Abstract
Background
Achievement of negative margins is the goal of curative intent surgery for hilar cholangiocarcinoma. This study analyzed factors affecting survival in hilar cholangiocarcinoma patients and compared short- and long-term outcomes of left- and right-sided resections.
Methods
One hundred and five patients out of 124 diagnosed with Klatskin tumors underwent major liver resection. Sixty-one patients underwent right-sided resections (right group), whereas 44 underwent left-sided resections (left group). Perioperative morbidity, perioperative mortality, and overall and disease-free survival were compared between the groups.
Results
Morbidity and mortality were higher in the right group (59 and 8.2 %, respectively) than in the left group (38.6 and 2.3 %, respectively) (p < 0.005). The most frequent cause of death was liver failure. The R0 rate was 75.4 % in the right and 61.4 % in the left group. The 5-year survival rate was 42.8 % in the right and 35.3 % in the left group (p < 0.05). Patients in the left group more frequently developed local recurrence (87 vs. 69 % in the right group).
Conclusion
Lesion side impacts outcome: right resections still cause significant morbidity related to extensive parenchymal sacrifice but are associated with better long-term survival because right hepatic pedicle resection enables better radicality compared with left resections.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgical resection with negative margins represents the only potentially curative treatment for patients with hilar cholangiocarcinoma.1 Indeed, although R1 margins allow achievement of better long-term survival compared with unresected patients, R0 resection is still the only significant prognostic factor for survival that can be affected by pre- and intraoperative management and should therefore be considered the main endpoint of surgery.1 – 3 The diagnosis of a Klatskin tumor necessitates biliary confluence resection associated with major hepatectomy to reduce the risk of liver recurrence by controlling both direct parenchymal invasion and neoplastic infiltration along bile ducts.1 , 4 , 5 However, extensive parenchymal demolition, together with the high incidence of cholestasis-related complications, leads to significantly higher postoperative morbidity (29–75 %) and mortality (0–17 %) in association with this procedure relative to conventional hepatic surgery.2 , 6 , 7
To reduce the postoperative complication rate, thorough preoperative optimization is fundamental and should be performed in a multidisciplinary setting.8 , 9 The assessment of resectability and surgical planning are based on imaging findings, with focused evaluation of disease infiltration along the bile ducts and vascular involvement to determine the side (left/right) and extent (major/extended) of the planned hepatectomy.4 , 10 , 11 The biliary confluence has a close anatomical relationship with the right hepatic vascular pedicle that is located just behind it. Therefore, the primary endpoint of this study was to evaluate the impact of lesion side on short- and long-term outcomes. Secondary endpoints were to assess the implications of lesion side on preoperative management and to determine the accuracy of lesion side as a prognostic factor.
Materials and Methods
Patients
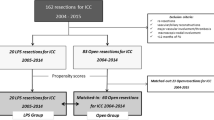
Between January 2004 and January 2014, 124 patients with hilar cholangiocarcinoma were candidates for surgery at the Hepatobiliary Surgery Unit of San Raffaele Hospital in Milan. Data from these patients were collected in a prospective database and are now retrospectively reviewed. Out of 124 patients, 14 were excluded from surgery during staging laparoscopy or at laparotomy. Five patients underwent biliary confluence resection associated with minor hepatectomy. Therefore, the study population consisted of 105 patients: 61 had right disease extension (right group) requiring right hepatectomy or right trisectionectomy and 44 had left disease extension (left group) requiring left hepatectomy or left trisectionectomy. Approval to perform this retrospective study was obtained from the IRB and consent from subjects was waived.
Preoperative Workup
Preoperative workup has been described elsewhere.9 Standard thoracoabdominal imaging (computed tomography and magnetic resonance cholangiopancreatography) was routinely performed in all candidates prior to surgery; more recently, endoscopic ultrasound (EUS) was also introduced during the preoperative workup to evaluate biliary and vascular involvement. Both disease infiltration along the bile ducts and infiltration/encasement of the portal/arterial vessels were considered before planning the side and extent of resection.
