Abstract
Introduction
Endoscopic gastroplasty and gastric volume reduction techniques have been shown to achieve significant weight loss and improvement in comorbid conditions. The objective of this study is to assess the feasibility and safety of a novel fully automated, operator-independent endoscopic suturing system (EndoZip™) for minimally invasive treatment of obesity.
Design
Single-center pilot feasibility study.
Patients
Eleven patients with a body mass index (BMI) of 30 to 40 kg/m2 with or without obesity-associated comorbidity.
Interventions
Gastric volume reduction with EndoZip™ system.
Main Outcome Measurements
Primary outcome was to assess the technical feasibility and safety. The secondary outcome was to determine %total body weight loss (TBWL) and %excess weight loss (EWL) at 6 months.
Results
The mean ± SD age was 42.7 ± 5.6 years, and the mean ± SD BMI was 36.9 ± 2.8 kg/m2. A majority (64%) were men. The procedure was technically successful (100%) in all patients. A median of 3 (range, 2–4) full-thickness sutures were placed, and the mean procedure time was 54.6 ± 23.9 (23–100) min. No immediate complications occurred, and all were discharged in 24 h. One patient developed respiratory infection 3 days after the procedure and required hospitalization. The infection was mild and resolved with antibiotic treatment. At 6-month follow-up, the mean ± SD TBWL, %TBWL, and %EWL were 17.8 ± 6.7 kg, 16.2 ± 6.0%, and 54.3 ± 28.4%, respectively (p < 0.001).
Limitations
Limited number of patients.
Conclusion
Our first-in-human study showed that the Endozip™ device could be safely used for the treatment of obesity. The early weight loss results are promising. An extended feasibility study on a larger sample size is being planned (Clinicaltrials.gov. NCT03472196).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic gastroplasty techniques have gained wider acceptance and are evolving to become a mainstream treatment option for obesity [1, 2]. Several studies have established its safety, feasibility, reproducibility, and medium-term efficacy [3,4,5,6]. Endoscopic gastroplasty using the overstitch device has shown to achieve more total body weight loss as compared with high-intensity diet and lifestyle therapy and intragastric balloons [7, 8]. The weight loss effect sustained up to 24 months (20.9%) [9]. The mechanistic studies have established that imbricating different walls of the stomach in an endoscopic gastroplasty procedure alters the gastric motility, induces satiation, and results in weight loss [10]. Despite the promising results, the expertise to perform such procedure is not widely available, and only a few centers lead these endoscopic treatments. The frequently cited reasons are (a) complexity with the procedure, (b) steep learning curve, (c) long procedure time, (d) uncertainty on suture depth, and (e) lack of trained assistance [11,12,13,14,15].
Newer devices and techniques analogues to the bariatric surgical procedures are in a different phase of development to provide a tailored approach to obesity treatment. They target both the restrictive and malabsorptive mechanism described with the surgical techniques [16,17,18]. The early results so far appear encouraging. However, some of these techniques are more challenging, requiring even higher levels of operator dexterity [18, 19]. This may limit their widespread dissemination and adoption as a treatment option for the obesity pandemic. There is a clear need for the development of a device that is easy to use, safe, efficacious, and consistently delivers full-thickness sutures, and, at the same time, requires only a shorter learning curve to master the technique.
Recently, a new endoluminal-sutured gastroplasty system (EndoZip™, NitiNotes Surgical, Caesarea, Israel) has been developed to ease the complexity associated with existing endoscopic gastroplasty devices. It is a fully automated, operator-independent, and a minimally invasive suturing system that is postulated to create durable restrictive sutures in the stomach. Animal and bench studies have shown that the device is capable of approximating the gastric tissue segments (anterior, greater curve, and posterior segments) and restrict the gastric lumen effectively. We performed a first-in-human study to assess the technical feasibility of this novel device to treat obesity. We report the feasibility and safety data with this new procedure.
Methods
Trial Design
We conducted a prospective single-center study at the Bariatric Endoscopy unit of HM Sanchinarro University Hospital, Madrid, Spain, between May and November 2018. The institutional review board approved the study. All authors had access to the study data and reviewed and approved the final manuscript (Clinicaltrials.gov, NCT03472196). The study was conducted in accordance with the ethical principles detailed in the Declaration of Helsinki and was consistent with the Good Clinical Practices recommendation. We reported our outcome according to the CONSORT recommendation of reporting a trial.
