Abstract
Background
Laparoscopic roux-en-Y gastric bypass (LRYGB) has gained increasing popularity as the primary procedure of choice for the management of patients with morbid obesity. Despite the advances, a few patients will still develop complications and predicting these early complications in morbidly obese patients can prove to be difficult. Radiological investigations have limited diagnostic value and have associated side effects and cost. We propose that C-reactive protein (CRP) is a useful predictor for early postoperative complications.
This study aims to determine the ability of CRP taken on postoperative day 1 (POD 1) and 2 to predict occurrence of complications within 30 days of surgery.
Methods
This retrospective observational study selected 183 consecutive patients from the York bariatric database between 01 December 2010 and 23 March 2015. Exclusions: Patients undergoing dual procedures, conversion to open, and if no postoperative CRP measurement was performed.
Results
In total, 138 patients satisfied the inclusion criteria during the study period (median age 44 years [20–68], BMI 50.6 kg/m2 [38.3–62.5]). Fifteen (10.8 %) patients had minor complications (CD of 2) and 8 (5.6 %) had major complications (CD 3 or above). A CRP of greater than 127 mg/L on POD 2 was found to predict complications with 93 % sensitivity and 64 % specificity with diagnostic accuracy 0.82 (95 % confidence interval 0.731–0.908).
Conclusions
In our patients, CRP on POD 2 has been shown to be a good predictor of both minor and major complications and can therefore be used to guide clinicians in making decision as to which patients may need further investigation or who can be safely discharged.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity is a complex and multifactorial disease which is associated with significant morbidity and mortality [1]. There has been a dramatic rise in operative rates for patients with morbid obesity. Surgical intervention is directed toward those patients with a BMI of >35 kg/m2 with significant obesity related comorbidity or patients with a BMI of >40 kg/m2 as it has been shown to be more effective than medical management [1–3].
In the past few decades, laparoscopic options have become a well-established modality of treatment [1, 2]. Laparoscopic roux-en-Y gastric bypass (LRYGB) has gained increasing popularity as the primary procedure of choice for the surgical management of patients with morbid obesity [2].
Identification of patients who are at risk of complications is of great clinical importance to improve clinical outcomes, improve patient experience, and guide resource allocation. Patients undergoing surgery for morbid obesity may have prolonged hospital stays. This is understandable when the complications of LRYGB can cause significant morbidity and even mortality [2]. It is more difficult to clinically ascertain if a morbidly obese patient has a complication and many surgeons rely on radiological investigations, such as upper GI series, to assist with the diagnosis of complications; these however may have limited diagnostic value [1] and add additional cost [1, 7].
It is well documented that the stress response of surgery leads to a rise in serum C-reactive protein (CRP) and that CRP measurement is a cheap (£2.27 at York Hospital laboratory), easily accessible, and frequently used blood test. In healthy postoperative patients, the peak concentration of CRP will be seen 48–72 hours postoperatively and will then fall [4]. This leads to the assumption that a persistently raised or climbing CRP thereafter is caused by ongoing inflammatory processes unrelated to the trauma of surgery [4]. There is persuasive evidence that the use of CRP as a predictor of clinical outcomes in open surgery is of clinical benefit; however, the value of CRP following laparoscopic surgery and how CRP might predict later outcome are still unclear [5, 6].
The pathophysiology of obesity being responsible for an elevated baseline of CRP is well documented and thought to be due to the increased adipose tissue and accumulation of free fatty acids promoting the release of proinflammatory cytokines and thus the hepatic genesis of CRP [1, 9].
The sensitivity and specificity of CRP as a predictor of complications post-LRYGB is not widely reported and varies greatly. There is a reported range of sensitivities between 53 and 100 % and specificity between 71.6 and 95.5 % [1, 2, 5–11]. The postoperative day (POD) on which CRP measurement is at the optimal time to predict outcome varies from POD 1 to POD 5. The threshold of CRP for an increase in complications varies from over 100 on POD 1, 229 on POD 2, and above 136 on POD 5 [1, 2, 5–11].
There remains some uncertainty, therefore, as to the timing of CRP measurements and whether CRP measured between POD 1 and POD 5 can predict occurrence of complications. This study has the following aims:
-
1.