Tumor Classification and Histopathological Examination
Histological staging was determined according to TNM classification following the criteria of the American Joint Committee on Cancer (AJCC).12 Bismuth–Corlette classification13 was used to define tumor extension along the intrahepatic bile ducts preoperatively. Frozen sections of both proximal and distal margins were intraoperatively examined to rule out residual disease along the bile ducts.
Resectability Criteria
The Memorial Sloan Kettering Cancer Center (MSKCC) staging system was used to assess resectability.4 Nodal involvement was not considered an absolute contraindication to surgery unless metastases beyond the hepatoduodenal ligament were detected.4
Preoperative Management
Standard preoperative management has been described elsewhere.9 Briefly, placement of percutaneous transhepatic biliary drainage (PTBD) in the future liver remnant (FLR) was indicated in jaundiced patients who were candidates for portal vein embolization (PVE) because of inadequate FLR volume at CT scan.14 In patients with adequate FLR, the need for PTBD of the FLR was evaluated on a case-by-case basis according to the severity (total bilirubin >15 mg/dL) and duration (>15 days) of jaundice.
Surgery
Lymphadenectomy and segment 1 resection were routinely performed. Tumor infiltration at intraoperative frozen section examination constituted an indication for widening the margins within the liver parenchyma as much as technically feasible along with multiple segmental biliary enteric anastomosis.
Outcome Evaluation
Preoperative patient and disease characteristics as well as requirement for biliary drainage and PVE were recorded. Postoperative complications were reviewed for 90 days following liver resection and were graded retrospectively according to the Dindo–Clavien classification of surgical complications.15 Postoperative mortality was defined as any death during hospitalization or within 90 days after resection. Postoperative liver failure was defined according to the ISGLS definition.16 Patient survival was determined from surgery until the time of death or most recent follow-up. Three- and 5-year overall and disease-free survival were evaluated using the Kaplan–Meier method.
Statistical Analysis
Comparisons were performed using the χ 2 test or Fisher’s exact test for categorical data and the Mann–Whitney U test for ordinal data. Cox regression was used to determine independent predictors of outcome, using survival as the dependent variable and factors found to be significant (p < 0.05) in univariate analysis as covariates. Nonparametric data analysis was performed using the χ 2 or Fisher’s exact test as appropriate. All data are expressed as mean plus standard deviation or as median and range when appropriate. Significance was defined as p < 0.05. All analyses were performed using the statistical package SPSS 18.0 (SPSS, Chicago, IL, USA).
Results
Preoperative Characteristics
The preoperative characteristics of the 105 patients treated with curative intent surgery are summarized in Table 1. Sixty-one males (58.1 %) and 44 females (41.9 %) with a median age of 60 years (range 36–82 years) were included in the study. The incidence of jaundice was similar between the groups (85.2 % in the right group and 86.4 % in the left group), even though the number of patients with total bilirubin >15 mg/dL was significantly higher in the right group (47.5 vs. 38.6 % in the left group; p = 0.049).
Preoperative Management and Surgical Details
Among jaundiced patients, 63.9 % in the right group and 52.3 % in the left group underwent preoperative biliary drainage (p = 0.027). Twenty-nine patients (representing 47.5 % of the right group 27.6 % of the whole series) underwent PVE for inadequate FLR, with a mean volume increase of 45.6 ± 29.7 %. No patients in the left group required portal vein occlusion. Forty-three right hepatectomies and 18 right trisectionectomies were performed in the right group, whereas 32 left hepatectomies and 12 left trisectionectomies were performed in the left group (p = NS). The right and left groups were comparable in terms of use of the Pringle maneuver, intraoperative blood loss, rate of intraoperative blood transfusion administration, and surgery length, as shown in Table 2. Portal vein resection with end-to-end anastomosis was performed as necessary in eight cases of vein wall infiltration by neoplastic tissue. Arterial resection and reconstruction were required in four patients who showed vessel encasement or infiltration.
