Abstract
Introduction
Pancreatic cancer is considered a systemic disease at presentation. Therefore, multimodality therapy with surgical resection and chemotherapy is the standard of care for locoregional disease. We described treatment patterns and time trends with regard to age and treatment center in the receipt of multimodality therapy.
Methods
We used the National Cancer Data Base to identify patients ≥18 years old with stage I and II pancreatic adenocarcinoma. Treatment was defined as no treatment, resection only, chemotherapy only, or multimodality therapy, which consisted of both chemotherapy (neoadjuvant or adjuvant) and resection. Trends in the receipt and type of treatment were compared.
Results
Of 39,441 patients, 22.8 % of patients received no treatment, 18.5 % received chemotherapy only, 23.0 % underwent surgical resection alone, and 35.8 % of patients received multimodality therapy. Receipt of multimodality therapy increased from 31.3 % in 2004 to 37.9 % in 2011 (p < 0.0001). Patients >55 years were less likely to receive multimodality therapy (56–64 years: OR 0.83, 95 % CI 0.78–0.89; 65–75: OR 0.60, 95 % CI 0.55–0.65; ≥76: OR 0.17, 95 % CI 0.16–0.19 compared to patients 18–55). Compared to community hospitals, patients treated at an NCI-designated center were more likely to receive multimodality therapy (OR 1.62, 95 % CI 1.46–1.81) and, if they received multimodality therapy, delivery of chemotherapy in the neoadjuvant compared to adjuvant setting (OR 2.82, 95 % CI 2.00–3.98).
Conclusion
Despite increased use of multimodality therapy, it remains underutilized in all patients and especially in older patients. Receipt of multimodality therapy and neoadjuvant therapy is highly dependent on treatment at NCI-designated cancer centers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer remains an aggressive malignancy, with an overall 5-year survival rate of <4 %.1 Surgical resection remains the only potentially curative option, but even with R0 resection, 5-year survival rates range from 15 to 25 % and most patients recur with distant metastatic disease.2 – 4 As such, pancreatic cancer is considered a systemic disease at diagnosis, and chemotherapy, combined with surgical resection, is recommended for all early stage cancers. Since the initial report of the benefit of adjuvant chemotherapy and radiation from the Gastrointestinal Tumor Study Group (GITSG) in 1985,5 multiple studies have demonstrated the benefit of chemotherapy in the adjuvant setting.6 – 8 Single-institution studies over the last decade have demonstrated similar or greater benefit with chemotherapy with or without radiation delivered in the neoadjuvant setting.9 – 12
Despite the benefit of multimodality therapy, previous studies show that only 25–35 % of patients with locoregional pancreatic cancer undergo resection.13 – 15 In addition, significant treatment disparities exist; resection is performed less often in older patients and African-Americans, independent of tumor stage and comorbidities.13 , 15 , 16 In the subset of patients who undergo surgical resection, adjuvant therapy is also underutilized. Forty-four to 69 % of patients in single-institutional10 , 17 – 20 and 48 to 51 % in population-based studies21 , 22 received adjuvant therapy after surgical resection. In studies evaluating completion of neoadjuvant therapy given with curative intent, only 46–53 %9 , 10 of patients receiving initial chemotherapy ultimately proceeded to surgical resection. Despite the potential benefits of neoadjuvant therapy, population-based studies report that approximately 90 % of older patients receiving multimodality therapy received chemotherapy in the adjuvant setting, and 97 % of older patients who initially underwent chemotherapy never had a subsequent operation.21 , 22
Previous population-based studies evaluating receipt of multimodality therapy are limited to older patients or span a time period when the use of neoadjuvant therapy was uncommon.21 , 22 The objective of this study was to describe variations in patterns and time trends of receipt of multimodality therapy by age, treatment facility category, and utilization of neoadjuvant chemotherapy using a more contemporary cohort (2004–2011) of patients diagnosed with localized pancreatic cancer in the National Cancer Database (NCDB).
Methods
Data Source
The National Cancer Database (NCDB) is a national oncology outcomes database jointly sponsored by the American College of Surgeons and the American Cancer society.23 The data represent approximately 70 % of newly diagnosed cancer cases nationwide and consist of over 30 million medical records. Reportedly the largest clinical registry worldwide, the data are collected from hospital registries in more than 1500 Commission on Cancer accredited facilities.