Participants
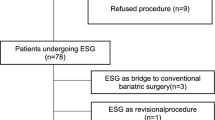
The study involved three distinctive phases: (a) screening, (b) intervention, and (c) follow-up.
Screening Phase
We screened 14 patients and identified 13 eligible candidates for endoscopic treatment of obesity after failed diet and lifestyle therapy. We excluded one as the patient was non-committal to post-procedure follow-up. We explained the risks and benefits of the procedure and obtained informed consent from the patients. We included patients (1) age older than 18 years, (2) able to comply with the procedure and provide informed consent, (3) BMI of 30–40 kg/m2, (4) failed to achieve significant weight change (± 5% of total body weight) with standard medical therapy during 6 months prior to enrollment, and (5) fully ambulatory, without chronic reliance on walking aids.
We excluded those with (1) previous bariatric, gastric, or esophageal surgery; (2) gastrointestinal conditions like hiatus hernia (> 5 cm), severe GERD, Barrett’s esophagus, esophageal stricture, Zenker’s diverticulum, achalasia, peptic ulcer disease, gastrointestinal tumors, esophageal or gastric varices, portal gastropathy, or gastroparesis, and intestinal obstruction; (3) poorly controlled diabetes mellitus or change in diabetes medications/dosage in the previous 3 months before enrollment; (4) uncontrolled hypertension; (5) heart failure, NYHA grade 2 and above; (6) chronic obstructive pulmonary disease (COPD); (7) renal and/or hepatic insufficiency/disease (creatinine above 1.5 mg/dL); (9) uncontrolled thyroid disease; (10) pregnancy; (11) coagulopathy; (12) immunosuppressive therapy; (13) poorly controlled psychiatric disease; (14) chronic drugs or alcohol abuse; (15) malignancy; (16) participating in another clinical study with an investigational new drug, biological, or therapeutic device within 6 months prior to enrollment in this study; and (17) unable to discontinue either prescription or over the counter weight loss medications for at least 30 days prior to the procedure.
Intervention
The EndoZip™ System
The Nitinotes EndoZip™ system is designed to create multiple internal gastric segmentation by approximating the opposing wall of the stomach using an endoscopic approach.
The EndoZip™ insertion tube contains 6 disposable components: (a) distal bougie, (b) endoscope port designed for an ultrathin upper endoscope, (c) needle retriever, (d) needle driver, (e) working channel, and (f) vacuum port. The device is embedded with a custom-designed, auto-driven, helical needle and utilizes a 2–0 USP polypropylene suture for plication (Fig. 1).
Procedure
A single endoscopist performed all the procedures. The endoscopist underwent extensive training to become familiar with the steps of EndoZip™ system before starting in humans. The training was conducted on ex vivo animal models and post-sleeve gastrectomy explants to understand and learn the necessary steps and maneuvers of EndoZip™. Following this, further training was held on the in vivo pig model to achieve competency and to plan the suture pattern before the application of this technique in human cases (Fig. 2).
We performed the procedure with the patient under general anesthesia and used CO2 for insufflation. We administered antibiotics before starting the procedure. We performed an upper endoscopy to examine the stomach and to identify conditions that would restrict EndoZip™ application. We always used an overtube to facilitate easy insertion of the EndoZip™ system. After the introduction of the system, we identified the site for suture, typically along the greater curvature. We started at the distal body and then progressed proximally. Based on the gastric orientation, we placed the device nearer to the anterior wall or the posterior wall of the body. We then applied suction using a specialized suction device to achieve a manometric measurement of 70 kpa and decompressed the gastric lumen. This converged the opposite gastric walls into the bougie and created a stricture like segmentation of the stomach. After achieving this, the automated helical needle loaded with a polypropylene suture was driven through the gastric tissue within the bougie from the distal to the proximal end, creating a continuous suture.
The needle was retracted, and the commercially available cinching device was used to tighten and plicate the approximated tissue segments. We then removed the EndoZip™ device and confirmed the plication using an endoscope. The number of sutures placed depends on the size and anatomy of the stomach and the flexibility of this first generation suturing device (Fig. 3).
