Abstract
Summary
The rationale of this study was to examine the effectiveness of 6-month high-impact step aerobics (SA) or moderate-intensity resistance training exercise (RT) on bone mineral density (BMD) and bone bending strength in sedentary women. Results show that SA enhanced BMD in the heel, lower leg, and lumbar spine 2.
Introduction
To determine the effectiveness of 6 months of high-impact step aerobics (SA) or moderate-intensity resistance training (RT) on areal bone mineral density (aBMD) and tibial bending strength in sedentary premenopausal women.
Methods
Sixty-nine women (20–35 years old) who were randomly assigned to RT (n = 22), SA (n = 26), or non-treatment control (CON, n = 21) groups completed the study. SA had a minimum of 50 high-impact landings each training session. RT had a periodized lower body resistance training program incorporating eight exercises (65–85% of 1 repetition maximum: 1-RM). Both RT and SA met 3 times weekly. aBMD was assessed using dual X-ray absorptiometry (DXA). Tibial bending strength was assessed using mechanical response tissue analysis (MRTA). Measurements at 6 months were compared to baseline using ANCOVA, adjusted for baseline measures and covariates with α = 0.05.
Results
Calcaneus aBMD (0.0176 vs -0.0019 or -0.0009 g/cm2 relative to RT, p < 0.004, and CON, p < 0.006, respectively), lower leg aBMD (0.0105 vs -0.0036 g/cm2, relative to RT, p = 0.02), and lumbar spine 2 (L2) aBMD (0.0082 vs -0.0157 g/cm2 relative to CON, p < 0.02) were significantly greater in the SA group after 6 months. Tibial bending strength and bone resorption biomarkers were unchanged in all three groups after 6 months.
Conclusion
Sedentary premenopausal women engaging in 6 months of high-impact aerobic exercise improved aBMD in the calcaneus, lower leg, and L2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis and related fractures are important health problems increasing with age and with significant costs [1]. Early intervention can help to decrease the likelihood of developing the disease. Physical activity or exercise training enhances bone development can optimize bone accrual, increase bone strength, and may prevent osteoporosis related fractures during old age [2, 3]. Bone research has focused on postmenopausal [4,5,6,7,8] and, to a lesser extent, premenopausal women [9, 10]. Early detection and intervention to build bone strength through lifestyle programs are key to preventing osteoporosis-related fractures. Research on exercise and bone health in healthy young women is under-represented in the literature and holds promise for prevention of osteoporosis [11]. Supervised exercise intervention in this population may have benefits of increasing BMD, maximizing bone mass [9, 12].
Resistance training has been used extensively to study the tensile loading of bone [13, 14], but in premenopausal women, there is controversy on whether this alone may produce benefits on bone density. Some studies have shown that resistance training can increase areal bone mineral density (aBMD) of the lumbar spine and/or hip [14]. A recent meta-analysis among premenopausal women found that exercise training improves both femoral neck and lumbar spine aBMD [10]. Studies have used exercise intensity of 65–80% 1-RM with multiple different exercises for 18 weeks [15] or 52 weeks [9] on aBMD.
Compressive loading exercise routines that have produced increases in bone density in sedentary, postmenopausal women include heel drops [16], jumping and skipping [17], and jump step aerobics [18]. Most of these exercises are typified by having a fairly large magnitude ground reaction force (> 2.5 times body weight) that is rapidly applied. Heinonen et al. [18] measured peak ground reaction forces as high as 5.6 times body weight during landing exercise resulting in a 1.6% increase in femoral neck aBMD.
In young healthy women, the application of a non-invasive, mechanical response tissue analyzer (MRTA), quantifying the relation between tibial bending strength and aBMD [19], has not been reported. We applied the MRTA technology because it does not expose the participants to radiation during scanning and has low instrumentation cost and a high correlation with the three-point bending strength test [20,21,22,23,24].
The purpose of this study was to determine the effectiveness of two different modes of exercise training on areal bone mineral density and tibial bending strength in sedentary premenopausal women.