Cohort Selection
We included patients older than 18 years of age diagnosed with a single primary or first primary pancreatic adenocarcinoma between 2004 and 2011. Pancreatic adenocarcinomas were identified using the third edition of the International Classification of Diseases for Oncology (ICD-O-3) primary site ICD-O-3 codes: C250-C259 and histology ICD-O-3 codes: 8000/3, 8010/3, 8020/3, 8021/3, 8022/3, 8050/3, 8140/3, 8141/3, 8211/3, 8230/3, 8500/3, 8521/3, 8260/3, 8262/3, 8441/3, 8450/3, 8453/3, 8470/3, 8471/3, 8472/3, 8473/3, 8480/3, 8481/3, 8503/3. American Joint Committee on Cancer (AJCC) stage was identified in each patient. For those that did not have pathological AJCC stage evaluated (unresected patients), clinical AJCC stage was used. Our final cohort included only patients with stage I and stage II cancers. We excluded patients who received hospice care (N = 4326) or were missing data on gender (N = 19), node status (N = 32), treatment status (N = 899), US region (N = 138), and other critical data (N = 1110). Our analysis included patients who were documented as having refused treatment or died before treatment as reported in the NCDB; however, following sensitivity analysis with exclusion of these patients it did not change our analysis and therefore was not reported in the results (N for no surgery = 804; N for no chemotherapy = 1733).
We did not stratify our analysis by tumor stage given inherent bias in the way data are collected. Once undergoing resection, patients can potentially be pathologically “upstaged” from stage I to stage II disease based on the presence of nodal metastases or extent of tumor on final pathology.
Covariates
Patient baseline demographic and clinical characteristics included age, race/ethnicity, income, education, region of treatment and type of facility providing treatment, form of insurance, stage, grade, year of diagnosis, and nodal status. Charlson comorbidity index was used to measure patient comorbidity. Driving distance was calculated based on centroid of patient’s zip code at diagnosis and street address of reporting facility.
Outcome Variable: Initial Treatment Modality
We defined the following treatment groups: (1) untreated (did not receive chemotherapy or surgical resection), (2) chemotherapy without surgery, (3) surgery without chemotherapy, and (4) multimodality therapy. The multimodality therapy group was further subdivided into neoadjuvant therapy (chemotherapy before resection) or adjuvant (resection before chemotherapy) therapy. Receipt of radiation was also identified (yes/no), but not used to classify treatment. Surgical resection was identified by “surgical procedure of the primary site” for resection of the primary tumor (Facility Oncology Registry Data Standards [FORDS] codes 25-80). Neoadjuvant therapy was defined as receipt of chemotherapy in the 6 months prior to surgical resection, and adjuvant chemotherapy was defined as the receipt of chemotherapy within 6 months after resection. Six months was chosen as a treatment cutoff for adjuvant therapy to exclude patients who may have received salvage or palliative chemotherapy for recurrence. Ninety-day mortality was calculated from date of diagnosis for patients who received surgery first, chemotherapy first, and no treatment at all.
Patients were only classified as having neoadjuvant therapy if they received both chemotherapy and surgical resection. If patients received chemotherapy alone, they could not be classified as having neoadjuvant therapy as we cannot determine intent of treatment in the NCDB. The same applies for patients classified as receiving adjuvant therapy; only patients who received both surgical resection followed by chemotherapy were categorized into the adjuvant treatment group.
Statistical Analysis
Statistical analysis was performed using SAS version 9.3 (SAS institute, Cary, North Carolina). Summary statistics were calculated for the overall cohort. Covariates were compared across treatment groups, and trends in the receipt of any therapy and multimodality therapy were compared across age groups. We used chi-square tests to test significance for categorical variables and Cochran-Armitage test for trend to assess changes over time. Statistical significance was considered when 2-side p value was <0.05.
Multivariable Analysis
A multivariable logistic regression model evaluating factors associated with receipt of multimodality therapy was performed for the entire cohort. Variables included age, sex, race/ethnicity, year of diagnosis, US region, facility type, insurance, income, education, and driving distance. Stage, nodal status, and grade were excluded from the model as resected patients were staged pathologically and unresected patients were staged clinically, introducing potential bias.
For patients who received multimodality therapy, an additional multivariable logistic regression model was created to determine factors associated with receipt of chemotherapy in the neoadjuvant setting. This model included the aforementioned variables.
Survival Analysis
Unadjusted Kaplan-Meier estimates of overall survival were obtained for patients based on treatment group (no treatment, chemotherapy only, surgery only, or multimodality therapy). We also compared unadjusted survival in patients who completed multimodality therapy in the neoadjuvant versus adjuvant setting. To adjust for immortal-time bias, a sensitivity analysis was done where patients were excluded if they did not survive 30 days following diagnosis. This minimally changed the results in each treatment group. As such, we only present the raw group (i.e., N = 12,561 for adjuvant therapy versus N = 12,406 following sensitivity analysis).