To determine the ability of CRP taken on POD 1 and POD 2 to predict occurrence of complications within 30 days of surgery.
-
2.
To determine the cutoff values for CRP (POD 1 and POD 2) that might best discriminate the development and non-development of complications within 30 days of surgery.
Method
Data from all consecutive patients who underwent LRYGB from the prospectively maintained York bariatric database between the dates of 01 December 2010 to 30 March 2015 were collected. The York unit has four upper GI surgeons performing LRYGB and all were included. Patients were excluded if they underwent dual procedures, were converted to open procedures, or who had no postoperative CRP measurement on record.
Data was extracted from the electronic patient care records (Clinical Patient Database software) and inputted into an encrypted excel spread sheet. The following was recorded: patient characteristics including date of birth, age at operation, gender, BMI, and ASA grade. Intraoperative details including surgeon name and occurrence of intraoperative complications were recorded. Postoperative CRP measurements for POD 1 to POD 5, length of stay (LOS), and occurrence of complications within 30 days of surgery were measured. Complications were defined using the Clavien-Dindo classification [12]. A grade II classification or above was taken to indicate that a postoperative complication has occurred.
Statistical Analysis
Statistical analysis was performed using SPSS Statistics 21 (IBM Software, USA). The ability of POD 1 and POD 2 CRP to predict postoperative complications was assessed using receiver operating characteristic (ROC) curves and area under the curve (AUC) analysis. As CRP is a continuous variable and there is no known diagnostic criterion for being positive or negative, this analysis allows the test to be assessed but also given a “cutoff” for diagnostic accuracy [13]. The data for sensitivity (true positive fraction) is plotted against specificity (false positive fraction) which generates a curve. The better the test, the closer to the upper left hand corner the curve will plot [13]. A test which runs along to the diagonal line depict a diagnostic test with the same performance as chance, i.e., the results will be unrelated to disease status [13]. For continuous results, a cutoff for a positive result is often assigned by an arbitrary value set. ROC analysis avoids this by assessing the sensitivity and specificity at differing cutoff to calculate the optimal cut off point. The AUC is interpreted as the independent average value of the sensitivity for all possible specificities. A value of 0.5 describes a test no better than chance, a score of 1 would describe a test with a 100 % diagnostic accuracy, and a value of 0 would describe a test which was incorrect every time [13].
Results
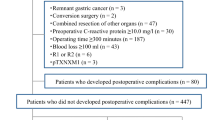
The York bariatric database identified 183 patients. One hundred and thirty eight satisfied the inclusion criteria, 34 males and 104 females, median age 44 years [range 20–68], and median BMI 50.6 kg/m2 [range 38.3–62.5]; mode ASA grade was 2 [range1–3].
The excluded patients were for dual procedures performed (n = 6), conversion to an open procedure (n = 6), no CRP measurement on POD 1 or POD 2 (n = 24), reoperation before a CRP measurement had been taken (n = 2), and incorrect coding of LRYGB (n = 7). The 24 patients excluded with no CRP measurement on POD 1 or POD 2 had a median age of 47 (27–70), median LOS of 4 days (2–8 days), ASA of 2 (2–3), and BMI of 49.9 kg/m2 (36–66.7).
Postoperative CRP levels were recorded on POD 1 to POD 5 when measured; not all patients had levels taken daily (Table 1). It can be seen from Table 1 that the CRP measurements had a large range of values on each day. The trend of median CRP over the first 5 days can been seen in Fig. 1. This data corroborates the literature that CRP peaks in the 48–72-hours period then tails off [4]. We found there was a slight upward trend in CRP on POD 5. We postulate that this is due to two reasons: firstly, due to the small sample size of patients having a CRP measurement POD 5 as most patients were well and discharged home before POD 5. Secondly, the patients who were tested on POD 5 were those who were remaining in the hospital due to a complication and as such would have a higher CRP.