Histopathological data are summarized in Table 2. R0 resection was achieved in 73 patients (69.5 % of the whole series). Thirty patients (28.6 %) had R1 margins (14 on the biliary stump, 9 on connective tissue, 4 because of portal vein involvement, and 3 because of liver parenchyma infiltration). Sixteen patients (26.2 %) in the right group and 11 patients (25 %) in the left group had positive intraoperative margins on frozen section analysis; there was no significant difference between the groups. In these patients, additional resection of the margins was performed to the extent technically feasible, resulting in R0 bile duct resection in 13 patients in the right group and 9 patients in the left group (p = NS). Perineural invasion was detected in 29 patients (47.5 %) in the right group and 26 patients (61.4 %) in the left group (p = 0.043), whereas lymphatic invasion was present in 32 patients (52.5 %) in the right group and 26 patients (59.1 %) in the left group (p = 0.005). Whereas evidence of macroscopic vascular invasion did not statistically differ between the groups, a significantly higher rate of microvascular invasion (47.7 %; 21 patients) was found in the left group compared with the right group (34.3 %, 21 patients).
Postoperative Outcome
Whole series morbidity was 50.5 % (59 and 38.6 % in the right and left groups, respectively; p = 0.028). Mortality was 5.7 % (8.2 and 2.3 % in the right and left groups, respectively; p = 0.0065). Postoperative complications are detailed in Table 3. Both minor (Dindo grades I and II) and major (Dindo grades III–V) events were more frequent in the right group compared with the left group. Separate analysis of single complications showed a different incidence of wound infection (11.5 % in the right group and 6.8 % in the left group), fever (21.35 % in the right group and 13.6 % in the left group), deep vein thrombosis (3.3 % in the right group and 0 % in the left group), and liver failure (11.5 % in the right group and 4.5 % in the left group) between the groups. Six patients died in the postoperative period: four (all belonging to the right group) developed irreversible and progressive signs of liver failure (progressive isolated hyperbilirubinemia without evidence of biliary obstruction and with ensuing encephalopathy and hepatic coma in two cases, refractory ascites and pleural effusion complicated by pneumonia and subsequent respiratory failure in one case, and hyperbilirubinemia together with portal hypertension leading to gastric bleeding refractory to endoscopic treatment in one case)16; one patient (from the right group) developed septic shock from cholangitis; and one patient from the left group had severe bilateral pulmonary embolism leading to respiratory failure and then cardiac arrest.
The median postoperative stay was shorter in left group (11 days; range 8–31) compared with the right group (15 days; range 9–69).
Prognostic Factors
Prognostic factors after resection were evaluated in the entire series of patients (105 patients). In univariate analysis, 13 clinicopathological factors were analyzed; among them, 9 were significantly associated with prognosis (see Table 4 for details). Multivariate analysis revealed side of hepatectomy, Bismuth type, nodal status, and resection margins to be independent prognostic factors.
Long-term Survival
The median follow-up was 23 months (range 3–98 months). The 3- and 5-year survival rates were 51.3 and 39 %, respectively. Disease-free survival was 39.5 % at 3 years and 28.1 % at 5 years. Local recurrence was the most frequent pattern of recurrence (75 % had isolated local recurrence, 20 % had both local and distant metastases, and 5 % developed distant metastases only). Survival was then further analyzed according to the side of hepatectomy; the respective 3- and 5-year survival rates were 49.5 and 35.3 % in the left group and 53.2 and 42.8 % in the right group, a statistically significant difference (see Fig. 1). Patients in the left group more frequently showed local recurrence (87 % of patients presented with local recurrence, 13 % with both local and distant metastases, and no patients developed distant metastases only) compared with the right group (69 % of patients had isolated local recurrence, 22 % had local and distant metastases, and 9 % developed only distant metastases).