Gastric plication using the EndoZip™ system. a The device is introduced through an overtube and placed along the greater curve. b The air is suctioned utilizing a vacuum system, and the gastric lumen is decompressed. The opposing gastric walls converge inside the bougie. c The automated helical needle loaded with the polypropylene suture is driven through the gastric tissue within the bougie from the distal end to the proximal end. d A continuous running helical suture with 4 circumferential turns per suture is created. e The helical needle is retracted and removed. f Using a commercially available cinching device, the opposing walls are tightened and cinched to form a plication
Follow-up
The patients were followed bi-weekly post-procedure by a nutritionist, psychologist, and physiotherapist (optimal-24 visits). The follow-up program comprised of dietary instructions, psychological support, physical activity, and a planned counseling schedule, as well as a timeline for future visits.
The body requirements and individual taste preferences were taken into account in designing hypocaloric diets. The energy requirements were calculated from the Harris-Benedict formula and, according to the type of physical activity, were decreased by about 2.6 MJ/day to induce an approximate loss of between 0.5 and 1 kg/week. In the first month, we maintained the patients on a strict liquid diet (4 weeks). We subsequently escalated the intake to semi-solid and solid food as tolerated. The diet was the Mediterranean type in which the distributions of the principal components were as recommended by the Spanish Society of Community Nutrition [20]. We devised an individualized exercise plan (aerobic or resistance training—30 min/day) depending on the capacity of the patients and avoided an increase in intra-abdominal pressure during the first month. We encourage walking in the initial phase and then progressively increased the intensity of exercise.
At 1 month and 6 months, we performed an endoscopy to assess the integrity of the sutures. We defined intact suture as the ability to identify the approximated gastric tissue with a visible suture track or the cinch.
Statistical Methods
This was a prospective pilot study in human subjects; thus, no power calculations were performed a priori. We expressed the continuous variables as mean ± standard deviation (SD) or median (range) and categorical variables as a percentage. We used paired Student’s t test for comparison of weight loss outcomes at baseline and 6 months after the procedure. All variables were tested for normality using the Shapiro-Wilk test. A p < 0.05 was considered to be significant.
Outcomes
The primary outcome was to assess the technical feasibility and safety of the EndoZip™ system to treat obesity. Our secondary outcome was to report the efficacy of treatment as measured by %total body weight loss (%TBWL) and %excess weight loss (%EWL) at 6 months. We evaluated the stability of sutures and presented the suture durability data at 1 month and 6 months. We reported the adverse events according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) Version 4.03.
We also collected patients’ gastrointestinal symptoms at baseline and 6 months after the procedure to assess quality of life following the procedure. Patients were asked to grade their symptoms on a scale from 0 to 5, where 0 is no symptom, and 5 is severely suffering from the symptom. Symptom list included nausea, upper abdominal pain, bloating, heartburn, reflux, retching, and vomiting.
Results
Patient Characteristics
Of the enrolled 13 participants, we excluded 2 patients because of consent related issues. Eleven patients received the study procedure, and the majority were men (n = 7, 64%). The mean ± SD age was 42.7 ± 5.6 (range, 35–51) years, and the mean ± SD BMI was 36.9 ± 2.8 kg/m2 (Table 1). The procedure was technically successful in all patients (100%). There was no device failure. A median of 3 (range, 2–4) suture was performed. The mean ± SD procedure time was 54.6 ± 23.9 (23–100) min. There were no intraprocedural complications. In the immediate post-procedure period, 50% required analgesics for pain, and 10% required anti-emetics. The medications were subsequently discontinued within 10 days. The average length of stay was 1 day. However, one patient (age, 44 years; diabetes mellitus) was admitted 2 days after the procedure for chest pain, dyspnea, and hemoptysis. He was treated for respiratory infection with antibiotics and was discharged within 48 h. The respiratory infection was categorized as mild and was attributed to the general anesthesia and/or the procedure.
Weight Loss Results
All eleven patients adhered until 6-month follow-up and achieved significant weight loss (p < 0.001) (Table 2). The mean ± SD TBWL at 3 months and 6 months was 14.8 ± 4.8 kg and 17.8 ± 6.7 kg, respectively. The mean ± SD %TBWL at 3 months and 6 months was 13.5 ± 4.7% and 16.2 ± 6.0%, and the mean ± SD %EBWL was 46.5 ± 28.6% and 54.3 ± 28.4%, respectively.
Suture Durability
All patients underwent endoscopic evaluation at 1 month and 6 months to assess for suture durability (Fig. 4). Most patients (n = 9, 82%) had intact sutures at 1 month and 6 months (n = 8, 73%). In two patients, we placed 4 sutures during the index procedure and observed 3 during the endoscopic assessment at 1 and 6 months. In the third patient, we identified only two of the three sutures, although all of them were intact at the 1-month examination. In all these 3 patients, a linear scar could be identified despite the absence of visible suture or cinch suggesting changes at the deeper layers of the stomach. We observed similar weight loss in those with and without intact sutures (16.5% vs. 15.4%, p = 0.78).
