO2. Optodes of each device were placed on the patient’s forehead, at 4 cm from the superciliary arch, to avoid the frontal sinus [7] (Fig. 1).
For optimal optode placement, the frontal sinus was avoided by affixing the optode on the forehead, 4 cm above the superciliary arch (i.e., the eyebrow). Scalp–cortex distance (SCD) was defined as the distance between the scalp surface and the frontal cerebral cortex in reference to a mid-sagittal plane of T1-weighted magnetic resonance image of the head
Scalp–cortex distance (SCD)
All patients were evaluated for the presence of cerebrovascular disease by preoperative brain MRI. SCD was measured on a T1-weighted MRI image as the distance from the surface of the scalp on the upper forehead, at 4 cm from the superciliary arch, to the frontal cerebral cortex (Fig. 1).
Data collection
Patient medical records were reviewed for preoperative clinical and demographic characteristics according to the hospital information system.
Data analysis
Continuous variables were presented as mean ± standard deviation. For each device, data were evaluated by univariate analysis to determine correlations between rSO2 values and each clinical variable. Multiple regression analysis by the least-squares method was performed on the data showing significant correlation coefficients in the univariate analysis. The ratio of rSO2 values measured by each device for each patient was determined as the F/I ratio, and univariate and multivariate analyses were conducted in a similar manner to investigate the correlation between differences in the values according to device selection and preoperative characteristics. Furthermore, patient characteristics for which the measured values between the two devices were equivalent, were obtained by receiver operating characteristic (ROC) analysis. On the basis of the similar concepts of bioequivalence for drugs [8], variables with an F/I value from 0.85 to 1.25 were assumed to be equivalent measured values between the two devices.
Differences with p < 0.05 were considered statistically significant. Statistical analyses were performed using JMP ver 12.0 (SAS Institute, Carey, NC, USA).
Results
Patients’ characteristics (Table 1)
Patients’ characteristics including age, sex, body surface area, preoperative left ventricular ejection fraction (LVEF), SCD, hemoglobin concentration (Hb), total bilirubin (T-bil), preoperative hemodialysis (HD), and other comorbidities are listed in Table 1.
rSO2 values
Mean cerebral rSO2 was significantly higher in the “F value”; [I value: 57.3 ± 8.5 (%), F value: 68.8 ± 4.5 (%); (p < 0.0001)] than in the “I value”. F/I ratio was 1.22 ± 0.23 (Table 1).
Univariate analysis
Univariate analysis was performed with rSO2 values and all characteristics measured by each device. In the “I value”, SCD, LVEF, Hb, HD, hypertension, diabetes mellitus (DM), and dyslipidemia (DL) were correlated with measured values. In the “F value”, HD and T-bil were correlated with the measured values. In the F/I value, SCD, LVEF, Hb, HD, DM, and DL were correlated with measured values (Table 2).
Multivariate analysis
Multiple regression analysis was performed using data that showed significant correlation coefficients in the univariate analysis. Results revealed that SCD, LVEF, and Hb remained significant factors in the “I value” and that HD remained a significant factor in the “F value”. Further, SCD, Hb, and HD remained significant factors in the F/I value (Table 3) (Fig. 2). HD cases were associated with 1.4-times higher F/I value than non-HD cases (HD: 1.60 ± 0.17, non-HD: 1.18 ± 0.18).
In the F/I ratio, scalp–cortex distance (SCD), hemoglobin concentration (Hb), and the presence or absence of hemodialysis (HD) remained significant factors in multiple regression analysis. A higher F/I ratio indicates a measurement discrepancy between the two devices. The F/I ratio for the non-HD cases was 1.18 ± 0.18 and that for HD cases was 1.60 ± 0.17
Evaluation of equality between devices
In multivariate analysis in which rSO2 values measured by the two devices were equivalent (F/I = 0.85–1.25), cutoff values of SCD, Hb, and the presence or absence of HD were determined by ROC analysis. The area under the curve was 0.82 (p < 0.001). Cutoff values for equivalence were SCD < 18.2 mm, Hb > 13.2 g/dl, and non-HD cases (Fig. 3).
