Abstract
Summary
The objective of this study was to examine the effectiveness of an osteoporosis prevention program on knowledge and perception of self-efficacy in adopting preventive osteoporosis behaviors in premenopausal women working in sedentary occupations. Results show the improvement in knowledge and self-efficacy was statistically significant respectively (p < 0.001) and (p = 0.001).
Introduction
The main purpose of the study was to evaluate the effectiveness of an osteoporosis prevention educational program on knowledge and perception of self-efficacy in adopting preventive osteoporosis behaviors in Tunisian premenopausal women working in sedentary occupations.
Methods
A quasi-experimental pre-post intervention study design. Our study population was composed of female employees, aged 35–50 years, of a company located in the industrial zone Sousse, situated in the center East of Tunisia. Three data collection methods were used: a questionnaire exploring socio-demographic characteristics and anthropometric measures, the Osteoporosis Knowledge Test, and the Osteoporosis Self-Efficacy Scale. The intervention consisted of an educational program relating to the promotion of calcium intake and physical activity. We are referred to the “Health Belief Model.”
Results
A survey conducted on 97 women. Only 81 subjects completed the study and are included in data analyses. The total knowledge score regarding osteoporosis improved by + 14.57 which corresponds to percentage of 109% between the pre- (T1) and post-test (T2). This improvement in knowledge was statistically significant (p < 0.001), going from 13.41 ± 3.94 at T1 to 27.98 ± 2.49 at T2. The total osteoporosis self-efficacy score has increased by + 9.56, or a percentage of 15% between the pre- and post-test. This improvement in self-efficacy was statistically significant (p = 0.001), going from 64.18 ± 20.84 at T1 to 73.73 ± 14.35 at T2.
Conclusion
It is important to create an appropriate environment for the adoption of favorable behaviors to healthy bones and to promote health education with political commitment and collaboration with different sectors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is defined as a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture [1]. Curtis et al. (2017) have reported that osteoporosis is an important public health problem worldwide, even in developing countries [2]. Globally, one in three women and one in five men aged 50 years or older will suffer from an osteoporotic fracture [3]. Each year, with the aging of the population, the prevalence of osteoporosis increases significantly and it contributes to about 9 million fractures [3]. Tunisia, a lower middle-income country, is not spared from this major public health problem. The prevalence of postmenopausal osteoporosis in Tunisian women over 50 years old is 23.4% [4]. The prevalence of osteoporosis was higher in the elderly population and in particular, after menopause, in women, due to the acceleration of estrogen deficiency [5, 6].
The morbidity of osteoporosis is reflected in the incidence of fragility fractures; in fact, in the European Union, in 2010, 3.5 million new osteoporotic fractures were recorded [7]. The 2011 audit on the epidemiology, costs, and burden of osteoporosis in Middle East and Africa estimated that in Tunisia, the number of osteoporotic hip fractures in 2010 was 3164 cases in persons aged 50 years or over. This number is projected to reach 5101 by 2020 and 8850 by 2039 [8].
Osteoporosis also contributes to mortality [9]. In France, one in five women died within a year of being hospitalized for a femoral neck fracture [10].
Complications of osteoporosis also increase health care expenditures. In 2010, the direct cost of osteoporosis in Europe was estimated to be 37 billion euros (US$40 billion). These costs are expected to increase by 25% by 2025 [7]. The 2011 audit on the epidemiology, costs, and burden of osteoporosis in Middle East and Africa cited that in Tunisia, direct hospital costs for osteoporotic hip fractures have been estimated at €4 million [8]. In 2013, Dutch researchers evaluated the total cost incurred by clinical fractures in 116 osteoporotic patients aged 50 years or older. The indirect expenses accounted for half of the total cost [11].
Insufficient awareness of osteoporosis and lack of educational programs to prevent osteoporosis are among the important reasons for osteoporosis [12].
