Abstract
Background
Bariatric surgery involves the risk of postoperative infectious complications, in particular, anastomotic leaks and intra-abdominal abscesses. C-reactive protein (CRP) is a nonspecific marker of inflammation which has gained attention as a test to predict postoperative infectious complications. This systematic review and meta-analysis evaluated the diagnostic value of CRP to detect postoperative infectious complications after bariatric surgery.
Methods
Search of MEDLINE, EMBASE, CENTRAL, and PubMed databases were performed. Articles measuring serum CRP postoperatively in patients with obesity undergoing bariatric surgery were included. Main outcomes included diagnostic value of postoperative serum CRP (area under the curve (AUC), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV)). Diagnostic accuracy of included studies was assessed using QUADAS-2.
Results
Six studies including 2770 patients met the inclusion criteria. The derived CRP cutoff values were 71.4 mg/dL, 130.3 mg/dL, and 118.7 mg/dL on postoperative days (PODs) 1, 3, and 5, respectively. Pooled AUC was similar across PODs 1, 3, and 5 with AUC being highest on POD 5 (0.88 ± 0.07). PPV was between 19 and 21%, and NPV was between 98 and 99%. CRP levels were significantly higher (P < .0001) in postoperative infectious complication group versus the no complication group on PODs 3 and 5.
Conclusions
High NPV and moderately high sensitivity on PODs 1, 3, and 5 may help predict patients who are at a low risk of infectious complication following bariatric surgery. High specificity on PODs 1 and 3 also indicates that it can be useful for early diagnosis of postoperative infectious complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity has become a global health epidemic [1]. As such, the number of people with obesity undergoing bariatric surgery across the world has doubled since 2000 [2]. As part of a multidisciplinary approach to the management of obesity, bariatric surgery has been shown to be an effective means of allowing for sustained weight loss and decreased obesity-associated comorbidities compared to the medical management of morbid obesity [3]. As with any surgical procedure, bariatric surgery involves the risk of postoperative infectious complications, such as anastomotic leaks and formation of intra-abdominal abscesses [4]. These complications are typically diagnosed clinically, with or without the use of radiographic studies [5]. Unfortunately, as many as 79% of anastomotic leaks occur beyond postoperative day (POD) 10 and following hospital discharge [6]. Thus, the predictive value of clinical symptoms in the postoperative period is not sufficient in identifying all infectious complications.
C-reactive protein (CRP) is a serum acute-phase reactant produced by the liver in response to proinflammatory cytokines that play a role in activating the complement system [7]. As a nonspecific marker of inflammation that can be tested easily, at low cost and with good reliability, CRP level has gained traction as a test to address the shortcomings of the clinical assessment of postoperative infectious complications [8, 9]. In colorectal surgery, it has been validated as a useful negative predictor test for septic complications and specific laboratory cutoff values have been established [10]. Currently, in bariatric surgery, the use of CRP is limited [11]. Furthermore, there is significant heterogeneity in the current cutoff values and days of measurement of CRP following bariatric surgery [12,13,14,15,16,17]. The time frame in which CRP levels are used in the bariatric surgery setting range from the day of surgery to POD 30 [12,13,14,15,16,17]. As such, it remains unclear when CRP is most useful as a predictive tool in the postoperative period, as well as what CRP level is most accurate in predicting postoperative infectious complications in bariatric surgery.
As the morbidity associated with postoperative infectious complications following bariatric surgery is well established, the utility of CRP to predict which patients are at greatest risk is an important topic that has not yet been systematically reviewed. This systematic review and meta-analysis aims to further validate the predictive value of CRP for detecting postoperative infectious complications and to establish clinically valuable cutoff values for CRP levels following bariatric surgery.
Materials and Methods
Search Strategy
We searched the following databases covering the period from database inception through October 19, 2018: MEDLINE, EMBASE, Web of Science, and PubMed. The search was designed and conducted by a medical research librarian with input from study investigators (complete search strategy available in Appendix). We searched the references of published studies and searched gray literature manually to ensure that relevant articles were not missed. We did not discriminate full texts by language. The protocol of this study was registered before commencement in the Prospective Register of Systematic Reviews (PROSPERO).