Methods
Subjects
Initially, 143 women from the California counties of Los Angeles and Orange were recruited for the study. These women consisted of four major racial-ethnicity groups: European-White, African-American, Hispanic, and Asian. Prior to inclusion in the study, all subjects signed a written informed consent approved by the Institutional Review Board of California State Polytechnic University, Pomona, CA. The procedures used in this study adhere to the principles of the Declaration of Helsinki.
Participants’ weight (kg), weight (cm), and tibia length (cm) were measured twice by trained research assistants during the screening process. Inclusion criteria included being between 20 and 35 years of age, healthy, sedentary, and premenopausal with normal menstrual function. Exclusion criteria included the presence of the following: obesity (BMI > 30 kg/m2); underweight (BMI < 18 kg/m2); chronic drug or alcohol use; amenorrhea (0–3 cycles per year); and diagnosed cardiovascular or pulmonary disease, orthopedic disorders, chronic disease associated with bone health (thyroid dysfunction), gastrointestinal disease, eating disorders, kidney disorder, any form of cancer, and liver disease. Contraceptive use was not an exclusion criteria. “Sedentary” was defined as participation in 2 times or less a week of aerobic exercise or resistance training in the past 3 years [25]. This was verified via a self-reported Exercise and Health History Questionnaire. After being screened for eligibility, 90 subjects were randomized into 1 of 3 groups: resistance training (RT, n = 32), step aerobics (SA, n = 30), and non-treatment control (CON, n = 28). At the 6-month period, 69 subjects completed the study: RT, n = 22; SA, n = 26; and CON, n = 21. Adequate calcium intake was ensured by having all participants add 1000 mg of calcium supplement to their diet on a daily basis.
Training sessions
Both training groups met for three supervised sessions each week (45 min per session). Each training session involved 5–10 min of warm-up followed by 30 min of aerobic exercise or resistance training routine, ending with 5–10 min of cool-down and stretching exercise. Attendance was recorded for all training sessions.
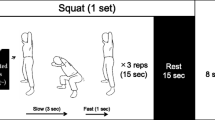
The RT program was designed to produce primarily tensile and some axial loading on the bones of the lower limb. Intensity of RT was increased from 65 to 85% 1-RM with 10–12 repetitions performed per set. Exercises performed included the leg press, back squat, leg extension, leg flexion, seated calf, standing calf, back extension, and the abdominal curl. Exercise loads were determined from 1-RM performed at baseline and at 3 months. Following an initial week of orientation to the lifts, 1-RM was evaluated. This was achieved employing a circuit fashion where, initially, light loads were applied for each lift (10 repetitions). Higher loads with fewer repetitions were progressively added, continuing in a circuit fashion. Once a 2–3 RM was achieved, the subject remained at the lift site for a 2-min recovery before testing for the respective maximum load.
The SA program was designed to incorporate high-impact landings into a traditional step aerobics routine. Traditional step aerobics involves the performance of exercise routines to music using an aerobics step that was between 8 and 12 inches in height. After the first 6 weeks of familiarization with traditional step aerobics, two-legged landings (involving an aerial phase) from the step to the ground were carefully and gradually incorporated into the aerobics routine. From week 7 to week 26, high-impact landings were performed during each training session, with the number of landings increasing from 50/session in week 7 to an average of 100/session in weeks 12–26. Landings from each participant were periodically monitored using a force measuring platform (model BP600900, AMTI, Maryland, USA) to ensure that large ground reaction forces (> 2.5 times body weight) were being produced with the high-impact landing maneuvers as incorporated into the step aerobics routine. Average force of all landings across all subjects during the 26 week training period were 3.2 ± 0.3 body weight.
Procedures
All measurements were performed prior to random assignment to treatment groups (baseline) and after 6 months of participation in the study.
Bone density measurements
Areal bone mineral density (aBMD) was scanned and analyzed by the same trained technician at baseline and after 6 months using a dual energy X-ray absorptiometry (DXA, Hologic QDR 4500 W, Waltham, MA). A single X-ray absorptiometry was used to scan for calcaneus aBMD (GE X-ray Madison, WI). Specific DXA aBMD measurements were made for each of the lumbar spine (L1–L4), femoral neck, femoral trochanter, Ward’s triangle, and lower leg. The DXA scanner was blinded to group assignments of the participants.
