Abstract
Background
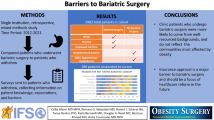
Despite an increase in bariatric surgery across Quebec, Canada, access is still limited. Furthermore, there are differences in resources and multidisciplinary capabilities of providing centers that may impact quality of care and outcomes.
Methods
We performed an online survey of all bariatric surgeons in the province of Quebec, Canada, using the LimeSurvey software.
Results
Forty-six surgeons from 15 centers were surveyed. Response rate was 87% (n = 40). Only 13 (35%) surgeons have any formal fellowship training in bariatric surgery and 74% perform > 50 cases/year. All surgeons perform sleeve gastrectomy, 34% do duodenal switch, and 44% provide major revisions. Thirty-one surgeons (77%) identified access to operating room as the main cause for surgical delays. While most surgeons (52%) considered < 6 months as an acceptable wait-time, only 33% achieved this in their practice. Majority (70%) favored a centralized provincial referral system. Patient’s geographical convenience, procedural choice, and multidisciplinary capabilities of providing centers are identified as important determinants for centralized referrals (93, 78, and 55%, respectively). Virtually, all supported accreditation/designation of centers and creation of Quebec Bariatric Network for quality control and research (85 and 98%, respectively).
Conclusion
Bariatric surgical patterns vary among designated centers in Quebec, Canada. Access to multidisciplinary care and surgeon’s fellowship training may be contributing factors for the observed variability. Wait-lists are long and timely access to surgery remains an issue. There is near consensus for establishing a centralized referral system, designation of referral vs. primary centers, and creating Quebec Bariatric Network for research and quality control.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity is a major public health problem worldwide. It is currently estimated that nearly one out of four Canadian is obese [1]. Obesity and its associated comorbidities result in significant loss of disability-adjusted life years, mortality, and increase in healthcare cost [2,3,4]. Bariatric surgery is the cornerstone of treatment of obesity and related diseases [5,6,7]. As a result, bariatric surgery has been increasingly performed in North America, and attempts have been made to increase access to surgery in Canada especially the province of Quebec [8, 9].
In 2009, Quebec’s Ministry of Health enacted a series of actions to improve access to bariatric surgery and increased the number of surgical sites across the province. The ministry opened five new bariatric centers in regional Quebec, named two hospitals as centers of excellence and introduced measures to increase surgical volume in all existing centers [10]. Despite these efforts, surgical wait-lists remain long in most centers, and timely access to definitive care is limited and impacted by various center-dependent capabilities and practice patterns. Also in 2009, a neighboring Canadian province, Ontario, instituted a more comprehensive reform of the bariatric surgery system with the creation of the Ontario Bariatric Network (OBN). OBN accredits centers of excellence, manages a common patient registry for quality improvement and research, and manages a centralized Web-based referral system [11].
Hence, we sought to investigate the differences in practice patterns among bariatric surgeons in Quebec. In addition, we aimed to evaluate the differences in resources and multidisciplinary capabilities of bariatric centers that may impact quality of care. Finally, we inquired about potential areas in need of improvement by surveying all the bariatric surgeons in the province.
Methods
In March 2017, an online survey was created using “LimeSurvey Version 2.63” with online responses hosted on McGill University’s servers. Questions were designed to evaluate resources, training, practice patterns, and opinions of bariatric surgeons regarding areas in need of improvement. The single link to the survey was distributed via email to all bariatric surgeons of the 15 designated bariatric centers in the province of Quebec, Canada. A second reminder email was sent a week later to improve response rate. The survey remained open for answers for 1 month. The study was approved by the institutional Ethics Review Board.
From the 15 individual providing centers, 2 are surgery-alone satellite sites of larger institutions and are used by the same respective surgeons for less complex cases. Thus, with respect to bariatric center-dependent descriptive statistics, proportions and frequencies are calculated using 13 as the total number for the providing centers. The anonymous results were compiled, and descriptive statistical analyses were carried out using the STATA software (Stata Corp, Texas, USA) version 12. Inference is based on a two-sided 5% level.