Outcomes Assessed
Primary outcomes included diagnostic value of postoperative serum CRP after bariatric surgery in patients experiencing postoperative infectious complication (area under the curve (AUC), sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Secondary outcomes were the following: (1) serum CRP levels at postoperative days 1, 2, and 3 in patients that experienced postoperative infectious complication or no complication; (2) length of stay (days) in the hospital after bariatric surgery; and (3) hospital readmission after bariatric surgery.
Study Selection and Data Extraction
Articles were eligible for inclusion if they measured serum CRP postoperatively in patients with morbid obesity (BMI > 40 kg/m2 or > 35 kg/m2 with obesity-related comorbidities) undergoing bariatric surgery and reported one of our relevant primary outcomes. Relevant studies that did not report any diagnostic values or did not conduct a predictive analysis of postoperative infectious complications (e.g., anastomotic leak, intra-abdominal infections) for CRP were excluded. We excluded studies with less than 10 eligible patients. Two reviewers independently evaluated the systematically searched titles and abstract using a standardized, pilot-tested form. Discrepancies that occurred at the title and abstract screening stages were resolved by automatic inclusion to ensure that all relevant papers were not missed. Discrepancies at the full-text stage were resolved by consensus between two reviewers, and if disagreement persisted, a third reviewer was consulted. Two reviewers independently conducted data abstraction onto a data collection manual designed a priori. Abstracted data included study characteristics and patient demographics (e.g., author, year of publication, study design, age, % female, preoperative BMI, % diabetes), postoperative outcomes (e.g., prevalence of anastomotic leak/fistula, infectious complications), CRP measurements (e.g., CRP cutoff value, time points when CRP was measured, CRP levels at each postoperative day), and outcomes.
Quality Assessment
Quality assessment for each study was assessed using QUADAS-2 (quality assessment for studies of diagnostic accuracy studies-2) tool (e.g., appraisal by use of empirical evidence, expert opinion, and formal consensus to assess the quality of primary studies of diagnostic accuracy) [18].
Data Synthesis and Analysis
All statistical analysis and meta-analysis were performed on STATA version 14 (StataCorp, College Station, TX) and Cochrane Review Manager 5.3 (London, UK). The weighted geometric mean was used to derive the pooled CRP cutoff value at each postoperative day. The pooled prevalence of postoperative infectious complications, sensitivity, specificity, PPV, and NPV was calculated using the Freeman–Tukey double arcsine transformation of proportions. Pooled diagnostic values and their respective 95% confidence intervals (CI) were obtained using DerSimonian and Laird random effects meta-analysis of proportions. Inverse-variance method was used to calculate pooled AUC of CRP in each postoperative day. We also performed pairwise meta-analyses using a DerSimonian and Laird random effects model for continuous variables such as postoperative levels of CRP and length of stay between patients with complications versus no complications. The threshold for statistical significance was set a priori at alpha = 0.05. Pooled effect estimates were obtained by calculating the mean difference (MD) in outcomes along with their respective 95% confidence intervals (CI) to confirm the effect size estimation. Mean and standard deviation were estimated for studies that only reported median and interquartile range (IQR) using the estimation method proposed by Wan et al. [19]. Assessment of heterogeneity was completed using the inconsistency (I2) statistic. We considered I2 higher than 50% to represent considerable heterogeneity.
Results
Study Characteristics
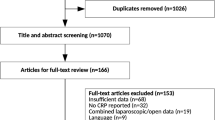
From 1091 potentially relevant citations received from electronic databases and reference searches, 6 studies met the inclusion criteria (3 prospective, 3 retrospective) with the data sufficient to be included in the meta-analysis. Figure 1 depicts a PRISMA flow diagram of study selection process. All studies measured the level of CRP after bariatric surgery and reported at least one of the outcomes of interest. In total, there were 2770 patients (75.8% female, mean age of 40.49 years, and preoperative BMI of 43.59 kg/m2). Included studies were conducted between 2012 and 2018. Types of bariatric surgery performed were laparoscopic sleeve gastrectomy (LSG; three studies), Roux-en-Y gastric bypass (RYGB; two studies), and both (one study). Detailed study characteristics of included studies are reported in Table 1. Definitions for postoperative leak were homogeneous across studies as they defined leak as presence of contrast material outside of the GI tract shown by a radiologic examination or during reoperation (Supplementary Table S1). Moreover, included studies defined postoperative infection as any presence of leak, abscess collection, or presentation of any septic complication after surgery. Specific prevalence for postoperative leak could not be measured due to studies often not reporting postoperative leak and postoperative infectious complication separately.
