Abstract
Objective
To examine the associations between physical activity and quality of life for colorectal cancer survivors; and to describe the associations of medical and sociodemographic attributes with overall quality of life, and their moderating effects on the relationships between physical activity and quality of life.
Methods
Telephone interviews were conducted with 1,996 colorectal cancer survivors recruited through the Queensland Cancer Registry. Data were collected on current quality of life; leisure-time physical activity pre- and post-diagnosis; cancer treatment and side-effects; and general sociodemographic attributes. Hierarchical generalized linear models identified variables significantly associated with quality of life.
Results
After controlling for sociodemographic variables, disease-specific variables, treatment side-effects, and pre-diagnosis leisure-time physical activity, there were significant differences in quality of life scores by post-diagnosis physical activity category. Compared to participants who were inactive after their diagnosis, those who were sufficiently active had a 17.0% higher total quality of life score. Physical activity also had a significant independent positive association with the physical well-being, functional well-being, and additional concerns subscales of the FACT-C.
Conclusions
Our findings demonstrate that quite modest changes in leisure-time physical activity are associated with quality of life. Colorectal cancer survivors may benefit from a more active lifestyle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past 20 years, there has been a rapid growth in research investigating relationships between physical activity and improved quality of life outcomes for cancer survivors. Some 40 reports of randomized, controlled trials have been published, and there have been a number of reviews on the topic [1–5]. However, there have been few well-designed observational studies conducted, to determine the natural patterns of physical activity among representative samples of cancer survivors, and to identify the associations of physical activity with quality of life.
Observational studies provide opportunities to use large, population-based samples; this is in contrast to intervention studies, in which participants with advanced disease or significant co-morbidities are usually excluded [6–10]. While observational studies cannot establish causal relationships, their findings are important for generating hypotheses to be tested by subsequent intervention studies, and identifying information that should be gathered about exposures and outcomes. Observational studies with large, population-based samples can provide representative data on the full range of variation in the attributes of interest.
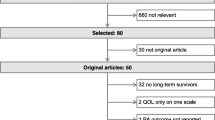
We have identified only 13 observational studies dealing specifically with the relationships between physical activity and quality of life among cancer survivors [11–23], all of which have reported positive associations. These descriptive studies have varied in size and scope. Five had sample sizes of less than 100 [15, 17, 19, 21, 23], giving less precision for estimates of effects; four had an overall response rate of less than 50% [15, 16, 18, 20]; and seven used convenience samples [11, 14, 15, 17, 19, 21, 23]. Thus, the representativeness of their findings is limited. Breast cancer survivors were the most commonly studied cancer group [14, 19, 21]. There were two studies of colorectal cancer survivors [13, 15], and one each for endometrial [16], multiple myeloma [18], non-Hodgkin’s lymphoma [20], and head and neck cancers [23]. Four sampled a mix of cancer survivors [11, 12, 17, 22]. There are different patient demographic profiles, disease-related factors and treatment regimes between cancer populations that may alter associations between physical activity and quality of life [5, 24]. It is therefore difficult to interpret the findings of these mixed-diagnosis studies.
While each of the observational studies conducted to date have reported some positive associations between physical activity and quality of life, these associations are indicative only, given the methodological shortcomings of the studies. There is a need for descriptive studies using large representative samples of survivors of particular cancers, to provide data on the associations between physical activity and quality of life, and how these associations may vary across the range of relevant personal and behavioral attributes. Such data can provide evidence to inform the development of physical activity interventions for cancer survivors.
We examined the associations of pre-to-post diagnosis changes in levels of leisure-time physical activity with quality of life in a large, population-based sample of colorectal cancer survivors. We also examined the associations of medical and sociodemographic attributes with overall quality of life, and their moderating effects on the relationships between physical activity and quality of life.
Materials and methods
Study participants
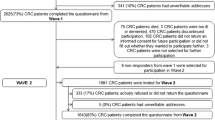
Data were collect as part of the Colorectal Cancer and Quality of Life Study, the methods of which are described in detail elsewhere [25]. Briefly, the study is a population-based longitudinal study of the predictors of quality of life up to five years after diagnosis. Study participants had a first primary diagnosis of colorectal cancer between 1 January 2003 and 31 December 2004, and were between the ages of 20 and 80 years at the time of diagnosis. The treating doctors of 3,626 eligible patients were approached in writing for permission to contact their patients regarding the study. Letters were re-sent to non-responding doctors two weeks after the initial mailing, and doctors were then telephoned on a weekly basis until an answer was received. The 3,182 patients for whom consent was received were then mailed information about the study and a consent form. Those who did not respond were sent a second letter two weeks later, and non-responders received two follow-up telephone calls and a final mailing. A flow diagram describing recruitment to, and participation in, the study is presented in Fig. 1. The University of Queensland’s Behavioral and Social Science Ethical Review Committee approved the study’s procedures.
