Abstract
Background
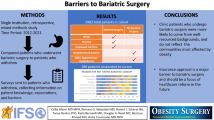
The Ontario Bariatric Network implemented an online referral system to completely replace a fax-based system in 2015. Strategies such as electronic information transfer have been suggested to improve the bariatric referral process but few studies exist demonstrating their efficacy. Therefore, the purpose of this study was to determine the impact on referral rates to bariatric surgery after converting to an online referral system from a fax-based system.
Methods
All referrals from 2011 to 2015 were included in the study. The main outcomes included the total number of referrals and whether a practitioner increased referrals after the implementation of the online referral system. A hierarchical logistic regression model was used for the final analysis. Predictors of interest included physician and neighbourhood level factors
Results
Referrals more than doubled overall and increased significantly across all health regions. Compared to practitioners in their first five years, all other experience groups were approximately 50% less likely to increase referrals. Compared to those within 50 km of a bariatric facility, practitioners 50–99 km (OR 0.76 95% CI 0.58–0.98 p = 0.04) and 100–199 km (OR 0.73 95% CI 0.55–0.96 p = 0.03) away were both significantly less likely to increase referrals.
Conclusion
This study found that referrals increased significantly after implementing an online referral system. Furthermore, physicians in their first five years of practice as well as those practicing closer to bariatric centers were more likely to increase referrals. Our findings demonstrate that an online referral system may aid in increasing referrals to bariatric surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Obesity is a significant public health concern in Canada, affecting approximately 24% of the population [1]. Severe obesity has been well established as a major risk factor for early mortality, cancer and chronic conditions such as diabetes and cardiovascular disease [2, 3]. It also has been shown to lead to an increased utilization of health resources and a resultant financial burden on the healthcare system [4]. Of the various interventions that exist to treat severe obesity, bariatric surgery has been demonstrated to be the most effective, leading to significant and sustained weight loss as well as resolution of comorbid conditions [4, 5]. Current Canadian clinical practice suggests bariatric surgery as the treatment of choice for severely obese patients (class II and class III obesity) for whom other, non-surgical interventions have failed [6]. To receive bariatric surgery in Ontario, patients must be referred to the appropriate specialist after being deemed eligible. Because the majority of referrals come from primary care physicians, they serve as a vital gateway to this treatment.
While the number of bariatric surgeries performed has increased in recent years [4, 7], less than 1% of patients who could benefit from bariatric surgery undergo it [8], highlighting, among other things, problems with the referral process. This is particularly concerning given that primary care providers have recognized the benefits and efficacy of bariatric surgery at achieving long-term weight loss [9, 10]. A recent study of the referral process in the United States highlighted a lack of effective information transfer between primary care providers and specialists as one of the greatest problems in the referral process [11]. Poor integration of care and variation in referral thresholds were also cited as important issues. Specific to bariatric surgery, several studies have highlighted lack of resources, high costs, and limited knowledge of bariatric procedures as barriers to surgical referral. [1, 9, 12] These factors all contribute to the disparity between the number of people who could benefit from surgical treatment and those who actually receive it. In addition, practitioners were deterred from referring severely obese patients due to the complicated and time-consuming referral process [11]. However, despite these identified issues with bariatric referrals, little is known as to how to best address them.
General strategies, such as standardized referral guidelines, pre-screening of referrals, and the use of electronic information transfer (such as web-based referral systems), have been suggested to improve the process [11], but few studies exist demonstrating their efficacy. As such, the purpose of this study was to determine the impact of an online referral system on referral rates to bariatric surgery.
Materials and methods
Design and setting
This was a longitudinal analysis that looked at the effect of an online referral system on the rate of referral to bariatric surgery. This study was approved by the Hamilton Integrated Research Ethics Board.