Outcomes
The pooled prevalence (SD) of postoperative infectious complications for included studies was 4.0% (0.83) on POD 1, 4.4% (1.37), on POD 3, and 3.7% (1.54) on POD 5. The derived CRP cutoff values were 71.4 mg/dL on POD 1, 130.3 mg/dL on POD 3, and 118.7 mg/dL on POD 5. CRP levels were significantly higher in postoperative infectious complication group versus the no complication group throughout POD 3 and 5. Moreover, length of stay was significantly longer in the postoperative infectious complication group by 1.28 days (MD 1.28, 95% CI, 1.04–1.52, P < .0001) (Supplementary Fig. S1).
The six studies included had various time points for measuring predictive value of CRP postoperatively. A meta-analysis of predictive values of CRP for postoperative infectious complication was performed for POD 1 (three studies), POD 3 (three studies), and POD 5 (three studies) as they were most commonly reported across studies. We did not meta-analyze other PODs due to it being reported in less than three studies. Pooled AUC was similar across POD 1, 3, and 5, with AUC being highest on POD 5 (AUC of 0.88 (0.07)). Sensitivity was highest at 91% on POD 5 with a CRP cutoff value of 118.7 mg/L, but POD5 had a lowest specificity of 83% compared to other PODs (Tables 2 and 3). Specificity was highest in POD 1 of 94% with CRP cutoff value of 71.4 mg/L, but with lowest sensitivity of 77%. Predictive parameters including PPV (between 19 and 21%) and NPV (between 98 and 99%) were similar across all postoperative days. CRP values were significantly higher in the postoperative infectious complication group than the no complication group in POD 3 (MD 117.43, 95% CI 76.54 to 158.31, P < 0.00001) and POD 5 (MD 120.25, 95% CI 57.12 to 183.38, P = 0.0002) (Supplementary Fig. S2–4).
Risk of Bias
Table 4 presents the quality assessment of included studies using the QUADAS-2 tool. Applicability of the included studies was appropriate for patient selection, index test, and reference standard. One study had poor applicability for patient selection due to excluding patients with acute and proved postoperative complications between days 0 to 5. All of the studies (6/6 studies) did not blind surgeons or investigators to results of CRP postoperatively. Moreover, the majority of the studies did not consecutively measure CRP data every day after surgery. Three studies measured CRP levels on one specific day after surgery, and two other studies measured CRP every other day of the operation. Four studies had slight variations in definitions of postoperative infectious complication after surgery, and only two studies had directly investigated the predictive value of CRP to postoperative leak after bariatric surgery.
Discussion
This systematic review and meta-analysis demonstrates that CRP level can be a valuable test in predicting the risk of postoperative infectious complication following bariatric surgery. More specifically, derived CRP cutoff values for POD 1, 3, and 5, demonstrated high specificity and sensitivity, as well as high negative predictive value (NPV), for the detection of postoperative infectious complication after LSG and RYGB. The greatest sensitivity for postoperative infectious complication was on POD 5, and specificity was highest on POD 1. A risk of bias assessment of the evidence using QUADAS-2 found there to be high risk of bias, but good applicability of the evidence for the use of derived CRP cutoff values and pooled AUC. Importantly, these data demonstrate a pooled prevalence of complications reaching as high as 4.4% in the first 5 days following bariatric surgery, suggesting that there is a role for CRP to play in early detection of postoperative infectious complication in bariatric surgery.
Although the present systematic review is the first to explore the utility of CRP in predicting postoperative infectious complication in bariatric surgery, the utility of CRP levels to rule out postoperative infectious complication has been established in other surgical fields. Specifically, the predictive capability of CRP levels following colorectal surgery was recently meta-analyzed [10]. CRP values on POD 3, 4, and 5 after colorectal surgery are useful negative predictive tests, with NPVs of 97% for each of the given cutoff values (172 mg/L, 124 mg/L, and 144 mg/L, respectively). Similarly, CRP measurement in esophagogastric resection has demonstrated high NPV for the development of postoperative infectious complication [20]. The CRP levels on POD 2, 3, and 6 had NPVs of 100% for postoperative infectious complication with cutoffs of 209 mg/L, 190 mg/L, and 154 mg/L, respectively. Given the high NPV and sensitivity that CRP levels demonstrate for detection of postoperative infectious complication following other gastrointestinal surgeries, it is reasonable to speculate that the predictive capabilities of CRP demonstrated in the current study, especially the NPVs greater than 98%, are accurate.
