Abstract
Background
Numerous studies have shown that portal vein resection during pancreatectomy can help achieve complete tumor clearance and long term-survival. While the safety of vascular resection during pancreatectomy is well documented, the risk of superior mesenteric vein/portal vein (SMV/PV) thrombosis after reconstruction remains unclear. This study aimed to describe the incidence and risk factors of SMV/PV thrombosis after vein reconstruction during pancreatectomy.
Methods
All patients who underwent portal vein resection (PVR) during pancreatectomy (2007–2019) were identified from a single institution prospective clinical database. Demographic and clinical data, operative and pathological findings, and postoperative outcomes were analyzed.
Results
Pancreatectomy with PVR was performed in 220 patients (mean age 65.1 years, male/female ratio 0.96). Thrombosis occurred in 36 (16.4%) patients after a median of 15.5 days [IQR 38.5, 1–786 days]. SMV/PV patency rates were 92.7% and 88.7% at 1 and 3 months, respectively. The rate of SMV/PV thrombosis varied according to SMV/PV reconstruction technique: 12.8% after venorrhaphy, 13.2% end-to-end anastomosis, 22.6% autologous vein, and 83.3% synthetic graft interposition (p < 0.0001). SMV/PV thrombosis was associated with increased 90-day mortality (16.7% vs 4.9%, p = 0.02) and overall 30-day complication rate (69.4% vs 42.9%, p = 0.006). Pancreatectomy type, neoadjuvant chemoradiation, pathologic tumor venous invasion, resection margin status, and manner of perioperative anticoagulation did not influence the incidence of PV thrombosis. SMV/PV thrombosis was associated with a nearly 5-times increased risk of postoperative sepsis after pancreatectomy.
Conclusion
Portal vein thrombosis developed in 16% of patients who underwent pancreatectomy with PVR at a median of 15 days. PVR with synthetic interposition graft carries the highest risk for thrombosis.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Due to the close anatomical relationship between the superior mesenteric vein/portal vein (SMV/PV) and the posterior neck of the pancreas, venous involvement by tumor or inflammation occurs frequently. SMV/PV involvement was historically considered a sign of advanced pancreatic cancer; however, surgeons, seeking to expand the number of patients who could benefit from pancreatectomy for cancer, introduced en bloc venous resection.1 An early pioneer in this work was Fortner who in 1984 described the concept of regional pancreatectomy with vascular resection in 35 patients.2 This procedure encountered high mortality (26%) and morbidity that nullified any potential survival benefit. Over the past three decades, SMV/PV resection during pancreatectomy has grown in frequency as improved surgical outcomes were observed after careful preoperative planning with the aid of enhanced radiographic imaging. As indications for venous resection during pancreatectomy were refined, observational studies validated the safety of SMV/PV resection.3,4,5,6,7
Positive margin status after pancreatectomy for pancreatic ductal adenocarcinoma is associated with poor outcomes, including up to 45% local recurrence rate and decreased overall survival.8,9 This understanding led to the expert consensus statement from Evans et al. in 2009 that promoted venous resection as a standard of care when necessary to achieve negative resection margins.10 The current indications for SMV/PV resection during pancreatectomy can be divided into two basic categories: planned and unplanned. SMV/PV resection is most often planned preoperatively in borderline resectable tumors (NCCN) based on multiphase contrast-enhanced cross-sectional imaging with either computed tomography or magnetic resonance imaging.11 In a minority of cases, the need for venous resection with reconstruction is determined intraoperatively as a result of direct venous injury or dense tissue adhesions that do not permit safe mesenteric vessel dissection. Venous resection may also be required in cases of benign pathology carrying significant inflammation such as chronic pancreatitis, pseudocysts, or biopsied pancreatic cysts.