Measures
Data were collected by trained interviewers through a computer-assisted telephone interview. Current demographic information, including place of residence, marital status, educational attainment, and height and pre-diagnosis body mass (to determine body mass index; BMI) was self-reported at interview, as was treatment type. Age, sex, and site of disease were collected from pathology reports held within the Queensland Cancer Registry. Stage of disease was ascertained from participants’ surgeons for 64.4% of the sample. We supplemented these data with information on stage collected from participants’ medical oncologists and general practitioners, giving us stage of disease for a total of 94.0% of participants. Stage was gathered from pathology reports for an additional 2%, leaving only 4.0% of participants without stage data.
Physical activity was assessed using questions based on the Active Australia Survey, the standard instrument used to monitor physical activity participation in the Australian adult population [26, 27]. Participants were asked to report the amount of time they spent each week: walking for transport or recreation; in other moderate-intensity physical activity (e.g., gentle swimming, social tennis, golf); and in vigorous-intensity physical activity (e.g., jogging, cycling, aerobics, competitive tennis). Total times of more than 840 min (14 h) per week for any given activity category were re-coded to 840 min, to reduce errors from over-reporting [26]. Total leisure-time physical activity was calculated by adding together the time spent in each activity category. Vigorous activity was double-weighted to account for additional energy expenditure, using the standard Active Australia method [26]. Current Australian public-health guidelines advocate achieving the equivalent of 30 min of moderate-intensity physical activity on most, if not all, days of the week [28]. This is equivalent to accumulating 150 min of moderate-intensity activity per week (less if participating in vigorous-intensity activity). Based on these guidelines, participants were categorized as being either inactive (0 min per week), insufficiently active (1–149 min per week), or sufficiently active (150 min or more per week).
The Functional Assessment of Cancer Therapy – Colorectal (FACT-C; Version 4) is a 36-item quality of life questionnaire with five subscales: physical well-being; social/family well-being; emotional well-being; functional well-being; and colorectal cancer-specific additional concerns. Patients are asked to rate how they have felt over the past seven days, on a scale of 0 (‘not at all’) to 4 (‘very much’). Individual scores are compiled according to a standardized algorithm, so that each subscale is scored and then summed to provide an overall quality of life score. The overall quality of life score can range from 0 to 136 (two items relevant to stoma patients only are not included in the score), with higher scores indicating better quality of life. Each subscale has a maximum score of 28, except for the emotional well-being subscale, which has a maximum score of 24. The FACT-C has been shown to be a valid and reliable measure, and sensitive to changes in functional status [29]. A difference between-group scores on the FACT-C within the range of 5–8 points, accounting for differences across samples and settings, is defined as being clinically important [30].
Statistical analyses
To examine the representativeness of our sample, we compared participants to those who were eligible but did not complete the telephone interview, across sex, age, place of residence, site, and stage (variables available to us through the Queensland Cancer Registry), using χ2 tests.
Descriptive statistics were used to describe overall quality of life, and the subscales of the FACT-C. Means and standard deviations were computed, and as quality of life data tend to be skewed, we also calculated medians and inter quartile ranges for these scales.
We used hierarchical generalized linear models to identify variables significantly associated with quality of life. The quality of life data were skewed to the left, therefore we reverse-scored these data and used the gamma variance function (and the log-link function) in our modeling.
Using the overall FACT-C score as the criterion variable, predictor variables were entered in blocks specified a priori: sociodemographic variables; disease-specific variables; treatment side-effects; pre-diagnosis physical activity; and then post-diagnosis physical activity. This formed our main effects model. We then repeated the same model, but added an interaction term for pre-diagnosis and post-diagnosis physical activity. We included variables in our pre-determined sociodemographic, disease-specific, and treatment side-effects blocks if they had a bivariate association with the criterion variable of p < 0.20.
The same modeling procedures were repeated using the five different subscales of the FACT-C as the criterion variables.
Results
There were 1,966 participants who completed the telephone interview (57.4% overall response rate). About 80% of participants were interviewed within six months of their diagnosis (mean = 4.5 months, standard deviation = 1.5 months).
Our comparison of study participants to non-participants (see Table 1), using the limited data available to us for non-participants, found no difference in the sex distribution between participants and non-participants. However, our sample did under-represent older (aged 70–80 years) colorectal cancer survivors, those with rectal cancer and those with more advanced disease (χ2 test, p < 0.05 for each).