A large body of research has investigated the role of knowledge in preventing the development of osteoporosis and has reported that female nursing students or workers have severe knowledge deficits, and educational interventions are useful for increasing knowledge [12, 13]. Many studies indicated health behavior change is more likely to occur when person-centered interventions are designed to increase knowledge, health beliefs, skills, and abilities [14]. Katherine et al. (2018) have shown that knowledge alone is not enough to initiate preventive behaviors. We just have to recognize that improving knowledge and self-efficacy is just one step in desired behavioral change. Ultimately, both are necessary components of education that can be facilitated by health care providers [15]. Therefore, health education based on improving self-efficacy can positively affect osteoporosis preventive behavior [12, 16, 17]. Self-efficacy is the personal belief in one’s own ability to perform an action [18].
McLendon and Woodis showed in their study in 2014 that young (less than 50 years old) and premenopausal women can increase their peak bone mineral density and reduce the risk of osteoporosis later in life by following preventive measures [19].
A workplace osteoporosis prevention intervention program significantly improved calcium intake and weight-bearing physical activity in adult (aged 25–49 years) and sedentary women [20, 21]. Therefore, premenopausal and sedentary women are the most at-risk populations and a target group for osteoporosis prevention.
The objective of this study was to evaluate the effectiveness of an osteoporosis prevention educational program on knowledge and perceived self-efficacy to adopt osteoporosis preventive behavior in Tunisian premenopausal women working in sedentary occupations.
Methods
Study design
A single-group quasi-experimental pre-post intervention study was conducted in 2019 on a group of female participants who were selected and asked to complete pre- and post-intervention questionnaires.
Study population
Our study population was composed of female employees of a company located in the industrial zone Sousse, situated in the center East of Tunisia.
In order to select the field of the study, a sampling by reasoned choice was favored [22]. This consisted of selecting a participating location where women work in sedentary occupations for up to 8 h of paid work during the study period (7 months) for recruitment of female employees to participate in data collection and pre-post intervention activities. Variables were measured before and 3 months after the intervention (a stopping period and effect latencies). At the firm level, women were selected using non-probability and accidental sampling [22].
The sample size estimate was based on a 5% significance level and 80% study power, to detect a 20% difference in knowledge level between pre- and post-intervention. According to a 2015 experimental study, before an osteoporosis prevention educational program, Jordanian women in the group had moderate knowledge (42%) [23]. We added 20% to account for non-responders and dropouts. Thus, 97 women are needed in the experimental group (according to Biosta TGV).
Eligibility criteria
The inclusion criteria were volunteered healthy, premenopausal women aged 35–50 years and worked in a sedentary job (at least 50% of working hours).
The exclusion criteria were as follows: Participants had a pathology that could induce osteoporosis. The most common causes of secondary osteoporosis include gastrointestinal disorders, endocrinopathies, hematological disorders, renal disease, and autoimmune disorders.
The excluded disorders included menopause (no menses > 12 months), known osteoporosis, hysterectomy, oophorectomy, hormone replacement therapy, corticosteroid therapy, prior osteoporosis education, or current pregnancy.
Data collection
The variables studied are related to knowledge and perception of self-efficacy in adopting an osteoporosis preventive behavior as well as the factors that can influence them (such as age, educational level, income, living environment, and medical histories: anemia, a stomach ulcer, allergic, migraine, asthma, diabetes) in relation to osteoporosis.
Data were collected by three measurement instruments:
-
A questionnaire on socio-demographic characteristics, medical histories, and anthropometric measurements (weight and height).
-
The revised Osteoporosis Knowledge Test (OKT).
-
The Osteoporosis Self-Efficacy Scale (OSES).
These measures were distributed by researchers (the principal investigator and two pre-trained health professionals) to all participants in face-to-face interviews in the company’s infirmary.
The validation of the English versions of the OKT and OSES in Arabic, in the Tunisian socio-cultural context, was carried out using a method inspired by Vallerand’s (1989) cross-cultural validation [24].
In this perspective, after having carried out the first three steps of Vallerand’s method, preparation of the preliminary version and its evaluation and modification by committee approach as well as the evaluation of the experimental version by pre-testing, we were interested in the content validity and the reliability evaluation of both instruments. Validity and reliability showed that the Content Validity Index (CVI) of the translated OKT is equal to (0.87). This score is considered acceptable. The OKT showed satisfactory internal consistency (α = 0.735) and excellent reliability as intraclass correlation coefficient (ICC = 0.953).