Endoscopic appearance and durability of sutures after EndoZip™ in a study patient. a–c Endoscopic view of the stomach after EndoZip procedure. Three sutures were placed in the distal to the proximal gastric body. d–f All the sutures were durable at 1 month. Long segment mucosal bridging can be appreciated. g–i At 6 months, all the sutures continued to remain intact. The cinch and the visible suture track can be observed. The narrowed configuration of the gastric lumen was maintained
Symptom Response
We found no significant change in gastrointestinal symptoms as compared with the baseline in most patients. One patient reported improvement in 3 symptoms that he suffered before the procedure—heartburn, bloating, and upper abdominal pain. A second patient reported improvement in abdominal bloating.
Discussion
Our study shows that endoscopic gastroplasty using the EndoZip™ device is feasible for the treatment of class I and class II obesity. The early weight loss results achieved at 6 months are promising, and it may fulfill the ASGE/ASMBS minimum threshold of 25% EWL with < 5% serious adverse events at 12 months [21].
The goal of treatment in obesity management is to induce and sustain weight loss with low risk of adverse events. Bariatric surgery, although effective, is associated with a risk of complications and cannot be extended to “obese but less heavy” patients as the surgical risk overrides the gain of treatment [22, 23]. Unfortunately, this group constitutes the majority of the obese population, where effective treatment is lacking. Endoscopic techniques that can restrict the food intake or induce malabsorption may become an effective and attractive treatment option for this broader group of patients with obesity who are not suitable for bariatric surgery [24]. Endoscopic gastroplasty using the Endozip™ device shortens the greater curvature of the stomach, reduces the gastric body, and limits its distensibility, thereby, decreasing the meal volume and enabling the patients to achieve early satiety. We believe that the long transmural sutures may have impacted on the gastric emptying and contributed to weight loss in addition to the close nutritional follow-up. In our study, all the patients achieved significant weight loss at 6 months within a structured MDT follow-up program. The overall weight loss results and safety profile observed thus far are comparable with other endoscopic gastroplasty procedures.
Several endoscopic gastroplasty techniques are currently available for the treatment of obesity. In the endoscopic sleeve gastroplasty procedure using the Apollo Overstitch device, continues sutures are placed manually in the body of the stomach to create a sleeve-like configuration. The reported weight loss at 2 and 5 years are 17.6% and 14.5%, respectively [5, 25]. However, there is still a debate on the number of sutures required, the suture pattern, and the number of bites per suture needed to achieve desired weight loss. Recently, some concerns have been raised on the durability and long-term efficacy of ESG because of partial-thickness suturing and early suture loss [26]. In the primary obesity surgery endolumenal (POSE) procedure, the fundus of the stomach was approached in a retroflexed position, and preferentially plicated to reduce the accommodation. A randomized study failed to demonstrate meaningful weight loss results over a sham group [27].
Nevertheless, both the procedures are technically challenging and require specialized endoscopes and a high level of operator expertise. Saumoy et al. showed that mastery with endoscopic sleeve gastroplasty was achieved only after 55 procedures, with the first 20 cases requiring more than 100 min for completion [11]. From our extensive experience with POSE, we observed the learning curve was even steeper than ESG. Thus, the complexity of these procedures has resulted in limited widespread dissemination, and only a few centers have adopted them in clinical practice.
The novel EndoZip™ system introduces automation in endoscopic suturing to overcome the dependence on endoscopist skills and the need for specialized endoscopes. It delivers robust full-thickness sutures consistently, a feature that is key to any durable and successful EG technique. At 1 month and 6 months, most of the full-thickness sutures were still intact. The resultant gastroplasty-related anatomical changes with Endozip™ may have contributed to the significant weight loss. The duration of stay in the hospital was only 24 h, and all patients were discharged without any significant symptoms. Overall, the procedure was safe, with no serious adverse events recorded at 6 months. We observed that the learning curve can be shorter with the EndoZip™ system. The first 3 procedures required 78 min on average (range, 55–100 min) for completion. The procedure duration progressively decreased to an average of 49 min (range, 23–75 min) after 9 procedures. However, larger studies are required to confirm this finding.
