Abstract
Summary
Data on direct and indirect costs of clinical fractures in 116 osteoporotic patients 50 years and older were prospectively collected using cost diaries. Indirect costs accounted for roughly half of the total costs, with a contribution of at least 81 % of these costs in employed patients.
Introduction
The aim of this prospective study was to gain insight into the current total costs of clinical fractures in osteoporotic patients aged 50 years and older.
Methods
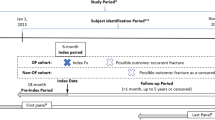
In a study in the Netherlands, patients prospectively filled out cost diaries every 3 months, during 1 year after a clinical fracture. Primary analyses were performed on those patients with all four cost diaries returned. In-depth analyses of indirect costs were performed, dividing results for employed and unemployed patients. Sensitivity analyses using imputation techniques were performed on patients who returned two or three diaries
Results
Of the 116 included patients, 69 completed all four diaries, 24 only two or three, and 23 patient completed one or no diaries. For all fractures, approximately 50 % of the total costs were due to indirect costs; employed patients contributed for at least 81 % of the indirect cost. Humerus fractures were most expensive with a total 1-year cost of €16.841 per patient. Indirect costs in the group with clinical spine fractures were highest (€12.522), accounting for 89.1 % of the total costs for this fracture.
Conclusion
Indirect costs account for roughly half of the total costs of clinical fractures, which are largely related to sick leave. When performing cost analyses in fracture patients, we advise a societal perspective in which indirect costs are also considered, and to apply a patient derived prospective data collection method to get a ‘true’ and complete image of the total costs due to clinical fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a disease which is characterized by low bone mineral density and bone fragility, increasing the risk of fractures [1]. It is estimated that in the Netherlands each year around 80.000 persons aged 50 years or older experience a clinical fracture [2]. Several studies have shown that osteoporotic fractures not only decrease physical functioning and vitality of elderly patients, but also have large (socio)economic consequences for the patient and the society [3–7]. It is predicted that costs will even rise further due to an increase of elderly people leading to a raise in osteoporosis prevalence and fracture incidence [8, 9]. Worldwide, several studies have been performed in which the economic burden of this disease was assessed, including only direct medical costs in most studies. These costs or often derived from several (national) databases as this information is easier to collect than indirect costs, especially when study populations are large [4, 10]. But it is recommended that for cost-effectiveness studies, a societal perspective is applied in which all kind of costs need to be considered (both direct and indirect costs), especially in chronic disorders which are known to have severe socioeconomic impact [11]. Some studies did include indirect costs, but also in these studies data were retrieved from databases [7, 12], retrospective surveys of patients or questionnaires [13, 14]. A limitation of these methods is recall bias, no availability of detailed resource use, and no insight in medical consumption which is not covered by insurance companies. Therefore cost diaries have more advantages than information from questionnaires of surveys, particularly when they are used in a prospective design [11]. Recently, the ASBMR taskforce have given the advice to set up fracture liaison services (FLS) to screen for osteoporosis in as much as possible elderly patients with recent fractures, since subsequent fracture risk is high in elderly with a recent fracture, and since effective and relatively safe anti-osteoporotic drugs are available [15]. But up to now, no one has calculated the costs of such a service. In this article, we will show both the direct and indirect costs of osteoporotic fractures using cost diaries to collect prospective patient data.
Patients and methods
FLS patient population
Four hospitals throughout the Netherlands set up a FLS, and also participated in a study in which the effect of the FLS on preventing new fractures was assessed, and to see if compliance to subsequent treatment of osteoporosis in patients with a fracture was increased [16]. For this study, patients aged 50 years and older, presenting with a low trauma fracture at the emergency room (ER) between July 2007 and December 2008, were invited for osteoporosis screening at the FLS. All patients were treated according to protocol, including DXA and LVA (=lateral vertebral assessment evaluation), and evaluation of fall risk and presence of secondary osteoporosis. The protocol is described more in detail in the study of Eekman et al. [16]. When osteoporosis was diagnosed and included into this study, treatment with calcium, vitamin D and bisphosphonates, as secondary prevention, was started.
