Abstract
Introduction
Early leakage detection following bariatric procedures is crucial, but a standardized evaluation method is lacking. The aim was to validate the potential benefits of postoperative day 1 (POD1) C-reactive protein (CRP) levels and white blood cell (WBC) counts in distinguishing at-risk patients following Roux-en-Y gastric bypass (RYGB) while considering the impact of obesity-related chronic inflammation.
Methods
Retrospective analysis of 261 consecutive patients aged 18–65 years with a body mass index (BMI) of 32.5–50 kg/m2 who underwent primary RYGB between 2017 and 2022. Sequential changes in CRP levels and WBC counts measured 48 h preoperatively and on POD1 morning were collected and compared between patients with/without complications and in patients without complications stratified by preoperative CRP levels.
Results
Female patients and those with a higher BMI tended to have higher baseline CRP levels, which were positively related to postoperative CRP. Patients experiencing complications had higher WBC counts and a higher prevalence of WBC counts >14,000/μl (77.8% vs. 25.4%; p<0.001) than those without complications. Baseline CRP ≥ 0.3 mg/dl, a longer operative time, and blood loss >10 ml were significantly more common with WBC counts above 14,000/μl; a reasonable range of change in WBC count (∆WBC) derived from its positive correlation to postoperative WBC count (r=0.6695) may serve as a useful complementary indicator.
Conclusion
An individualized CRP threshold setting and integrated interpretation of the WBC count can be more appropriate than using static criteria for differentiating at-risk patients after RYGB. Further studies are needed to validate these findings and determine their generalizability.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bariatric/metabolic surgery is an essential treatment option for the management of severe obesity and related metabolic disorders [1], but it has a high inherent risk of leakage, particularly when the Roux-en-Y gastric bypass (RYGB) procedure is used [2]. The early diagnosis of a leak is crucial for the avoidance of clinically significant outcomes, but this can be challenging due to the ambiguous and delayed onset of the initial symptoms [3].
To predict the occurrence of gastrointestinal anastomotic leakage, current screening methods have limitations in terms of accessibility, timeliness, and accuracy. For example, independently, vital signs may not indicate overt physiological disturbances until it is too late [4], and contrast swallow studies are time-consuming and have limited diagnostic value [5]. Although serum C-reactive protein (CRP) levels and white blood cell (WBC) counts are commonly used acute phase indicators for various gastrointestinal procedures [6], data on the optimal timing of their assessment and criteria for referral in the bariatric setting are inconclusive [7]. Because the extent of surgical trauma can affect postoperative CRP levels [8], it is also uncertain whether standards for these indicators, mostly derived from mixed procedures, can be applied to RYGB [7,8,9,10]. In addition, it has been reported that obesity-related chronic inflammation leads to generally elevated inflammatory biomarkers preoperatively [11]; the potential impact of such a “noisy background” on the interpretation of correlated testing results has not been fully investigated. To address these challenges in the era of enhanced recovery programs (ERAS), this study centers on the comprehensive examination of daily detected inflammation indices, aiming to uncover an approach that holds clinical interpretive advantages. The primary objective is to examine the practicality of utilizing CRP levels and WBC counts as indicators for identifying high-risk patients after RYGB. The secondary objective was to understand the impact of baseline inflammation on the interpretation of correlated testing results. We believe that our research findings will contribute to a safer approach that allows early discharge for most RYGB patients and ultimately improves patient care.
Materials and Methods
We conducted a retrospective cohort study analyzing data from consecutive patients who underwent bariatric/metabolic surgery at a university-affiliated hospital between January 2017 and June 2022. The study was approved by the local institutional review board, and the requirement to obtain informed consent was waived owing to the retrospective study design. We conducted the study in compliance with the ethical standards outlined in the 1964 Declaration of Helsinki and its subsequent amendments.
Inclusion and Exclusion Criteria
To be included in the study, patients had to be 18 years or older, have a body mass index (BMI) of 32.5 kg/m2 or higher with one or more obesity-related comorbidities, or have a BMI ≥ 37.5 kg/m2 or < 50 kg/m2 who underwent primary RYGB. The criteria for selection incorporate a low BMI threshold in accordance with regional ethnic guidelines [12] and align with local health insurance benefit prerequisites. Patients with chronic inflammatory diseases, patients receiving immunosuppressive medications at the time of the procedure, and patients who were on long-term steroid treatment within the past 6 months were excluded from the study. Patients who underwent concomitant procedures or who experienced any intraoperative complications were also excluded. We identified eligible patients and extracted data from electronic medical records using Microsoft Excel 2010 software based on the aforementioned criteria.