Based upon the pre-diagnosis amount of physical activity reported, 53% of participants (55% of men; 51% of women) were categorized as sufficiently active, that is, they had accumulated at least 150 min of moderate-intensity activity or 90 min of vigorous-intensity activity per week, or an equivalent combination of moderate and vigorous activity. Fewer (32% of participants; 36% men and 28% women) achieved 150 min of physical activity per week after their diagnosis. Quality of life scores ranged from 26 to 136; distributions are described in Table 2.
Regression models did not yield significant pre- by post-diagnosis physical activity level interaction effects on quality of life scores. Hence, we present the main effect models in Table 3. With regard to the overall FACT-C model, each block entered into the model was significant, except for pre-diagnosis physical activity. However, it was important to control for previous levels of physical activity in order to assess the statistical effects of changes in physical activity levels from pre- to post-diagnosis on perceived quality of life. The factors that were most different to their expected values were: marital status (those that were married or in a de facto relationship had on average 19.1% higher FACT-C scores than those who had never been married); stoma (those who did not have a stoma created had 16.0% higher FACT-C scores than those who had had a permanent stoma created); and each of the key symptoms. Those who did not experience fatigue had FACT-C scores that were 64.4% higher than those who did; those who did not experience nausea had quality of life scores 41.0% higher than those who did; and those who did not have problems with faecal control had FACT-C scores 24.7% higher than those who did.
Our main variable block of interest was post-diagnosis physical activity. After controlling for sociodemographic variables, disease-specific variables, treatment side-effects, and pre-diagnosis physical activity, we found that there was a significant difference in quality of life scores between those who, at post-diagnosis, were inactive, insufficiently active, and sufficiently active. Post-diagnosis physical activity had a significant independent positive effect on quality of life, as operationalised by the FACT-C score. After controlling for the level of pre-diagnosis physical activity, those who were sufficiently active post-diagnosis had a 17.0% higher FACT-C score, and those who were insufficiently active post-diagnosis had a 9.1% higher FACT-C score, than those who were inactive post-diagnosis.
For brevity, and given that our main aim was to evaluate the associations between physical activity and quality of life, in Table 4 we present only the physical activity blocks (pre- and post-diagnosis) from the hierarchical generalized linear models (main effects) we created for each of the FACT-C subscales. After adjusting for sociodemographic variables, disease-specific variables, treatment side-effects, and pre-diagnosis physical activity, post-diagnosis physical activity was significantly associated with the physical well-being, functional well-being, and with the additional concerns subscales. After adjusting for pre-diagnosis physical activity, compared to those who were inactive after their diagnosis, participants who were sufficiently active post-diagnosis had: 22.9% higher physical well-being scores; 26.7% higher functional well-being scores; and they scored 14.7% higher on the additional concerns (colorectal cancer-specific) scale.
Discussion
We found strong positive associations between leisure-time physical activity and quality of life in a large population-based sample of colorectal cancer survivors. Participants who met the current Australian public-health guidelines on physical activity (achieving the equivalent of 150 min of moderate-intensity activity or more per week) had significantly higher overall quality of life scores, and higher scores on the physical well-being, functional well-being, and additional concern subscales of the FACT-C. The strong association between leisure-time physical activity and functional well-being is of particular note, as decline in functional capacity is common among cancer survivors [31]. Our results showed that, after controlling for pre-diagnosis physical activity, colorectal cancer survivors who were physically active following their diagnosis had 26.7% higher functional well-being than those who were inactive.
The 17.0% higher overall quality of life score for people who were physically active post-diagnosis, in comparison to those who were inactive post-diagnosis, equates to a difference that exceeds the minimally important difference for this scale. Based on the full range of FACT-C scores, the differences could have ranged from four to 23 points, with an average difference around 19 points. Changes between five and eight points are considered the smallest changes of clinical significance for the FACT-C [30].
To date, studies investigating the relationship between physical activity and quality of life have generally reported that there are positive associations. Broadly, the findings of these studies suggest that participants who met physical activity recommendations (the relevant amounts varied between studies, but were generally equivalent to 150 min of moderate-intensity activity per week) had higher quality of life scores. A number of the studies described physical activity at different time points across the cancer experience, and found that physical activity levels tended to decrease following diagnosis, and then increase following treatment; however, they did not always return to pre-diagnosis levels. This pattern of activity change seems to be consistent across cancer groups [11, 13–16, 18, 20]. Pattern of change in activity has also been associated with quality of life following diagnosis [11, 13–15].