Cost study
Structure and components of the cost diary
As part of this larger trial, one centre (VU University medical center (VUmc)) asked their patients to maintain cost diaries in the first year after their fracture, in which all actual costs due to clinical fractures were collected, in line with a societal perspective. The medical ethics commission of the VUmc approved this study, and informed consent was obtained before inclusion. Each diary covered a period of three months. Every diary was presented on an A4 paper (see Appendix). The diaries are a modified version of the diaries used in an earlier published article [17]. Instructions on how to fill out the diaries were given during inclusion into the study. During every quarterly contact, patients were asked to return the diary, and a new one for the upcoming three months was sent. To stimulate a high response, prepaid envelopes were provided to the patients.
To allow multiplication with unit prices, patients were asked to record resource use as detailed as possible. The following resource use was requested:
-
(a)
Direct medical costs: all costs related to the visits of the general practice, specialist care, paramedic care, days of hospitalisation, need of plaster or surgical interventions, use of anti-osteoporotic drugs and out-patient and in-patient care.
-
(b)
Direct non-medical costs: all costs paid by the patients and their family such as over-the-counter medication, need for paid and unpaid household help, transportation and alternative therapies.
-
(c)
Indirect costs: all costs related to costs arising from sick leave (absenteeism). Both paid work and voluntary work was included.
In addition to the diaries, two other sources were consulted to assess resource use: (1) patient medical records specifying for probable secondary osteoporosis and number of hospitalization days. And (2), the electronic hospital administration system was consulted to retrieve information on costs for operations and physical therapy.
The valuation of resource use
In the Netherlands, hospitals are paid by tariffs per DRG (diagnosis related group). In this study however, we looked at true costs related to individual fractures. The applied cost structures dated from 2008 and, if necessary, prices were updated using the Dutch consumer price index (www.cbs.nl). No discounting was used. Appendix 2 provides the applied costs per unit of resource use.
According to Dutch guidelines, vertebral fracture assessments (VFA) were performed in all patients without any extra costs [2]. Standard cost prices were used for a hospitalization day, outpatient care (specialists), a visit to a therapist (e.g. physiotherapy, manual therapy, occupational therapy), an hour of help in the housekeeping and an hour of voluntary work [18]. Prices of medication were obtained through a national website which provides the costs of all medications [19]. Costs of operations of severe or complicated fractures, e.g. hip or humerus fracture, including the necessary radio diagnostic tests, were computed by the department of planning and control of the VUmc. All radiologic diagnostic tests made in relation to the fracture during one year of follow-up were taken into account.
Sick leave from paid work was valued according to the friction cost method, that is, only sick leave during a friction period (22 weeks) needed to replace a person is taken into account [18, 20]. This method leads to more accurate cost data, compared to the human capital method (which assumes costs due to unproductivity by the sick person as long as this person is sick). This leads to an overestimation of the costs. Using the shadow price method, unpaid work was valued at the cost of the professional required to replace the unpaid worker [18, 21]. The shadow price of voluntary work and informal care was assumed to be equal to the tariff for cleaning work.
Statistical analyses
Completers analyses
Primary analyses were performed using the data of patients who returned all four cost diaries. Per type of resource, the mean costs per patient per year were calculated. As cost data are typically skewed, confidence intervals (CI) for costs were estimated using bias-corrected accelerated bootstrapping techniques. In brief, 2000 datasets of the same sample size as the original dataset were sampled with replacement from the original data [22, 23]. Due to small sample sizes, no statistical analyses were performed to assess differences in costs between the different types of fractures. Only descriptive data was assessed with Statistical Package for the Social Sciences (SPSS statistical software, Version 15.0; SPSS, Inc., Chicago, IL, USA) and StataSE 12.
Sensitivity analyses
At first, sensitivity analyses were performed in those patients who returned two or three cost diaries. Three different imputation methods were used: (1) zero imputation method, in which all resource use was considered to be zero for the missing dairies. (2) Means imputation method: per time period the means for direct (medical and non-medical), indirect and total costs of those patients who did return the dairies, were calculated. These mean values were imputed for the missing diaries at each time period separately. And (3) the Expectation Maximization (EM) Algorithm method was used. This is an iterative optimisation method to estimate missing data given available data, using SPSS 12.0.1 [18]. Secondly, sensitivity analyses were performed using the completers group and the group who returned two or three diaries. Imputation techniques were the same as described above.