Results of receiver operating characteristic analysis for the evaluation of equality between devices are shown. Measured rSO2 values of the two different devices were equivalent with the F/I value from 0.85 to 1.25. Area under the curve (AUC) was 0.82 (p < 0.001). Cutoff values for equivalence were a scalp–cortex distance of < 18.2 mm, a hemoglobin concentration of > 13.2 g/dl, and the absence of hemodialysis
Discussion
Perioperative central nervous system disorder in cardiac surgery is a prognostic factor [9]. Since Jöbsis et al. have reported their real-time, non-invasive monitoring method of tissue oxygen sufficiency using NIRS devices [10], clinical applications of such devices have expanded and there have been several reports on their use for the early detection of intraoperative cerebral ischemia or preoperative risk stratification [1, 11, 12]. Furthermore, the application of NIRS devices during cardiac surgery minimizes the risk of stroke and translates to the avoidance of prolonged ventilation, shorter ICU or hospital stay, and reduced medical cost [3, 11, 13,14,15]. Thus, the use of such devices can be recommended as an early warning system for ischemic event, which is one of the risks of cardiac surgery.
Most NIRS devices use a fixed reference ratio between the arterial and venous contribution to the signal, as 25/75 (%) or 30/70 (%), and measured values depend on consecutive changes in tissue oxygen consumption [16]. With the INVOS 5100C, the normal cerebral rSO2 value is 67 ± 9% and values of < 50 or > 85 in adult patients undergoing cardiac surgery are considered statistically abnormal [17].
Many NIRS devices interpret the difference in near-infrared light absorption between oxyhemoglobin and deoxyhemoglobin using a modified Beer–Lambert method, which has been used for the calculation of NIRS measurements and includes optical path length in its formula as a constant. Therefore, changes in optical path length would cause a discrepancy between actual and measured rSO2 values [18]. Furthermore, differences in the use of the wavelength of the spectrum and measuring algorithms among the devices result in variations in measured rSO2 values.
In this research, measured rSO2 levels were significantly higher for the “F value” than for the “I value”. SCD, Hb, and the presence or absence of HD significantly correlated with the F/I value. Furthermore, SCD, Hb, and LVEF affected rSO2 levels of the “I value”, and the presence or absence of HD affected rSO2 levels of the “F value”.
Effects of SCD
Near-infrared light passes through tissue, including bones. The skull bone or bone–dura interfaces directly under the optode, and to a lesser extent, the dura and the cerebrospinal fluid (CSF) layer have been reported to function as optical channels [19]. Reportedly, the thickness of the skull bone affects rSO2 measurement [18, 19]. Moreover, less near-infrared light returns to the detector in cases with thicker or large amount of CSF layer [18, 20]. Therefore, an SCD that is greater than the distal-sensing depth of the device can theoretically cause a low rSO2 measurement. In addition, the thickness of the CSF layer is included in the SCD. Furthermore, the distal sensing depth of each device, which is defined by optical path lengths and other device-oriented parameters, is approximately 20 mm for the INVOS 5100C and approximately 25 mm for the FORE-SIGHT ELITE. Thus, it is possible that the differences in distal sensing depth between the two devices widened their differential measurement due to increase in SCD.
Effects of hemoglobin concentration
Low Hb concentration increases the spaces between Hb molecules, which allow near-infrared light to travel a greater distance. Therefore, Hb concentration influences mean optical path lengths. A report wherein phase-resolved spectroscopy was used to emit near-infrared light with a modulated intensity and optical path length was measured from a phase shift has confirmed that optical path length increased as blood was diluted and as Hb concentration decreased during CPB [21]. However, as mentioned above, distal sensing depth affected by optical pathway depth is approximately 20 mm for the INVOS 5100C and 25 mm for the FORE-SIGHT ELITE. These data suggest that in this study, low Hb concentration caused a lower rSO2 level for the “I value” than for the “F value”.
Effects of hemodialysis
It has been reported that patients on HD have lower cerebral blood flow in the frontal lobe than patients with the end-stage renal disease who are not on HD [22]. Thus, the presence or absence of HD could affect low rSO2 values. Nevertheless, this study revealed increased cerebral blood flow in patients with the end-stage renal disease, including those not on HD, compared with healthy controls. However, the effect of hemodialysis remains ambiguous and requires further investigation.
Effects of left ventricular ejection fraction
Patients with reduced LVEF have insufficient oxygen delivery (DO2) [23]. Therefore, compared to patients with the same preoperative resting oxygen consumption (VO2), DO2 in their venous blood is lower, which results in lower rSO2 values. In this study, rSO2 values of each device were calculated using the difference between near-infrared light absorptions of oxyhemoglobin and deoxyhemoglobin according to their spectrum range (INVOS 5100C; two wavelengths, FORE-SIGHT ELITE; five wavelengths). However, emitted light can be diffused, absorbed, or scattered, and not all photons return to the detector. Therefore, a fixed mean optical pathway length may indicate that calculated changes in oxyhemoglobin concentrations can result in over- or under-estimation of measured values, depending on the conditions. The advantage of the FORE-SIGHT ELITE that uses additional three wavelengths is that it is possible to compensate for these signal losses and to account for interference from other factors, such as pigmentation [24]. Thus, we believe that the INVOS 5100C was affected by lower LVEF, which causes changes in oxyhemoglobin consumption under optodes.