Results
Forty-six surgeons were surveyed and the response rate was 87% (n = 40). Thirteen (35%) of the surgeons completed at least a 1-year fellowship or received some additional training in bariatric surgery. Regarding surgeon-specific volume, 74% (n = 28) reported that they perform ≥ 50 bariatric cases, and 35% carry out ≥ 100 cases per year. While all surgeons perform sleeve gastrectomy, only 55% (n = 21) do gastric bypass, and 34% (n = 13) perform duodenal switch. The detailed reported variability among the surgeons with respect to the number and the type of bariatric procedures performed annually is provided in Table 1.
With respect to center-specific surgical volume, 38% (n = 5) are very high-volume centers performing ≥ 300 bariatric surgeries per year. In terms of multidisciplinary capabilities, multiple resources were identified by the respondents as being necessary to a bariatric surgery program. All surgeons agreed on the need for dedicated bariatric nurse and nutritionist, and 92% of centers (n = 12) have access to these services. However, only 38% (n = 5) have a dedicated psychologist, 31% (n = 4) have a dedicated endocrinologist, and only 54% (n = 7) are equipped with a prospective bariatric data registry. Table 2 shows in detail the surgeon-reported variability in center-specific multidisciplinary capabilities.
Regarding access to bariatric surgery and surgical delays, while 53% (n = 21) of surgeons agree that an acceptable wait-list should be ≤ 6 months, only 33% (n = 13) report achieving it. Furthermore, 28% (n = 11) of surgeons report wait-times longer than 12 months. The most important factors reported by the surgeons for long delays were access to the operating room (78%; n = 31), availability of other healthcare specialists such as a dedicated bariatric nutritionist (58%; n = 23), and other medical consultants (35%; n = 14). Table 3 shows the determinants of delays in access to bariatric surgery as reported by the surgeons.
Finally, with respect to quality of care improvement initiatives, 70% of surgeons (n = 28) support the implementation of an online province-wide centralized referral system for bariatric surgery. Surgeons agree that the referral should be based on patient’s geographical convenience and distance to a providing center (93%; n = 37), patient’s choice for a given type of surgery (78%; n = 31), and based on center-specific multidisciplinary capabilities (55%; n = 22). Majority of surgeons support the creation of an accreditation system for center classification/designation, e.g., referral vs. primary sites based on expertise, multidisciplinary capabilities, and surgical volume (85%; n = 34). Virtually, all surgeons support the creation of a provincial bariatric network to enable data collection for ongoing research and quality control (98%; n = 39). A detailed list of potential areas in need of improvement in bariatric care as reported by surgeons is provided in Table 4.
Discussion
This study surveys all practicing bariatric surgeons in Quebec with a response rate of 87%. These surgeons practice at all known 15 providing centers in a single payer system within the province. Thus, given the excellent response rate, our study is a suitable representation of the current landscape of bariatric surgery from the point of view of the respective surgeons practicing in the province.
Regarding surgeon-specific variability in practice patterns, almost 75% of surgeons perform ≥ 50 bariatric procedures per year where sleeve gastrectomy comprises more than half of these surgeries. This finding is in keeping with current trends in other North American studies [12, 13]. Recently, Khorgami et al., using data from the American College of Surgeons National Surgical Quality Improvement Program, reported a sharp rise in sleeve gastrectomies to 58% of all primary bariatric procedures performed with a decline in gastric bypass to 29% [13]. Furthermore, our survey demonstrated that while gastric bypass comprised over 20% of bariatric procedures, duodenal switch consisted nearly 10% of all bariatric procedures and represented a third of all diversionary-type procedures performed in Quebec. Also, 18% of surgeons perform > 10 duodenal switch cases annually which may even underestimate the overall number since surgeons in at least three major centers also perform the single-anastomosis duodenal switch also known as single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) [14]. The higher frequency of diversionary-type procedures, especially duodenal switch, could partly be explained by Quebec being home to two of the pioneers of the duodenal switch procedure [15].