Tibial bending strength assessment
We employed the MRTA instrument (Gait Scan, Inc., NJ, USA) to assess tibial bending strength. A single trained researcher (MTCL) performed the MRTA measurements and analyzed all measures per manufacturer’s standard protocol and was blinded to group assignments of the participants. The utility of MRTA technology has been reported elsewhere [19, 23].
Briefly, the MRTA instrument assesses, non-invasively, the mechanical properties of the tibia by measuring the mechanical response of the bone to low-frequency random vibration generated by a mechanical shaker through a probe placed on the skin and subcutaneous tissue over the mid-diaphysis of the tibia (Fig. 1). Each MRTA measurement produces an impedance response curve across all signal frequencies. From the tibia MRTA measurement, cross-sectional bending strength, EI in Nm2, was obtained. The E is represented by the material elastic property of Young’s modules, and the I represents the cross-sectional moment of inertia and resistance of bending loads reflecting structural geometry. The product of EI represents bone bending strength [22, 23]. The EI is calculated using the relation based on elementary beam theory: EI = kb L3 / 48, where kb is the lateral bending strength and L is the total bone length [23, 24]. The relationship between EIMRTA and DXA obtained BMD with in vivo monkey tibia and frozen monkey tibia was R2 = 0.98 and 0.89, respectively [24]. The upper limit of an acceptable measurement for root mean squared error (RMSE) for all MRTA measurements was set at < 8%; our RMSE range was 3–7%. The average CV of the MRTA measurement was 4.5% for the tibial EI.
Cross-link deoxypyridinoline assay
Urinary cross-link deoxypyridinoline (µDPD) is a bone resorption marker. Subjects’ baseline and 6-month urine specimens were obtained after a 10-h overnight fast and adequate hydration. Analysis for µDPD (Metra kit for deoxypyridinoline crosslink EIA, Quidel Corporation, Santa Clara, CA) and creatinine (Metra creatinine kit, Quidel Corporation) for all specimens from each subject was carried out in duplicate on the same day by the same investigator (SBA) blinded to the group assignment of the subjects at the conclusion of the study. The within subject variability (CV) for µDPD and creatinine assay was 8.8% and 8.2%, respectively.
Power analysis for sample size determination
For multiple group comparison, the sample size for a directional hypothesis with a desired power of 0.80, and a significance level at 0.05, was estimated to be 78 participants [26]. Vainionpää et al. [27] used a random sample of 80 women (aged 35 to 40 years old) assigned to high-impact exercise (n = 39) or non-exercise control (n = 41), respectively, for femoral neck, intertrochanteric, and total hip BMD as the outcome variables. Our sample sizes of 90 women assigned to resistance training (RT, n = 32), high-impact step aerobics (SA, n = 30), and non-treatment control (CON, n = 28) were sufficient to conduct the analyses without committing a type II error related to the primary purpose of the study outcome variables.
Statistical analyses
Data were analyzed using the SAS statistical software (version 8.0.2). Initially, group (resistance training, high-impact step aerobics training, and control) differences in baseline anthropometric, physiological, bone mineral density, and bone bending strength data were compared using analysis of variance. These comparisons were done among those who completed the 6-month intervention and had follow-up aBMD and bone bending strength data. Similar comparisons were done across ethnic groups where sufficient samples were available (European-White, Hispanic, and Asian). All variables tested between groups using ANOVA were continuously distributed. Analysis of covariance, with repeated measures across all factor, was used to examine for independent group differences in changes from baseline to 6 months in the primary outcome variables of aBMD and bone bending strength. In addition to the baseline measure of the outcomes being assessed, covariates included in the statistical analyses were age; ethnic group (in comparison to European-White); and baseline obtained measures of weight, height, fat mass, and lean mass. When a significant group difference in any outcome was present, a repeated measures ANCOVA was performed for that variable, with the group entered as the between subject factors and the 2 time points entered as within subject factors. Statistical significance was set at alpha < 0.05. Results are presented as means ± SD or means ± SE as indicated.