RYGB Procedure
RYGB is considered the standard procedure and the procedure we perform most often in a shared decision-making process [13]. The surgical procedure was performed by a single surgeon with a consistent technique, the details of which are described elsewhere [14].
Clinical Care and Evaluations
The preoperative work-up included chest radiographs, electrocardiograms, and esophagogastroduodenoscopy, and a complete blood count and CRP level were routinely obtained within 48 h before the surgery and on the morning of POD1. Standard CRP levels were measured using the Beckman Coulter AU clinical chemistry system, and WBC counts were measured using the Beckman Coulter DxH system. The reference range for CRP was less than 0.5 mg/dl, and results less than 0.1 mg/dl were reported as 0.1 mg/dl due to measurement limitations. The reference range for the WBC count was between 4.8 and 10.8 × 103/μl. Perioperative care was performed following a consistent ERAS protocol [14], and discharge was allowed on the morning of POD1 if vital signs were stable, pain was tolerable, and the results of laboratory tests were within the acceptable range. For any patients who were subjectively unwell or had concerning testing results, a cautious approach was used that included 4–6 h of close in-hospital observation, alleviating medications and further imaging studies if there were any clinically suspicious signs. Data on patient characteristics, including sex, age, BMI, and comorbidities, and intraoperative details, including the operation time, blood loss, and occurrence of intraoperative complications as well as change in the CRP level (∆CRP=postop CRP-preop CRP) and change in WBC count (∆WBC=postop WBC-preop WBC), were collected. Early postoperative complications were defined as any deviation from the standard-of-care treatment within our center within 30 days after surgery. Leakage was diagnosed with computed tomography based on peritoneal fluid collection, abscess formation, or abnormal gas patterns adjacent to anastomosis and proof upon reoperation. To minimize the impact of procedure context and sampling timeframe, the thresholds used as the main putative screening criteria in this study were a CRP level >10 mg/dl [15] and a WBC count exceeding 14,000/μl [6], as both are POD1 and RYGB specific. Other POD1 indicators that are not specifically proposed after RYGB, including a CRP threshold ≥6.1 mg/dl [7], neutrophil percentage >85% [16], and neutrophil-to-lymphocyte ratio ≥ 10 [17], were also analyzed. The primary outcomes assessed included comparing various markers between those with and without complications. A subgroup analysis was conducted in which patients without complications were stratified by baseline CRP level to determine the influence of baseline inflammation, group 1 (<0.3 mg/dl), group 2 (0.3–0.9 mg/dl), and group 3 (≥1 mg/dl), in accordance with the definition of clinically significant inflammation [11, 18], which served as the secondary outcome measures. Patients were followed up postoperatively at 1 week; 1, 3, 6, and 12 months; and then every half-year after surgery. Per the study results, a comprehensive interpretation method considering the complimentary role of individual indicators is proposed.
Statistical Analysis
R version 4.2.0 (R Foundation for Statistical Computing, Vienna, Austria) was used to perform statistical analyses. The Shapiro–Wilk test was used to assess the normality of the continuous variables, and the results are reported as the mean with standard deviation or median with quartiles. Student’s t test or the Mann–Whitney U test was used to compare groups as appropriate. Categorical variables are reported as counts with percentages and were evaluated using Fisher’s exact test or the chi-squared test. Spearman’s correlation coefficient was used to assess the relationship between variables, and linear regression model analysis was employed to identify associations between variables. p values < 0.05 were considered statistically significant.
