Abstract
There is a need for more information on the quality of life (QoL) in patients undergoing chemotherapy. We wanted to investigate the perception of health status in colon cancer patients before, 3 and 6 months after chemotherapy. A secondary purpose was to assess the different perceptions of QoL between men and women during and after adjuvant or palliative therapy. We investigated 100 patients throughout chemotherapy for colon cancer. Data were collected through the SF-36 questionnaire. The score of all variables analyzed in the study group was lower than in the control group, which indicates a lower performance status, more marked in the female sex. Patients were then subdivided by the state of disease (localized or metastatic) and the variables, were evaluated before, 3 and 6 months after therapy. In patients treated with adjuvant treatment, there was a worsening of the performance status, followed by an increase after 6 months. We found that after 3 months of therapy, affected male patients perceived more limitations in carrying out their work, other daily activities and social relationships, owing to both their emotional state and their physical health. In metastatic patients the values of the eight variables decreased dramatically after 6 months, indicating a worsening of the QoL. In patients who received adjuvant treatment there was a certain worsening of the health status at 3 months, followed by a general improvement after 6 months. This improvement was not observed in patients undergoing palliative therapy. Several differences were observed between men and women in performance status after treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quality of life (QoL) in cancer patients received considerable attention in the last two decades. The phrase, ‘health-related quality of life (HRQoL)’ is a multidimensional concept that includes perceptions related to physical, psychological status of the individual and the subjective perception of position in social context of their relationships [1–6].
A recent study suggests that interventions to improve colorectal cancer patients’ QoL may be more effective if they target psychosocial aspects, symptoms, and lifestyle variables in an integrated approach [7]. The results of other studies demonstrate that cancer patients undergoing chemotherapy show a worsening of their physical capacity (muscle strength, aerobic capacity), physical activity level and of general well-being. Physical programs that combine high- and low-intensity activities may be used as complementary support for cancer patients undergoing chemotherapy [8].
The increasing importance given to QoL plays an important role in the approach to cancer patients. Fatigue—which is a non-specific, multidimensional condition including psychological, social, and physiological aspects—is increasingly recognized as the most common and frequent side effect in colon cancer patients during their treatment (surgery, radiation and/or chemotherapy) [9]. Control of pain and fatigue during oncological diseases has been the object of many clinical trials, since these diseases have a significant impact on mobility, independence and mental state of patients and his/her family [10].
The aim of our study was to compare the impact of the ‘experience cancer’ on physical, mental and general health of colon cancer patients before medical treatment, and 3 and 6 months after medical treatment. Moreover, we wanted to assess the different perceptions of QoL between men and women during and after adjuvant and palliative therapy.
Materials and methods
Study group
This is an observational investigation. A total of 130 patients with colon malignancies were identified through the Oncology Center of Modena between 2008 and 2012 (all stage TNM II, III and IV individuals without relevant comorbidities). Of the consecutive 130 patients, 100 (70 %) accepted to participate, while 10 died during the study; 5 were not interested in the project and 15 refused to collaborate because of their illness or comorbidities. The subjects were informed about the project with a letter requesting them to participate in the study and to be available for an interview.
At the time of the interview we provided detailed information on the design, purposes and duration of the study. For all participants we collected clinical data by means of questionnaires. As a comparison group, we chose healthy men and women of the same age as patients to whom the SF-36 questionnaire was administered.
As a matter of fact the optimal time for assessing patients and evaluating their clinical status may depend on many factors, such as duration of treatment, type of drug, type of patient, age of patient and comorbidities. Three and six months were chosen rather arbitrarily; however, we reasoned that after these periods patients should be able to feel and refer changes in their physical status and QoL [11].
Treatment
This study was conducted at the Division of Internal Medicine 1 and at Oncology Center of the University of Modena and Reggio Emilia. Patients were interviewed before starting chemotherapy, then at 3 months (during therapy) and at 6 months (end of therapy for patients undergoing adjuvant therapy). Patients with stage II-III disease are usually treated—when possible, owing to comorbidities—with adjuvant chemotherapy some 1–2 months after surgery. In our patients, the most common regimen included Fluoropyrimidines including 5-Fluorouracyl (5-FU), Leucovorin, with or without Oxalyplatin or Capecitabine. For stage IV disease (advanced disease, often inoperable), first-line chemotherapy included 5-FU+ Leucovorin or Irinotecan with or without monoclonal antibodies [12, 13].