Setting
The Ontario Bariatric Network was established by the Ontario Ministry of Health and Long-Term Care in the middle of the 2009 fiscal year with full operation beginning in 2010. Referrals to bariatric surgery within the Ontario Bariatric Network are made to a centralized referral system that allows for an equitable distribution of patients among the 9 bariatric centers in 5 cities (Ottawa, Hamilton, Toronto, Guelph and Thunder Bay). All centers are accredited as Centers of Excellence by the Ontario Bariatric Network. Upon referral, each physician is given a bariatric registry referral identification number. Referrals are accepted for any patients that meet National Institutes of Health criteria though patients are required to undergo a 6-month preparation process before receiving the actual surgery.
Referral system changeover
On April 1, 2015 the Ontario Bariatric Network completely switched from a fax-based referral system to an online system. Before this time, only fax referrals were accepted and the changeover happened over a four-day period. After this period, fax-based referrals were no longer accepted. There was a communiqué sent out to family physicians in Ontario alerting them of the change to the referral process.
Study data and data sources
All surgical referrals to the Ontario Bariatric Network for the years 2011–2015 were included in the study. Referrals were stored in a database developed by the Population Health Research Institute and the Center for Surgical Invention and Innovation. Referrer data, including date of graduation, specialty, and gender, were abstracted from the College of Physicians and Surgeons of Ontario public database of physicians. Neighborhoods were defined as forward sortation areas which are denoted by the first three digits of a postal code. There are 514 forward sortation areas in Ontario. Rurality was defined by the postal code. Distance from a neighborhood to a bariatric center was calculated from the neighborhood centroid to the nearest facility. Public Health Units, a region type recognized by Statistics Canada, were the health regions of interest [13]. There are 34 Public Health Units in Ontario which are divided based on health planning and promotion goals. Neighborhood income was defined as the median individual income and data were derived from Statistics Canada [14].
Outcomes and predictors
The main outcome of this study was the total number of referrals at the provider, neighborhood and health region level. A secondary outcome of interest was whether a physician increased their referral total after implementation of the online referral system. Comparisons were made between the 2015 referral rate and the mean annual referral rate from 2011 to 2014. Our predictors of interest included physician and neighborhood characteristics. Physician characteristics included gender, specialty and years of experience. Rurality, having their office within the same health region as a bariatric center, distance to the closest bariatric center and neighborhood income were the neighborhood predictors of interest.
Statistical analysis
Descriptive statistics were used to characterize the patient population. The χ2 statistic was used to compare categorical variables. Neighborhoods were classified into 4 quantiles based on income. A three-level hierarchical logistic regression model was used to determine factors predicting an increase in referrals. To account for unmeasured confounding at the health region, neighborhood and provider level and to obtain unbiased effect estimates, identifiers for each level were used as cross-classified random effects. Fixed effects included physician characteristics including gender, specialty, and years experience as well as neighborhood characteristics including rurality, having a bariatric center within the health region, income, and distance the closest bariatric center. Monte Carlo Markov Chain estimation was used for the logistic regression model with 100,000 iterations after a 5000 iteration burn-in. All chains were examined for convergence. Statistical significance was set at p < 0.05. Data were analyzed using Stata (StataCorp version 12.1; College Station, TX) and MLwiN (Version 2.26; Centre for Multilevel Modelling, University of Bristol). Spatial analysis for Fig. 1 was carried out using the ArcGIS Desktop suite (Environmental Systems Research Institute ArcMap10.1, Redlands, CA).
Results
Table 1 presents the mean number of referrals by year at the provider, neighborhood, and health region levels. At all three levels, a consistent trend was seen. Between 2011 and 2014, the mean annual number of referrals to the Ontario Bariatric Network was relatively constant at approximately 1 referral per provider, 24 per neighborhood, and 293 per health region. After the implementation of the online referral system, the number of referrals doubled at each level. The mean number of referrals per individual was 2.1 (p < 0.001), while the mean number of referrals at the neighborhood and health region levels were 52.0 (p < 0.001) and 671.0 (p < 0.001), respectively.