Results
Out of 270 patients who underwent primary RYGB during the study period, 9 patients were excluded, including one patient with chronic inflammatory disease, one patient on long-term steroids, six patients who underwent concomitant procedures, and one patient who experienced intraoperative bleeding requiring blood transfusion. Among the remaining 261 patients, 9 patients (3 female) experienced complications with a median age of 33.0 (34.0–28.0) and a median BMI of 41.1 (42.7–38.1) kg/m2 that all occurred within 3 days post operation, including leakage (n=1), cellulitis (n=1), wound hematoma (n=2), hematemesis (n=2), and melena (n=3). Three readmissions, including two for hematemesis and one for anastomotic leakage, were performed. The index case of leakage received relaparoscopic repair and recovered uneventfully. No deaths occurred. The other 252 patients who did not experience complications had a median age of 37.5 (43.0–30.0) years and a median BMI of 37.2 (39.6–35.2) kg/m2, and 54.4% were female.
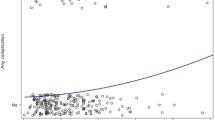
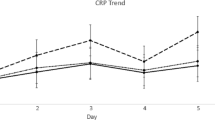
Table 1 shows no difference in CRP level pre- and postoperatively or incidence with CRP >6 mg/dl between the groups. While none had CRP>10 mg/dl, the index case with leakage (CRP = 8 mg/dl) and 10 out of 252 patients without complications had postoperative CRP> 6 mg/dl. Patients with complications had a higher postoperative WBC count (16.06 (17.10–14.29) vs. 12.26 (14.03–10.73); p=0.001), more WBC counts >14,000/μl (7/9, 77.8% vs. 64/252, 25.4%; p<0.001), and a higher ∆WBC than those without complications (6.21 (8.64–4.73) vs. 3.82 (5.40–2.62); p=0.005). As depicted in Fig. 1, a correlation matrix demonstrating moderate positive correlations of WBC counts (r=0.62) and CRP levels (r=0.41) pre- and postoperatively was found in those without complications. Table 2 shows the clinical characteristics of patients without complications categorized based on their baseline CRP levels. Among them, female patients (group 3, 74.2% vs. group 2, 47.5% vs. group 1, 49.0%; p=0.001) and those with a higher BMI (group 3, 39.1 (41.9–36.2) kg/m2 vs. group 2, 37.0 (39.4–34.9) kg/m2 vs. group 1, 36.0 (37.9–34.3) kg/m2; p<0.001) tended to have higher baseline CRP levels. Table 3 presents the POD1 parameters of the subgroups. While Group 3 had higher postoperative CRP levels (2.1 (2.90–1.60)) than group 2 (1.4 (1.90–1.00)) and group 1 (1.1 (1.60–0.75); p<0.001), there was no difference in the incidence of CRP > 6 mg/dl between the groups. Group 3 also had significantly higher preoperative WBC counts (9.08 (10.58–7.68)) than group 2 (8.23 (9.53–7.18)) and group 1 (7.59 (9.05–6.72); p=0.001), a higher postoperative WBC count than group 1 (12.82 (14.80–11.21) vs. 11.86 (13.21–10.57); p=0.025), and a higher percentage of patients with a WBC count >14,000/μl (22 (35.5%)) than group 2 (36 (25.9%)) and group 1 (6 (11.8%); p=0.013).
Spearman’s correlation coefficients were used in the matrix to summarize the correlations between variables. Correlation coefficient interpretation: r=0.00–0.10 negligible correlation, r=0.10–0.39 weak correlation, and r=0.40–0.69 moderate correlation. p value: ***, 0–0.001; **, 0.001–0.01; *, 0.01–0.05; •, 0.05–0.10
Discussion
The inherent leakage rate for RYGB can be as high as 8.3% [19]; however, there is currently no high level of evidence or supporting methods to prevent or reduce this risk. As the initial symptoms may be ambiguous, early recognition of leakage after RYGB can be challenging. In fact, leakage has been reported to be diagnosed at a median of 3 days postoperatively [3]. Considering that most of our patients were discharged on POD1 following RYGB under a coherent ERAS protocol [14] and that clinical outcomes can significantly worsen if leaks or severe complications are not detected and treated promptly [20], it is essential to have a reliable early indicator. To achieve this goal, the current study conducted a comprehensive POD1 data analysis and specifically examined the role of POD1 CRP level and WBC count because both are low-cost, readily accessible, and supported by evidence. The results showed a low incidence of complications, which aligned with national statistics [21], and bleeding and leakage were the most common complications. CRP > 6 mg/dl was able to screen the index case with leakage, and a minor subset of patients without complications presented with CRP exceeding this limit. While female patients and those with a higher BMI tended to have higher baseline CRP levels, postoperative CRP levels were found to be positively related to baseline levels. Patients with complications had a higher WBC count and were more likely to have WBC counts >14,000/μl than those without complications. For a nonnegligible percentage of patients without complications likely presenting with WBC counts >14,000/μl, a baseline CRP >0.3 mg/dl as well as other interfering factors, such as baseline WBC count and perioperative factors, should be considered.