Although SMV/PV resection and reconstruction has proven to be safe in experienced pancreatic surgery centers, vascular resection during pancreatomy is still associated with potentially severe complications.12,13,14
Patients may remain asymptomatic with post-pancreatectomy mesenteric vein thrombosis, but acute SMV/PV thrombosis can be associated with acute mesenteric congestion, venous mesenteric ischemia, portal hypertension, and liver dysfunction. Postoperative thrombosis of the SMV/PV after reconstruction has been described in up to 30% of patients; however, the risk of SMV/PV thrombosis after resection and reconstruction remains unclear.10,15,16 This study aimed to describe the incidence and risks of venous thrombosis after pancreatectomy.
Methods
Patient Selection
From 2007 to 2019, data from 2,700 consecutive patients who underwent pancreatectomy at a single academic institution were prospectively collected in a database. For the purpose of this study, the database was retrospectively reviewed, and patients who underwent SMV/PV resection during pancreatectomy for any indication were included. Patients with incomplete data for analysis were excluded from this study.
Parameters Assessed
The primary outcome of this study was the incidence of postoperative SMV/PV thrombosis after pancreatectomy. Thrombosis was diagnosed on any postoperative imaging study, including liver duplex ultrasound or contrast-enhanced computed tomography. All patients were evaluated in clinic for a postoperative visit at 1 month. Patients were then followed every 3 to 4 months with physical evaluation, laboratory testing (serum liver function and CA19-9) and surveillance contrast-enhanced abdominal CT imaging for the first 2 years by the surgical or medical oncology team. After the first two years of follow-up, surveillance was extended to a semi-annual basis and usually conducted by a medical oncology team outside of the academic institution. Positive radiographic findings, e.g., local and systemic tumor recurrence and late postoperative complications, were typically communicated to the primary surgeon and captured in the institution’s prospective pancreatomy outcome database.
A secondary outcome was the determination of risks factors associated with development of SMV/PV thrombosis. Individual patient demographic, clinical, laboratory, surgical, pathological, and postoperative outcomes data were gathered and used for analysis. Postoperative complications were recorded and graded according to the Clavien-Dindo classification.
Surgical Technique of Venous Resection and Reconstruction
All surgical procedures were performed with curative intent by a team of eight surgeons with significant pancreatic operative experience. Vascular reconstruction was performed by either primary pancreatic surgeons or organ transplant surgeons. For oncologic procedures, the NCCN guidelines in place at the time of surgery were used to define resectability status at diagnosis and for decision-making regarding potential venous resection. Determination of resectability of pancreatic cancer prior to the formal establishment of NCCN guidelines was made at the discretion of the operative surgeon. Five types of venous reconstruction were routinely performed: lateral venorrhaphy, venorrhaphy with patch repair, primary end-to-end anastomosis, and interposition grafting with either autologous vein or prosthetic graft. Whenever feasible, venorrhaphy with/without patch or primary end-to-end anastomosis was the favored reconstruction technique. When a tension-free primary repair or anastomosis could not be achieved despite maximal mobilization maneuvers, SMV/PV reconstruction was performed with an interposition graft, either autologous (internal jugular or splenic vein) or prosthetic (PTFE graft or cryopreserved vein, human cadaveric or bovine).
Immediately prior to resection, the vein was clamped proximally and distally, and systemic heparin at a dose of 70 units/kg was administered intravenously by the anesthesia team. The primary pancreatic surgeon performed almost all of the segmental resections of the portal vein or SMV with primary anastomosis. Vascular reconstructions involving multiple anastomoses or complex interposition grafting usually required assistance from a solid organ transplant surgeon.
When the splenic vein was ligated, an effort to reimplant it was made when technically feasible in order to avoid the development of postoperative hypersplenism or sinistral portal hypertension. When a long segment of splenic vein was resected or when the pancreas was transected beyond the neck, reimplantation was usually not attempted. Similarly, when the entire portosplenomesenteric confluence was involved with tumor, splenic vein reimplantation was not performed for oncological considerations.