Results
Patient Demographics, Tumor Characteristics, and Treatment
We identified 39,441 patients with stage I and stage II pancreatic adenocarcinoma. Summary statistics for the overall cohort and by treatment group are shown in Table 1. The mean age of the cohort was 68.1 ± 11.6 years with 59.0 % of patients >65 years of age. Majority of patients (73.6 %) were white, 51.2 % were female, and 10.5 % of patients had more than one comorbidity. The fewest patients were treated a community hospital (6.1 %); 19.7 % were treated at a NCI designated cancer center, 30.6 % at a teaching/research center, and 34.0 % at a comprehensive community cancer center.
In the overall cohort, 8996 (22.8 %) patients received no treatment, 7277 (18.5 %) received chemotherapy only, 9072 (23.0 %) underwent surgical resection alone, and 14,096 (35.8 %) patients received multimodality therapy (Table 1, Fig. 1). In the entire cohort, clear contraindications and/or refusal of surgical resection were only coded in 5 % of the entire cohort. Of the 8812 patients who underwent chemotherapy as the initial treatment modality, only 1535 (17.4 %) patients subsequently underwent surgical resection. In contrast, 58.1 % (N = 12,561) of the 21,633 patients who initially underwent resection subsequently received chemotherapy. Ninety-day mortality was 1.4 % in patients undergoing chemotherapy as the initial treatment modality, 6.5 % in patients undergoing surgery as the initial treatment modality, and 1.4 % in untreated patients (Table 2). Of the 14,096 patients treated with multimodality therapy, 10.9 % of patients received it in the neoadjuvant setting and 89.1 % in the adjuvant setting (Fig. 1). Forty-four percent (44.6 %) of patients receiving some chemotherapy and/or surgery had concurrent radiation; 60.7 % of patients who received adjuvant therapy (N = 7,623) and 76.7 % of patients who received neoadjuvant therapy (N = 1,117) had concurrent radiation.
Treatment patterns in all patients with stage I and II pancreatic cancer. Total cohort of 39,441 patients; 8996 (22.8 %) patients received no treatment, 7277 (18.5 %) received chemotherapy only, 9072 (23.0 %) underwent surgical resection alone, and 14,096 (35.8 %) patients received multimodality therapy. Of patients these patients, 1535 subsequently underwent surgical resection; 12,561 underwent surgical resection first, followed by adjuvant chemotherapy
Unadjusted Factors: Trends in Treatment
From 2004 to 2011, the percentage of untreated patients decreased from 26.2 to 22.0 %, chemotherapy alone increased from 16.2 to 20.2 %, and surgery alone decreased from 26.2 to 19.8 %, and use of multimodality therapy increased from 31.3 to 37.9 % of patients (Table 1 and Fig. 2a; p for trend <0.0001). In patients who received multimodality therapy, delivery in the neoadjuvant setting increased from 4.5 to 16.7 % with reciprocal decrease of delivery in the adjuvant setting (Fig. 2b, p for trend <0.0001).
a Trends in all modalities of treatment over time in all patients diagnosed with pancreatic adenocarcinoma from 2004 to 2011. The percentage of untreated patients decreased from 26.2 to 22 %, chemotherapy alone went from 16.2 to 20.2 %, surgery alone decreased from 26.2 to 19.8 %, and utilization of multimodality therapy increased from 31.3 to 37.9 % of patients. b Trends in utilization of neoadjuvant therapy over time in all patients from 2004 to 2011. The receipt of neoadjuvant therapy increased from 4.5 to 16.6 % and use of adjuvant therapy decreased over the time period from 95.5 to 87.5 %. c Management of patients with locoregional pancreatic cancer varied by age group. Patients older than 76 years of age were most likely to go untreated with 45.2 % receiving no treatment versus only 9.4 % of patients between ages 18 to 55. Receipt of multimodality treatment was only 15.3 % in patients older than 76 years of age compared to 51 % of patients between the years of 18 to 55
There was significant disparity in the receipt of treatment by age group. Patients older than 76 years of age were most likely to go untreated with 45.2 % receiving no treatment compared to only 9.4 % of patients between ages 18 to 55 years. While rates of surgical resection or chemotherapy alone were similar across age groups, older patients were much less likely to receive multimodality therapy, decreasing from 51.0 % of patients 18–55 years to only 15.3 % of patients 76 years and older (Fig. 2c). For patients receiving multimodality therapy, 11.3 % of patients aged 18–55 years and 9.2 % of patients aged 76 years and older received it in the neoadjuvant setting (p = 0.03). The 90-day mortality increased with increasing age (Table 2). In patients receiving surgery as the initial treatment modality, the 90-day mortality increased from 2.11 % in patients 18–55 years to 10.19 % in patients 76 and older (p < 0.0001). The mean length of stay did also increase slightly with increasing age (18–55: 11.4 ± 15.1 days; 56–65: 11.9 ± 13.2 days; 66–75: 12.2 ± 11.6 days; 76+: 13.1 ± 12.3 days). In the patients who underwent surgery as the initial treatment modality and survived 90-days (N = 20,386), rates of adjuvant therapy were 70.0, 68.6, 61.0, and 42.7 % across age groups (p < 0.0001).