Certain aspects of this first-generation automatic suturing device need further improvement. The rigidity of the EndoZip™ system restricts the maneuverability of the device within the stomach and limits the performance of multiple suture plication. Although the full thickness continuous suturing is effortless, we could only perform 2–4 sutures per patient because of the limited flexibility. Similarly, the visualization of the gastric lumen gets impaired when the vacuum is applied to approximate the opposing gastric wall inside the bougie. This lessens the precision, and, in some cases, instead of the desired anteroposterior gastric wall approximation, we only plicated the greater curvature to the posterior wall preventing the creation of a sleeve-like configuration. Lastly, the device needs to be removed and reloaded with suture after every plication. Trained assistance is required to set up the system and minimize the procedure time under anesthesia. To overcome these shortcomings, a radically new second-generation device with improved flexibility, visibility, and an enhanced motorized system to reduce the procedural steps and ease the technique, is under development.
Our study has a few limitations. The sample size was small, with limited follow-up time, and there was no control arm. All the procedures were performed only by a single endoscopist in one expert center. As it is a first-in-human study, the patients were followed up closely by the MDT, which may have impacted significantly the weight loss achieved. However, the patients enrolled in the study have failed prior diet and lifestyle therapies, and the available evidence suggests high-intensity diet, and lifestyle therapy alone is inferior in achieving significant weight loss compared with endoscopic gastric volume reduction. The results at 12 months and additional gastric motility and gastric volume assessment after the procedure may help us understand the actual efficacy of the procedure. This was only a pilot study to assess feasibility, and the preliminary results observed thus far sets the ground to perform more extensive comparative studies involving multiple centers in the future.
In conclusion, our first-in-human study has established the feasibility of the novel automated endoscopic full-thickness suturing device. This is a significant “work in progress” in obesity management, attempting to increase treatment penetration by simplifying the technique and minimizing operator dependence. In the next phase, with an improved device, we are planning an extended feasibility study on a large sample size to study the safety, long-term efficacy, changes in gastric motility, and impact on comorbidities.
Abbreviations
- TBWL:
-
Total body weight loss
- EWL:
-
Excess weight loss
- BMI:
-
Body mass index
- IGB:
-
Intragastric balloon
- ESG:
-
Endoscopic sutured gastroplasty
- SD:
-
Standard deviation
References
Abu Dayyeh BK, Rajan E, Gostout CJ. Endoscopic sleeve gastroplasty: a potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc. 2013;78:530–5.
Wallstabe I, Oberaender N, Weimann A, et al. Endoscopic sleeve gastroplasty using the novel Endomina device for morbidly obese patients. Endoscopy. 2018;50:E327–8.
Lopez-Nava G, Galvão MP, da Bautista-Castaño I, et al. Endoscopic sleeve gastroplasty for the treatment of obesity. Endoscopy. 2015;47:449–52.
Lopez-Nava G, Sharaiha RZ, Vargas EJ, et al. Endoscopic sleeve gastroplasty for obesity: a multicenter study of 248 patients with 24 months follow-up. Obes Surg. 2017;27:2649–55.
Alqahtani A, Al-Darwish A, Mahmoud AE, et al. Short-term outcomes of endoscopic sleeve gastroplasty in 1000 consecutive patients. Gastrointest Endosc. 2019;89:1132–8.
Li P, Ma B, Gong S, et al. Efficacy and safety of endoscopic sleeve gastroplasty for obesity patients: a meta-analysis. Surg Endosc. 2019 Jun;24:1–8. https://doi.org/10.1007/s00464-019-06889-6.
Cheskin LJ, Hill C, Adam A, et al. Endoscopic sleeve gastroplasty versus high-intensity diet and lifestyle therapy: a case-matched study. Gastrointest Endosc. 2019; https://doi.org/10.1016/j.gie.2019.09.029.
Fayad L, Cheskin LJ, Adam A, et al. Endoscopic sleeve gastroplasty versus intragastric balloon insertion: efficacy, durability, and safety. Endoscopy. 2019;51:532–9.
Sharaiha RZ, Kumta NA, Saumoy M, et al. Endoscopic sleeve gastroplasty significantly reduces body mass index and metabolic complications in obese patients. Clin Gastroenterol Hepatol. 2017;15:504–10.
Abu Dayyeh BK, Acosta A, Camilleri M, et al. Endoscopic sleeve gastroplasty alters gastric physiology and induces loss of body weight in obese individuals. Clin Gastroenterol Hepatol. 2017;15:37–43.e1.