Statistical Analysis
Data were compiled using Microsoft Excel 2016® (Redmond, WA). Descriptive statistics of continuous data included mean, standard error of mean, and range, whereas categorical variables were expressed as numbers and percentages. Subgroup comparisons of continuous and categorical data were performed with the Student’ t test and Fisher’s exact test, respectively. Independent factors associated with venous thrombosis were determined from uni- and multivariable analyses. Variables with p value < 0.1 in univariate analysis were entered into logistic regression. Statistical significance in multivariable analysis was considered at p < 0.05. All analyses were performed using IBM SPSS statistics version 25.0 (Armonk, NY: IBM Corp).
Results
Population
Among 2,700 patients who underwent pancreatic resection at a single academic center from 2007 to 2019, 220 (8%) patients underwent resection of the PV, SMV, or SMV/PV confluence. Median age of the study cohort was 66 years (SEM ± 11, range 27–88), with a sex ratio of 0.96 (108 men/112 women). Fifty-seven patients (25.9%) were smokers, and 54 (24.5%) were obese. Median follow-up was 257 days (± 720, range 31–3975). For the 220 patients with venous resection, the most common indication for pancreatectomy was malignancy in 92% (203/220), whereas the remaining 17 (8%) patients underwent pancreatic resection for benign pathology such as pancreatitis or cyst disease. Seventy patients (31.8%) received neoadjuvant chemotherapy, while 23 patients (10.5%) had preoperative radiation therapy. The population flow chart is presented in Fig. 1.
Surgical Outcomes
The most common operation performed was pancreatoduodenectomy (PD) in 181 (82%) patients (119 pylorus-preserving and 62 classic-type PD). Fourteen (7%) patients underwent distal pancreatectomy, and 25 patients (11%) required total pancreatectomy. Median operative time from anesthesia induction to extubation was 381 min (range, 168–1146 min). Median estimated blood loss was 800 mL (range, 100–2500 mL). Median occlusive clamp time for venous reconstruction was 21 min (range, 5–90 min).
Ninety-day mortality of the entire SMV/PV resection/reconstruction cohort was 6.8%, and any cause morbidity was reported in 47.3% of patients. Median length of hospital stay was 9 days (range, 2–74 days).
The length of hospital stays also increased with the complexity of venous reconstruction from a median of 8 days for venorrhaphy and primary end-to-end anastomosis to 10 days for autologous vein graft and 30.5 days for prosthetic graft (p < 0.0001). Patients with venous thrombosis experienced a longer hospital stay compared to patients without thrombosis, median 12 vs 8 days, p = 0.0009. Postoperative SMV/PV thrombosis was associated with an increased 90-day mortality (16.7% vs 4.9%, p = 0.02) and overall complication rate (69.4% vs 42.9%, p = 0.006).
Portal Vein Resection and Reconstruction
Four types of venous resection and reconstruction were used in 220 unique patients: venorrhaphy 39 (17.7%), primary end-to-end anastomosis 144 (65.4%), autologous interposition vein graft 31 (14.1%), and prosthetic interposition graft in 6 (2.7%). Lateral venorrhaphy was performed as a direct suture technique in all 39 patients. For patients requiring an interposition vein graft for reconstruction, internal jugular vein was used for 29 patients, splenic vein 2, bovine carotid graft 1, cadaveric vein graft 1, and polytetrafluoroethylene (PTFE) graft 4. Median occlusive venous clamp time required for reconstruction was significantly longer for interposition vein graft reconstruction compared to venorrhaphy or end-to-end anastomosis (31 ± 22 vs. 18 ± 12 min, p < 0.0001). The splenic vein was ligated at time of the anastomosis and not re-anastomosed in 86 patients (39%) due to technical challenges or intraoperative decision-making.