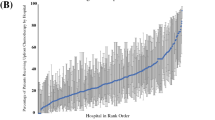
Patients treated at NCI designated cancer centers were less likely to go untreated and more likely to receive multimodality therapy (Table 1). In the 8812 patients who received chemotherapy as the initial treatment modality, the rate of subsequent surgical resection was 30.6 % at NCI designated cancer centers compared to 19.6 % at teaching centers, 15.9 % at other facilities, 10.9 % at comprehensive community cancer centers, and 5.9 % at community cancer programs. In patients who received multimodality therapy, 5.6 % of patients received neoadjuvant chemotherapy at a community cancer center, 8 % at a comprehensive community cancer center, 10.6 % at a teaching center, and 16.8 % at a NCI-designated center.
Multivariable Model: Factors Associated with Multimodality Therapy
In the adjusted model, increasing age remained strongly associated with a decrease in the receipt of multimodality therapy (Table 3). Consistent with the observed time trends in Fig. 2a, the odds of receiving multimodality therapy increased over time (Table 3), with a 40 % increased odds in 2011 compared to 2004 (OR 1.40, 95 % CI 1.28–1.54). The odds of receiving multimodality therapy decreased with increased age. Patients ≥76 years were less likely to receive multimodality therapy compared to patients 18–55 years (OR 0.17, 95 % CI 0.16–0.19) and Hispanics (OR 0.79 95 % CI 0.70–0.88) were significantly less likely to receive multimodality therapy compared to whites. Treatment at an NCI-designated center was associated with increased use of multimodality therapy compared to a community cancer program (OR 1.62 95 % CI 1.46–1.81; p < 0.0001).
In patients receiving multimodality therapy, neoadjuvant therapy was strongly associated with later year of diagnosis, NCI cancer center designation, and non-Medicare insurance. Factors such as age, fewer comorbidities, and higher education were not associated receipt of chemotherapy in the neoadjuvant vs. adjuvant setting (Table 3).
Survival
The overall 2-year survival based on treatment modality is demonstrated in Fig. 3a. Patients had improved survival if they received multimodality therapy. The 2-year survival was 7.7 % for untreated patients (median = 3.84 months), 12.3 % for chemotherapy alone (median = 10.26 months), 35.7 % for patients receiving surgery alone (median = 15.16 months), and 46.9 % for multimodality therapy (median = 22.36 months) (p < 0.0001). When comparing neoadjuvant and adjuvant therapy in all patients who received multimodality therapy, 2-year survival was higher for patients receiving neoadjuvant therapy (49.6 versus 46.5 %; median 23.9 vs 22.2 months; p = 0.01, Fig. 3b). When comparing survival rates and neoadjuvant versus adjuvant therapy in older patients, there was no difference (48.1 vs. 44.4 %. median 23.2 vs 20.9 months; p = 0.11).
a Overall 2-year survival probability for localized pancreatic cancer by treatment type (NCDB: 2004–2011). Multimodality therapy provided the greatest 2-year survival benefit of 46.9 % followed by 35.7 % with surgical resection, compared to only 12.3 % for chemotherapy alone and 7.7 % for untreated patients (p < 0.0001). b Overall 2-year survival probability in patients receiving adjuvant or neoadjuvant chemotherapy of localized pancreatic cancer (NCDB: 2004-2011). Neoadjuvant chemotherapy demonstrates a 2-year survival rate of 49.6 % versus 46.5 % in adjuvant therapy. This was statistically significant (p = 0.01)
Discussion
Our contemporary study using the NCDB demonstrates that the use of multimodality therapy for locoregional pancreatic cancer has increased over time. However, many patients still do not receive multimodality therapy, despite evidence for improved survival with its use.22 , 24 , 25 Although an increasing number of studies report on both use and effectiveness of neoadjuvant therapy from specialized centers, the use of neoadjuvant therapy in the setting of clearly resectable disease remains a topic of debate. Adjuvant chemotherapy is still given in nearly 90 % of patients who received multimodality therapy in the general population. Finally, we observed that older patients and patients treated at non-NCI designated centers were less likely to undergo multimodality therapy.