Results
Sixty-nine participants (a 77% retention rate and met a 80% or better session attendance) completed the 6 month assessments. Mean (± SD) age of the subject cohort was 24.9 (± 4.7) years, with a range from 20 to 35 years. Overall, at enrollment, 28 (31%) subjects were European-White, 4 (4%) African-American, 32 (36%) Hispanic, and 26 (29%) Asian. A number of subjects who completed the intervention and the 6-month follow-up analyses for aBMD and tibial bending strength measures were 22 (RT), 26 (SA), and 21 (CON). These subjects form the basis of the analyses below.
The randomization process balanced all characteristics, with the exception of age which was slightly greater in the CON group as compared to the RT and SA group (p < 0.01 or 0.02) (Table 1). There were no significant differences in other baseline anthropometric and physiological parameters and in baseline aBMD among the groups. Also, there were no group differences in baseline measurements of tibial bending strength and bone resorption biomarker (µDPD).
Table 2 compares group differences in changes from baseline to 6 months for aBMD (g/cm2) and tibial bending strength, EI (N/m2), adjusted for baseline measures and covariates. The covariates include age; ethnic group (in comparison to European-Whites); and baseline obtained measures of weight, height, and lean mass. Changes from baseline to 6 months were significantly greater for calcaneus aBMD (3.3% vs -0.3%, p = 0.004) in the SA group as compared to the RT group. Changes for lumbar spine 2 (L2) aBMD (0.8% vs -1.5%, p = 0.02) from baseline to 6 months were greater in the SA group relative to the CON group; and changes in lower leg aBMD (0.9% vs -0.3%, p = 0.02) from baseline to 6 months were also greater in the SA group relative to the RT group. From baseline to 6 months, insignificant negative changes in trochanter, Ward, femoral neck, and total hip aBMD were found in the SA group relative to the RT group. Also, no significant group differences from baseline to 6-month changes in tibial bending strength and µDPD were noted.
Note that there were differences across the major represented ethnic groups (European-White, Hispanic, and Asian) in several key covariates, as well as in aBMD and tibial bending strength variables. Height, weight, and body mass index were all lower in Asian than in European-White or Hispanic ethnic groups (p < 0.05 to p < 0.001) (data not shown). Because of lower body weight, total lean body mass was also lower in Asian than in European-White or Hispanic groups (p < 0.01 to p < 0.001) (data not shown).
Discussion
Our results show that SA increased aBMD of the calcaneus, L2, and lower leg, while RT induced no significant changes from baseline to 6 months in any of these measures. SA experienced an insignificant reduction in trochanter, Ward, femoral neck, and total hip aBMD relative to RT (Table 2).
High-impact step aerobics exercise did not increase aBMD at any sites at the trochanter, Ward, femoral neck and total hip, or tibial bending strength (Table 2). Our results conflict with several previous studies using high-impact step aerobics exercise. Vainionpää et al. [2] demonstrated a significant change after 52 weeks of progressive high-impact exercise three times per week in femoral neck aBMD in comparison to a non-exercise control group (1.1% vs -0.4%; p = 0.003), intertrochanteric aBMD (0.8% vs -0.2%; p = 0.029), and total hip aBMD (0.1% vs -0.3%; p = 0.006). There were no exercise-induced effects in the L2–L4 aBMD [2]. In previous research, aerobic exercise with intermittent bouts of high-impact activity has been shown to induce a significant increase in aBMD of the trochanter but not at the femoral neck or Ward’s triangle [28]. Further, a 1–2% increase in aBMD at the hip was reported after 72 weeks of training [13]. From another study, using a combination of high-impact exercise and resistance training programs, researchers found a 2.6% increase in aBMD at the trochanter after 104 weeks of participation [29]. In the present study, we observed that the SA training protocol induced a significant increase in aBMD of the calcaneus (3.3% vs -0.3% in RT, p = 0.004), L2 (0.8% vs -1.5% in CON, p = 0.02), and lower leg (0.9% vs -0.3% in RT, p = 0.02) (Table 2), indicating that aBMD at sites proximal to the impact forces such as the calcaneus and lower leg other than the hip were affected by the high-impact step aerobics exercise. Notably, the SA protocol did not induce an osteogenic response in tibial bending strength. It is possible that the high-impact SA training protocol employed in our study may not have been of sufficient duration to induce osteogenic effect on aBMD at the hip, femoral neck, and L1–L4. However, the SA protocol (from week 8 to week 26) provided an average of 50 high-impact landings per session. The amount of force acting on the skeleton during the landing phase averaged 4.2 times body weight which was comparable to previously reported values for similar exercises [29].