Discussion
Surgical planning and preoperative optimization are fundamental steps in the therapeutic management of patients with hilar cholangiocarcinoma.8 , 9 The extent and side of the planned liver resection are determined according to disease infiltration along the bile ducts and toward hepatic vessels.3 , 4 Further patient management diverges depending on the planned strategy; the predominant side of the tumor, and therefore hepatectomy side, has significant influence on short- and long-term patient outcomes.10 , 11 Regarding Bismuth–Corlette evaluation, no significant discrepancies were recorded between preoperative (based on imaging) and postoperative (based on histology) classification in our patient series. Therefore, in our experience, Bismuth–Corlette classification is still a valid tool for assessing disease infiltration along the bile ducts and staging biliary involvement. However, it should not be evaluated alone but rather viewed as strictly dependent on the sensitivity and specificity of preoperative imaging techniques. The final assessment of resectability is therefore based on MSKCC criteria.
The present series reported significantly higher morbidity and mortality rates in patients who underwent right-sided resections compared with those who underwent left-sided resections; nevertheless, the long-term outcome was poorer for patients in the left group, who had a 35.3 % 5-year survival rate compared with 42.8 % in the right group. These findings may reflect the need to consider left- and right-sided lesions as two deeply different clinical contexts, therefore requiring distinct management both preoperatively and in terms of oncological management. The biliary confluence indeed lies on the right part of the hepatic pedicle, with the right portal vein just behind it and the right hepatic artery running behind the biliary confluence. Consequently, even with comparable preoperative staging, patients with right disease extension may benefit from a broader clearance of lymphatic and fibroconnective tissue during right resections, leading to a more radical procedure. Indeed, in the present series, hepatectomy side was associated with prognosis, irrespective of hepatectomy extension, leading to a better long-term outcome in the right group with a lower incidence of local recurrence.
However, some previous series in the literature have shown opposing results,17 – 19 perhaps because of differences in selection criteria for surgery, differing indications for extended hepatectomies and vascular resections (many authors routinely perform right or left trisectionectomy combined with portal vein resection according to a “no touch technique”18 , 19), and differences in the incidence of R1 resections. The present study further highlights the crucial role of a correct preoperative management flowchart in optimizing short-term results. Furthermore, surgical planning cannot be overlooked as part of a tailored treatment plan. Indeed, in right resections the management of severe jaundice and inadequate FLR, which are associated with postoperative morbidity and mortality, frequently requires step-by-step optimization before surgery. The role of “on principle” biliary drainage in lowering the risk of morbidity and mortality is still a matter of debate in the literature.20 – 24 Two recent reviews20 , 24 concluded that drainage of the FLR is strongly recommended in the following situations: planned PVE because of an inadequate FLR; borderline FLR volume, even in the absence of planned PVE; and when cholestasis-related complications occur.
In the authors’ experience, patients scheduled for right hepatectomy should be managed according to FLR volume as outlined below. If FLR is inadequate, the patient is a candidate for external PTBD followed by PVE; in cases with adequate volume hypertrophy, surgical resection with an acceptable risk of postoperative liver failure is achievable. If FLR is adequate, the timing of surgery is dependent on the severity of jaundice. In patients with a recent onset of jaundice (<15 days) and a bilirubin level <15 mg/dL, upfront surgery is indicated. In patients with more prolonged jaundice (>15 days) and/or a bilirubin level >15 mg/dL, the placement of external PTBD in the FLR (left liver) is indicated, and surgery is delayed until effective bilirubin reduction. In contrast, left hepatectomy or left trisectionectomy is on principle associated with an adequate FLR, so the timing of surgical treatment should be based only on the need for jaundice resolution.