Twenty-three patients had postoperative complications. Fifteen (10.8 %) patients had minor complications (CD of 2) and 8 (5.6 %) had major complications (CD 3 or above). Of the complications, seven patients required surgical intervention; there was one patient with an anastomotic leak, one with a bleeding anastomosis, and one with small bowel obstruction. Two patients required endoscopic evaluation. Five patients had wound infection or leak requiring antibiotics or readmission. Seven patients developed respiratory complications and one patient developed diabetic ketoacidosis. Table 2 demonstrates the observed complication breakdown.
The median LOS was 4 days (range 2–62 days). Table 3 demonstrates the LOS for both cohorts of patients. The median LOS for patients without complications was 4 days (range 2–7 days) and for those with complications was 6.5 days (range 2–62 days).
The cohort of patients who developed complications and those who did not are well matched in baseline characteristics. For those who did not have complications, the median age was 43, median ASA was 2, and median BMI was 50.7. For those who did have complications, the median age was 44, median ASA was 2, and median BMI was 50.15. There is a female preponderance for both cohorts. However, male gender has a higher representation in the cohort with complications with a ratio of 4.7:1 (F/M) compared to a ratio of 2.7:1 (F/M) in the cohort of patients without complications. This finding is expected as male gender is a known risk factor for postoperative complications following obesity surgery [14, 15].
Patients who developed complications had a significantly higher CRP on POD 2 than did those who did not (p < 0.0005); this is clearly demonstrated in Fig. 2 (Mann-Whitney U 249.000, Wilcoxon W 4527.000, Z − 3.957, Asymp. Sig. (two-tailed) 0.000).
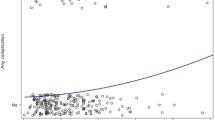
Analysis of the AUC of the ROC curve demonstrated that day 1 CRP AUC is 59 % (95 % confidence interval, 45.4–72 % p = 0.279) (Fig. 3a). The line plotted hugs the diagonal line.
Analysis of the AUC of the ROC curve demonstrated that day 2 CRP AUC is 82 % (95 % confidence interval, 73.1–90.8 % p < 0.0005) (Fig. 3b), as can be seen from the ROC curve moving close to the upper left hand corner—the ROC point.
A CRP of greater than 127 mg/L on postoperative POD 2 was found to predict complications with 93 % sensitivity and 64 % specificity with diagnostic accuracy 0.82 (95 % confidence interval 0.731–0.908, p < 0.0001) (Fig. 3b).
Discussion
As experience with bariatric surgery improves and laparoscopic techniques employed, rates of postoperative complications following bariatric surgery are reducing. Despite this, when they occur, they are serious and can be fatal. The morbidly obese patient is complex and makes early diagnosis of complications more difficult. In this study, we demonstrate how the use of CRP can be useful in this decision-making process. We demonstrate the expected rise and fall of CRP in all postoperative patients in addition to showing the difference between those patients who develop complications and those who do not.
Pike and colleagues [2] propose an attractive fast-track management strategy for discharging patients on POD 1. They have reported that a POD 1 CRP is a good predictor of later complications. In a review of their fast-track LRYGB service, they report that most of their 112 patients were discharged on day 1 following surgery [2]. They found that a POD 1 CRP above 100 mg/L predicted major postoperative complications with 100 % sensitivity, 95 % specificity, and a diagnostic accuracy of 0.98. However, this was in relation to a single surgeon experience with a dedicated fast-track service that may not be available at present in some hospitals. Currently, there is no national standard for postoperative management and as such, clinical practice varies.
Unlike previous studies, we found no predictive benefit of measuring CRP on POD 1. We found a diagnostic accuracy of only 59 %, i.e., marginally better than chance alone. In this cohort, we found CRP measurement on POD 2 appears to be a good predictor of postoperative complications. We demonstrate that a CRP of above 127 mg/L predicts postoperative complications with a sensitivity of 93 % and specificity of 64 %. We recommend that POD 2 is the optimum time to sample CRP to use as a predictor of complications.