The lack of osteogenic response of the tibial bending strength and lack of change in hip and L1–L4 aBMD suggests that the total number of weeks (i.e., 26 weeks) and/or the high-impact step aerobics training routine were not sufficient for generating an osteogenic response at these sites. The hip, L1–L4 vertebrae, and the tibia were not impacted by the loading forces during SA training. In support of this assumption are the results obtained from the µDPD, a bone resorption marker, representing general systemic osteogenic effect in bones. The possibility exists that our high-impact step aerobics routine did not reach a minimum effective strain stimulus for inducing osteogenic responses in the hip, L1–L4 vertebrae, or tibia, regions which were not proximal to the impact loading forces [30]. This was evidenced in the negative aBMD outcomes of total hip and L1–L4 vertebrae from the DXA scan in the SA group and in the absence of a change in the tibial bending strength derived from MRTA assessment (Table 2). It is worth noting that the tibial bending strength (i.e., EI) obtained from the MRTA analysis measured only the tibia without involving the fibula and calcaneus, whereas the lower leg aBMD obtained by DXA scan included the tibia and fibula which may help to explain the disconnect between the observed tibial bending strength and aBMD results for the lower leg.
The moderate-intensity resistance training program, based upon traditional periodized cycles [31], was designed to generate resistive forces up to 80% of 1-RM, which was greater than that employed in other studies that also used sedentary participants [15, 32]. Our RT design did not result in significant changes in L1–L4 aBMD or total hip aBMD (Table 2). In contrast, people engaged in long-term, competitive resistance training tend to have greater aBMD than others [33, 34], although not necessarily at the hip [34]. The RT duration, in terms of number of weeks, employed in the present study might not have been long enough to induce site-specific osteogenic responses in the bone. Other studies employing RT have failed to report changes in aBMD at the hip or L1–L4 following 26 weeks [35], 52 weeks [9, 15], and up to 156 weeks of “nonstrenuous” resistance training [36]. Additionally, our RT protocol did not induce an osteogenic response on tibial bending strength (Table 2).
This study has limitations that should be addressed. The primary outcome of our study is aBMD change; however, it has the inherent limitations for bone strength and fracture analysis. It has been shown that bone mineral content and structural adaptation due to exercise training can enhance mechanical load [19, 37]. However, only approximately 60–70% of bone strength adaptation can be explained by aBMD, and other characteristics of the quality of bones are not included (i.e., microarchitecture) [38]. Therefore, aBMD changes, assessed by DXA, may not be a perfect indicator of osteogenic response to exercise training. In the present study, the absence of broad changes to bone density or tibial bending strength could be related to the length of the study (i.e., 26 weeks) or the intensity of musculoskeletal loading during resistance training (i.e., 65–80% 1-RM in the RT).
We conclude that sedentary premenopausal women engaging in 6 months of high-impact aerobic exercise improved aBMD in the calcaneus, lower leg, and L2, not tibial bending strength. Moderate-intensity resistance training failed to elicit significant effects on site-specific aBMD or tibial bending strength, relative to controls and to high-impact aerobic exercise. The direct clinical importance of the positive changes in calcaneus, lower leg, and L2 aBMD in SA are not known. The generalizability of these responses can be extended to women in the 20–35-year age range who are using hormonal birth control. The lack of osteogenic response on other skeletal sites in the SA and RT group may be due to short intervention duration (i.e., 26 weeks). Further research is warranted to elucidate the applicability of combining RT and SA protocols or combining RT, SA, and whole-body vibration training with longer intervention length of 52 weeks for improvement or maintenance of aBMD in the lumbar spine and femoral neck and tibial bending strength in sedentary premenopausal women.