Post Venous Reconstruction Management
Sixty-two percent of patients received some form of postoperative anticoagulation. The remainder of patients received only intraoperative intravenous heparin or direct flushing of the SMV and PV with heparin at time of the vein anastomosis. Postoperative anticoagulation regimen following vein resection and reconstruction was not standardized and reflected the discretion of the primary operative surgeon. Variability of postoperative anticoagulation was observed: heparin or vitamin K antagonists (21.7%), antiplatelet therapy with aspirin (33%), or both (7.7%).
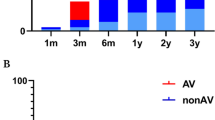
PV Thrombosis and Patency
Venous thrombosis occurred in 36 (16.4%) patients after a median of 15.5 days [IQR 38.5, 1–786]. Fourteen patients (6.4%) had thrombosis within the first 7 postoperative days. A significant difference in the rate of thrombosis according to venous reconstruction technique was observed. Five patients (12.8%) developed thrombosis after venorrhaphy, 13.2% after end-to-end anastomosis, 22.6% with autologous interposition vein graft, and 83.3% with synthetic graft, p < 0.0001. Overall patency rate of all PV/SMV resections and reconstructions was 92.7% and 88.7% at 1 and 3 months, respectively (Fig. 2). When patency rate was analyzed according to type of reconstruction, the use of interposition prosthetic graft carried the highest risk for thrombosis, as shown on the Kaplan Meier graph (Fig. 3).
Patients with early (within 7 days) vs. late (> 7 days) thrombosis were compared. Results are presented in Table 1. The two groups were comparable for all demographic and intraoperative variables. Clamping time was only available in a minority of patients but appeared to be significantly longer in the early thrombosis population. The postoperative anticoagulation regimen was different between the two groups, with a majority of early thrombosis patients being on heparin/Lovenox (n = 8/14), whereas patients with late thrombosis were more often not anticoagulated or on aspirin only (n = 16/22).
Seven of the 36 patients (19.4%) underwent a second operation for thrombus or consequences of it. The second operation was performed within a median of 1 day (± 1.11, range 1–4). One patient underwent a third operation for recurrent thrombosis. During reoperations, a thrombectomy and revision of the venous reconstruction was performed in 100%. In 2 cases, ischemic bowel was found. In the first case, the transverse colon was ischemic, and a partial colectomy with handsewn anastomosis was performed. In the second case, due to extensive small bowel necrosis, transition to comfort measures was decided by the family.
Predictors of Thrombosis
Patients with venous thrombosis were not significantly different from patients without thrombosis in terms of demographic data or preoperative comorbidities other than obesity (36% vs 22%) or preoperative biliary stenting (67% vs 45%), Table 2. No difference in the preoperative serum platelet count was observed between patients with or without thrombosis (244 k ± 105 vs 257 k ± 119 k, p = 0.54).
When pathology data were compared between these two groups, no difference in the malignancy rate (94.4% vs 91.8%, p = 1.0) or rate of negative R0 margin (70.7% vs 77.4%, p = 0.52) was observed. Tumor invasion of the vein on final pathology was present in 41.7% of patients who developed thrombosis versus 48.4% of patients who did not (p = 0.47). The univariable analyses regarding demographic and clinical data and perioperative and postoperative variables are presented in Table 2 and 3, respectively.
Multivariable analysis of patients with thrombosed versus patent venous reconstruction is summarized in Table 4. Pancreatectomy type, neoadjuvant chemotherapy, or chemoradiation did not influence the incidence of PV thrombosis. PV resection was not independently associated with postoperative pancreatic fistula or delayed gastric emptying. Patients with postoperative PV/SMV thrombosis experienced significantly higher rates of postoperative sepsis in multivariable regression analysis (25% vs 6%, p = 0.03) with a relative hazard ratio of 4.5 (95% CI 1.2–17.1).
Interestingly, no difference in the rate of SMV/PV thrombosis was found for patients who received postoperative anticoagulation with heparin or vitamin K antagonists or postoperative antiplatelet therapy with aspirin. Similarly, there was no difference in the rate of SMV/PV thrombosis based on splenic vein ligation or reimplantation (44% vs 38%, p = 0.64).