Assumptions
If data in the diaries were incomplete and could not be retrieved through the earlier described data sources (patient medical records, and hospital system), some assumptions were made to limit missing data. Firstly, related to physiotherapy visits: if frequency was missing, we assumed a visit of once a week. Secondly, concerning care from family/relatives, if total hours of help were not given, we assumed a frequency of 1 h twice a week. This allowed for a maximum of 26 h of help in 3 months. Thirdly, concerning medication, if dose was not specified, a worst case scenario was assumed. For example: for acetaminophen the assumption of six pills per day was made, which summed up to 504 pills per 3 months. For injections, the total amount in milligrammes (mg) was calculated, and converted to the number of pills of that same substance.
Results
Baseline characteristics
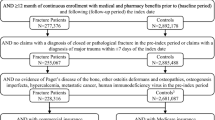
Totally, 278 patients of 50 years and over with a recent fracture visited the FLS of the VUmc. From these VUmc patients, 58 had a normal T-score, 100 patients a T-score between 1 and the −2, and 120 patients had a T-score of ≤2. Arbitrarily, we had previously defined that patients 50 years and over with a recent fracture, and a T-score < −2 had an indication for anti-osteoporotic treatment, in accordance with other FLS services [24]. These patients were suitable for this sub-study. Four patients were excluded, as these patients had hand/feet fractures. Of the 116 patients, 23 either never returned a cost diary or only one, 24 patients returned two or three diaries and 69 patients completed all diaries. Table 1 shows the baseline characteristic per subgroup of returned diaries. The patients in the primary analysis (n = 69) were mostly women (81.2 %) and had a mean age of 65 years (SD 9). About 41 % of these patients were employed, and wrist fractures were the most common fractures (n = 23, 33.3 %). Mean spine T-score was −2.07 (SD 0.78) and mean hip T-score was −1.46 (SD0.78). The group of patients who returned two or three diaries or zero or one dairy was comparable with the completers. Only the mean age was three years higher in the group with 2/3 diaries and in both groups less patients were employed, compared to the completers.
Completers analyses
All costs per fracture are specified in Table 2. Regardless type of fracture, our 69 patients were hospitalized for a total of 138.01 days, with a mean length of stay of 2 days. Total costs for hospitalization were €71.215, corresponding to a mean cost of €1.032 per patient. Humerus fractures were the most expensive fractures with total costs of €16.841 per patient per year of which 47.4 % were direct costs (medical and non-medical) and 52.6 % indirect costs. The second most expensive fracture was a clinical spine fracture (total costs €14.048: 10.9 % direct and 89.1 % indirect costs). Total costs for a wrist fracture were lowest (€4.014: 35.8 vs. 64.2 % direct and indirect costs respectively) followed by elbow fractures (€7.741: 35.0 % direct costs vs. 65.0 % indirect costs). Direct medical costs were highest for hip fractures (€9.929) which is mostly driven by the large number of hospitalization days (8 vs. 0.8 days for wrist fractures) compared with other fractures.
Indirect costs
In the completers group, for all fractures except hip, indirect costs represent more than half of the total costs (approximately 60 % in most fracture types). Although clinical spinal fractures provide the lowest direct medical and non-medical costs, indirect costs in this group were highest accounting for 89.1 % of the total costs for this type of fracture.
When looking in-depth in the indirect costs (Fig. 1), almost all of these costs are due to sick leave in employed patients. Unemployed patients consisted of retired, unemployed and work disabled patients. For example, employed patients with a wrist fracture (n = 5) had mean indirect costs of €9.553 compared to €638 for unemployed patients (n = 18). Thus, 80.6 % of the mean total indirect costs in wrist fractures (€2.575) are produced by employed patients. We calculated this as follows: (a) total indirect costs is (5 × €9.553 = €47.765) + (18 × €638 = €11.484) = €59.249; (b) the percentage of the mean total indirect costs of wrist fractures due to employed patients is (€47.765 / €59.249) × 100 = 80.6 %; (c) mean indirect costs of all wrist fracture patients is €59.249 / 23 = €2.575. We applied this for all fracture types resulting in the fact that in the group of patients with ankle fractures, mean total indirect costs were mainly driven by employed patients (96.4 %), and for all other fractures 95 % or more of the total indirect costs were due to employed patients.