References
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
Vainionpää A, Korpelainen R, Leppäluoto J, Jämsä T (2005) Effects of high-impact exercise on bone mineral density: a randomized controlled trial in premenopausal women. Osteoporos Int 16:191–197
Gordon CM, Zemel BS, Wren TA, Leonard MB, Bachrach LK, Rauch F et al (2016) The determinants of peak bone mass. J Pediatrics 180:261–269. https://doi.org/10.1016/jjpeds.2016.09.056
Riggs BL, Melton L Jr (1992) The prevention and treatment of osteoporosis. N Engl J Med 327:620–627
Marcus R, Greendale G, Blunt BA et al (1994) Correlates on bone mineral density in postmenopausal estrogen/progestin intervention trial. J Bone Miner Res 9:1467–1476
Center JR, Nguyen TV, Schneider D et al (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA et al (2001) Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA 286:2815–2822
Hauselmann HJ, Rizzoli R (2003) A comprehensive review of treatment for postmenopausal osteoporosis. Osteoporos Int 14:2–12
Liang MTC, Bruan W, Basin SL, Dutton D, Pontello A, Wong ND, Spalding TW, Arnaud SB (2011) Effect of high-impact aerobics and strength training on BMD in young women aged 20–35 years. Int J Sports Med 32:100–108
Kelley GA, Kelley KS, Kohrt WM (2013) Exercise and bone mineral density in premenopausal women: a meta-analysis of randomized controlled trials. Int J Endocrinol 2013:741639. https://doi.org/10.1155/2013/741639
Gourlay MC, Brown SA (2004) Clinical considerations in premenopausal osteoporosis. Arch Intern Med 164:603–606
Taaffe DR, Robinson TL, Snow CM, Marcus R (1997) High-impact exercise promotes bone gain in well-trained female athletes. J Bone Miner Res 12:255–260
Friedlander AL, Genant HK, Sadowsky S, Byl NN, Glüer CC (1995) A two-year program of aerobics and weight training enhances bone mineral density of young women. J Bone Miner Res 10:574–585
Gleeson PB, Protas EJ, LeBlanc AD, Schneider VS, Evans HJ (1990) Effects of weight lifting on bone mineral density in premenopausal women. J Bone Miner Res 5:153–158
Vuori I, Heinonen A, Sievänen H, Kannus P, Pasanen M, Oja P (1994) Effects of unilateral strength training and detraining on bone mineral density and content in young women: a study of mechanical loading and deloading on human bones. Calcif Tissue Int 55:59–67
Bassey EJ, Ramsdale SJ (1995) Weight-bearing exercise and ground reaction forces: a 12-month randomized controlled trial of effects on bone mineral density in healthy postmenopausal women. Bone 16:469–476
Bassey EJ, Rothwell MC, Littlewood JJ, Pye DW (1998) Pre- and postmenopausal women have different bone mineral density responses to the same high-impact exercise. J Bone Miner Res 13:1805–1813
Heinonen A, Kannus P, Sievänen H, Oja P, Pasanen M, Rinne M, Uusi-Rasi K, Vuori I (1996) Randomised controlled trial of effect of high-impact exercise on selected risk factors for osteoporotic fractures. Lancet 348:1343–1347
Liang MTC, Arnaud SB, Steele CR, Hatch P, Moreno A (2005) Ulnar and tibial bending stiffness as an index of bone strength in synchronized swimmers and gymnasts. Eur J Appl Physiol 94:400–407
Hutchinson TM, Bakulin AV, Rakhmanov AS, Martin RB, Steele CR, Arnaud SB (2001) Effects of chair restraint on the strength of tibia in rhesus monkeys. J Med Primatol 30:313–321
Kiebzak GM, Box JH, Box P (1999) Decreased ulnar bending stiffness in osteoporotic Caucasian women. J Clin Densitom 2:143–152
Steele CR, Zhou L-Z, Guido D, Marcus R, Heinrichs WL (1988) Cheema C Noninvasive determination of ulnar stiffness from mechanical response – in vivo comparison of stiffness and bone mineral content in humans. J Biomech Eng 110:87–96