Criteria for selection of subjects
The criteria for admission to the study were the following:
-
Age at diagnosis between 26 and 75 years;
-
Pathological Stage TNM II, III and IV (corresponding to Dukes’ B, C and D);
-
Selection period: April 2008–April 2012;
-
Ability to understand properly the questionnaire concerning QoL;
-
In all patients selected in the study, adjuvant chemotherapy was administered for 6 months. Patients with advanced disease received a frontline therapy for 6 months; afterwards the treatment diverged consistently from patient to patient.
Health assessment (SF-36 questionnaire) [14]
Data were collected through the Short-Form (SF-36) questionnaire [14]. In addition, the interview included questions concerning side effects related to chemotherapy.
SF-36 is a generic multidimensional questionnaire consisting of 36 items. The SF-36 comprises 36 questions measuring eight health scales: physical functioning (limitations to everyday activities), role limitations due to physical problems (the degree by which physical health interferes with work and other activities), bodily pain, general health, vitality, social functioning (interference with social activities), role limitations due to emotional problems (the degree in which emotional problems interfere with work or other activities) and mental health (sense of nervousness and depression). According to standard scoring procedures, the sub-categories were linearly converted to a 0–100 scale, with higher scores indicating better functioning and lower scores worse performance (Table 1).
Control group
The control group was a representative sample of healthy Italian adults, selected by the Research Institute of Statistics and Analysis of Public Opinion (Milan). Scores for all scales were transformed to a score where 0 represents worse health and 100 indicates good health [15].
Statistical analysis
The raw data were analyzed using SPSS version 19.0. Descriptive statistics included means, ranges and standard deviations for demographics, medical variables, physical activity, diet behavior, QoL, and social support. Correlations and analyses of variance examined the relationship between sociodemographic data, clinical data and QoL. The significance of the QoL and other scale changes between the baseline and after treatment were analyzed using paired t test. Mean scores of the SF-36 scales were compared with previously published data for the general population [16] after matching for sex. The rationale for this adjustment is based on previous work showing the importance of such approach when reference data for HRQoL comparisons are used [17]. The weighted means were compared and interpreted taking into account previous experience indicating that a difference of at least 10 points can be considered to be clinically meaningful [18]. Student’s t tests were performed (after checking for a normal distribution of the scores) to verify the influence of treatment and patients’ characteristics for each of the selected HRQoL domains (p value <0.05 was considered as statistical significant).
Results
Patient characteristics
During the study period, 100 patients affected by colon cancer were included. The patients’ mean age at diagnosis was 59.9 ± 1.3 years (range 26–79). There were 46 men and 54 women. Twenty-eight patients were in Dukes B stage, 42 in Dukes C, and 30 showed metastatic disease (Dukes “D”). Twenty-two percent of tumors were localized in the sigmoid, 22 % in the ascending colon, 18 % in the transverse colon, 23 % in the cecum, 7 % in the descending colon, 5 % in the flexures and, 3 % in the rectum sigmoid junction.
Health assessment
The results were expressed as average values included between the lower and the higher scores of the eight domains evaluated by the SF-36.
We compared the SF-36 summary scores of patients to the Italian reference data, divided by sex. There were no significant differences between the SF-36 scores obtained at the beginning of chemotherapy for colon cancer and the same scores of a sample of the general population of a similar age.
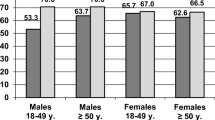
In study group, the eight analyzed variables were lower than in the control group, which indicates a lower performance status, more marked in the female sex. Among the variables, physical role (perception of physical capacities) was reduced in both sexes (through not significantly) when compared to the reference population (Figs. 1, 2).
Figures 3 and 4 represent a comparison of SF-36 scores between men and women subdivided by type of chemotherapy (adjuvant and palliative) at the beginning, 3 and 6 months after treatment.
Status of disease
In patients with localized disease, we observed a reduction of all items at 3 months (indicating worsening of the performance status), followed by an increase after 6 months.
In men, Physical Role score (perception of physical capacities) was significantly different (p < 0.05) at the end of the therapy; in other words, men had more difficulties in carrying out daily activities (Fig. 3). In women, there was a statistically significant difference (p < 0.05) of Bodily Pain score (perception of physical pain) at the end of therapy; i.e. the perception of physical pain was increased (Fig. 4). As expected, the frequency of symptoms in patients receiving adjuvant chemotherapy increased after 3 months and then decreased after 6 months of therapy. In addition, 30 % of these patients reported weight loss at the end of therapy. The response of patients during adjuvant treatment was as follows: 50 patients (72 %) had complete response to chemotherapy, 10 (14 %) were in stable condition and 10 (14 %) had evidence of disease progression.