The CVI of the OSES translated into Arabic is equal to (0.807). Thus, the statements of the (OSES) measure the concepts under study. The OSES showed good internal consistency (α = 0.880) and excellent reliability as intraclass correlation coefficient (ICC = 0.994).
The reliability and validity of the revised OKT were proven. The revised OKT consists of two subscales assessing knowledge about appropriate activity for osteoporosis prevention (items 1–17 and 30–32) and the subscale about nutrition (items 1–11 and 18–32) [25].
The OSES is a 12-item visual analog scale composed of two subscales: the OSES-Physical Activity (items 1–6) and the OSES-Calcium (items 7–12). The reliability and validity of the original OSES have been proven [26].
The intervention program
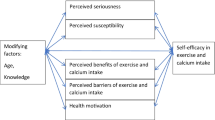
The “Health Belief Model” (HBM) guided the design and implementation of the intervention program [18]. The osteoporosis educational program was developed by the principal investigator according to contemporary empirical knowledge and guidelines from the International Osteoporosis Foundation (IOF), 2017 [27].
The different activities were health education sessions related to the promotion of calcium intake and physical activity. The intervention lasted 2 months (July, August 2019). Each woman received four 1-h health education sessions during 1 month. These sessions were conducted in a conference room located within the company. We have obtained permission from the director of the company to organize these education sessions during the participants’ working time (the last hour of their professional activities).
The women’s education was provided by the researcher and experts (a nutritionist and a physical medicine-rehabilitation physician). Each session consisted of screenings of scenarios, slides (PowerPoint), and face-to-face lectures using the discussion method (questions and answers), as well as posters and educational brochures. The detailed protocol of the intervention was published [28].
To ensure the reproducibility of the intervention, the interveners as well as the supports were the same for the four groups. The course of the sessions respected the steps and the scheduled times. Training is offered to all interveners who implement this intervention program in order to minimize inter-individual variability.
To promote compliance, wall posters relating to the promotion of calcium intake and physical activity were displayed throughout the intervention in the company.
After advice from experts in preventive medicine, all intervention activities and educational materials were adapted to the socioeconomic and cultural habits of the female employees. To maintain and improve the activity of the experimental group, telephone messages in educational text about osteoporosis were sent to the participants during 1 month of follow-up. Each woman received 32 messages relating to risk factors for osteoporosis, physical activity, the promotion of calcium intake, and the general area including information on diagnosis, treatment, and bone development.
Ethical considerations
The study has been approved by the Ethic Committee of Sahloul University Hospital. Authorization was obtained from the corresponding author to use the questionnaires. In addition, we acquired permission from the Sousse occupational medicine group and from the director of the company. Informed consent was obtained from all individual participants included in the study. The women were willing to participate and free to withdraw. Finally, we respected the confidentiality, the rights, and the integrity of the participants.
Statistical analysis
The chi-square test (X2) was used for the comparison of qualitative variables. For the comparison of medians, non-parametric tests were applied for the comparison of ranks via the Mann–Whitney-Wilcoxon test and the Kruskal–Wallis test, depending on the indication for independent or paired samples.
The accepted confidence interval was 95%, and the significance level was set at p < 0.05 for all comparisons.
Results
Response rate
Before the intervention began, the study population consisted of 97 premenopausal women. After the intervention, only 81 women participated in the study. The response rate was 83.5%.
Analyses were only performed on the 81 women that completed the study.
Socio-demographic characteristics
A total of 81 female participants completed the study. The women had a mean age of 40.27 ± 3.58 years. One in ten participants had a university degree. The proportion was 11.1%. Almost all the interviewed women had an average income (between 403.104 and 1209.312 dinars/month, i.e., between 144.17 and 432.50 dollar US/month). The proportion was 96.3%. Most of participants resided in urban areas (93.8%). 59.3% of the participants had medical histories: 19.8% were anemic, 18.5% had a stomach ulcer, 16% were allergic, 8.6% complained of migraine, 3.7% had asthma, and 3.7% had diabetes (Table 1).
aMedical histories: anemic, stomach ulcer, allergic, migraine, asthma, and diabetes.