Currently, there is no consensus on a standardized assessment method for the early detection of postoperative complications post RYGB [22]. Clinically, in the absence of consistent criteria, discharging these patients early or not is usually up to the surgeon’s discretion. In actual practice, we examine independent vital signs because these are frequently referred to as essential indicators in identifying complications early [23]; however, none of our patients experienced fever, dyspnea, tachycardia, or unstable blood pressure on POD1, which encompasses cases involving leakage as well. Subsequently, we prefer CRP as our first-line screening tool because it is commonly utilized as a priority diagnostic tool [7,8,9,10, 15], reported to be useful at early detection of postoperative leak and complications [7] and considered a better prognostic marker than WBC count in the bariatric setting due to its higher negative predictive value [8]. The study’s first exam referred to a CRP threshold of >10 mg/dl, and the results showed that such a threshold appeared to be inappropriate for none of the cases with CRP exceeding this limit. It is also clearly higher than in other reports based on combined procedures (range, 5–8.05 mg/dl) [7,8,9,10], and the difference can be partially attributed to a greater CRP surge that is related to more extensive tissue trauma after RYGB than after sleeve gastrectomy [8]. Given the linear relationship between pre- and postoperative CRP, factors inherent to the study population that may affect preoperative baseline values must be considered. For example, Asian patients have a lower median BMI [11] and a smaller proportion of female patients included in our case than Western patients [24] and presumably have a weaker systemic inflammatory response to obesity than North American/European patients [25]. Altogether, these factors may have contributed to a lower baseline CRP level, eased the surgical procedure [26], and tempered the CRP surge [27]. Meanwhile, just as there is a great variation in the proposed CRP criteria [7], these findings support a tailor-made threshold setting in considering study designs, procedure factors, and specific populations. As the ideal can be verified in subsequent studies, the ensuing question of how to adjust the threshold by adapting to these factors remains to be determined. Nevertheless, the study supports the rationale of setting a lower CRP cutoff in our case, and the result that most of our patients without complications had a CRP< 6 mg/dl (242/252) is concordant with the notion of systematic reviews and meta-analyses that a POD1 CRP level below 6.1 mg/dl is associated with a less than 2% risk of complications [7]. However, because the reported sensitivity of POD1 CRP varies greatly (27–100%) [7,8,9,10, 15] and the positive predictive value for POD1 CRP was found to be lower than the CRP measurement at POD 2 or later [8, 10, 28, 29], as suggested, we are more alert regarding in-hospital observation for those with CRP exceeding preset limits [9]. On the other hand, because CRP measurement can be constrained by the sampling timeframe and is not expected to reach its peak until 48–72 h after surgery [28] and the postoperative CRP surge tended to be modest in our case, the supplementary role of other tests is required to help determine the suitability of early release for those with within-range CRP.