Discussion
The intimate anatomic relationship between the pancreas and the portomesenteric vascular axis often results in venous involvement by pancreatic inflammation or pancreatic neoplasms. The now outdated term of resectability has evolved over the past few decades as portomesenteric vascular invasion by tumor or infiltration by inflammation is no longer considered a contraindication to operative resection.10,11 Up to 30% of patients undergoing pancreatic resection for cancer require portal or superior mesenteric vein resection in order to accomplish complete tumor clearance. Portomesenteric venous resection achieves higher complete resection rates with negative margins without significantly increased mortality and morbidity.6,17,18,19
One of the most serious complications after pancreatectomy with portomesenteric vein resection is venous thrombosis. In this current single-institution series of 220 pancreatectomies with SMV/PV resection, 16% of patients developed postoperative venous thrombosis at a median time of 15 days regardless of the type of anticoagulation or antiplatelet regimen. Vein reconstruction with interposition grafting carried the highest risk for thrombosis. Venous thrombosis may be attributable to technical factors related to the reconstruction or other pre-disposing factors such as intra-abdominal sepsis that was found to be highly associated with SMV/PV thrombosis. The increased 90-day mortality associated with venous thrombosis, 16.7% compared to 4.9% in patients without thrombosis (p = 0.02), may result from severe complications associated with acute SMV/PV thrombosis including bleeding or ascites production from sudden onset portal hypertension, intestinal venous ischemia, or anastomotic breakdown.20 Acute portal vein thrombosis after pancreatectomy is not necessarily a devastating complication by itself and can be an incidental finding during contrast-enhanced cross-sectional imaging in asymptomatic patients. Delayed presentation of portal vein thrombosis more than 6 months after pancreatectomy for pancreatic cancer often reflects locoregional tumor recurrence.21,22,23
Rates of thrombosis following pancreatoduodenectomy with portal vein resection, reported in several retrospective series with variable length of follow-up, range from 11 to 25%.19,20,23,24,25,26,27 In the present study, venous thrombosis after resection and reconstruction was 16% and similar to previously reported studies.21 Reconstruction with prosthetic interposition grafting carried the highest risk for thrombosis (13.9%) in this study. Past studies attempted to analyze the role of the type of venous reconstruction with regard to thrombosis and established an association between prosthetic PTFE graft reconstruction of the SMV/PV with poor outcomes.16 A systematic review by Chandrasegaram et al. suggested that prosthetic graft use during vein reconstruction was a risk factor for thrombosis even though statistical significance was not demonstrated due to a small number of patients.28 Other studies, however, have shown that PTFE graft use for vein reconstruction is associated with a vein patency rate of 64% at 1 year.25,29 Chu et al. also showed that early portal vein thrombosis was more common in patients who had a prosthetic PTFE graft reconstruction.25 The selection of interposition graft reconstruction should be weighed against the increased risk of thrombosis associated with prosthetic material. In most cases, an end-to-end venous anastomosis can be achieved without tension after appropriate mobilization of the root of the mesentery and liver ligaments even when the length of the resected vein is over 5 cm.30 Venous thrombosis was associated with a nearly 5 times increased risk of postoperative sepsis that raises a question of causality. Infection is a well-described independent risk factor for thrombosis. Intra-abdominal sepsis creates a hypercoagulable state that may potentiate mesenteric vein thrombosis similar to the phenomenon that is observed in patients with infected pancreatic necrosis.31 Intra-abdominal sepsis due to organ-space infection may cause a direct compressive effect on the portomesenteric venous circulation leading to thrombosis. Conversely, primary SMV/PV thrombosis can lead to mesenteric venous stasis with possible ischemia and the risk of bacterial translocation.