In patients with impaired liver function due to prolonged cholestasis and with small tumoral volume, although extensive parenchymal demolition leads to higher morbidity and mortality rates compared with conventional hepatic surgery (the complication rate following hepatectomy for other primary and secondary liver tumors is around 20 %,25 with a mortality rate <3 % in a recent series26), the recent results of Klatskin tumor surgery are encouraging.3 Despite this, septic and metabolic complications may contribute to worsening of borderline hepatic function in these patients, leading to both anatomical and functional damage to the liver architecture, which may be fatal. Furthermore, drastic reduction of the vascular bed during major hepatectomy may lead to acute portal hypertension and life-threatening secondary complications; indeed, four patients in the present series died because of irreversible liver failure.
To deal with the poorer prognosis of patients with left-sided infiltration, both a tailored surgical strategy and additional therapies can be proposed. In the present series, long-term outcome did not seem to be influenced by the extent of resection, perhaps as a result of the relatively small number of patients; despite this, a role for left trisectionectomy in the treatment of hilar cholangiocarcinoma with left infiltration (even in patients who are candidates for left hepatectomy) has been reported in the literature.27 , 28 The radical surgical clearance of microscopic disease that is presumed to be responsible for local recurrence is the rationale of this strategy. Left trisectionectomy is generally considered a demanding procedure that requires advanced skills in hepatobiliary surgery but, when performed in high volume centers, is associated with the same morbidity and mortality rates reported for left hepatectomy. Hosokawa et al.27 reported better overall survival and a reduced incidence of locoregional recurrence (although these findings did not reach statistical significance) among patients who underwent left trisectionectomy leading to R0 resection, suggesting that locoregional recurrence after R0 resection relates not only to length of the ductal-free margin but also to other factors such as depth of tumor invasion into the liver parenchyma and fibroconnective tissue of the hepatic pedicle, vascular invasion, and lymphatic involvement.
In the present series, 26.2 % of patients in the right group and 25 % of those in the left group had positive proximal margins at intraoperative frozen section and therefore required further biliary resection; although performing this procedure on the right side of the biliary tree is frequently more technically demanding because of features of the right intrahepatic ducts (shorter length, more distal binary confluence of the segmentary branches), no differences in the achievement of negative margins were identified. Ribero et al.28 also reported that additional resection of positive intraoperative margins improves survival and should be attempted whenever possible. Furthermore, patients in whom R0 resections are obtained after biliary margin enlargement have similar outcomes compared with patients who undergo primary R0 resections.
The role of additional neoadjuvant or adjuvant therapies in patients with resectable Klatskin tumors is still controversial and is debated in the literature, so standardized indications are not available.29 , 30 Whereas no systemic adjuvant therapy appears to be associated with a survival benefit, encouraging results have been reported by the Mayo Clinic with the use of preoperative chemoradiation in patients with advanced hilar cholangiocarcinoma.31 As reported by Gerhards et al., resected patients may benefit from adjuvant radiotherapy in terms of improved median survival times,32 and the use of targeted therapies (anti-EGFR and antiangiogenic drugs33) and photodynamic treatments34 has also been reported in this setting. Although all of these options need to be confirmed by large-scale randomized trials, they may represent valuable alternatives with the potential to improve outcomes for patients with negative prognostic factors. A prospective trial evaluating the impact of neoadjuvant or adjuvant radiotherapy in patients requiring left-sided resections would be useful.
The retrospective design of the present series can be considered a study limitation, together with the relatively small sample size collected from a single institution and the relatively recent introduction of standard preoperative optimization. Because of these limitations, it is possible that the study may have overestimated the real impact of lesion side on prognosis or underestimated the value of upfront extended resections in patients with a high risk of recurrence. We truly hope that a future international multi-center prospective trial will provide conclusive data by comparing patients undergoing right- and left-sided resections, evaluating the impact of extended hepatectomies and vascular reconstructions, and eventually focusing on patients with demonstrated negative prognostic factors. Otherwise, the use of extended hepatectomies and vascular reconstructions, which clearly have some advantages but are technically more demanding and carry increased risk, is not ethically justified.