An early population-based study using the NCDB found that from 1985 to 1995, 49.6 % of patients with stage I and II cancers had not undergone any form of treatment.26 A later study also using the NCDB (1985 to 2003) found the proportion of untreated patients with stage I and II disease had decreased to less than 25 %.27 Our more recent cohort shows little additional improvement, and 23 % of our cohort remained untreated (22 % in 2011). However, there has been an increase in the use of surgical resection for locoregional disease. Bilimoria et al.27 reported an increase in surgical resection from 37.2 % of patients undergoing resection in 1985 up to 49.7 % in 2003; our study shows a continued increase of 58 % of patients undergoing resection between 2004-2011.
Utilization of multimodality therapy varies. Our previously published study reported only 11.1 % of Medicare beneficiaries received multimodality therapy between the years of 2002 to 2007.21 Conversely, Tzeng and colleagues found that 75.2 % of patients who underwent resection received some form of multimodality therapy; however, this was from a single-institution NCI-designated center that included patients undergoing treatment with curative intent.10 Our study shows an increase in use of multimodality therapy on the population level from 31.3 % in 2004 to 37.9 % in 2011 as our study included patients of all ages and all types of treatment facilities.
Many previous studies evaluated the use of multimodality therapy, but solely in the adjuvant setting.26 , 27 Population-based studies utilizing SEER-Medicare (Surveillance, Epidemiology, End Results Program) reported only 48 % of Medicare beneficiaries received adjuvant treatment (radiation, chemoradiation, or chemotherapy) through 2002,22 , 24 with a slight increase to 51 % in a study through 2007.21 A study by Kooby and colleagues6 using the National Cancer Database between the years from 1998 to 2002 reported an adjuvant therapy rate of 45 % after surgical resection (either chemotherapy alone or chemoradiation). A study using the Oregon State Cancer Registry identified 228 patients of all ages who underwent pancreatic resection between 1996 and 2003; 54 % of these patients received adjuvant therapy.7 Compared to studies from these earlier time periods, our study demonstrates a slight increase in use over time, as 58 % of resected patients received adjuvant therapy. While our study demonstrates an increase in adjuvant therapy in resected patients of all ages, only 50 % of resected patients 66 and older underwent adjuvant therapy, with essentially no change from the 2007 SEER data reported above.21 Given that elderly patients are still less likely to receive adjuvant treatment, concerns for completing adjuvant therapy in this more vulnerable population may be well founded.
In studies from specialized centers, while treatment with neoadjuvant therapy has increased in patients with resectable disease, superiority to adjuvant therapy in improving overall survival has not been proven and its use remains controversial.9 , 25 , 28 Reportedly, patients are more likely to complete multimodality therapy, as complications related to surgical resection often delay or prohibit the use of adjuvant therapy.29 However, this has not been proven and our data show that at the population level, when multimodality therapy is given, it is given in the neoadjuvant setting in 10.8 % of cases, with little change from previous studies. Parmar et al. reported that only 5.6 % of Medicare beneficiaries receiving multimodality therapy received it in the neoadjuvant setting.21 A California population-based study including 458 resected patients of all ages reported only 8.5 % of patients who received multimodality therapy received it in the neoadjuvant setting.30
We did, however, observe an increase in the use of neoadjuvant therapy over time, with 16.7 % of patients who underwent some form of multimodality therapy received therapy in the neoadjuvant setting in 2011. This increase is likely to due to the contemporary time period and the larger sample of younger patients.