As depicted in Table 1, there is a major variability among surgeons regarding the number and types of bariatric procedures performed annually. Our survey demonstrated that only 35% of the respondents have obtained a formal fellowship or any dedicated training in bariatric surgery; the rest are all general surgeons who are grandfathered into performing bariatric surgery or have likely learned on-the-job from formally trained colleagues. In univariate analysis, we found that surgeons who completed a dedicated training in bariatric surgery were significantly more likely to perform diversionary-type procedures (analysis not shown in the results). Also, very high-volume university centers where > 300 bariatric surgeries were performed every year were found to perform significantly more anastomotic procedures (univariate analysis not shown in the results). These findings are not surprising. In fact, Doumouras et al. recently showed that health outcomes of 18,398 patients, who underwent bariatric surgery across Canada during 2008 until 2015, were better when the procedure was carried out at a high-volume center and by a surgeon who also had a high surgical volume [16]. Gastric bypass accounted for nearly 77% of all procedures and for each increment of 25 bariatric cases per year by a surgeon, the odds of all-cause morbidity was 0.94 times lower; furthermore, high-volume university centers also conferred a 0.75 lower odds [16]. Hence, higher surgeon and center volumes as well as surgeon’s bariatric fellowship training are not only likely to increase the frequency of diversionary-type procedures but also improve the respective outcomes as shown by multiple studies [17,18,19].
Center-specific variability in bariatric surgery and the respective multidisciplinary capabilities could also potentially impact outcomes. We found that while greater majority of providing sites have access to dedicated bariatric nursing and nutritionists, interventional radiology, and gastroenterology, more than half lack access to other important multidisciplinary care such as dedicated psychologist/social worker, endocrinologist, and bariatrician. Also, only 54% of centers are equipped with a prospectively kept bariatric database. Furthermore, following the expansion of the number of providing centers after the 2009 initiative by Quebec’s Ministry of Health [10], almost a third of the current bariatric surgeons work at newly added low-volume centers. Surgical outcomes are most likely impacted by such circumstances. The role of center accreditation to improve bariatric outcomes has been shown in several studies [20,21,22]. In addition, a recent study using the claims data of more than 145,000 patients who underwent bariatric surgery at centers of excellence during 2010 and 2013 showed that risk and reliability-adjusted serious complications varied 17-fold at each center [23]. High-volume centers (> 448 mean cases/year) had the lowest frequency and variation in their respective postoperative complications [23]. Hence, one way to provide the best possible care at all sites would be by accrediting different sites and designating centers to carry out specific missions especially in terms of set numbers and types of bariatric procedures to be performed. For instance, designated primary care facilities would provide less complex primary bariatric surgery and referral centers would be equipped to provide more complex bariatric procedures either primary or revisional and to more medically complex patients. This approach would likely have a positive impact on the access to bariatric surgery as well.
Timely access to surgery is an important quality indicator. We found that while more than half of surgeons agreed that after the initial visit an acceptable time to surgery should be ≤ 6 months, only a third were able to achieve it and another third described wait-times > 12 months. Furthermore, according to the official website of Quebec’s Health Ministry that tracks center-specific wait-times for elective surgeries in 9-month blocks, the percentage of patients waiting for bariatric surgery who go on to receive the treatment within 6 months of being listed can be as low as 36% [24]. The mean wait-time among the 15 surgical sites is 5 months and ranges from 1 month to a year [24]. These estimates are from the April 2017 to January 2018 period, which reflects the time period after the survey. However, the wait-times have not drastically changed for each center compared to the previous 9-month block. Also, the center-dependent wait-times do not always accurately reflect surgeon-specific wait-times which can be even longer. The long wait-lists are despite the 2009 initiative by Quebec’s Ministry of Health to increase the number of bariatric centers in the province and the absence of preoperative dietary requirement by the single payer system unlike the situation in the USA. We found that while the most limiting factor was access to the operating room, more than a third of surgeons attributed their surgical delays to lack of access to multidisciplinary capabilities, mainly dedicated nutritionists and other medical consultants. Similar to Quebec, in 2009, the neighboring province of Ontario also expanded the number of bariatric centers but simultaneously restructured the entire bariatric care network [11]. In Quebec, the government opted to improve access by allowing new centers closer to various communities to perform bariatric surgery, whereas in Ontario, bariatric surgery was centralized to few centers of excellence in high-volume institutions while creating regional assessment treatment centers to capture the population outside those centers and provide the non-surgical aspect of obesity treatment around the bariatric procedure performed in a remote center of excellence [11]. Consequently, the center designation/regionalization is shown to enhance access to surgery and efficiency of bariatric care across Ontario, lower postoperative use of hospital services, and improve short- and long-term outcomes [25,26,27]. Our survey showed that 85% of bariatric surgeons in Quebec agree with accrediting centers and designating them to achieve certain objectives.