Therefore, the values reported in the pre-test were for the 81 participants who completed the post-intervention questionnaire.
Evolution of knowledge about osteoporosis according to the Osteoporosis Knowledge Test
The total knowledge score regarding osteoporosis had improved by + 14.57, i.e., 109% increase between the pre-test (T1) and post-test (T2). Indeed, this improvement in knowledge was statistically significant (p < 0.001), increasing from 13.41 ± 3.94 at T1 to 27.98 ± 2.49 at T2. Concerning the nutrition and physical activity subscales, the evolution was statistically significant in both cases, but more important for nutrition (p < 0.001) than for physical activity (p < 0.001). Actually, the mean score of the nutrition subscale had increased from 11.07 ± 3.56 at T1 to 23.02 ± 2.14 at T2. In addition, the mean score of the physical activity subscale increased from 8.97 ± 3.03 at pre-test (T1) to 17.41 ± 1.56 at post-test (T2) (Table 2).
An improvement in knowledge about osteoporosis had concerned all participants. The 2-month intervention significantly improved knowledge on calcium intake and physical activity.
Data in Table 3 reflect change following intervention results (Table 3).
Socio-demographic characteristics had no statistically significant influence on the development of knowledge about osteoporosis. The p values in (Table 3) represent non-significant differences between age groups on total score change, PA score change, and calcium score change, then non-significant effects of educational level, income, living environment, and medical histories on total score change, PA score change, and calcium score change (Table 3).
Evolution of osteoporosis self-efficacy according to the Osteoporosis Self-Efficacy Scale
The total score of osteoporosis self-efficacy had improved by + 9.56, i.e., 15% increase between pre- and post-test. This improvement was statistically significant (p = 0.001) from 64.18 ± 20.84 at T1 to 73.73 ± 14.35 at T2 (Table 4).
Concerning the OSES subscales, the evolution was statistically significant in both cases but more important for calcium (p = 0.002) than for physical activity (p = 0.039). The mean score of the calcium subscale had increased from 65.45 ± 24.99 at T1 to 76.54 ± 14.53 at T2. The mean score of the physical activity subscale was improved from 62.90 ± 26.31 at pre-test to 70.93 ± 17.68 at post-test (Table 4).
A positive change in the perception of self-efficacy was observed in 61.7% (n = 50) of cases.
The evolution of the perception of self-efficacy in adopting an appropriate physical activity for the prevention of osteoporosis was influenced by the age of the participants (p = 0.019). The overall difference of PA score by age groups is statistically different, with an overall p value of 0.019 (Table 5).
This difference was especially identified in women aged between 35 and 39 years than those aged between 45 and 50 years (p = 0.006).
The p values in (Table 5) represent there were differences in calcium score change in urban and rural groups as well as differences in total and calcium scores between women with and without medical histories.
The living environment and medical histories had a significant influence on the self-efficacy to adopt an osteoporosis preventive behavior linked to a diet rich in calcium (p = 0.007). This development was most noticeable among participants of rural origin and with medical histories (Table 5).
On the other hand, an improvement in self-efficacy in adopting an osteoporosis preventive behavior was statistically influenced by the existence of medical histories (p = 0.018).
The medical histories emerged as a factor encouraging the adoption of a diet rich in calcium in our population (p = 0.007) (Table 5).
This intervention study demonstrates the positive impact this educational program can have on the perception of self-efficacy in adopting an appropriate physical activity for the prevention of osteoporosis and on the self-efficacy to adopt an osteoporosis preventive behavior linked to a diet rich in calcium in women age 35–50 at risk for osteoporosis. The 2-month intervention significantly improved the self-efficacy in adopting an osteoporosis preventive behavior. Data in Table 5 reflect change following intervention results (Table 5).