Of the 8812 patients who underwent chemotherapy as the initial treatment modality, only 17 % went on to surgical resection.9 , 10 Again, in our study, patients classified as having neoadjuvant therapy received both surgical resection and chemotherapy; those who received chemotherapy alone were not classified as neoadjuvant as we do not know the intent of their treatment. Based on the literature and knowledge of practice patterns, it seems that neoadjuvant therapy is the preferred modality in a handful of specialized centers. Patients treated at NCI-designated cancer centers were more likely to be treated, more like to receive multimodality therapy, and more likely to receive it in the neoadjuvant setting. The higher rates of surgery after chemotherapy in NCI designated centers suggest that in this setting, it is more often given with curative intent. In reports from these specialized centers, 77–87 % of patients undergoing multimodality therapy do so in the neoadjuvant setting.9 , 10 The reasons for this higher utilization of neoadjuvant therapy at NCI-designated centers are unclear, but may be related to center preference, more aggressive treatment strategies for borderline resectable disease, patient selection, patient decision-making, intent to resect, or more rigorous follow-up. Our trends over time suggest that this is being more widely adopted, but still not the standard of care for those with resectable disease and understandably so given that optimal timing of chemotherapy has yet to be clearly defined.
There are limitations to our study; as a retrospective cohort study, ours is subject to potential selection bias. Our results demonstrate disparities in treatment based on age and treating facility. We cannot definitively make conclusions as to why these treatment patterns occur or the intent of treatment for patients who received chemotherapy alone or first. The NCDB lacks information on variables such as progression of disease, which may also explain the disparities in treatment. Patient preference or inability to tolerate treatment could contribute be contributing factors as well. Given there were a greater proportion of older individuals with 90-day mortality, this may explain issues with older patients not receiving multimodality therapy in the adjuvant setting, or patients may have simply not elected to undergo an invasive operation or receive rigorous chemotherapy treatments based on their own personal wishes. Finally, our cohort includes stage II cancers, some of which may be locally advanced and unresectable or borderline resectable.
Conclusion
Our study provides insight into treatment patterns of patients on a national scale across all facilities for patients of all ages. We observed that despite increased use of multimodality therapy in this more contemporary time period, it still remains underutilized. Our data also suggest that 90-day mortality was highest in older patients and those receiving surgery first, suggesting postoperative complications may preclude older patients from receiving multimodality therapy. When multimodality therapy is administered in the neoadjuvant setting, this is only in a minority of cases, despite higher rates of utilization and completion at specialized centers. Its use remains debatable and factors such as facility type and age play an important role in determining which patients receive such treatment.
References
Siegel, R., D. Naishadham, and A. Jemal, Cancer statistics, 2013. CA Cancer J Clin, 2013. 63(1): p. 11-30.
Sugiura, T., K. Uesaka, K. Mihara, et al., Margin status, recurrence pattern, and prognosis after resection of pancreatic cancer. Surgery, 2013. 154(5): p. 1078-86.
Raut, C.P., J.F. Tseng, C.C. Sun, et al., Impact of resection status on pattern of failure and survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Ann Surg, 2007. 246(1): p. 52-60.
Hernandez, J., J. Mullinax, W. Clark, et al., Survival after pancreaticoduodenectomy is not improved by extending resections to achieve negative margins. Ann Surg, 2009. 250(1): p. 76-80.
Smaglo, B.G. and M.J. Pishvaian, Postresection chemotherapy for pancreatic cancer. Cancer J, 2012. 18(6): p. 614-23.
Kooby, D.A., T.W. Gillespie, Y. Liu, et al., Impact of adjuvant radiotherapy on survival after pancreatic cancer resection: an appraisal of data from the national cancer data base. Ann Surg Oncol, 2013. 20(11): p. 3634-42.
Mayo, S.C., D.F. Austin, B.C. Sheppard, et al., Adjuvant therapy and survival after resection of pancreatic adenocarcinoma: a population-based analysis. Cancer, 2010. 116(12): p. 2932-40.
Kosuge, T., T. Kiuchi, K. Mukai, et al., A multicenter randomized controlled trial to evaluate the effect of adjuvant cisplatin and 5-fluorouracil therapy after curative resection in cases of pancreatic cancer. Jpn J Clin Oncol, 2006. 36(3): p. 159-65.
Cooper, A.B., H.M. Holmes, J.K. des Bordes, et al., Role of neoadjuvant therapy in the multimodality treatment of older patients with pancreatic cancer. J Am Coll Surg, 2014. 219(1): p. 111-20.
Tzeng, C.W., H.S. Tran Cao, J.E. Lee, et al., Treatment sequencing for resectable pancreatic cancer: influence of early metastases and surgical complications on multimodality therapy completion and survival. J Gastrointest Surg, 2014. 18(1): p. 16-24; discussion 24-5.
Golcher, H., T.B. Brunner, H. Witzigmann, et al., Neoadjuvant chemoradiation therapy with gemcitabine/cisplatin and surgery versus immediate surgery in resectable pancreatic cancer: Results of the first prospective randomized phase II trial. Strahlenther Onkol, 2014.