While this systematic review and meta-analysis focused on CRP, previous studies have evaluated other easily measured acute-phase reactants, such as procalcitonin, white blood cells (WBC), iron, and albumin for the early detection of postoperative infectious complication following bariatric surgery [11, 12, 21,22,23,24]. A recent study by Frask et al. [21] evaluated the utility of procalcitonin for the early detection of nonseptic and septic complications following LSG. Although they demonstrated that patients who develop postoperative septic complications have procalcitonin levels on POD 2 20 times greater than those patients that do not have septic complications, they did not analyze the predictive value of procalcitonin in this setting, and therefore, the clinical use of this marker is still in question. Similarly, Kassir et al. [22] demonstrated a significant increase in postoperative procalcitonin values in patients developing fistula or abscess following LSG (0.1 08 mg/L vs. 0.0 62 mg/L, P = 0.0006) without evaluating the overall predictive value of the marker. Interestingly, one of the studies included in this systematic review and meta-analysis also evaluated the efficacy of WBC as a predictor of postoperative infectious complication [12]. The subsequent receiver–operator curve analysis demonstrated WBC levels have high specificity for postoperative infectious complication on POD 3 and 5 (92.4% and 98%, respectively). In contrast, a meta-analysis by Zhang et al. [23] concluded that due to inconsistent serial changes in WBC postoperatively, it was not useful at predicting postoperative infectious complications in bariatric surgery. Of note, iron was also included as a parameter of interest in the study by Albanopoulos et al. [12]. They observed a decrease in the availability of iron and an elevated ferritin level in patients that experienced postoperative infectious complication. Finally, albumin has been evaluated as a preoperative predictor of postoperative infectious complication following bariatric surgery. In a study by Turner et al. [24] in which 11 preoperative variables were identified and analyzed, albumin was among the four strongest independent predictors of postoperative morbidity. Future studies are needed to further evaluate the utility of these various markers both independently, as well as combined with CRP levels.
Despite the heterogeneity and the high risk of bias within the included studies, this study provides a useful framework for the analysis of CRP measurements after bariatric surgery. These data demonstrate that CRP is clinically useful as both a negative and a positive test. The high NPV and the moderately high sensitivity on POD 1, 3, and 5 can help predict patients who are at a low risk of developing a postoperative infectious complication following bariatric surgery. This can facilitate confidence in early discharge strategies aimed at system wide cost-saving due to lower length of stay. Furthermore, the high specificity that was demonstrated for POD 1 and POD 3 CRP measurements also indicates that it can be useful for early diagnosis of postoperative infectious complication. This may be related to the increasing frequency of laparoscopic surgery, in which CRP levels return to baseline more quickly as a result of less tissue trauma and blood loss [25]. Bariatrics, like any surgical specialty, benefits from early identification and treatment of infectious complications. Taken together, patients with increased CRP levels (> 74.1 mg/L on POD 1, > 130.3 mg/L on POD 3, and/or > 118.7 mg/L on POD 5) following bariatric surgery, are more likely to have a postoperative infectious complication and would require additional clinical investigation or further observation. Caution should be used in this work-up, as the low PPV and low incidence of postoperative complications in bariatric surgery means that even in positive test results, the risk of a complication is only around 20%. Thus, while observation and low-risk testing can be considered, a positive CRP value should not automatically necessitate a CT scan or operative exploration. That being said, an elevated CRP on POD1 will identify nearly 80% of leaks and more than 90% of postoperative infectious complications by POD5, so while not perfect, this level of sensitivity in detecting the small proportion of patients should be a considered an excellent test in prudent clinical hands. Overall, as the cost of determining CRP level as part of normal blood work in Canada is $5.94 and the morbidity associated with the test is negligible, this a useful tool in assessing risk of postoperative infectious complication following bariatric surgery.