Proposals
In cardiovascular surgeries, the risk of cerebral ischemia related to CPB is a matter of concern. Therefore, the early detection of desaturation is extremely important. Initially, as a first alert, the rSO2 value indicator will turn yellow at < 40% or at a 20% decline from the baseline value for the INVOS 5100C. These threshold values reflect the findings of previous studies [2, 3, 17]. In contrast, the FORE-SIGHT ELITE sets the first alert of rSO2 value indicator at absolute value of < 60% [25]. However, normal values are not clearly indicated.
From these findings, it is important to consider that rSO2 can be lower in patients on HD and in patients with anemic, reduced left ventricular function, or brain atrophy. In this study, we demonstrated that an SCD of > 18.2 mm and Hb concentration of < 13.2 g/dl were associated with a higher F/I ratio. Moreover, HD cases were associated with a 1.4-times higher F/I ratio than non-HD cases. High F/I ratio indicates a measurement discrepancy between the two devices. Notable, there was approximately 10% difference between preoperative values of the two devices that serve as indicators of brain ischemia in patients undergoing cardiovascular surgery. Considering that the measured value of the FORE-SIGHT ELITE is defined as the “absolute value” [24] and that a critical decline from the initial values has not been clearly defined for this device, the alert should be set at a lower fluctuation level of < 20% from the baseline value. In particular, inter-patient variations were greater in the INVOS 5100C than in the FORE-SIGHT ELITE, which were caused by variations in SCD, Hb, and LVEF. Thus, the INVOS 5100C can be considered to be more sensitive to changes in Hb and LVEF, which are prone to occur during cardiovascular surgeries. Moreover, in case of patients with preoperative brain MRI, distal sensing depths should be considered when making appropriate device selections: patients with a short SCD should be subjected to measurements with the INVOS 5100C, whereas patients with a long SCD should be subjected to measurements with the FORE-SIGHT ELITE. Optimal criteria for device selection confirming the avoidance of “patient-device mismatch” may help the precise detection of peripheral cerebral ischemic changes.
Study limitations
One of the limitations of this study is that its analysis was conducted on data representing a small sample size of ≤ 100 subjects in a single-center design. As for equivalency, it cannot be denied that the findings are unique to this limited number of cases. Moreover, it is possible that the inter-group differences in values measured during cardiac surgery are different from those measured preoperatively due to changes in Hb concentrations and perfusion caused by hemodilution during CPB, thus, warranting further investigation.
Conclusion
We prospectively examined differences in preoperative rSO2 values in adult cardiac surgeries measured using devices from two manufacturers and their correlations with various preoperative factors. rSO2 values were significantly higher for the “F value” than for the “I value”, and SCD, Hb, and the presence or absence of HD showed significant correlations with the F/I ratio and rSO2 values. In clinical practice, an appropriate device should be selected according to preoperative patient characteristics, and factors influencing rSO2 values should be taken into account to ensure the correct interpretation of measured values.
Change history
17 July 2018
In the original publication, the length unit of the SCD in Table 1 and Fig. 2 has been incorrectly published as cm. The correct length unit is mm.
References
Tsai HI, Chung PC, Lee CW, Yu HP. Cerebral perfusion monitoring in acute care surgery: current and perspective use. Expert Rev Med Devices. 2016;13:865–75.
Denault A, Deschamps A, Murkin JM. A proposed algorithm for the intraoperative use of cerebral near-infrared spectroscopy. Semin Cardiothorac Vasc Anesth. 2007;11:274–81.
Colak Z, Borojevic M, Bogovic A, Ivancan V, Biocina B, Majeric-Kogler V. Influence of intraoperative cerebral oximetry monitoring on neurocognitive function after coronary artery bypass surgery: a randomized, prospective study. Eur J Cardiothorac Surg. 2015;47:447–54.
Gottlieb EA, Fraser CD Jr, Andropoulos DB, Diaz LK. Bilateral monitoring of cerebral oxygen saturation results in recognition of aortic cannula malposition during pediatric congenital heart surgery. Paediatr Anaesth. 2006;16:787–9.
Chan SK, Underwood MJ, Ho AM, So JM, Ho AK, Wan IY, Wong RH. Cannula malposition during antegrade cerebral perfusion for aortic surgery: role of cerebral oximetry. Can J Anaesth. 2014;61:736–40.