POD 2 CRP is a highly sensitive predictor of “at-risk patients”. Having the ability to easily and cheaply identify such patients is of great clinical importance. The CRP measurement will add to the clinician’s decision making and allow targeted investigations and additional monitoring to these patients who have a CRP above 127 mg/L. It has been suggested that radiological studies to detect intestinal leaks following LRYGB should be limited to patients with clinical symptoms such as tachycardia or respiratory distress [7]. Taking this approach limits the amount of radiation patients are exposed to along with lowering the amount of false-positive and false-negative results routine performance would yield [1, 7]. However, waiting for patients to develop symptoms will, of course, lead to the delay in detection of complications and thus negatively affect patient outcomes. Adding the CRP level to the clinical picture can raise clinical suspicion in those patients who may not be displaying early signs of complications and allow targeted diagnostic management.
Based on our findings, it may be worth considering a protocol where patients who have a CRP below 127 mg/L POD 2 in the context of a normal clinical examination can be discharged home safely on POD 2. We suggest the cohort of patients with an elevated CRP are monitored more closely, have repeat blood monitoring, and a consideration of radiological imaging should be taken at this point. This postoperative management strategy would improve patient care, target resources to the patients most at risk of complications, and would save bed days. Using a retrospective model applied to our patients, we can calculate the approximate cost in terms of bed days. This relies on the assumption that all patients are clinically stable at POD 2. Fifty-nine patients had a CRP below 127 mg/L recorded on POD 2 who had no postoperative complications—97 % (n = 57) of those patients stayed longer than 2 days. This is at the cost of 121 bed days. Twenty-nine patients had a CRP recorded above 127 mg/L and had no complications, thus would stay in hospital for another day at a cost of 29 bed days. Three patients would be discharged who would later develop a complication. At York Teaching Hospital, the cost per bed day is £848. This is a saving of 92 bed days at a cost of £78,016.
We suggest that serial CRP levels are taken on POD 2 and POD 3 if the patient is not discharged on POD 2. From our data, patients who had a CRP >127 mg/L on POD 2 who had no complications had a median POD 2 CRP of 171.5 mg/L (95 % CI 151.41–191.59), which rose to a median POD 3 CRP of 195 mg/L (95 % CI 165.57–224.43). Patients who had a CRP >127 mg/L on POD2 who developed complications had a median POD 2 CRP of 177.5 mg/L, which rose to a median POD 3 of 212 mg/L. Due to the small number of patients (n = 26) who had both POD 2 and POD 3 CRP measurements, this study is unable to conclude what represents a clinically significant rise in CRP POD 3.
The 30-day morbidity in our study is comparable to data currently published, between 4.4 and 29 % [1, 5–7], suggesting that our cohort of patients is representative. The incidence of anastomotic leak was low at 0.7 % (n = 1); this is also consistent with the previously reported rate of anastomotic leak being between 0.4 and 5.2 % [1].
The baseline characteristics of our complication group and non-complication group are well matched for age, ASA, and BMI thus reducing confounding factors. There was a larger representation of females in both groups but relatively a higher number of males in the complication group. This result was expected and is mirrored in previous literature where the male sex is an independent cause of complications [15]. The Obesity Surgery Mortality Risk Score uses male gender as one of a five-point score to classify postoperative risk [14, 15].
The main limitation of this study is the retrospective design. Consequentially, the data is limited, as CRP was not routinely taken in all patients. To ascertain any likely selection bias, we compared the patient demographics of the patients included to those excluded due to the fact that no CRP was performed on days 1 or 2 (Table 4) and found no difference between the two. We therefore do not think we have selected out those patients more likely to have had complications because they had CRP performed on POD 1 or POD 2.
Due to the retrospective data collection, it is impossible to report whether the CRP measurement was performed as a routine test or whether the CRP was requested due to clinical suspicion of complications. As such, we limited the analysis of CRP to POD 1 and POD 2 as later CRP measurements (POD 3, POD 4, POD 5) are in a cohort of patients who remain in the hospital for clinical reasons. Table 4 compares the characteristics of the patients who were excluded due to having no CRP measurement (n = 24) to those who were included (n = 138). The groups are matched on age, sex, ASA grade, LOS, and BMI; the complication rate is 12.5 to 16.6 % meaning that we have not excluded a cohort of patients who are different to the study population.