The findings of the present study should be interpreted with some important limitations in mind. Firstly, differences in study design and methodology limits this systematic review and meta-analysis due to the heterogeneity of the included studies. Second, there are no randomized controlled trials evaluating the use of CRP following bariatric surgery; therefore, all of the studies included were observational studies. Furthermore, we only included studies that utilized ROC analysis, which limited us to the inclusion of six observational studies, all of which were determined to be at a substantial risk of bias according to QUADAS-2. While we do not believe that the inclusion of additional studies would have significantly changed our results due to the large patient populations that were evaluated in the included studies, added studies might have allowed for CRP cutoff values to be derived for more postoperative days. In addition, added studies would have allowed for further evaluation of LOS in hospital and other patient-oriented outcomes that might have better characterized the clinical utility of CRP after bariatric surgery. Third, postoperative infectious complication is fairly rare following bariatric surgery. As such, there was a limited number of patients in the included studies that experienced postoperative infectious complication. Further multicenter studies should be conducted in order to confirm results existing in the current literature. Fourth, there is variability in the expected LOS in hospital ensuing bariatric surgery from institution to institution. Thus, it is possible that CRP cutoff values for POD 3 and POD 5 might not be appropriate for a given institution. For instance, some centers are experimenting with same-day discharge after both LSG or RYGB, despite some literature demonstrating increasing rates of complications, readmissions, and reoperations [26]. Lastly, LSG was performed much more frequently than RYGB in the included studies. While LSG has been used with increasing frequency over the past decade, RYGB still remains the most commonly performed bariatric procedure [2]. Therefore, further studies analyzing the ROC relating CRP and postoperative infectious complication following RYGB may better characterize the predictive value of CRP in bariatric surgical procedures today.
Conclusion
In conclusion, CRP can be a useful and cost-effective test to detect postoperative infectious complications following bariatric surgery when used with the cutoffs determined in this systematic review and meta-analysis. The sensitivity demonstrated on POD 1, 3, and 5 indicates that a negative CRP test can be a useful test in ruling out a postoperative infectious complication. Moreover, the high specificity demonstrated on POD 1 and 3 indicates that a positive CRP test can be useful in the early identification of patients at increased risk of postoperative infectious complication.
References
Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–9.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36.
Farrell TM, Haggerty SP, Overby DW, et al. Clinical application of laparoscopic bariatric surgery: an evidence-based review. Surg Endosc Other Interv Tech. 2009;23:930–49.
Sakran N, Goitein D, Raziel A, et al. Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients. Surg Endosc Other Interv Tech. 2013;27:240–5.
Bellorin O, Abdemur A, Sucandy I, et al. Understanding the significance, reasons and patterns of abnormal vital signs after gastric bypass for morbid obesity. Obes Surg. 2011;21:707–13.
Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc Other Interv Tech. 2012;26:1509–15.
Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111:1805–12.
Adamina M, Steffen T, Tranatino I, et al. Meta-analysis of the predictive value of C-reactive protein for infectious complications in abdominal surgery. Br J Surg. 2015;102:590–8.
Simon L, Gauvin F, Amre DK, et al. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection : a systematic review and meta-analysis. Clin Infect Dis. 2004;39:206–17.
Singh PP, Zeng ISL, Srinivasa S, et al. Systematic review and meta-analysis of use of serum C-reactive protein levels to predict anastomotic leak after colorectal surgery. Br J Surg. 2014;101:339–46.
Csendes A, Burgos AM, Roizblatt D, et al. Inflammatory response measured by body temperature, C-reactive protein and white blood cell count 1, 3, and 5 days after laparotomic or laparoscopic gastric bypass surgery. Obes Surg. 2009;19:890–3.
Albanopoulos K, Alevizos L, Natoudi M, et al. C-reactive protein, white blood cells, and neutrophils as early predictors of postoperative complications in patients undergoing laparoscopic sleeve gastrectomy. Surg Endosc Other Interv Tech. 2013;27:864–71.
Warschkow R, Tarantino I, Folie P, et al. C-reactive protein 2 days after laparoscopic gastric bypass surgery reliably indicates leaks and moderately predicts morbidity. J Gastrointest Surg. 2012;16:1128–35.
Romain B, Chemaly R, Meyer N, et al. Diagnostic markers of postoperative morbidity after laparoscopic Roux-en-Y gastric bypass for obesity. Langenbeck's Arch Surg. 2014;399:503–8.