Figure 1 depicts the percent change in referrals between the mean annual total for 2011–2014 and the 2015 total number of referrals among the health regions. The lowest percent change was 23%, and there was a significant increase in every single health region. The most substantial increases were for health regions that had a bariatric surgical center. These are depicted by the regions with the darkest color on the map.
Figure 2 depicts the number of new referrers by year. This illustrates that the number of new referrers decreased every year from 2011 to 2014. This also demonstrates that the increases in 2015 were not simply the result of the same physicians increasing their number of referrals but that a significant number of new referrers were brought into the system.
Table 2 presents the associations between physician characteristics and an increase in referrals. A total of 5317 physicians made referrals to the Ontario Bariatric Network from 2011 to 2015 and 68% increased referrals after implementation of the online system. Primary care specialists comprised 88.3% of the cohort, and 27.8% of physicians were in their first 5 years of practice. Global associations between an increase in referrals and female practitioners status, specialty, and years experience were seen on univariate testing.
Table 3 presents the associations between neighborhood level variables and an increase in referrals. More than 38% of practitioners worked in neighborhoods that were in the same health region as a bariatric center and nearly 60% had practices within 50 km of a bariatric center. Only 11.3% of practitioners were from rural neighborhoods. Univariate associations between an increase in referrals and neighborhood characteristics were found for being in the same health region as a bariatric facility, income quantile, and distance from bariatric center though not for rurality.
Table 4 presents the results of the hierarchal regression that modeled the odds of a provider increasing referrals after the implementation of the online referral system. Compared to male providers, female practitioners had a 17% higher odds of increasing referrals (OR 1.17 95% CI 1.03–1.32 p = 0.02). Moreover, general practitioners were no more likely to increase referrals than any subspecialty. Conversely, years of experience had a significant impact on the odds of an increase in referrals as the odds decreased with years of experience and, compared to the practitioners with less than 5 years of experience, all other experience groups had odds that were approximately 50% lower with the lowest odds being for the group that had more than 40 years experience (OR 0.44 95% CI 0.32–0.59 p < 0.001). With regards to neighborhood characteristics, proximity as well as having their practice in the same health region as a bariatric facility had significant impacts on the likelihood of increasing referrals. Practitioners within the same health region as a bariatric center were 35% more likely to increase referrals in 2015 (OR 1.35 95% CI 1.01–1.76 p = 0.04). Similarly, compared to those within 50 km of a bariatric facility, practitioners 50–99 km (OR 0.76 95% CI 0.58–0.98 p = 0.04) and 100–199 km (OR 0.73 95% CI 0.55–0.96 p = 0.03) away both were significantly less likely to increase referrals after implementation of an online system. A similar effect was seen for practitioners living more than 200 km away but did not reach statistical significance (OR 0.79 95% CI 0.57–1.05 p = 0.10). Neighborhood income quantile and rurality had no effect on the odds of an increase in referrals.
Discussion
This study investigated the effect of the implementation of an online referral system on referrals to bariatric surgery in a single-payer, universal healthcare system. We found that there was a significant increase in referrals and that these increases were widespread, with every health region increasing referrals by at least 23%. To better evaluate this variation, we investigated the physician and neighborhood level characteristics that influenced the increases. At the physician level, female practitioners and having less than 5 years experience were major drivers of having an increased referral rate after implementation. Closer proximity to a bariatric surgery center as well as having a bariatric surgery center within the same health region both had significant effects on odds of increased referrals after the implementation of the online referral system.