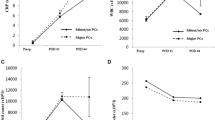
As the second most commonly utilized indicator, the results indicate the general usefulness of WBC count and inferred indicators for patients with complications, including significantly higher WBC counts and WBC counts exceeding 14,000/μ postoperatively. Part of the reason can be because of the sampling timeline. Unlike CRP, the WBC count has an earlier peak that occurs on POD1 [30]. Accordingly, early release is deemed appropriate in cases of patients with CRP <6 mg/dl and WBC count <14,000/μ for expedited early hospital discharge is suggested when CRP levels are within the range and clinical signs are reassuring [15], and WBC count >14,000/μ is able to identify most cases of complications. However, the major flaw of the index criteria resides in a profound impact of baseline WBC count since it is positively correlated with postoperative WBC count. In fact, patients with abnormal preoperative WBC counts (>10.8 (103/μl)) were more likely to have postoperative WBC counts >14,000/μl than those without (20/27, 77.5% vs. 44/225, 19.5%). Further analysis revealed that patients with a postoperative WBC count ≥14,000/μl had significantly higher preoperative WBC counts (10.22 (11.79–9.45) vs. 7.80 (8.91–6.90); p<0.001), a longer operative time (88 (103–80) min vs. 83 (96–74) min; p=0.041), more blood loss >10 ml (7 (10.8%) vs. 4 (2.1%); p=0.007), a higher ∆WBC count (5.87 (7.81–4.22) vs. 3.30 (4.57–2.39); p<0.001), and a longer hospital stay (26 (45–24) vs. 24 (27–22); p=0.009) than those with a postoperative WBC count <14,000/μl (Table 4). Whereas higher baseline CRP levels, intraoperative meaningful blood loss, and, as reported, a longer operation time [19] all likely contributed to a higher prevalence of WBC count >14,000/μ, to achieve this goal, relying solely on individual inflammation indices appears inadequate, and a thorough assessment of postoperative WBC counts, accounting for potential influencing factors, is necessary. It is speculated that operative time and blood loss may serve as surrogate indicators of surgical difficulty encountered and elicit tissue trauma with a stronger leukocyte response. However, we did not find a linear correlation of these factors with postoperative WBC count. Since there was a higher median ΔWBC in patients with complications, a reasonable range of ∆WBC values derived from the dataset of those without complications based upon its linear positive correlation to the postoperative WBC count (r=0.6695), as shown in Fig. 2, can be a useful auxiliary indicator and avoids the interference of the effect of baseline WBC count at the same time (Fig. 3). For postoperative WBC counts in the range of 8000–22,000/μl, each increase in WBC of 2000/μl corresponds to a control table where ΔWBC values can be estimated, from which a reasonable range for ΔWBC is estimated to be 1500 to 9200/μl. In other words, a WBC spike beyond the bounds of this extrapolation could indicate a high-risk scenario that warrants careful handling. In summary, in contrast to the previous standard of care, which lacked consistent referral thresholds and was at the discretion of the surgeon, the present study advocates for an enhanced approach. This approach involves establishing a tailored CRP threshold set at a lower level, followed by a thorough analysis of the WBC count, accounting for whether the ΔWBC falls within an acceptable range. These findings are then integrated into a structured three-step flowchart under the prerequisite of stable hemodynamics (Fig. 4). Retrospectively for the validation of the model, the first step involves using a CRP level threshold of 6 mg/dl to exclude complications, and further observation or clinically indicated examinations are suggested for those patients with CRP> 6 mg/dl. Next, 6 out of 8 patients with complications were classified as at-risk, and a total of 184 of 250 patients were deemed appropriate for early discharge following a WBC count threshold of 14,000/μl. The third step involved using the derived ΔWBC threshold as a supplementary indicator, and early discharge was suitable for 38 out of the remaining 66 patients with acceptable ΔWBC counts. In pursuit of this objective, the suggested measures successfully reduced the number of patients considered high-risk and proved valuable in distinguishing those with WBC counts outside the normal range. This approach addresses the limitations of the previous method, which relied solely on clinical case judgment of CRP level or WBC count. Other potential benefits of obviating unnecessary in-hospital observation or advanced imaging exams can be confirmed by follow-up studies. The pitfall of this framework was that out of the 8 patients experiencing complications, 4 would have still been permitted to be discharged, including those with cellulitis, melena, abdominal wall hematoma, and hematemesis. Given that prior studies have shown that the parameters examined were not reported to have efficacy in differentiating patients with bleeding-related complications [31] and because we did not find a complementary role of other non-RYGB-specific indicators, future investigations will not only delve into the intricacies of individual indices but also consider incorporating other promising assays to provide additional insights and further refine clinical practice.