The Colorectal Cancer and Quality of Life Study is the most comprehensive study to describe the associations between physical activity and quality of life among colorectal cancer survivors. The large, population-based sample, and use of well-tested measures of leisure-time physical activity and quality of life, are strengths of the study. However, by assessing only leisure-time physical activity, patterns of physical activity may have been misclassified. The inclusion of occupational and domestic activities may have changed the study outcomes.
Self-reported physical activity data are likely to be limited somewhat by recall error, perceived social desirability and other biases [32, 33]. Other limitations of our study include the retrospective assessment of pre-diagnosis physical activity, and the possible cross-contamination of responses due to assessing pre- and post-diagnosis physical activity during the same interview. Also, as 42.6% of the eligible sample did not complete the telephone interview, due to death, non-consent or inability to be contacted, some sample bias would exist. The under-representation of older participants, and those with rectal cancer and later stage disease supports this concern.
Due to the cross-sectional nature of these data, it is unclear whether the positive association between physical activity and quality of life is a causal one. Participants with compromised quality of life may be less able or inclined to engage in physical activity, compared to participants with higher levels of quality of life. However, intervention trials have shown significant benefits for cancer survivors participating in structured physical activity programs [8, 34, 35]. It is therefore likely that quality of life variance between physically active and inactive patients is a combination of both factors.
Our findings showed that quite modest changes in physical activity were associated with quality of life; for example, there were improvements among those who moved from the inactive category pre-diagnosis to the insufficiently active category post-diagnosis. This may have implications for those who are unable to take part in structured exercise programs: simple advice on increasing moderate physical activity, such as walking, is likely to be beneficial for this group.
Further research is needed to establish whether the physical activity and quality of life are consistent, or if they are variable over time. Longitudinal data would help to assess whether physical activity has a sustained effect on quality of life. There have been no prospective, observational studies of physical activity and quality of life among colorectal cancer survivors to date. The longest published, prospective study in this area followed 69 breast cancer survivors over 12 months. This study found that physical activity levels did not change, but that quality of life did improve with time. Physical activity was associated with improved physical functioning, but not overall mood or cancer-related symptoms [19].
The long-term health issues specific to cancer survivors are emerging as a public-health concern. While some ongoing morbidity is inevitable in this growing population, physical activity has potential to increase quality of life and functional capacity, and decrease co morbid conditions among cancer survivors.
References
Galvao D, Newton R (2005) Review of exercise intervention studies in cancer patients. J Clin Oncol 23:899–909
Knols R, Aaronson N, Uebelhart D, Fransen J, Aufdemkampe G (2005) Physical exercise in cancer patients during and after medical treatment: a systematic review of randomized and controlled clinical trials. J Clin Oncol 23:3830–3842
Oldervoll L, Kaasa S, Hjermstad M, Lund J, Loge J (2004) Physical exercise results in the improved subjective well-being of a few or is effective rehabilitation for all cancer patients? Eur J Cancer 40:951–962
Schmitz K, Holtzman J, Courneya K, Masse L, Duval S, Kane R (2005) Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidem Biomar 14(7):1588–1595
Stevinson C, Lawlor D, Fox K (2004) Exercise interventions for cancer patients: systematic review of controlled trials. Cancer Cause Control 15:1035–1056
Mock V, Pickett M, Ropka M, Muscari Lin E, Stewart K, Rhodes V et al (2001) Fatigue and quality of life outcomes of exercise during cancer treatment. Cancer Pract 9(3):119–127
Segal R, Evans W, Jonhson D, Smith J, Colletta S, Gayton J et al (2001) Structured exercise improves physical functioning in women with stages I and II breast cancer: results of a randomized controlled trial. J Clin Oncol 19(3):657–665
Courneya K, Mackey J, Bell G, Jones L, Field C, Fairey A (2003) Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulonary and quality of life outcomes. J Clin Oncol 21(9):1660–1668
Daley A, Mutrie N, Crank H, Coleman R, Saxton J (2004) Exercise therapy in women who have had breast cancer: design of the Sheffield women’s exercise and well-being project. Health Ed Res 19(6):686–697
Rabin C, Pinto B, Trunzo J, Frierson G, Bucknam L (2006) Physical activity among breast cancer survivors: regular exercisers vs participants in a physical activity intervention. Psycho-oncol 15(4):344–354