Due to the retrospective design of this study, portomesenteric vein thrombosis could represent either the cause or effect of sepsis. However, while sepsis developed in 25% of patients who experienced SMV/PV thrombosis after vein resection and reconstruction, only 14% of the thrombosis cohort had a postoperative pancreatic fistula.
Several studies have analyzed the optimal postoperative anticoagulation regimen following venous resection and reconstruction.13,23,28,29,30,32 However, we did not find any difference in the incidence of thrombosis associated with the type of postoperative anticoagulation or antiplatelet regimen. While all patients in this study received full systemic heparinization prior to vein clamping at the time of resection, prophylactic regimens varied according to individual surgeon preference in the postoperative period. Once SMV/PV thrombosis was diagnosed, patients were all treated with therapeutic unfractionated or low molecular weight fractionated heparin as a bridge to a vitamin K antagonist. A recent meta-analysis incorporating 13 studies (N = 361 patients) with both benign and malignant pancreatic pathologies found no differences in morbidity, mortality, or incidence of early portal vein thrombosis after pancreatectomy with venous resection and reconstruction regardless of the postoperative anticoagulation and/or antiplatelet regimen (aspirin, clopidogrel, heparin, vitamin K antagonist).28
Even though this single center study is the largest retrospective review of a prospective pancreatectomy outcomes database to examine the incidence and risk factors for portomesenteric thrombosis after pancreatectomy with vein resection and reconstruction, we recognize several limitations. A single-institution surgical series spanning over 12 years includes outcomes reflecting practice changes with regards to pre-, peri-, and postoperative management. Although the use of neoadjuvant chemotherapy and chemoradiation increased during the study period, especially for patients with borderline resectable or locally advanced pancreatic cancer, we did not observe an association with postoperative SMV/PV thrombosis after PVR. The type of vein reconstruction and indication for each technique, including intraoperative decision-making with regard to splenic vein reimplantation, reflected individual surgeon preference in this study as did the choices of prophylactic anticoagulation in the postoperative setting. Routine portal venous duplex or contrast-enhanced cross-sectional imaging was not performed routinely in all patients; thus, the incidence of early SMV/PV thrombosis is not captured for asymptomatic patients without clinically apparent complications.
In conclusion, this current series suggests that portal vein thrombosis after portal vein resection during pancreatectomy is a common complication (16%) and is associated with a complicated postoperative course and increased mortality. Primary venous reconstruction with either direct venorrhaphy or tension-free end-to-end anastomosis should be attempted as a first choice as the use of an interposition graft, especially synthetic, carries significant risk for venous thrombosis.
References
Harrison LE, Klimstra DS, Brennan MF. Isolated portal vein involvement in pancreatic adenocarcinoma. A contraindication for resection? Ann Surg. 1996;224(3):342-9.
Fortner JG. Regional resection of cancer of the pancreas: a new surgical approach. Surgery 1973; 73:307–20.
Ishikawa O, Ohigashi H, Imaoka S, et al. Preoperative indications for extended pancreatectomy for locally advanced pancreas cancer involving the portal vein. Ann Surg 1992; 215:231–6.
Roch AM, House MG, Cioffi J, Ceppa EP, Zyromski NJ, Nakeeb A, Schmidt CM. Significance of Portal Vein Invasion and Extent of Invasion in Patients Undergoing Pancreatoduodenectomy for Pancreatic Adenocarcinoma. J Gastrointest Surg. 2016 Mar;20(3):479-87.
Zhou Y, Zhang Z, Liu Y, Li B, Xu D. Pancreatectomy combined with superior mesenteric vein-portal vein resection for pancreatic cancer: a meta-analysis. World J Surg 2012; 36:884–91.
Tseng JF, Raut CP, Lee JE, et al. Pancreaticoduodenectomy with vascular resection: margin status and survival duration. J Gastrointest Surg 2004;8(8):935-49.