Sensitivity analyses
At first, a sensitivity analyses was performed on only the group of patients with two or three patients (Table 3). Thirteen patients completed three diaries and eleven patients completed two. As expected, costs are lower in this group as less patients were employed, leading to less indirect costs. Despite this fact, mean indirect costs still account for at least 50 % of the mean total costs when looking at the means and EM imputated data. Only in patients with ankle fractures this percentage is lower (40–46 %) compared to that in the completers group (67 %). In patients with a hip fracture, indirect costs account for roughly 10 % of the total costs compared to 21 % in the completers group. But both percentages are low compared to indirect costs in other fractures. Direct medical and non-medical costs are somewhat higher in this group of patients, compared to the completers group (approximately 40–50 vs. 35–45 %). No confidence intervals have been retrieved for these analyses as the population numbers are too small, creating instable confidence intervals.
Secondly, a sensitivity analyses was performed combining patients with four diaries returned and those returning two or three diaries (n = 93). Results of these analyses can be found in Appendix 2. Costs were similar or lower than in the primary analysis. Patients with a clinical spine fracture (n = 4) returned all four diaries. As such, costs in the sensitivity analysis are the same as in the primary analysis.
Discussion
In this study, patients 50 years and over with recent fractures and a low T-score filled out cost diaries, prospectively, for 1 year. The key message is that indirect costs account for roughly half of the total costs of clinical fractures, which is largely related to sick leave. For instance, humerus fractures produced the most total costs (€16.841) of which more than half is due to indirect costs. Sick leave in employed patients account for at least 81 % of the mean indirect costs for a fracture.
Our observation that at least 50 % of the total costs are due to indirect costs, regardless of type of fracture (hip and clinical fractures aside), is much higher compared to estimations in other studies. For example, in the study of Tarride et al., performed in Canada, only 5 % of the total costs were derived from indirect costs [6]. This was calculated using several assumptions. No actual sick leave data was used. Another study, performed in Austria, found a contribution of 34 % of indirect costs on the total costs, also based on data from national databases and calculation assumptions [13]. A study performed in Sweden used data for indirect costs, retrieved during retrospective patient surveys [25]. Patients were asked about days of sick leave in the past 4 weeks prior to a visit. A mean total of sick leave per period was then calculated. In this study, only patients with wrist fractures were employed (32 %), leading to total indirect costs of €43.992. This is comparable with the indirect cost in employed patients with a wrist fracture in our study (n = 5, 22 %, total indirect costs €47.765). But the contribution per patient in our study is considerably higher than in the study from Sweden, which might be due to the prospective way of data collection used in our study, compared to the retrospective method in Sweden. And we collected actual data per three months, as the study in Sweden collected data per 4 weeks prior to a visit and extrapolated this to a longer period, which might lead to an underestimation of the true costs.
To compare our data with other studies, we need to look at direct costs as well. Hospitalization costs in our study were low. For example, in a study performed in Switzerland, mean hospital costs per patient were €11,850.70 (14.616 CHF) for a clinical fracture, regardless type of fracture. These costs were mainly driven by hip fractures who have the longest stay in a hospital (mean 19.1 days), accounting for at least 50 % of these costs [4]. This is comparable in a Canadian study (mean 15.5 days, 50 % of the costs) [6, 7], and in several other studies [3, 13, 26–28]. In Ireland, this percentage was lower (about 35 %, mean 21.4 days) [8]. In our study, patients with a hip fracture were hospitalized for a mean of 8 days, which is substantially lower than in other countries. Also, only four patients (5.8 %) in our study had a hip fracture. This is not in line with the prevalence of hip fractures in the Netherlands (16.1 %) [2, 16]. Assuming this percentage would have been present in our study, 11 patients of the 69 would have had a hip fracture. This would substantially increase the contribution of the costs of hip fractures on the total costs for all fractures in our study, probably also accounting for half of the hospitalization costs, in line with other studies.