Discussion
Prevention of osteoporosis is the main strategy to fight this disease and its complications. This should begin in adolescence and should target modifiable risk factors [19]. This study provides further confirmation of the concept that an educational program may be effective in helping individuals understand how to maintain bone health. In fact, the Health Belief Model (HBM) is conceptual framework in health behavior research, both to explain change and maintenance of health-related behaviors and as a guiding framework for health behavior interventions [18]. This conceptual framework contains several primary concepts susceptibility, seriousness, threat, benefits and barriers to a behavior, and cues to action, and, most recently, includes self-efficacy [18].
We have proved that improvement in knowledge was statistically significant (p < 0.001), going from 13.41 ± 3.94 at T1 to 27.98 ± 2.49 at T2. Also, we have showed that improvement in self-efficacy was statistically significant (p = 0.001), going from 64.18 ± 20.84 at T1 to 73.73 ± 14.35 at T2.
We have demonstrated that our program had a beneficial effect on women’s knowledge significantly. Moreover, Malakeh et al. (2015) showed in their randomized controlled trial that the knowledge of Jordanian women and teachers improved significantly in the intervention group, compared to the control group [23].
These results are comparable with those of the study by Endicott (2013) who showed that the knowledge of English-speaking and perimenopausal women about osteoporosis prevention significantly increased (p < 0.001) [17]. The author also demonstrated the importance of starting education about osteoporosis risk factors and preventive measures as early as possible in the perimenopausal years because this can reduce morbidity later in life [17].
The effectiveness of osteoporosis prevention interventions was demonstrated in the quasi-experimental study by Abo El Matty Shahbo et al. (2016). The authors proved that knowledge about osteoporosis increased significantly (p < 0.05) after the intervention in female Egyptian students and female employees, respectively [12].
Physical activity and adequate calcium intake are among the most recommended measures for osteoporosis prevention [29]. Regarding the OSES subscales, the change was statistically significant in both cases but greater for calcium (p = 0.002) than physical activity (p = 0.039). Dutto et al. (2021) showed that sedentary premenopausal women engaging in 6 months of high-impact aerobic exercise improved bone mineral density in the calcaneus, lower leg, and lumbar spine 2 [30]. But, Pender (2011) showed that physical activity is not considered an appropriate activity for women in some ethnic groups [31].
Our study showed that predictor of the evolution of the perception of self-efficacy in adopting an appropriate physical activity for the prevention of osteoporosis among woman was the younger age. This difference was especially identified in women aged between 35 and 39 years than those aged between 45 and 50 years (p = 0.006). The advancing age is certainly associated with more fatigue sensation, which may decrease patient’s level of commitment to physical activity. In agreement with this finding, Hanan Saied et al. (2011) found a negative relationship between age and commitment to physical activity [32].
Adequate calcium intake is another factor in the prevention of osteoporosis. The mean score change of a calcium subscale was significantly higher in women from a rural background and those with medical histories. Our study is comparable to the article by Janiszewska et al. (2016), which identified the influence of living environment on perceived self-efficacy to adopt a calcium-rich diet. The authors observed that Polish women living in small towns were characterized by a significantly higher sense of self-efficacy. They more often reported the intention to consume calcium-containing products than women in the countryside or in the big city [33]. In our study, the evolution of the total self-efficacy score was significantly different according to the existence or not of medical histories (p = 0.018) since the evolution of osteoporosis self-efficacy in women with medical histories was significantly higher. This is one of the strengths of our study because this result has not been obtained by other programs. Endicott (2013) showed that there were no statistically significant results regarding self-efficacy between the two groups of women with and without family medical histories [17].
Other studies corroborate our findings. Jeihooni et al. (2016) in a randomized controlled trial showed that Iranian women’s perceived self-efficacy was significantly improved in the intervention group, compared to the control group [34]. Tan et al. (2016) conducted a randomized controlled trial in 16 workplaces in Singapore. The authors showed that there is an increase in the self-efficacy of sedentary women to adopt osteoporosis preventive behavior compared to the control group [21]. The workplace is a favorable place for health education. For many adults, the workplace is a key environment for being physically active and reducing sedentary behavior. Increased physical activity throughout the workday can help increase productivity as well as reduce injuries and absenteeism [35]. Workplace health promotion programs aiming to improve individual quality of life and nutrition and/or increase physical activity generate financial savings in terms of reduced absenteeism and medical costs [35].