Data was collected from the CPD computer program and as such, the clinical notes were not seen. All observations (such as temperature and heart rate) are documented electronically on CPD, and we were able to document all abnormalities, radiological interventions, readmissions, and re-attendances to A&E (all notes are scanned onto CPD). In addition to this, a comprehensive discharge letter is constructed by each operating consultant surgeon after discharge directly from the patient notes. We therefore did not feel we would gain extra information in obtaining the notes.
Conclusion
To conclude, CRP measurement POD 2 is a highly sensitive predictor of postoperative complications post-LRYGB. A measurement >127 mg/L should alert the clinician to target extra monitoring and consider further investigations to diagnose early complications and reduce postoperative morbidity and mortality. A measurement below 127 mg/L, along with a normal clinical examination, can aid the decision making for a safe and timely discharge from hospital.
These results are sufficiently compelling to warrant a large, higher powered, multicentered prospective study to further investigate the predictive value of CRP in LRYGB patients.
References
Romain B, Chemaly R, Meyer N, Chilintseva N, Triki E, Brigand C, Rohr S. Diagnostic markers of postoperative morbidity after laparoscopic roux-en-Y gastric bypass for obesity. Langenbeck’s Arch Surg. 2014;399(44):503–8.
Pike TW, White AD, Snook NJ, Dean SG, et al. Simplified fast-track laparoscopic roux-en-Y gastric bypass. Obes Surg. 2015;25(3):413–7.
MacKay GJ, Molloy RG, O’Dwyer PJ. C-reactive protein as a predictor of postoperative infective complications following elective colorectal resection. Color Dis. 2011;13(5):583–7.
Straatman J, Van der Peet D. C-reactive protein after major abdominal surgery: biochemical and clinical aspects. Amsterdam Medical Student Journal. 2015;2:1–3.
Adamina M, Steffen T, Taratino I, Beutner U, Schmied BM, Warschow R. Meta-analysis of the predictive value of C-reactive protein for infectious complications in abdominal surgery. Br J Surg. 2015;102(6):590–8.
Takeno A, Takiguchi S, Fujita J, Tamura S, Imamura H, Fujitani K, Matsuyama J, Mori M, Doki Y. Clinical outcome and indications for palliative gastrojejunostomy in unresectable advanced gastric cancer: multi-institutional retrospective analysis. Ann Surg Oncol. 2013;20(11):3527–33.
Warschkow R, Taratino I, Folie P, Beutner U, Schmied BM, Bisang P, Schultes B, Thurnheer M. C-reactive protein 2 days after laparoscopic gastric bypass surgery reliably indicates leaks and moderately predicts morbidity. J Gastrointest Surg. 2012;16(6):1128–35.
Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444(7121):875–80.
Warsi A, Heptinstall L, Asaria M, Passafiume F, Jaw M, Barecca M, Whitelaw D, Jain VK. The significance of routine white cell count (WCC) and C-reactive protein (CRP) measurements following laparoscopic roux-en-Y-gastric bypass (LRYGB). Obesity Surg. 2012;22(9):1362.
Aguilo R, Agrawell S. Fast track laparoscopic roux-en-y gastric bypass surgery. Obes Surg. 2013;23(8):1195.
Crowe C, Garg T, Leva N, Rivas H, Morton J. Predictors of cardiopulmonary complications following bariatric surgery. Gastroenterology. 2013;144(5):1086–7.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4(2):627–35.
Lorente L, Ramon J, Vidal P, Goday A, Parri A, Lanzarini E, Pera M, Grande L. Obesity surgery mortality risk score for the prediction of complications after laparoscopic bariatric surgery. Cirugia Espanola (English Edition). 2014;92(5):316–23.
Livingston EH, Huerta S, Arthur D, Lee S, De Shields S, Heber D. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg. 2002;236(5):576–82.
Acknowledgments
The authors would like to acknowledge the help of Mr. David Locker for his hard work and maintaining the prospective bariatric patient database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required. Informed consent does not apply to this submission.
Rights and permissions
About this article
Cite this article
Williams, M.R., McMeekin, S., Wilson, R.J.T. et al. Predictive Value of C-Reactive Protein for Complications Post-Laparoscopic Roux-En-Y Gastric Bypass. OBES SURG 27, 709–715 (2017). https://doi.org/10.1007/s11695-016-2349-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2349-z