Arnaud SB, Steele CR, Zhou L-J, Hutchinson T (1991) Marcus R (1991) A direct non-invasive measure of long bone strength. Proc Ann Int Cong IEEE Eng Int Med Biol Soc 13:1984–1985
Roberts SG, Hutchson TM, Arnaud SB, Kirati BJ, Martin RB (1996) Steele CR (1996) Noninvasive determination of bone mechanical properties using vibration response: a refined model and validation in vivo. J Biomech 29(1):91–98
American College of Sport Medicine, ACSM’s guideline for exercise testing and prescription, 10th edn. Wolters Kluwer, Philadelphia, p 4–8
Thomas JR, Nelson JK (2001) Research methods in physical activity, 4th edn. Human Kinetics, Champaign, p 138–140
Vainionpää A, Korpelainen R, Vihriala E, Rinta-Paavola A, Leppaluoto J, Jamsa T (2006) Intensity of exercise is associated with bone density change in premenopausal women. Osteoporos Int 17:455–463
Bassey EJ, Ramsdale SJ (1994) Increase in femoral bone density in young women following high-impact exercise. Osteoporos Int 4:72–75
Heinonen A, Sievänen H, Kannus P, Oja P, Vuori I (1996) Effects of unilateral strength training and detraining on bone mineral mass and estimated mechanical characteristics of the upper limb bones in young women. J Bone Miner Res 11:490–501
Frost HM (2003) Bone’s mechanostat: a 2003 update. Anat Rec A Discov Mol Cell Evol Biol 275:1081–1101
Stone MH (1990) Muscle conditioning and muscle injuries. Med Sci Sports Exerc 22:457–462
Pruitt LA, Taaffe DR, Marcus R (1995) Effects of a one-year high-intensity versus low-intensity resistance training program on bone mineral density in older women. J Bone Miner Res 10:1788–1795
Heinonen A, Oja P, Kannus P, Sievänen H, Mänttäri A, Vuori I (1993) Bone mineral density of female athletes in different sports. Bone Mineral 23:1–14
Tsuzuku S, Ikegami Y, Yabe K (1998) Effects of high-intensity resistance training on bone mineral density in young male powerlifters. Calcif Tissue Int 63:283–286
Chilibeck PD, Calder A, Sale DG, Webber CE (1996) Twenty weeks of weight training increases lean tissue mass but not bone mineral mass or density in healthy, active young women. Canadian J Physiol and Pharmaco 74:1180–1185
Sinaki M, Wahner HW, Bergstralh EJ, Hodgson SF, Offord KP, Squires RW, Swee RG, Kao PC (1996) Three-year controlled, randomized trial of the effect of dose-specified loading and strengthening exercises on bone mineral density of spine and femur in nonathletic, physically active women. Bone 19:233–244
Wang Q, Nicholson PH, Suuriniemi M, Lyytikainen A, Helkala E et al (2004) Relationship of sex hormones to bone geometric properties and mineral density in early pubertal girls. J Clin Endocrinol Metab 89(4):1698–1703
Ammann PR, Rizzoli R (2003) Bone strength and its determinant. Osteoporos Int 14:13–18
Acknowledgements
We would like to acknowledge Dr. Scott Stevenson who designed the resistance training program; our graduate students for their assistance in the project; and the participants for their time, effort, and commitment in completing the study.
Funding
This project was supported by The National Institutes of Health Grant GM053933-06 to M.T.C.L., D.J.D., W.A.B., and S.L.B.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dutto, D.J., Liang, M.T.C., Braun, W.A. et al. Effect of 6-month high-impact step aerobics and resistance training on BMD and tibial bending strength in sedentary premenopausal women. Osteoporos Int 33, 695–701 (2022). https://doi.org/10.1007/s00198-021-06106-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06106-y