Kobayashi K, Kitamura T, Kohira S, Torii S, Horai T, Hirata M, Mishima T, Sughimoto K, Ohkubo H, Irisawa Y, Matsushiro T, Hayashi H, Miyata Y, Tsuchida Y, Ohtomo N, Miyaji K. Factors associated with a low initial cerebral oxygen saturation value in patients undergoing cardiac surgery. J Artif Organs. 2017;20:110–6.
Gregory AJ, Hatem MA, Yee K, Grocott HP. Optimal placement of cerebral oximeter monitors to avoid the frontal sinus as determined by computed tomography. J Cardiothorac Vasc Anesth. 2016;30:127–33.
Food, Administration D, Center for Drug Evaluation and Research (CDER). Guidance for industry: bioavailability and bioequivalence studies for orally administered drug products—general considerations. Washington, DC: FDA; 2003.
Arrowsmith JE, Grocott HP, Reves JG, Newman MF. Central nervous system complications of cardiac surgery. Br J Anaesth. 2000;84:378–93.
Jöbsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science. 1977;198:1264–7.
Scheeren TW, Schober P, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput. 2012;26:279–87.
Heringlake M, Garbers C, Käbler JH, Anderson I, Heinze H, Schön J, Berger KU, Dibbelt L, Sievers HH, Hanke T. Preoperative cerebral oxygen saturation and clinical outcomes in cardiac surgery. Anesthesiology. 2011;114:58–69.
Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM 3rd, Rodriguez AL, Magovern CJ, Zaubler T, Freundlich K, Parr GV. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg. 2009;87:36–44.
Goldman S, Sutter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7:E376–81.
Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, Cleland A, Schaefer B, Irwin B, Fox S. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51–8.
Bickler PE, Feiner JR, Rollins MD. Factors affecting the performance of 5 cerebral oximeters during hypoxia in healthy volunteers. Anesth Analg. 2013;117:813–23.
Edmonds HL Jr, Ganzel BL, Austin EH 3rd. Cerebral oximetry for cardiac and vascular surgery. Semin Cardiothorac Vasc Anesth. 2004;8:147–66.
Yoshitani K, Kawaguchi M, Miura N, Okuno T, Kanoda T, Ohnishi Y, Kuro M. Effects of hemoglobin concentration, skull thickness, and the area of the cerebrospinal fluid layer on near-infrared spectroscopy measurements. Anesthesiology 2007;106:458–62.
Young AE, Germon TJ, Barnett NJ, Manara AR, Nelson RJ. Behaviour of near-infrared light in the adult human head: implications for clinical near-infrared spectroscopy. Br J Anaesth. 2000;84:38–42.
Okada E, Delpy DT. Near-infrared light propagation in an adult head model. II. effect of superficial tissue thickness on the sensitivity of the near-infrared spectroscopy signal. Appl Opt. 2003;42:2915–22.
Yoshitani K, Kawaguchi M, Okuno T, Kanoda T, Ohnishi Y, Kuro M, Nishizawa M. Measurements of optical pathlength using phase-resolved spectroscopy in patients undergoing cardiopulmonary bypass. Anesth Analg. 2007;104:341–6.
Jiang XL, Wen JQ, Zhang LJ, Zheng G, Li X, Zhang Z, Liu Y, Zheng LJ, Wu L, Chen HJ, Kong X, Luo S, Lu GM, Ji XM, Zhang ZJ. Cerebral blood flow changes in hemodialysis and peritoneal dialysis patients: an arterial-spin labeling MR imaging. Metab Brain Dis. 2016;31:929–36.
Oliveira MF, Zelt JT, Jones JH, Hirai DM, O’Donnell DE, Verges S, Neder JA. Does impaired O2 delivery during exercise accentuate central and peripheral fatigue in patients with coexistent COPD-CHF? Front Physiol. 2015. https://doi.org/10.3389/fphys.2014.00514.
Fischer GW, Silvay G. Cerebral oximetry in cardiac and major vascular surgery. HSR Proc Intensive Care Cardiovasc Anesth. 2010;2:249–56.
Fischer GW, Lin HM, Krol M, Galati MF, Di Luozzo G, Griepp RB, Reich DL. Noninvasive cerebral oxygenation may predict outcome in patients undergoing aortic arch surgery. J Thorac Cardiovasc Surg. 2011;141:815–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kobayashi, K., Kitamura, T., Kohira, S. et al. Cerebral oximetry for cardiac surgery: a preoperative comparison of device characteristics and pitfalls in interpretation. J Artif Organs 21, 412–418 (2018). https://doi.org/10.1007/s10047-018-1052-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-018-1052-3