Dib F, Parenti LR, Boutten A, et al. Diagnostic performance of C-reactive protein in detecting post-operative infectious complications after laparoscopic sleeve gastrectomy. Obes Surg. Obes Surg. 2017;27:3124–32.
Ruiz-Tovar J, Muñoz JL, Gonzalez J, et al. C-reactive protein, fibrinogen, and procalcitonin levels as early markers of staple line leak after laparoscopic sleeve gastrectomy in morbidly obese patients within an enhanced recovery after surgery (ERAS) program. Surg Endosc Other Interv Tech. 2017;31:5283–8.
Kröll D, Nakhostin D, Stirnimann G, et al. C-reactive protein on postoperative day 1: a predictor of early intra-abdominal infections after bariatric surgery. Obes Surg. 2018;28:2760–6.
Whiting P, Rutjes A, Westwood M, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol BioMed Cent. 2014;14:135.
Gordon AC, Cross AJ, Foo EW, et al. C-reactive protein is a useful negative predictor of anastomotic leak in oesophago-gastric resection. ANZ J Surg. 2018;88:223–7.
Frask A, Orłowski M, Dowgiałło-Wnukiewicz N, et al. Clinical evaluation of C-reactive protein and procalcitonin for the early detection of postoperative complications after laparoscopic sleeve gastrectomy. Videosurgery Other Miniinvasive Tech. 2017;2:160–5.
Kassir R, Blanc P, Tibalbo LMB, et al. C-reactive protein and procalcitonin for the early detection of postoperative complications after sleeve gastrectomy: preliminary study in 97 patients. Surg Endosc. 2015;29:1439–44.
Zhang K, Xi H, Wu X, et al. Ability of serum C-reactive protein concentrations to predict complications after laparoscopy-assisted gastrectomy. Medicine (Baltimore). 2016;95:1–7.
Turner PL, Saager L, Dalton J, et al. A nomogram for predicting surgical complications in bariatric surgery patients. Obes Surg. 2011;21:655–62.
Nguyen NT, Goldman CD, Ho HS, et al. Systemic stress response after laparoscopic and open gastric bypass. J Am Coll Surg. 2002;194:557–66.
Inaba CS, Koh CY, Sujatha-Bhaskar S, et al. Same-day discharge after laparoscopic roux-en-y gastric bypass: an analysis of metabolic and bariatric surgery accreditation and quality improvement program database. J Am Coll Surg. 2018;226:868–73.
Acknowledgements
We thank Andrea McLellan, an expert medical librarian, for her assistance with the literature search strategy development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yung Lee and Tyler McKechnie are joint first authors
Electronic Supplementary Material
ESM 1
(DOCX 2468 kb)
Appendix. Complete search strategy
Appendix. Complete search strategy
1 exp bariatric surgery/
2 bariatric*.mp.
3 gastroplast*.mp.
4 ((gastric or jejunoileal or jejuno-ileal or ileojejunal or ileo jejunal or gastroileal or roux-en-y) adj2bypass*).mp.
5 gastrojejunostom*.mp.
6 intestinal bypass*.mp.
7 lipectomy/
8 lipectom*.mp.
9 lipoplasty/
10 lipoplast*.mp.
11 lipolysis/
12 lipolysis.mp.
13 liposuction/
14 liposuction*.mp.
15 gastric band*.mp.
16 biliopancreatic bypass/
17 bilio-pancreatic diversion.mp.
18 biliopancreatic diversion*.mp.
19 exp gastrectomy/
20 gastrectom*.mp.
21 duodenal switch.mp.
22 gastric plication.mp.
23 gastric placation.mp.
24 gastric balloon/
25 gastric bubble*.mp.
26 ballobes balloon*.mp.
27 duodenal ileostomy.mp.
28 or/1-27
29 exp C-Reactive Protein/
30 CRP.mp.
31 C Reactive Protein.mp.
Rights and permissions
About this article
Cite this article
Lee, Y., McKechnie, T., Doumouras, A.G. et al. Diagnostic Value of C-Reactive Protein Levels in Postoperative Infectious Complications After Bariatric Surgery: a Systematic Review and Meta-Analysis. OBES SURG 29, 2022–2029 (2019). https://doi.org/10.1007/s11695-019-03832-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03832-5