Patient referral for bariatric surgery is another important area in need of improvement. While access to surgery has significantly increased in Quebec, only an average of 10 per 1000 obese patients in the province receive surgery [28]. Consults from primary care physicians or other specialists are mostly underused but often misplaced or duplicated to multiple centers, which in turn causes a ripple effect by prolonging surgical wait-lists at multiple centers. We found that 70% of surgeons agreed on centralizing the referral system within the province. Virtually, all surgeons thought that the referral system should be based on patient’s geographical convenience to the closest center and 78% believed that referrals should take into account the patient’s procedure choice. Moreover, half or more of surgeons thought that the respective institutional wait-lists for a given procedure and their multidisciplinary capabilities should be used in the centralized referral algorithm. In 2015, the OBN completely switched from a fax-based system to a centralized online referral system for bariatric surgery; Doumouras et al. showed that implementation of centralized online referral system more than doubled the consults across all health regions [29]. Referring physician education and proximity to providing centers were also found to be important factors in optimizing referrals [29]. Thus, a more selective referral sent via a centralized online system is likely to improve access to surgery, lower duplication of consults, and allow for an efficient use of resources in designated centers.
Finally, we found that there appears to be a consensus among the surgeons who are virtually all in favor of creating a centralized provincial bariatric network. Such standardized network would be similar to OBN and would enable implementation of quality control initiatives, collection of data for ongoing research, and ultimately improvement of bariatric care delivery and outcome [25, 27].
This survey has certain limitations. The information obtained may be subject to recall bias and reflect the surgeon’s perception of their respective practice which may differ from the reality if compared to administrative data. Despite obtaining a high response rate, the state of bariatric surgery in Quebec cannot be illustrated solely based on the survey results from the bariatric surgeons. Moreover, due to the small sample size of the surgeons and the centers in Quebec, no inferential statistical analyses were reported. The particularity of the single payer system and associated health policies may make these results difficult to extrapolate to different health systems. However, as a Canadian province, Quebec provides a unique opportunity to naturally exclude confounders such as insurance status, hospital ownership, and lack of access on comparisons between hospitals and surgeons in assessing bariatric surgery outcomes. In addition, a small number of bariatric procedures performed outside the public system in independent private clinics are not unaccounted for in this survey. This group, however, represents a small number of cases in the province.
Conclusions
Bariatric surgical patterns vary among designated centers in Quebec, Canada. Access to multidisciplinary care and surgeon’s fellowship training may be contributing factors for the observed variability. Wait-lists are long, and timely access to surgery especially for certain procedures remains an issue. In terms of quality improvement initiatives, there is near consensus for establishment of a centralized referral system, designation of referral vs. primary centers, and creation of Quebec Bariatric Network for quality control and ongoing research.
References
Navaneelan T, Janz T. Adjusting the scales: obesity in the Canadian population after correcting for respondent bias. Statistics Canada. May 2014; catalogue no. 82-624-X. Health at a Glance
Collaborators GBDO, Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration, Lu Y, Hajifathalian K, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383(9921):970–83.
Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–25.
Pajecki D, Dalcanalle L, Souza de Oliveira CP, et al. Follow-up of roux-en-Y gastric bypass patients at 5 or more years postoperatively. Obes Surg. 2007;17(5):601–7.
Sjostrom L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. Int J Obes. 2008;32(Suppl 7):S93–7.
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240(3):416–23. discussion 23-4
Bariatric Surgery in Canada. Canadian Institute for Health Information. 2015. Available at: https://www.cihi.ca/en/bariatric-surgery-in-canada-infographic. Accessed 01 Dec 2017.
Canadian Obesity Network-Réseau canadien en obésité. Report Card on Access to Obesity Treatment for Adults in Canada 2017. Canadian Obesity Network Inc 2017. Available at: http://www.obesitynetwork.ca/files/FULLREPORTfinalENG.pdf. Accessed 01 Dec 2017.