This study has several strengths and limitations. One of the strengths of this study is the use of cost dairies. This method allows for a more complete prospective data collection from patients, reducing recall bias in comparison to retrospective patient surveys or questionnaires [11]. There are no other studies performed in this type of patients using cost diaries. This makes our data rather unique. Another strength is that our study is unique in the in-depth analyses of indirect costs. When looking at the contribution of employed patients on the indirect costs, at least 81 % of these costs are due to sick leave and/or productivity loss. As far as we know, no other study has investigated this before. We think it is much better to include all costs, not only the direct (non)medical costs, usually paid by health insurance companies, but also the indirect costs (mainly influencing the financial status of the fracture patients themselves) to assess the economic burden of osteoporotic fractures.
A first limitation of this study is the relatively low population number in comparison with other performed studies. This might be due to the fact that we did not use information from databases, but prospective real-life data from diaries from patients. It is well-known that using cost diaries as a data collection method, is more time-consuming for patients and professionals, especially when the data needs to be entered in databases that can be analysed. However, in this study, the response rate for the dairies was acceptable as 82 % of the patients returned at least two diaries, and 59 % of the patients completed all four diaries over the 1-year follow-up.
A second limitation is the fact that only a few patients in this study had a hip or a clinical spine fracture. In this study, mostly hip fracture patients with relative good functional capacity came to the FLS, while those with severe immobility and comorbidity were not capable of visiting the outpatient clinic (e.g. residing in a nursing home) [16]. Related to the clinical spine fractures, in general, two out of three patients with this type of fracture, do not present with signs and symptoms of an acute fracture on the ER [29]. The indirect costs for hip fracture patients were the lowest (20.9 %), and for clinical spine fractures, the highest (89.1 %). In both groups, only two patients were employed, but apparently patients with a hip fracture experienced less sick leaves or received less salary compared to the employed patients with a clinical spine fracture. We have not found an explanation for this difference, other than the fact that the number of patients is very low.
In the diaries, patients were asked to fill out how often a visit to a therapist occurred. We did not ask for the specific costs the patient had to make to visit the therapist. These costs can of course fluctuate between patients, but we used mean costs derived from several tariffs from several therapist in the Netherlands. This might influence the data, but we think this contribution will not be large in relation to the total costs. And although our study was performed in the Netherlands, we looked at true costs of DXA measurements, anti-osteoporotic drugs, visiting physical therapists etc. Of course, these direct costs may differ somewhat per country, and there may be variations in indirect costs between countries also. Nevertheless, we assume that when applying a societal perspective in cost studies, the contribution of indirect costs will be roughly the same in other (western) countries, as in our study (50 %).
Another limitation of this study is the fact that these patients were seen in a university hospital, where costs are generally higher than in peripheral hospitals. This might lead to overestimation of costs. Compared to previous studies, the direct medical costs of humerus fractures were higher. But the costs of other types of fractures were comparable, thus probably overestimation in this study is limited [28, 30].
As in the advice of the ASBMR taskforce to improve secondary fracture prevention worldwide, fracture liaison services could play a big role in this solution [15, 24, 31]. To our knowledge, this is the first study assessing the costs of such a service, and also the first to use a patient derived prospective data collection method (cost diary) in this population group. In our study, indirect costs account for 50 % of the total costs of clinical fractures, and are mostly driven by sick leave of employed patients. We are curious to see if other research groups find the same results, which might lead to an improved and completer knowledge of the costs for treatment, and prevention of subsequent clinical fractures.