Saumoy M, Schneider Y, Zhou XK, et al. A single-operator learning curve analysis for the endoscopic sleeve gastroplasty. Gastrointest Endosc. 2018;87:442–7.
Hill C, El Zein M, Agnihotri A, et al. Endoscopic sleeve gastroplasty: the learning curve. Endosc Int Open. 2017;5:E900–4.
Shahnazarian V, Ramai D, Sarkar A. Endoscopic bariatric therapies for treating obesity: a learning curve for gastroenterologists. Transl Gastroenterol Hepatol. 2019;18(4):16.
Movitz BR, Lutfi RE. Endoscopic sleeve gastroplasty: are we burning bridges? Surg Obes Relat Dis. 2017;13:2056–8.
Jirapinyo P, Thompson CC. Training in bariatric and metabolic endoscopic therapies. Clin Endosc. 2018;51:430–8.
Turkeltaub JA, Edmundowicz SA. Endoscopic bariatric therapies: intragastric balloons, tissue apposition, and aspiration therapy. Curr Treat Options Gastroenterol. 2019;17:187–201.
Goyal D, Singh VK, Amateau SK, et al. Evolution of endoscopic bariatric devices: from development to practice. Am J Gastroenterol. 2019;114:679–83.
Sullivan S, Edmundowicz SA, Thompson CC. Endoscopic bariatric and metabolic therapies: new and emerging technologies. Gastroenterology. 2017;152:1791–801.
Machytka E, Bužga M, Zonca P, et al. Partial jejunal diversion using an incisionless magnetic anastomosis system: 1-year interim results in patients with obesity and diabetes. Gastrointest Endosc. 2017;86:904–12.
Grupo Colaborativo de la Sociedad Española de Nutrición Comunitaria (SENC, Aranceta Bartrina J, Arija Val V et al. Dietary guidelines for the Spanish population (SENC, December 2016); the new graphic icon of healthy nutrition. Nutr Hosp. 2016; 33: 1–48.
ASGE Bariatric Endoscopy Task Force and ASGE Technology Committee, Abu Dayyeh BK, Kumar N, et al. ASGE Bariatric Endoscopy Task Force systematic review and meta-analysis assessing the ASGE PIVI thresholds for adopting endoscopic bariatric therapies. Gastrointest Endosc. 2015;82:425–38.e5.
Aurora A, Khaitan L, Saber A. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc. 2012;26:1509–15.
Elms L, Moon R, Varnadore S, et al. Causes of small bowel obstruction after roux-en-Y gastric bypass: a review of 2,395 cases at a single institution. Surg Endosc. 2014;28:1624–8.
Jirapinyo P, Thompson CC. Endoscopic bariatric and metabolic therapies: surgical analogues and mechanisms of action. Clin Gastroenterol Hepatol. 2017;15:619–30.
Hajifathalian K et al. Long-term follow up and outcomes after endoscopic sleeve gastroplasty for treatment of obesity (5 year data). Gastrointest Endosc. 89(6):–AB58.
Alqahtani AR, Elahmedi M, Alqahtani YA, et al. Laparoscopic sleeve gastrectomy after endoscopic sleeve gastroplasty: technical aspects and short-term outcomes. Obes Surg. 2019. Obes Surg. 2019;29:3547–52.
Sullivan S, Swain JM, Woodman G. Randomized sham-controlled trial evaluating efficacy and safety of endoscopic gastric plication for primary obesity: the ESSENTIAL trial. Obesity (Silver Spring). 2017;25:294–301.
Funding
The study was sponsored by Nitinotes Surgical Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Gontrand Lopez-Nava is a consultant for Nitinotes Surgical, Apollo Endosurgery, and USGI Medical. Dr. Barham Abu Dayyeh is a consultant for Boston Scientific, Metamodix, BFKW, USGI Medical and Nitinotes Surgical. All other authors have no disclosure.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethics Approval
The study was conducted following the good clinical practice guidelines and adhered to the recommendation of the declaration of Helsinki. The institutional review board approved the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lopez-Nava, G., Asokkumar, R., Rull, A. et al. Safety and Feasibility of a Novel Endoscopic Suturing Device (EndoZip TM) for Treatment of Obesity: First-in-Human Study. OBES SURG 30, 1696–1703 (2020). https://doi.org/10.1007/s11695-019-04370-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04370-w