Currently, it is recognized that osteoporosis prevention intervention actions in the community and occupational settings have a definite effectiveness on increasing calcium intake, practicing weight-bearing physical activity, and thus decreasing the prevalence of osteoporosis [21, 34, 36].
Among the methodological limitations of our study, the absence of a comparison control group made this design delicate for obstacles to internal validity. To avoid the causal relationships being limited, we have paid attention to the main sources of disability (or bias) [22]. In order for the maturation process to have less influence on the results obtained, the research was extended over a short period of time (7 months) to participate in data collection and pre-post intervention activities [22]. It should be noted that in the context of the study, the various sources of possible competing explanations were almost absent since women did not participate in parallel in other educational programs [22].
Although the sampling was non-probability and it was accidental (for convenience), to control selection bias, eligibility criteria have been established to better maintain the homogeneity of the sample.
One of the strengths of this study is the credibility of results, since information bias was prevented by using measurement instruments that are reliable and validated in the Tunisian context. Data collection was carried out by a principal investigator and two pre-trained health professionals. The use of two measuring instruments allowed us to better interpret the data. The results give an overview of a large fringe of the population knowing that in Tunisia, the workplaces are increasingly extended in large cities and coasts. Finally, the recommendations arising from the analysis of the results are targeted and adapted to the Tunisian context. Thus, the program is well studied by experts based on a literature review; therefore, it is best suited to the Tunisian context.
Conclusion
Our results show the effectiveness of an osteoporosis prevention intervention program in promoting and adopting healthy and sustainable lifestyles among Tunisian premenopausal women working in sedentary occupations.
It is important to create an appropriate environment for the adoption of favorable behaviors to healthy bones and to promote health education with political commitment and collaboration with different sectors.
The potential of the intervention to prevent osteoporosis would be more accurately assessed using bone mineral density densitometry or other biomarker measures of bone remodeling. Resource and feasibility limitations precluded these possibilities in this work. This is an important consideration for future studies in this area.
References
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1):23–57. https://doi.org/10.1007/s00198-012-2074-y
Curtis EM, Moon RJ, Harvey NC, Cooper C (2017) The impact of fragility fracture and approaches to osteoporosis risk assessment worldwide. Bone 104:29–38. https://doi.org/10.1016/j.bone.2017.01.024
Cooper C, Ferrari S, Reginster JY , Dawson Hughes B, Rizzoli R, Kanis J (2017) Livre blanc de l’IOF sur l’ostéoporose. First edition. Suisse. Available on: http://share.iofbonehealth.org/WOD/Compendium/IOF-Compendium-of-Osteoporosis-FR-WEB.pdf
Sahli H, Testouri N, Chihaoui MB, Salah AH, Cheour E, Meddeb N, et al (2009) Bone mineral density in healthy Tunisian women. Maturitas. 63(3):227–32. Available on: https://www.ncbi.nlm.nih.gov/pubmed/19398172.