Proposed three-step flowchart that consists of stepwise interpretation of the postoperative CRP level, WBC count, and ΔWBC count. Step 1, CRP>6 md/dl or not; step 2, WBC count >14,000 or not; step 3, ∆WBC within acceptable range or not. OBS, observation; MBD; may be discharge; BT, body temperature; HR, heart rate; RR, respiratory rate
Limitations
The study’s findings may have limited generalizability due to several factors. First, it only included data from one surgeon, and the study population consisted of patients from a single ethnicity, which hampers the ability to apply the results to other surgical practices. Additionally, the study was retrospective, introducing potential biases in data collection and limiting the ability to establish causal relationships. Unlike other studies, the study did not aim to determine a specific cutoff for individual indicators, citing limitations within the research group with a low incidence of leak and infectious complications. As our study primarily concentrates on the integrated analysis of daily detected inflammation indices in the pursuit of a clinically beneficial approach, to validate the findings and gain deeper insights into the relationship between these biomarkers and outcomes after RYGB, a prospective study with a larger patient population, randomization, stratification by risk factors, and longer follow-up periods would be beneficial.
In summary, while CRP levels were affected by the measurement timeframe and clinical characteristics, the WBC count was more affected by the baseline CRP level, WBC count, and perioperative factors. Clinical utilization of the CRP level or WBC count alone for differentiating patients at high risk of postoperative complications appears to be insufficient. On the basis of our study findings, we recommend an alternative approach that incorporates out-of-the-box thinking by integrating various tests rather than relying on static criteria. The stepwise approach proposed here based on the concept of establishing an individualized CRP level combined with a comprehensive exploration of leukocyte-related data will improve patient care and ultimately support safer and earlier hospital discharge.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to restrictions by the local Institutional Review Board but are available from the corresponding author upon reasonable request and with permission from the local Institutional Review Board.
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Kim J, Azagury D, Eisenberg D, et al. ASMBS position statement on prevention, detection, and treatment of gastrointestinal leak after gastric bypass and sleeve gastrectomy, including the roles of imaging, surgical exploration, and nonoperative management. Surg Obes Relat Dis. 2015;11(4):739–48.
Gonzalez R, Sarr MG, Smith CD, et al. Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J Am Coll Surg. 2007;204(1):47–55.
Bellorin O, Abdemur A, Sucandy I, et al. Understanding the significance, reasons and patterns of abnormal vital signs after gastric bypass for morbid obesity. Obes Surg. 2011;21(6):707–13.
Quartararo G, Facchiano E, Scaringi S, et al. Upper gastrointestinal series after Roux-en-Y gastric bypass for morbid obesity: effectiveness in leakage detection. A systematic review of the literature. Obes Surg. 2014;24(7):1096–101.
Wysocki M, Małczak P, Wierdak M, et al. Utility of inflammatory markers in detection of perioperative morbidity after laparoscopic sleeve gastrectomy, laparoscopic Roux-en-Y gastric bypass, and one-anastomosis gastric bypass-multicenter study. Obes Surg. 2020;30(8):2971–9.
Bona D, Micheletto G, Bonitta G, et al. Does C-reactive protein have a predictive role in the early diagnosis of postoperative complications after bariatric surgery? Systematic review and Bayesian meta-analysis. Obes Surg. 2019;29(11):3448–56.
Chiappetta S, Jamadar P, Stier C, et al. The role of C-reactive protein after surgery for obesity and metabolic disorders. Surg Obes Relat Dis. 2020;16(1):99–108.
Villard MA, Helm MC, Kindel TL, et al. C-Reactive protein as a predictor of postoperative complications in bariatric surgery patients. Surg Endosc. 2019;33(8):2479–84.
Lee Y, McKechnie T, Doumouras AG, et al. Diagnostic value of C-reactive protein levels in postoperative infectious complications after bariatric surgery: a systematic review and meta-Analysis. Obes Surg. 2019;29(7):2022–9.
Chen SB, Lee YC, Ser KH, et al. Serum C-reactive protein and white blood cell count in morbidly obese surgical patients. Obes Surg. 2009;19(4):461–6.
Lee WJ, Wang W. Bariatric surgery: Asia-Pacific perspective. Obes Surg. 2005;15(6):751–7.
Lo HC, Hsu SC. A shared decision-making process may affect bariatric procedure selection and alter surgical outcomes: a single-unit retrospective study. Obes Surg. 2023;33(1):195–203.
Lo HC, Hsu SC, Hsu AC. Factors that hinder 24-hour discharge after laparoscopic Roux-en-Y gastric bypass: a retrospective analysis at a low-volume center. Obes Surg. 2022;32(3):749–56.