Fuhrman GM, Leach SD, Staley CA, Cusack JC, Charnsangavej C, Cleary KR, El-Naggar AK, Fenoglio CJ, Lee JE, Evans DB. Rationale for en bloc vein resection in the treatment of pancreatic adenocarcinoma adherent to the superior mesenteric-portal vein confluence. Pancreatic Tumor Study Group. Ann Surg 1996 Feb;223(2):154-62.
Yeo CJ, Cameron JL, Lillemoe KD, Sitzmann JV, Hruban RH, Goodman SN et al Pancreaticoduodenectomy for cancer of the head of the pancreas. 201 patients. Ann Surg 1995; 221: 721–33.
Ghaneh P, Kleeff J, Halloran CM et al. European Study Group for Pancreatic Cancer. The Impact of Positive Resection Margins on Survival and Recurrence Following Resection and Adjuvant Chemotherapy for Pancreatic Ductal Adenocarcinoma. Ann Surg 2019 Mar;269(3):520-9.
Evans DB, Farnell MB, Lillemoe KD, Vollmer C Jr, Strasberg SM, Schulick RD. Surgical treatment of resectable and borderline resectable pancreas cancer: expert consensus statement. Ann Surg Oncol 2009; 16:1736-44.
Tempero MA, Malafa MP, Chiorean EG, Czito B, Scaife C, Narang AK, Fountzilas C, Wolpin BM, Al-Hawary M, Asbun H, Behrman SW, Benson AB, Binder E, Cardin DB, Cha C, Chung V, Dillhoff M, Dotan E, Ferrone CR, Fisher G, Hardacre J, Hawkins WG, Ko AH, LoConte N, Lowy AM, Moravek C, Nakakura EK, O'Reilly EM, Obando J, Reddy S, Thayer S, Wolff RA, Burns JL, Zuccarino-Catania G. Pancreatic Adenocarcinoma, Version 1.2019. J Natl Compr Canc Netw. 2019 Mar 1;17(3):202-10.
Howard TJ, Villanustre N, Moore SA, DeWitt J, LeBlanc J, Maglinte D et al. Efficacy of venous reconstruction in patients with adenocarcinoma of the pancreatic head. J Gastrointest Surg 2003; 7: 1089–1095.
Siriwardana H. P. P. and Siriwardena A. K. Systematic review of outcome of synchronous portal–superior mesenteric vein resection during pancreatectomy for cancer. Br J Surg 2006; 93: 662–73.
Guilbaud T, Turrini O, Lemoine C, Le Treut YP, Ouaissi M, Moutardier V, Delpero JR. Venous Resection in Pancreatic Ductal Adenocarcinoma: Impact of Surgical Experience on Early Postoperative Courses. Anticancer Research Aug 2017;37 (8):4205-13
Gao W, Dai X, Dai C et al. Comparison of patency rates and clinical impact of different reconstruction methods following portal/superior mesenteric vein resection during pancreatectomy. Pancreatology 2016;16(6):1113–23.
Dua MM, Tran TB, Klausner J et al. Pancreatectomy with vein reconstruction: technique matters. HPB 2015;17(9):824–31.
Riediger H, Makowiec F, Fischer E, Adam U, Hopt UT. Postoperative morbidity and long-term survival after pancreaticoduodenectomy with superior mesenterico-portal vein resection. J Gastrointest Surg 2006; 10:1106-15.
Capussotti L, Massucco P, Ribero D, Viganò L, Muratore A, Calgaro M. Extended lymphadenectomy and vein resection for pancreatic head cancer: outcomes and implications for therapy. Arch Surg 2003; 138:1316-22.
Leach SD, Lee JE, Charnsangavej C, Cleary KR, Lowy AM, Fenoglio CJ, et al. Survival following pancreaticoduodenectomy with resection of the superior mesenteric-portal vein confluence for adenocarcinoma of the pancreatic head. Br J Surg 1998; 85:611-7.