Christians, K.K., S. Tsai, A. Mahmoud, et al., Neoadjuvant FOLFIRINOX for borderline resectable pancreas cancer: a new treatment paradigm? Oncologist, 2014. 19(3): p. 266-74.
Bilimoria, K.Y., D.J. Bentrem, C.Y. Ko, et al., National failure to operate on early stage pancreatic cancer. Ann Surg, 2007. 246(2): p. 173-80.
Vanderveen, K.A., R.J. Canter, D. Yin, et al., Factors affecting treatment delivery and outcomes of patients with early-stage pancreatic adenocarcinoma. Pancreas, 2011. 40(3): p. 480-2.
Riall, T.S., C.M. Townsend, Jr., Y.F. Kuo, et al., Dissecting racial disparities in the treatment of patients with locoregional pancreatic cancer: a 2-step process. Cancer, 2010. 116(4): p. 930-9.
Murphy, M.M., J.P. Simons, S.C. Ng, et al., Racial differences in cancer specialist consultation, treatment, and outcomes for locoregional pancreatic adenocarcinoma. Ann Surg Oncol, 2009. 16(11): p. 2968-77.
Cooper, A.B., A.D. Parmar, T.S. Riall, et al., Does the Use of Neoadjuvant Therapy for Pancreatic Adenocarcinoma Increase Postoperative Morbidity and Mortality Rates? J Gastrointest Surg, 2014.
Corsini, M.M., R.C. Miller, M.G. Haddock, et al., Adjuvant radiotherapy and chemotherapy for pancreatic carcinoma: the Mayo Clinic experience (1975-2005). J Clin Oncol, 2008. 26(21): p. 3511-6.
Herman, J.M., M.J. Swartz, C.C. Hsu, et al., Analysis of fluorouracil-based adjuvant chemotherapy and radiation after pancreaticoduodenectomy for ductal adenocarcinoma of the pancreas: results of a large, prospectively collected database at the Johns Hopkins Hospital. J Clin Oncol, 2008. 26(21): p. 3503-10.
Yeo, C.J., R.A. Abrams, L.B. Grochow, et al., Pancreaticoduodenectomy for pancreatic adenocarcinoma: postoperative adjuvant chemoradiation improves survival. A prospective, single-institution experience. Ann Surg, 1997. 225(5): p. 621-33; discussion 633-6.
Parmar, A.D., G.M. Vargas, N.P. Tamirisa, et al., Trajectory of care and use of multimodality therapy in older patients with pancreatic adenocarcinoma. Surgery, 2014. 156(2): p. 280-9.
Simons, J.P., S.C. Ng, T.P. McDade, et al., Progress for resectable pancreatic [corrected] cancer?: a population-based assessment of US practices. Cancer, 2010. 116(7): p. 1681-90.
Bilimoria, K.Y., A.K. Stewart, D.P. Winchester, et al., The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol, 2008. 15(3): p. 683-90.
Davila, J.A., E.Y. Chiao, J.C. Hasche, et al., Utilization and determinants of adjuvant therapy among older patients who receive curative surgery for pancreatic cancer. Pancreas, 2009. 38(1): p. e18-25.
Papalezova, K.T., D.S. Tyler, D.G. Blazer, 3rd, et al., Does preoperative therapy optimize outcomes in patients with resectable pancreatic cancer? J Surg Oncol, 2012. 106(1): p. 111-8.
Sener, S.F., A. Fremgen, H.R. Menck, et al., Pancreatic cancer: a report of treatment and survival trends for 100,313 patients diagnosed from 1985-1995, using the National Cancer Database. J Am Coll Surg, 1999. 189(1): p. 1-7.
Bilimoria, K.Y., D.J. Bentrem, C.Y. Ko, et al., Multimodality therapy for pancreatic cancer in the U.S. : utilization, outcomes, and the effect of hospital volume. Cancer, 2007. 110(6): p. 1227-34.
Sen, N., S. Falk, and R.A. Abrams, Role of chemoradiotherapy in the adjuvant and neoadjuvant settings for resectable pancreatic cancer. Clin Oncol (R Coll Radiol), 2014. 26(9): p. 551-9.
Merkow, R.P., K.Y. Bilimoria, J.S. Tomlinson, et al., Postoperative complications reduce adjuvant chemotherapy use in resectable pancreatic cancer. Ann Surg, 2014. 260(2): p. 372-7.
Artinyan, A., D.A. Anaya, S. McKenzie, et al., Neoadjuvant therapy is associated with improved survival in resectable pancreatic adenocarcinoma. Cancer, 2011. 117(10): p. 2044-9.