Liu X, Zhang R, Zhou Y, Yang Y, Si H, Li X, et al (2014) The effect of astragalus extractive on alveolar bone rebuilding progress of tooth extracted socket of ovariectomied rats. Afr. J. Tradit. Complement. Altern. Med; 11(5): 91–98. Available on: http://dx.doi.org/https://doi.org/10.4314/ajtcam.v11i5.15
Oden A, McCloskey EV, Kanis JA, Harvey NC, Johansson H (2015) Burden of high fracture probability worldwide: secular increases 2010–2040. Osteoporos Int 26:2243–2248. https://doi.org/10.1007/s00198-015-3154-6
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, et al (2013 ) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos; 8:136
International Osteoporosis Foundation (2011) The Middle East & Africa Regional Audit: epidemiology, costs & burden of osteoporosis in 2011.Available on: https://www.osteoporosis.foundation/sites/iofbonehealth/files/2019-06/2011_Middle_East_Africa_Audit_English.pdf
Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E et al (2016) Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthoped 7(3):171–176. https://doi.org/10.5312/wjo.v7.i3.171
Grange L, Chales G, Alliot Launois F (2017) Livre blanc des états généraux de l’ostéoporose. Association Française de Lutte Anti-Rhumatismale. Available on : http://www.aflar.org/IMG/pdf/livre_blanc-version_legere.pdf
EekmanDA TW, MM, Coupe VM, Erisek-Demirtas S, Kramer MH, Lems WF. (2013) Indirect costs account for half of the total costs of an osteoporotic fracture: a prospective evaluation. Osteoporos Int 25(1):195–204. https://doi.org/10.1007/s00198-013-2505-4
Abo El MattyShahbo G M, Abed El-Rahman M, El-mowafy R (2016) Evaluation of knowledge and self-efficacy about osteoporosis perception among females in the faculty of nursing in Port-Said, Egypt. International Journal of Caring Sciences; 9 (1): 72–79. Available on : https://pdfs.semanticscholar.org/4577/93149def17d8710a8f28b718ab0c41d32e77.pdf
Zhang YP, Li XM, Wang DL, Guo XY, Guo X (2012) Evaluation of educational program on osteoporosis awareness and prevention among nurse students, in China. Nurs Health Sci 14(1):74–80. https://doi.org/10.1111/j.1442-2018.2011.00665
Ryan, P., Schlidt, A. & Ryan, C (2013) The impact of osteoporosis prevention programs on calcium intake: a systematic review. Osteoporos Int .24, 1791–1801.https://doi.org/10.1007/s00198-012-2259-4
Arlinghaus KR, Johnston CA (2018) Advocating for behavior change with education. Am J Lifestyle Med 12(2):113–116. https://doi.org/10.1177/1559827617745479
Ozturk A, Sendir M (2011) Evaluation of knowledge of osteoporosis and self-efficacy perception of female orthopaedic patients in Turkey. Journal of Nursing and Health care of Chronic Illness 3(3):319–328. https://doi.org/10.1111/j.1752-9824.2011.01106.x
Endicott RD (2013) Knowledge, health beliefs, and self-efficacy regarding osteoporosis in perimenopausal women. J Osteoporos. https://doi.org/10.1155/2013/853531
Joanna Hayden (2014) Health belief model. In: Introduction to health behavior theory. Jones and Bartlett Learning books. Second Edition. Available on : https://books.google.tn/books?id=9YZSAAAAQBAJ&pg=PA63&hl=fr&source=gbs_toc_r&cad=4#v=onepage&q&f=false
McLendon AN, WoodisCB (2014) A review of osteoporosis management in younger premenopausal women. Women's Health 10(1), 59 77. Doi:https://doi.org/10.2217/whe.13.73.
.Tan AM, La Montagne A, Sarmugam R, Howard P. (2013) A cluster-randomised, controlled trial to assess the impact of a workplace osteoporosis prevention intervention on the dietary and physical activity behaviours of working women: study protocol. BMC Public Health 13(1):405. https://doi.org/10.1186/1471-2458-13-405
Tan AM, LaMontagne AD, English DR, Howard P (2016) Efficacy of a workplace osteoporosis prevention intervention: a cluster randomized trial. BMC Public Health 16(1):859. https://doi.org/10.1186/s12889-016-3506-y
Fortin M. F, Gagnon J (2016) Fondements et étapes du processus de recherche. Méthodes quantitatives et qualitatives. (3e édition). Montréal, Québec: Chenelière Éducation: 234–242.