Kang MJ, Jang JY, Chang YR, Jung W, Kim SW. Portal vein patency after pancreatoduodenectomy for periampullary cancer. Br J Surg 2015; 102:77-84.
Glebova NO, Hicks CW, Piazza KM, Abularrage CJ, Cameron AM, Schulick RD, Wolfgang CL, Black JH III. Technical risk factors for portal vein reconstruction thrombosis in pancreatic resection. J Vasc Surg. 2015 Aug; 62(2):424-33.
Delpero JR, Sauvanet A. Vascular Resection for Pancreatic Cancer: 2019 French Recommendations Based on a Literature Review From 2008 to 6-2019. Front Oncol. 2020; 10:40.
Ouaissi M, Sielezneff I, Pirro N, et al. Therapeutic anticoagulant does not modify thromboses rate vein after venous reconstruction following pancreaticoduodenectomy. Gastroenterol Res Pract. 2008;896320.
Smoot RL, Christein JD, Farnell MB. Durability of portal venous reconstruction following resection during pancreaticoduodenectomy. J Gastrointest Surg 2006; 10:1371–5.
Stauffer JA, Dougherty MK, Kim GP, Nguyen JH. Interposition graft with polytetrafluoroethylene for mesenteric and portal vein reconstruction after pancreaticoduodenectomy. Br J Surg 2009; 96:247–52.
Chu CK, Farnell MB, Nguyen JH, et al. Prosthetic graft reconstruction after portal vein resection in pancreaticoduodenectomy: a multicenter analysis. J Am Coll Surg. 2010; 211:316–24.
Sgroi MD, Narayan RR, Lane JS, et al. Vascular reconstruction plays an important role in the treatment of pancreatic adenocarcinoma. J Vasc Surg 2015; 61:475–80.
Chandrasegaram MD, Eslick GD, Lee W, Brooke-Smith ME, Padbury R, Worthley CS et al. Anticoagulation policy after venous resection with a pancreatectomy: a systematic review. HPB 2014; 16:691–8.
Smoot RL, Christein JD, Farnell MB. An innovative option for venous reconstruction after pancreaticoduodenectomy: the left renal vein. J Gastrointest Surg 2007; 11:425-31.
Wang F, Arianayagam R, Gill A, Puttaswamy V, Neale M, Gananadha S et al. Grafts for mesenterico-portal vein resections can be avoided during pancreaticoduodenectomy. J Am Coll Surg 2012; 215:569–79.
Roch AM, Maatman TK, Carr RA, Colgate CL, Ceppa EP, House MG, Lopes J, Nakeeb A, Schmidt CM, Zyromski NJ. Venous Thromboembolism in Necrotizing Pancreatitis: An Underappreciated Risk. J Gastrointest Surg. 2019 Dec;23(12):2430-8.
Clark W, Silva M, Donn N, Luberice K, Humphries LA, Paul H, et al. Targeting early deaths following pancreaticoduodenectomy to improve survival. J Gastrointest Surg 2012; 16:1869–74.
Author information
Authors and Affiliations
Contributions
Conception or design of the work: Roch, Kilbane, House.
Acquisition of data: Roch, Kilbane, House.
Analysis of data: Roch, House.
Interpretation of data: Roch, House, Ceppa, Nakeeb, Nguyen, Schmidt, Zyromski.
Drafting or revising of the work for important intellectual content: Roch, Ceppa, House, Nakeeb, Nguyen, Schmidt, Zyromski.
Corresponding author
Ethics declarations
Ethics Approval
Permission to conduct this retrospective study was obtained from the Indiana University Institutional Review Board Ethics Committee.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roch, A.M., Kilbane, E.M., Nguyen, T. et al. Portal Vein Thrombosis After Venous Reconstruction During Pancreatectomy: Timing and Risks. J Gastrointest Surg 26, 2148–2157 (2022). https://doi.org/10.1007/s11605-022-05401-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05401-1