Funding
Supported by grants from the Cancer Prevention Research Institute of Texas Grant # RP140020 , UTMB Clinical and Translational Science Award #UL1TR000071, NIH T-32 Grant # 5T32DK007639, and AHRQ Grant # 1R24HS022134.
Author information
Authors and Affiliations
Corresponding author
Additional information
Primary Discussant
Dr. Stephen W. Behrman, M.D. (Memphis, TN):
Dr. Dimou and her colleagues confirm that multimodality therapy is superior to single modality treatment in early stage pancreatic cancer. Sadly, when viewed through the lens of this population-based study, the picture of our compliance to this principle is not very flattering. Utilizing the National Cancer Database, the authors demonstrate a promising 40 % increased odds of receiving multimodality therapy from 2004 to 2011, but still only 35 % of almost 40,000 patients received combined modality treatment. These types of studies, unfortunately, often leave too much unsaid in terms of the vagaries that might determine why and whether the individual patient receives one type of treatment or another or whether they may not receive treatment at all. Having said so, the pulse of this study suggests we could raise the bar on survival from pancreatic cancer in this country if we just worked better as a team. I have the following questions:
1. Prior studies have demonstrated that advanced age is independently associated with morbidity and death following pancreatectomy and that serious complications increase the likelihood of not receiving adjuvant therapy by over 2-fold in this cohort. In your study, 45 % of those greater than age 76 received no treatment and only 15 % received multimodality treatment. Did you try to tease that out a bit further? Was there any data on post-operative complications (or perhaps length of stay or readmission as a surrogate)? What about ECOG status prior to initiation or completion of neoadjuvant therapy or prior to starting adjuvant therapy in these older patients?
2. Do you have any information on those that received neoadjuvant therapy in terms of how many progressed and thus did not have surgery or those that might have had deterioration in their performance status especially those in older populations where multimodality therapy was less often utilized?
3. While the use of multimodality therapy was higher in NCI-designated centers, those receiving neoadjuvant therapy were in the minority. Was the number having surgery following neoadjuvant therapy higher in NCI designated centers than other settings?
This manuscript is very well written and analyzed, and I would like to thank the program committee for the opportunity to discuss this fine work.
Closing Discussant
Dr. Dimou:
Dr. Behrman, thank you for your comments. Of the 4202 patients 76 and older, only 38 % who underwent surgery as the initial treatment modality received adjuvant chemotherapy within 6 months, which is less than the 63 % for the 17,431 patients in the overall cohort who had surgery first. While the National Cancer Database (NCDB) does not have information on post-operative complications or ECOG performance status, we are certain that postoperative complications combined with the lack of physiologic reserve in the older population lead to decreased rates. Data from the NSQIP pancreatectomy project demonstrated that older patients have similar complication rates, but are more likely to fail to rescue, suggesting that once they have complications, they are less likely to recover. However, it may also be that many older patients are not offered or choose not to have adjuvant therapy.
To answer your second question, the NCDB lacks information on progression of disease and performance status. The NCDB does, however, report on reasons for not undergoing treatment, including contraindications and patient refusal. Clear contraindications and refusal were only coded in 5 % of the entire cohort and does not fully describe the reasons for lack of treatment within the entire cohort, especially older patients. We suspect there is an element of physician nihilism, but also acknowledge the possibility that patient choice and subtle contraindications (or good patient selection) are not captured.
It is important to note that patients classified as having neoadjuvant therapy were only placed in this treatment group if they received both chemotherapy prior to resection and surgical resection. If they never received resection, patients were placed in the chemotherapy only category and not classified as neoadjuvant. We did an analysis of all patients who got chemotherapy as the initial treatment modality, recognizing that this is not always given with neoadjuvant intent. Only 17 % of patients who had chemotherapy first went on to surgical resection. At NCI-designated cancer centers, 30 % of patients who received initial chemotherapy went on to surgical resection. Likewise, NCI-designated centers were more likely to have patients undergo both surgical resection and adjuvant chemotherapy compared to other treatment facilities, and overall, more likely to provide some sort of treatment to patients compared to other treatment centers.
Rights and permissions
About this article
Cite this article
Dimou, F., Sineshaw, H., Parmar, A.D. et al. Trends in Receipt and Timing of Multimodality Therapy in Early-Stage Pancreatic Cancer. J Gastrointest Surg 20, 93–103 (2016). https://doi.org/10.1007/s11605-015-2952-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2952-7