Regarding patients with metastasis, the eight scores of the SF-36 decreased dramatically after 6 months (indicating a worsening of QoL). In both sexes, we observed a statistically significant reduction (p < 0.05) of Mental Health scores (perception of fear, depression, anger and nervousness). In men, however, there was a significant difference (p < 0.05) of Bodily Pain score (perception of physical pain) at the end of therapy, with an increase in the perception of physical pain (Fig. 5). In women, Social Relationship score was significantly decreased (p < 0.05) after 6 months; as a consequence of this, women perceived more limitation in social relationships (Fig. 6). In patients with metastasis, after 6 months all side effects—and in particular fatigue, nausea, vomiting and weight loss—increased in frequency. The behavior of patients during palliative treatment was as follows: 20 subjects (67 %) had evidence of disease progression, 10 (33 %) had a partial response to chemotherapy.
Discussion
The results of the present study can be summarized as follows. First, the control group showed better scores of SF-36 compared to our patients before chemotherapy. Second, several factors—including social relationships, physical activity, work activity—can be affected by the colon cancer event in a given individual, with some differences between men and women. Third, QoL in these patients can provide useful information concerning physical and emotional experiences.
In general terms, the patients who participated in the study were satisfied with the type of investigation and the way it was conducted. However, several patients expressed their concern when answering some questions, since these were sometimes perceived as being too personal and, consequently, affecting their privacy.
Sultan et al. [19] found that provision of emotional and instrumental support resulted in an improved QoL during and after the ‘cancer event’. Thus, these investigations lend some support to the close relationship between QoL and social relationships, as shown in the present study.
Moreover, perception of QoL during treatment, both adjuvant and palliative, was different between men and women. Patients undergoing adjuvant therapy obtained, after 6 months, a higher score in all eight scales compared with before therapy status (physical activity, physical role and emotional state, vitality, mental health, social activity, bodily pain and general health). Men had more difficulties in carrying out work activities, and felt more limited at the end of therapy. In contrast, women felt healthier than men at the end of treatment, though they perceived more bodily pain.
Patients with metastasis obtained, after 6 months, lower scores in all eight scales. Both men and women defined themselves as mentally vulnerable. Men perceived more often physical pain, while women had more difficulties in social relationships.
It has been suggested that an increase of physical activity, such as walking, might be of benefit in patients with colon malignancies and other neoplasms [20–24]. Studies in larger samples of colon cancer patients during chemotherapy are needed to confirm our preliminary observation and to identify factors related to QoL that are specific for this population, especially during palliative treatment [25].
The ‘cancer experience’ includes cognitive changes during and following chemotherapy, a fact which is well known by health care professionals. Numerous studies have been designed to investigate the incidence, causal mechanisms, and interventions to prevent or mitigate the impact of cancer and chemotherapy on cognition [26, 27]. Fewer studies, however, have been conducted to describe the experience of cancer-related cognitive changes from the patients’ perspective [28].
In conclusion, in patients who received adjuvant treatment there was a certain worsening of the health status at 3 months, followed by a general improvement after 6 months. This improvement was not observed in patients undergoing palliative therapy. Several differences were observed between men and women about performance status. Women undergoing adjuvant chemotherapy appeared to perceive more bodily pain at the end of therapy than men, whereas the opposite was true for patients with metastatic tumors.