Several studies have investigated referrals and found issues other than patient need influencing bariatric surgery referral. The relationship between bariatric referrals and provider characteristics, such as years of practice, specialty, and level of education, has been relatively well studied. Petrin et al. in a survey of family physicians, OB-GYNs, and nurse practitioners found that OB-GYNs and nurse practitioners were significantly less likely to refer patients when compared to family physicians [15]. Additionally, Balduf et al. reported that referring physicians tended to be younger, with fewer years of practice [16], whereas Auspitz et al. found that older physicians were more likely to refer their patients for bariatric surgery [1]. Interestingly, studies nearly unanimously found that referring physicians tended to be more knowledgeable about bariatric surgery [1]. Accordingly, Balduf et al. found that the mean knowledge score among referring physicians was significantly higher than among those that did not refer, a finding corroborated by Funk et al. [16, 17]. In our study, proximity to bariatric centers may be a proxy for familiarity with the procedure and process though, among other things, it may also represent an aversion to burdening the patients with greater distances. Furthermore, online referral systems have been implemented in several specialties with varying degrees of efficacy. Studies using online systems for referral to neurosurgical units [18] and specialized endocrinological care [19] reported improved continuity of care, fewer cases of delayed examination, and decreases in inappropriate referrals. Conversely, one study was unable to find an improvement in patient care following the implementation of an online referral system [20]. While flaws have been identified in online referrals, such platforms have been demonstrated to be feasible and promising options with the potential to increase the number of appropriate referrals and streamline the referral process, leading to improved patient continuity of care.
This study evaluated the effect of an online referral system on referrals to bariatric surgery. Most importantly, it found a significant increase in referrals after converting from a fax-based referral system. Referrals to bariatric surgery more than doubled across the province and brought more than 1500 new referrers into the system. This finding underscores the fact that factors secondary to patient need are major drivers of referrals to bariatric surgery. In this specific case, the referral system was important and had a substantial impact on the number of referrals. The effect was also demonstrated in all health regions as well as for all types of physicians. This is important as it demonstrates how integral the referral system is to a bariatric care network. We also evaluated physician and neighborhood factors affecting increases in referrals after the implementation of an online referral system. We found that physicians in the first 5 years of training are the most likely to increase their referrals after the implementation of an online system and this speaks to the fact that strategies to increase referrals may have disparate effects for physicians of differing experience levels. To this point, we also found geographic disparities in the effect of the online referral system. Physicians closer to bariatric centers as well as those in the same health region as bariatric centers were more likely to increase the referrals. Accordingly, this may represent some level of disparity in physician education about bariatric surgery based on location with those closer to bariatric centers having better education and comfort with the procedure. It may also be that physicians perceive closer distances as less of a burden for their patients and would be more likely to refer on this basis. Overall, there is likely no single thing but a combination of physician and geographic attributes which all contribute.
This paper has several limitations. Other important factors such as physician comfort with the procedure and education could not be assessed. In addition, a small percentage of referrals were from nurse practitioners, and these were not included in the study, although we do not feel that the effect on nurse practitioners would be substantially different than physicians. The study could also only look at physicians who had at some point referred to the bariatric network, and therefore the conclusions do not shed light on why physicians do not refer to bariatric surgery in the first place. Lastly, this study’s setting was a single-payer, universal healthcare system with complete regionalization of care. Therefore, in settings with multiple, competing hospital systems, the effect of an online referral system may not be as profound or applicable.
Conclusion
This study evaluated the effects of the implementation of an online referral system on referrals to bariatric surgery in a single-payer, universal healthcare system. After implementation, there was a significant increase in referrals that was substantial in every single health region. We also found that physicians in the first five years of practice as well as those practicing closer to bariatric centers were more likely to increase the referrals. Our findings demonstrate that factors other than need are substantial drivers of referral to bariatric surgery. In this study, an online referral system seemed to substantially increase referrals and attract new physicians to the referral process. Based on these results, we feel online referral systems could be implemented to maximize referrals in other, similar healthcare systems.