.Malakeh Z M, Toama Z T(2015) The effect of osteoporosis health education program based on health belief model on knowledge and health beliefs towards osteoporosis among Jordanian female teachers. European Scientific Journal. /SPECIAL/ edition vol.1 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431:385–398. Available on: https://eujournal.org/index.php/esj/article/view/5107/4879
Vallerand RJ (1989) Vers une méthodologie de validation transculturelle de questionnaires psychologiques : implication pour la recherche en langue Française. Can Psychol 30(4):662–680. https://doi.org/10.1037/h0079856
Gendler PE, Coviak CP, Martin JT, Kim KK, Dankers JK, Barclay JM et al (2014) Revision of the osteoporosis knowledge test: reliability and validity. West J Nurs Res 37(12):1623–1643. https://doi.org/10.1177/0193945914537565
Horan ML, Kim KK, Gendler P, Froman RD, Patel MD (1998) Development and evaluation of the osteoporosis self-efficacy scale. Res Nurs Health 21(5):395–403
International Osteoporosis Foundation (2017) What is osteoporosis? Available on: https://www.iofbonehealth.org/what-is-osteoporosis
Belgacem A, Laouani Kechrid C, Nouira A, Ben Dhiab M, Soussi S, Chelbi S (2020) Évaluation de l’efficacité d’un programme éducatif de prévention de l’ostéoporose chez les femmes tunisiennes pré ménopausées travaillant dans des occupations sédentaires : protocole de recherche. Francophone International Journal of Nursing Research 6(4):1–9. https://doi.org/10.1016/j.refiri.2020.100212
Raj JP, Venkatachalam S, Shekoba M, Norris JJ, Amaravati RS (2018) Dietary calcium intake and physical activity levels among people living in Karnataka, India – an observational hospital-based study. J Family Med Prim Care 7:1411–1416
Dutto DJ, Liang MTC, Braun WA, Bassin SL, Wong ND, Arnaud SB (2021) Effect of 6-month high-impact step aerobics and resistance training on BMD and tibial bending strength in sedentary premenopausal women. Osteoporos Int. https://doi.org/10.1007/s00198-021-06106-y
Pender N, Murdaugh C, Parsons MA. (2011) Health promotion in nursing practice. 6th edition. Pearson Education.
S.A. Hanan .Y Sahar (2011) Perceived self-efficacy and commitment to an exercise plan in patients with osteoporosis and osteoarthritis. International publication . Available on: https://www.researchgate.net/publication/290489523_Perceived_self-efficacy_and_commitment_to_an_exercise_in_patients_with_osteoporosis_and_osteoarthritis
Janiszewska M, Firlej E, Dziedzic M, Żołnierczuk-Kieliszek D (2016) Health beliefs and sense of one’s own efficacy and prophylaxis of osteoporosis in peri-and post-menopausal women. Ann Agric Environ Med 23(1):167–173. https://doi.org/10.5604/12321966.1196875
.Jeihooni AK, Hidarnia A, Kaveh MH, Hajizadeh E, Askari A, (2016) Application of the health belief model and social cognitive theory for osteoporosis preventive nutritional behaviors in a sample of Iranian women. Iran J Nurs Midwifery Res 21(2):131–141. https://doi.org/10.4103/1735-9066.178231
.Van Dongen JM, Proper KI, van Wier MF, Van der Beek AJ, Bongers PM, Mechelen W, et al (2011) Systematic review on the financial return of worksite health promotion programmes aimed at improving nutrition and/or increasing physical activity. Obes Rev ;( 12):1031–49. Doi: https://doi.org/10.1111/j.1467-789X.2011.00925.x
.V.H. Nguyen (2017) Osteoporosis prevention and osteoporosis exercise in community-based public health programs. Osteoporosis and Sarcopenia ; 3.18–3 .Doi : https://doi.org/10.1016/j.afos.2016.11.004
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study has been approved by the appropriate institutional and/or national research ethics committee (Ethic Committee of Sahloul University Hospital).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Belgacem, A., Laouani Kechrid, C., Nouira, A. et al. Effectiveness of an osteoporosis prevention educational program in Tunisian premenopausal women working in sedentary occupations: a quasi-experimental study. Arch Osteoporos 17, 81 (2022). https://doi.org/10.1007/s11657-022-01119-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01119-4