References
Demark-Wahnfried W, Jones LW (2008) Promoting a healthy lifestyle among cancer survivors. Hematol Oncol Clin North Am 22:319–342
Blanchard CM, Stein KD, Baker F, Dent MF, Denniston MM, Courneya KS, Nehl E (2004) Association between current lifestyle behaviours and health-related quality of life in breast, colon, and prostate cancer survivors. Psychol Health 19:1–13
Blanchard CM, Courneya KS, Stein K (2008) Cancer survivors’ adherence to lifestyle behaviour recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol 26:2198–2204
James AS, Campbell MK, DeVellis B, Reedy J, Carr C, Sandler RS (2006) Health behavior correlates among colon cancer survivors: NC STRIDES baseline results. Am J Health Behav 30:720–730
Lynch BM, Cerin E, Owen N, Aitken JF (2007) Associations of leisure time physical activity with quality of life in a large, population-based sample of colon cancer survivors. Cancer Causes Control 18:735–742
Peddle CJ, Au HJ, Courneya KS (2008) Associations between exercise, quality of life, and fatigue in colon cancer survivors. Dis Colon Rectum 51:1242–1248
Steginga SK, Lynch BM, Hawkes A, Dunn J, Aitken J (2009) Antecedents of domain-specific quality of life after colon cancer. Psychooncology 18:216–220
Ademsen L, Midtgaard J, Rorth M et al (2003) Feasibility, physical capacity, and health benefits of a multidimensional exercise program for cancer patients undergoing chemotherapy. Support Care Cancer 11:707–716
Kubista E (2001) Breast cancer: figures and facts. Wien Med Wochenschr 151:548–551
Stone PC, Minton O (2008) Cancer-related fatigue. Eur J Cancer 44(8):1097–1104
Theodoropoulos GE, Karantanos T, Stamopoulos P, Zografos G (2013) Prospective evaluation of health-related quality of life after laparoscopic colectomy for cancer. Tech Coloproctol 17(1):27–38
Chung KY, Saltz LB (2007) Adjuvant therapy of colon cancer: current status and future directions. Cancer J 13(3):192–197
Yau T, Chan P, Ching Chan Y (2008) Review article: current management of metastatic colorectal cancer—the evolving impact of targeted drug therapies. Aliment Pharmacol Ther 27:997–1005
Apolone G, Mosconi P (1998) The Italian SF-36 Health Survey: translation, validation and norming. J Clin Epidemiol 51(11):1025–1036
Brazier JE, Harper R, Jones NMB, O’Cathain A, Thomas KJ, Usherwood T, Westlake L (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BJM 305:18
Osoba D, Rodrigues G, Myles J et al (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16:139–144
Hjermstad MJ, Fayers PM, Bjordal K et al (1998) Using reference data on quality of life—the importance of adjusting for age and gender, exemplified by the EORTC QLQ-C30 (+3). Eur J Cancer 34:1381–1389
Pucciarelli S, Del Bianco P, Toppan P (2008) Health-related quality of life outcomes in disease-free survivors of mid-low rectal cancer after curative surgery. Ann Surg Oncol 15(7):1846–1854
Sultan S, Fisher DA, Voils CI, Kinney AY, Sandler RS, Provenzale D (2004) Impact of functional support on health-related quality of life in patients with colon cancer. Cancer 101:2737–2743
Ware JE Jr (1993) Measuring patients’ views: the optimum outcome measure. BMJ 306:1429–1430
Giovannucci E et al (1995) Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Int Med 122:327
Slattery ML et al (2003) Physical activity and colon cancer. Am J Epidemiol 158:214
Hou L (2004) Commuting physical activity and risk of colon cancer in Shangai, China. Am J Epidemiol 160:860
Slattery ML et al (2004) Associations between BMI, energy intake, energy expenditure, VDR genotype and colon and rectal cancers (United States). Cancer Causes Control 15(9):863–872
Stephenson LE, Bebb DG, Reimer RA et al (2009) Physical activity and diet behaviour in colorectal cancer patients receiving chemotherapy: associations with quality of life. BMC Gastroenterol 9:60
Hung HC, Chien TW, Tsay SL, Hang HM, Liang SY (2013) Patient and clinical variables account for changes in health- related quality of life and symptom burden as treatment outcomes in colorectal cancer: a longitudinal study. Asian Pac J Cancer Prev 14(3):1905–1909
Yokoyama T, Kurokawa Y, Kani R et al (2012) Assessment of health-related quality of life in cancer outpatients treated with chemotherapy. Gan To Kagaku Ryoho 39(3):409–414
Myers JS (2013) Cancer- and chemotherapy-related cognitive changes: the patient experience. Semin Oncol Nurs 29(4):300–307
Acknowledgments
The authors wish to thank the Consiglio Nazionale della Ricerca (CNR), The Italian Association for Cancer Research (AIRC), and The Lega Italiana Lotta Tumori (LILT), for generous support during the study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Domati, F., Luppi, G., Reggiani-Bonetti, L. et al. The perception of health-related quality of life in colon cancer patients during chemotherapy: differences between men and women. Intern Emerg Med 10, 423–429 (2015). https://doi.org/10.1007/s11739-014-1174-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-014-1174-4