Pike TW, White AD, Snook NJ, et al. Simplified fast-track laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2015;25(3):413–7.
Sroka G, Milevski D, Shteinberg D, et al. Minimizing hemorrhagic complications in laparoscopic sleeve gastrectomy--a randomized controlled trial. Obes Surg. 2015;25(9):1577–83.
Da Silva M, Cleghorn MC, Elnahas A, et al. Postoperative day one neutrophil-to-lymphocyte ratio as a predictor of 30-day outcomes in bariatric surgery patients. Surg Endosc. 2017;31(6):2645–50.
Kushner I, Rzewnicki D, Samols D. What does minor elevation of C-reactive protein signify? Am J Med. 2006;119(2):166.e17–28.
Koirala U, Thapa PB, Joshi MR, et al. Systemic inflammatory response syndrome following gastrointestinal surgery. JNMA J Nepal Med Assoc. 2017;56(206):221–5.
Marshall JS, Srivastava A, Gupta SK, et al. Roux-en-Y gastric bypass leak complications. Arch Surg. 2003;138(5):520–3.
Mocanu V, Mihajlovic I, Dang JT, et al. Evolving trends in North American gastric bypass delivery: a retrospective MBSAQIP analysis of technical factors and outcomes from 2015 to 2018. Obes Surg. 2021;31(1):151–8.
Thorell A, MacCormick AD, Awad S, et al. Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. 2016;40(9):2065–83.
Hamilton EC, Sims TL, Hamilton TT, et al. Clinical predictors of leak after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Endosc. 2003;17(5):679–84.
Choi J, Joseph L, Pilote L. Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev. 2013;14(3):232–44.
Kelley-Hedgepeth A, Lloyd-Jones DM, Colvin A, et al. Ethnic differences in C-reactive protein concentrations. Clin Chem. 2008;54(6):1027–37.
DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict mortality risk in patients undergoing gastric bypass. Surg Obes Relat Dis. 2007;3(2):134–40.
Matsui K, Sakuramoto S, Sugita H, et al. C-reactive protein adjusted for body mass index as a predictor of postoperative complications following laparoscopic gastrectomy for gastric cancer. Langenbecks Arch Surg. 2021;406(6):1875–84.
Williams MR, McMeekin S, Wilson RJ, et al. Predictive value of C-reactive protein for complications postlaparoscopic Roux-En-Y gastric bypass. Obes Surg. 2017;27(3):709–15.
Warschkow R, Tarantino I, Folie P, et al. C-reactive protein 2 days after laparoscopic gastric bypass surgery reliably indicates leaks and moderately predicts morbidity. J Gastrointest Surg. 2012;16(6):1128–35.
Csendes A, Burgos AM, Roizblatt D, et al. Inflammatory response measured by body temperature, C-reactive protein and white blood cell count 1, 3, and 5 days after laparotomic or laparoscopic gastric bypass surgery. Obes Surg. 2009;19(7):890–3.
Albanopoulos K, Alevizos L, Natoudi M, et al. C-reactive protein, white blood cells, and neutrophils as early predictors of postoperative complications in patients undergoing laparoscopic sleeve gastrectomy. Surg Endosc. 2013;27(3):864–71.
Author information
Authors and Affiliations
Contributions
H-CL designed the study, performed the surgical procedures, followed up the patients, and participated in the data analysis and the writing of the manuscript. S-CH contributed to the data collection and analysis. All authors have read and approved the final version to be published.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or national research committees and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare no competing interests.
Informed Consent
The requirement to obtain informed consent was waived because no identifiable patient data were disclosed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Individualized CRP threshold setting can be more appropriate for screening.
• Baseline CRP/WBC count and operative factors significantly affect postoperative WBC count.
• ∆WBC can be a useful supplementary indicator.
• A three-step flowchart is proposed.
Supplementary information
ESM 1
(XLSX 68 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lo, HC., Hsu, SC. Suggested Flowchart Through Integrated C-Reactive Protein and White Blood Cell Count Analysis for Screening for Early Complications After Gastric Bypass: a Single-Center Retrospective Study. OBES SURG 33, 3517–3526 (2023). https://doi.org/10.1007/s11695-023-06864-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06864-0