References
Sambrook P, Cooper C (2006) Osteoporos Lancet 367:2010–2018
Nederlandse Vereniging voor Reumatologie. (2011) CBO richtlijn osteoporose en fractuurpreventie
De Laet CE, van Hout BA, Hofman A, Pols HA (1996) Costs due to osteoporosis-induced fractures in the Netherlands; possibilities for cost control. Ned Tijdschr Geneeskd 140:1684–1688
Lippuner K, Golder M, Greiner R (2005) Epidemiology and direct medical costs of osteoporotic fractures in men and women in Switzerland. Osteoporos Int 16(Suppl 2):S8–S17
Roux C, Wyman A, Hooven FH, Gehlbach SH, Adachi JD, Chapurlat RD, Compston JE, Cooper C, Ez-Perez A, Greenspan SL, Lacroix AZ, Netelenbos JC, Pfeilschifter J, Rossini M, Saag KG, Sambrook PN, Silverman S, Siris ES, Watts NB, Boonen S (2012) Burden of non-hip, non-vertebral fractures on quality of life in postmenopausal women: the Global Longitudinal Study of Osteoporosis in Women (GLOW). Osteoporos Int 23:2863–2871
Tarride JE, Guo N, Hopkins R, Leslie WD, Morin S, Adachi JD, Papaioannou A, Bessette L, Brown JP, Goeree R (2012) The burden of illness of osteoporosis in Canadian men. J Bone Miner Res 27:1830–1838
Tarride JE, Hopkins RB, Leslie WD, Morin S, Adachi JD, Papaioannou A, Bessette L, Brown JP, Goeree R (2012) The burden of illness of osteoporosis in Canada. Osteoporos Int 23:2591–2600
McGowan B, Casey MC, Silke C, Whelan B, Bennett K (2012) Hospitalisations for fracture and associated costs between 2000 and 2009 in Ireland: a trend analysis. Osteoporos Int 24:849–857
Piscitelli P, Gimigliano F, Gatto S, Marinelli A, Gimigliano A, Marinelli P, Chitano G, Greco M, Di PL, Sbenaglia E, Benvenuto M, Muratore M, Quarta E, Calcagnile F, Coli G, Borgia O, Forcina B, Fitto F, Giordano A, Distante A, Rossini M, Angeli A, Migliore A, Guglielmi G, Guida G, Brandi ML, Gimigliano R, Iolascon G (2010) Hip fractures in Italy: 2000–2005 extension study. Osteoporos Int 21:1323–1330
Parthan A, Kruse M, Yurgin N, Huang J, Viswanathan HN, Taylor D. (2013) Cost Effectiveness of Denosumab versus Oral Bisphosphonates for Postmenopausal Osteoporosis in the US. Appl Health Econ Health Policy
Goossens ME, Rutten-van Molken MP, Vlaeyen JW, van der Linden SM (2000) The cost diary: a method to measure direct and indirect costs in cost-effectiveness research. J Clin Epidemiol 53:688–695
Pike CT, Birnbaum HG, Schiller M, Swallow E, Burge RT, Edgell ET (2011) Prevalence and costs of osteoporotic patients with subsequent non-vertebral fractures in the US. Osteoporos Int 22:2611–2621
Dimai HP, Redlich K, Peretz M, Borgstrom F, Siebert U, Mahlich J (2012) Economic burden of osteoporotic fractures in Austria. Health Econ Rev 2:12
Rabenda V, Manette C, Lemmens R, Mariani AM, Struvay N, Reginster JY (2006) The direct and indirect costs of the chronic management of osteoporosis: a prospective follow-up of 3440 active subjects. Osteoporos Int 17:1346–1352
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE Jr, McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27:2039–2046
Eekman D, van Helden S, Huisman A, Verhaar H, Bultink I, Geusens P, Lips P, Lems W. (2013) Optimizing fracture prevention: the fracture liaison service, an observational study. Osteoporos Int. doi:10.1530/boneabs.1.PP43
Coupe VM, Veenhof C, van Tulder MW, Dekker J, Bijlsma JW, Van den Ende CH (2007) The cost effectiveness of behavioural graded activity in patients with osteoarthritis of hip and/or knee. Ann Rheum Dis 66:215–221
Oostenbrink JB, Koopmanschap MA, Rutten FF (2002) Standardisation of costs: the Dutch manual for costing in economic evaluations. Pharmacoeconomics 20:443–454
Medicijnkosten. Themasite van het College voor zorgverzekeringen (CVZ). (2012) Medication costs. Accessed on 26 June 2012
Koopmanschap MA, Rutten FF (1996) A practical guide for calculating indirect costs of disease. Pharmacoeconomics 10:460–466
Busschbach JJ, Brouwer WB, van der Donk A, Passchier J, Rutten FF (1998) An outline for a cost-effectiveness analysis of a drug for patients with Alzheimer's disease. Pharmacoeconomics 13:21–34
Barber JA, Thompson SG (2000) Analysis of cost data in randomized trials: an application of the non-parametric bootstrap. Stat Med 19:3219–3236