Blanchard C, Baker F, Denniston M, Courneya K, Hann D, Gesme D et al (2003) Is absolute amount or change in exercise more associated with quality of life in adult cancer survivors? Prev Med 37:389–395
Blanchard C, Stein K, Baker F, Dent M, Denniston M, Courneya K et al (2004) Association between current lifestyle behaviors and health-related quality of life in breast, colorectal and prostate cancer survivors. Psychol Health 19(1):1–13
Courneya K, Friedenreich C (1997) Relationship between exercise pattern across the cancer experience and current quality of life in colorectal cancer survivors. J Altern Complem Med 3:215–226
Courneya K, Friedenreich C (1997) Relationship between exercise during treatment and current quality of life in breast cancer survivors. J Psychosoc Oncol 15:35–57
Courneya K, Friedenreich C, Arthur K, Bobick T (1999) Physical exercise and quality of life in postsurgical colorectal cancer patients. Psychol Health Med 4(2):181–187
Courneya K, Karvinen K, Campbell K, Pearcey R, Dundas G, Capstick V et al (2005) Associations among exercise, body weight, and quality of life in a population-based sample of endometrial cancer survivors. Gynecol Oncol 97:422–430
Courneya K, Keats M, Turner A (2000) Physical exercise and quality of life in cancer patients following high dose chemotherapy and autologous bone marrow transplantation. Psycho-oncol 9:127–136
Jones L, Courneya K, Vallance J, Ladha A, Mant M, Belch A et al (2004) Association between exercise and quality of life in multiple myeloma cancer survivors. Support Care Cancer 12:780–788
Pinto B, Trunzo J, Reiss P, Shiu S (2002) Exercise participation after diagnosis of breast cancer: trends and effects on mood and quality of life. Psycho-oncol 11:389–400
Vallance J, Courneya K, Jones L, Reiman T (2005) Differences in quality of life between non-Hodgkin’s lymphoma survivors meeting and not meeting public health exercise guidelines. Psycho-oncol 14:979–991
Young-McCaughan S, Sexton D (1991) A retrospective investigation of the relationship between aerobic exercise and quality of life in women with breast cancer. Oncol Nurs Forum 18(4):751–757
Bowker S, Pohar S, Johnson J (2006) A cross-sectional study of health-related quality of life deficits in individuals with comorbid diabetes and cancer. Health Qual Life Outcomes 4(17):1–9
Rogers L, Courneya K, Robbins K, Malone J, Seiz A, Koch L et al (2006) Physical activity and quality of life in head and neck cancer survivors. Support Care Cancer 14:1012–1019
Courneya K, Friedenreich C (1999) Physical exercise and quality of life following cancer diagnosis: a literature review. Ann Behav Med 21(2):171–179
Lynch BM, Baade P, Fritschi L, Leggett B, Owen N, Pakenham K et al (2007) Modes of presentation and pathways to diagnosis of colorectal cancer in Queensland. Med J Australia 186(6):288–291
Australian Institute of Health and Welfare (2003) The Active Australia Survey: A guide and manual for implementation, analysis and reporting. AIHW, Canberra
Bauman A, Armstrong T, Davies J, Owen N, Brown W, Bellew B et al (2003) Trends in physical activity participation and the impact of integrated campaigns among Australian adults, 1997–99. Aust N Z J Public Health 27(1):76–79
Department of Health and Aged Care (1999) National physical activity guidelines for Australians. Australian Government, Canberra
Ward WL, Hahn EA, Mo F, Hernandez L, Tulsky DS, Cella D (1999) Reliability and validity of the Functional Assessment of Cancer Therapy – Colorectal (FACT-C) quality of life instrument. Qual Life 8:181–195
Yost K, Cella D, Chawla A, Holmgren E, Eton D, Ayanian J et al (2005) Minimally important differences were estimated for the Functional Assessment of Cancer Therapy – Colorectal (FACT-C) instruments using a combination of distribution- and anchor-based approaches. J Clin Epidem 58:1241–1251
Hewitt M, Rowland J, Yancik R (2003) Cancer survivors in the United States: age, health, and disability. J Gerontology: Med Sci 58(1):82–91
Ball K, Owen N, Salmon J, Bauman A, Gore C (2001) Associations of physical activity with body weight and fat in men and women. Int J Obesity 25:914–919
Sallis J, Saelens B (2000) Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport 71:1–14
Courneya K, Friedenreich C, Sela R, Quinney A, Rhodes R, Handman M (2003) The group psychotherapy and home-based physical exercise (Group-Hope) trial in cancer survivors: physical fitness and quality of life outcomes. Psycho-oncol 12:357–374
Segal R, Reid R, Courneya K, Malone S, Parliament M, Scott C et al (2003) Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. J Clin Oncol 21(9):1653–1659
Acknowledgments
This study was funded by The Cancer Council Queensland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lynch, B.M., Cerin, E., Owen, N. et al. Associations of leisure-time physical activity with quality of life in a large, population-based sample of colorectal cancer survivors. Cancer Causes Control 18, 735–742 (2007). https://doi.org/10.1007/s10552-007-9016-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-007-9016-6