References
Auspitz M, Cleghorn MC, Azin A, Sockalingam S, Quereshy FA, Okrainec A, Jackson TD (2016) Knowledge and perception of bariatric surgery among primary care physicians: a survey of family doctors in Ontario. Obes Surg 26:2022–2028
Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, Rimm E, Colditz GA (2001) Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med 161:1581–1586
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S adults. N Engl J Med 348:1625–1638
Canadian Institute for Health Information (2014) Bariatric Surgery in Canada
Christou NV, Sampalis JS, Liberman M, Look D, Auger S, McLean APH, MacLean LD (2004) Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 240:416–423–424
Obesity Canada Clinical Practice Guidelines Expert Panel (2007) Canadian clinical practice guidelines on the management and prevention of obesity in adults and children. CMAJ 176176:1–117
Aird LNF, Hong D, Gmora S, Breau R, Anvari M (2016) The impact of a standardized program on short and long-term outcomes in bariatric surgery. Surg Endosc 31(2): 801–808
Welbourn R, Dixon J, Barth JH, Finer N, Hughes CA, le Roux CW, Wass J (2016) NICE-accredited commissioning guidance for weight assessment and management clinics: a model for a specialist multidisciplinary team approach for people with severe obesity. Obes Surg 26:649–659
Tork S, Meister KM, Uebele AL, Hussain LR, Kelley SR, Kerlakian GM, Tymitz KM (2015) Factors Influencing Primary Care Physicians’ Referral for Bariatric Surgery. JSLS J Soc Laparoendosc Surg 19(e2015):00046
Avidor Y, Still CD, Brunner M, Buchwald JN, Buchwald H (2007) Primary care and subspecialty management of morbid obesity: referral patterns for bariatric surgery. Surg Obes Relat Dis 3:392–407
Mehrotra A, Forrest CB, Lin CY (2011) Dropping the baton: specialty referrals in the United States. Milbank Q 89:39–68
Sarwer DB, Ritter S, Wadden TA, Spitzer JC, Vetter ML, Moore RH (2012) Physicians’ attitudes about referring their type 2 diabetes patients for bariatric surgery. Surg Obes Relat Dis 8:381–386
Statistics Canada (2013) Boundary files. http://www.statcan.gc.ca/pub/82-402-x/2013003/reg-eng.htm. Accessed 21 Aug 2016
Statistics Canada Table 111-0009 - Family characteristics, summary, annual (number unless otherwise noted), CANSIM (database). http://www5.statcan.gc.ca/cansim/a26?lang=eng&id=1110009. Accessed 10 Aug 2016
Petrin C, Kahan S, Turner M, Gallagher C, Dietz WH (2016) Current practices of obesity pharmacotherapy, bariatric surgery referral and coding for counselling by healthcare professionals. Obes Sci Pract 2:266–271
Balduf LM, Farrell TM (2008) Attitudes, beliefs, and referral patterns of PCPs to bariatric surgeons. J Surg Res 144:49–58
Funk LM, Jolles S, Fischer LE, Voils CI (2015) Patient and referring practitioner characteristics associated with the likelihood of undergoing bariatric surgery. JAMA Surg 150:999
Matloob SA, Hyam JA, Thorne L, Bradford R (2016) Improving neurosurgical communication and reducing risk and registrar burden using a novel online database referral platform. Br J Neurosurg 30:191–194
Oliva X, Micaló T, Pérez S, Jugo B, Solana S, Bernades C, Sanavia M, Delgado C (2013) Virtual referral system between specialized endocrinological care and primary care. Endocrinol Nutr 60:4–9
Choo MC, Thennakon S, Shapey J, Tolias CM (2011) A web-based referral system for neurosurgery – a solution to our problems? Br J Neurosurg 25:384–387
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Aristithes G. Doumouras, Sama Anvari, Ms. Ruth Breau, Mehran Anvari, Dennis Hong, and Scott Gmora have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Doumouras, A.G., Anvari, S., Breau, R. et al. The effect of an online referral system on referrals to bariatric surgery. Surg Endosc 31, 5127–5134 (2017). https://doi.org/10.1007/s00464-017-5578-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5578-x