Thompson SG, Barber JA (2000) How should cost data in pragmatic randomised trials be analysed? BMJ 320:1197–1200
Gutierrez L, Roskell N, Castellsague J, Beard S, Rycroft C, Abeysinghe S, Shannon P, Gitlin M, Robbins S (2012) Clinical burden and incremental cost of fractures in postmenopausal women in the United Kingdom. Bone 51:324–331
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034
Strom O, Borgstrom F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, Abdon P, Ornstein E, Ceder L, Thorngren KG, Sernbo I, Jonsson B (2008) Long-term cost and effect on quality of life of osteoporosis-related fractures in Sweden. Acta Orthop 79:269–280
Bessette L, Jean S, Lapointe-Garant MP, Belzile EL, Davison KS, Ste-Marie LG, Brown JP (2012) Direct medical costs attributable to peripheral fractures in Canadian post-menopausal women. Osteoporos Int 23:1757–1768
Hopkins RB, Tarride JE, Leslie WD, Metge C, Lix LM, Morin S, Finlayson G, Azimaee M, Pullenayegum E, Goeree R, Adachi JD, Papaioannou A, Thabane L (2013) Estimating the excess costs for patients with incident fractures, prevalent fractures, and nonfracture osteoporosis. Osteoporos Int 24:581–593
Maravic M, Le BC, Landais P, Fardellone P (2005) Incidence and cost of osteoporotic fractures in France during 2001. A methodological approach by the national hospital database. Osteoporos Int 16:1475–1480
Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ III (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7:221–227
van Helden S, Cauberg E, Geusens P, Winkes B, der van Weijden T, Brink P ((2007) The fracture and osteoporosis outpatient clinic: an effective strategy for improving implementation of an osteoporosis guideline. J Eval Clin Pract 13:801–805
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
D. A. Eekman and M. M. ter Wee contributed equally.
Appendix 1: cost diary
Appendix 1: cost diary
Complaints related to your fracture in the upcoming 3 months
-
are you unable to perform paid work?
Number of days sick leave
Total number of hours of sick leave
E.g. 5 days
36 hours
-
… are you unable to perform unpaid work? (e.g. voluntary work, housekeeping)
Number of days
Total number of hours
E.g. 2 days
4 hours
-
… have you visited or consulted your general practitioner?
Number of visits/consultations
Type of visit or consultation (consultation by telephone, at the practice or home visit by GP)
E.g. 3 visits
Visit to the practice
-
… have you received a medication prescription?
Name of medication
Number of pills and dosage
Total used amount
E.g. diclofenac
12 pills, 50 mg
3 pills a day during 4 days
-
… have you purchased medication yourself? (e.g. acetaminophen)
Name of medication
Number of pills and dosage
Total used amount
E.g. ibuprofen
20 pillen van 400 mg
1 pill a day during 6 days
-
… have you purchased other medical aids? (e.g. massage oil, brace)
Date of purchase
Type of aid
Price
E.g. May 30th
Brace
€ 85
-
… have you visited a therapist? (e.g. physiotherapist, chiropractor)
Number of visits
Type of therapist
E.g. 10 visits
Physiotherapist
-
… have you visited an alternative medicine specialist? (e.g. specialized in homeopathy, acupuncture)
Number of visits
Type of therapist
E.g. 2 visits
Acupuncturist
-
… have you visited a specialist? (e.g. orthopedic surgeon, neurologist)
Number of visits
Type of specialist
E.g. 1 visit
Orthopedic surgeon
-
… were radiological or laboratory tests done in the hospital? (e.g. X-ray, MRI-scan, blood test, DXA scan)
Type of test
Number of tests
e.g. X-ray
2
-
…. have you been admitted to the hospital?
Number of days
Which department?
What was the reason for admission?
E.g. admitted for 5 days
Orthopedic surgery
Operation wrist
Room for remarks/costs that do not fit into the tables:
(please be as specific as possible when describing the costs).
Thank you for filling out these forms!!!
Please send this diary as soon as you have completed it
Appendix 2
Appendix 3
Rights and permissions
About this article
Cite this article
Eekman, D.A., ter Wee, M.M., Coupé, V.M.H. et al. Indirect costs account for half of the total costs of an osteoporotic fracture: a prospective evaluation. Osteoporos Int 25, 195–204 (2014). https://doi.org/10.1007/s00198-013-2505-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2505-4