L’organisation de la chirurgie bariatrique au Québec: Plan d’action. La Direction des communications du ministère de la Santé et des Services sociaux du Québec. 2009. Available at: http://publications.msss.gouv.qc.ca/acrobat/f/documentation/2009/09-932-01.pdf. Accessed 01 Dec 2017.
Ontario Bariatric Network: Surgical program. 2015. Available at: http://www.ontariobariatricnetwork.ca/our-programs/surgical-program. Accessed 01 Dec 2017.
Abraham A, Ikramuddin S, Jahansouz C, et al. Trends in bariatric surgery: procedure selection, Revisional surgeries, and readmissions. Obes Surg. 2016;26(7):1371–7.
Khorgami Z, Shoar S, Andalib A, et al. Trends in utilization of bariatric surgery, 2010-2014: sleeve gastrectomy dominates. Surg Obes Relat Dis. 2017;13(5):774–8.
Sanchez-Pernaute A, Herrera MA, Perez-Aguirre ME, et al. Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up. Obes Surg. 2010;20(12):1720–6.
Marceau P, Biron S, Bourque RA, et al. Biliopancreatic diversion with a new type of gastrectomy. Obes Surg. 1993;3(1):29–35.
Doumouras AG, Saleh F, Anvari S, et al. The effect of health system factors on outcomes and costs after bariatric surgery in a universal healthcare system: a national cohort study of bariatric surgery in Canada. Surg Endosc. 2017;31(11):4816–23.
Ali MR, Tichansky DS, Kothari SN, et al. Validation that a 1-year fellowship in minimally invasive and bariatric surgery can eliminate the learning curve for laparoscopic gastric bypass. Surg Endosc. 2010;24(1):138–44.
Agrawal S. Impact of bariatric fellowship training on perioperative outcomes for laparoscopic roux-en-Y gastric bypass in the first year as consultant surgeon. Obes Surg. 2011;21(12):1817–21.
Aminian A, Chaudhry RM, Khorgami Z, et al. A challenge between trainee education and patient safety: does fellow participation impact postoperative outcomes following bariatric surgery? Obes Surg. 2016;26(9):1999–2005.
Jafari MD, Jafari F, Young MT, et al. Volume and outcome relationship in bariatric surgery in the laparoscopic era. Surg Endosc. 2013;27(12):4539–46.
Gebhart A, Young M, Phelan M, et al. Impact of accreditation in bariatric surgery. Surg Obes Relat Dis. 2014;10(5):767–73.
Azagury D, Morton JM. Bariatric surgery outcomes in US accredited vs non-accredited centers: a systematic review. J Am Coll Surg. 2016;223(3):469–77.
Ibrahim AM, Ghaferi AA, Thumma JR, et al. Variation in outcomes at bariatric surgery centers of excellence. JAMA Surg. 2017;152(7):629–36.
Access to specialized medical services-Bariatric surgery. 2018. Available at: http://wpp01.msss.gouv.qc.ca/appl/g74web/carte.asp. Accessed January 25, 2018.
Saleh F, Doumouras AG, Gmora S, et al. Outcomes the Ontario bariatric network: a cohort study. CMAJ Open. 2016;4(3):E383–E9.
Elnahas A, Jackson TD, Okrainec A, et al. The effect of the Ontario bariatric network on health services utilization after bariatric surgery: a retrospective cohort study. CMAJ OpenS. 2016;4(3):E489–E95.
Aird LN, Hong D, Gmora S, et al. The impact of a standardized program on short and long-term outcomes in bariatric surgery. Surg Endosc. 2017;31(2):801–8.
Sharma AM. Inequalities in access to bariatric surgery in Canada. CMAJ. 2016;188(5):317–8.
Doumouras AG, Anvari S, Breau R, et al. The effect of an online referral system on referrals to bariatric surgery. Surg Endosc. 2017;31(12):5127–34.
Acknowledgements
This study was accepted for a poster presentation during the Canadian Association of Bariatric Physicians and Surgeons (CABPS) 2017 meeting, in Niagara Falls, ON, Canada.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Andalib, A., Bouchard, P., Bougie, A. et al. Variability in Bariatric Surgical Care Among Various Centers: a Survey of All Bariatric Surgeons in the Province of Quebec, Canada. OBES SURG 28, 2327–2332 (2018). https://doi.org/10.1007/s11695-018-3157-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3157-4