Conclusion
In conclusion, the results from this study suggest that lesion side, and therefore hepatectomy side, impacts short- and long-term outcomes in patients with Klatskin tumors. Patients requiring right resections, which carry a high risk of postoperative complications, should undergo comprehensive and individually tailored preoperative management to lower the risk of postoperative complications (in particular, postoperative liver failure) that lead to a significant mortality rate in this patient population. In contrast, more extensive surgical or oncological protocols should be considered for patients with left-sided disease to deal with undetectable microscopic disease that is left untreated by surgical resection and elevates the risk of local recurrence.
References
Ito F, Agni R, Rettammel RJ, Been MJ, Cho CS, Mahvi DM, Rikkers LF, Weber SM. Resection of hilar cholangiocarcinoma: concomitant liver resection decreases hepatic recurrence. Ann Surg 2008; 248:273–9.
Ito F, Cho CS, Rikkers LF, Weber SM. Hilar cholangiocarcinoma: current management. Ann Surg 2009; 250(2):210–8.
Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, Nimura Y. Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg 2013; 258 (1):129–40.
Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BSJ, Klimsta D, Blumgart LH. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 2001; 234(4):507–17.
Van Gulik TM, Kloek JJ, Ruys AT, Busch OR, van Tienhoven GJ, Lameris JS, Rauws EA, Gouma DJ. Multidisciplinary management of hilar cholangiocarcinoma (Klatskin tumor): extended resection is associated with improved survival. Eur J Surg Oncol 2001; 37(1):65–71.
Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K, Matsumoto J, Kawasaki R. Outcome of surgical treatment of hilar cholangiocarcinoma: a special reference to postoperative morbidity and mortality. J Hepatobiliary Pancreat Sci 2010; 17(4):455–62.
Gomez D, Patel PB, Lacasia-Purroy C,, Byrne C, Sturgess RP, Palmer D, Fenwick S, Poston GJ, Malik HZ. Impact of specialized multi-disciplinary approach and an integrated pathways on outcomes in hilar cholangiocarcinoma. Eur J Surg Oncol 2014; 40(1):77–84.
Grandadam S, Compagnon P, Arnaud A Olivié D, Malledant Y, Meunier B, Launois B, Boudjema K. Role of preoperative optimization of the liver for resection in patients with hilar cholangiocarcinoma type III. Ann Surg Oncol 2010; 17(12):3155–61.
Ratti F, Cipriani F, Ferla F, Catena M, Paganelli M, Aldrighetti LA. Hilar cholangiocarcinoma: preoperative liver optimization with multidisciplinary approach. Toward a better outcome. World J Surg 2013; 37(6): 1388–96.
Neuhaus P, Thelen A. Radical surgery for right-sided Klatskin tumor. HPB 2008; 10:171–173.
Nimura Y. Radical surgery of left-sided Klatskin tumors. HPB 2008; 10:168–170.
American Joint Committee on Cancer. Extrahepatic bile ducts. In: Fleming ID, Cooper JS, et al., eds. AJCC cancer staging manual. Philadelphia: Lippencott-Raven 1997; 109 –111.
Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet 1975; 140(2):170–8.
Ratti F, Soldati C, Catena M, Paganelli M, Ferla G, Aldrighetti L. Role of portal vein embolization in liver surgery: single centre experience in sixty-two patients. Updates Surg 2010; 62(3–4):153–9.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanther R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-years experience. Ann Surg 2009; 250(2): 187–96.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, High TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan St, Nimura Y, Figueras J, Capussotti L, Buchler MW, Weitz J. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011; 149:713 – 724.
Unno M, Katayose Y, Rikiyama T, Yoshida H, Yamamoto K, Morikawa T, Hayashi H, Motoi F, Egawa S. Major hepatectomy for perihilar cholangiocarcinoma. J Hepatobil Pancreat Sci 2010; 17:463–469.
Neuhaus P, Jonas S, Settmacher U, Thelen A, Benckert C, Lopez-Hanninen E, Hintze RE. Surgical management of proximal bile duct cancer: extended right lobe resection increases resectability and radicality. Langenbecks Arch Surg 2003; 388:194–200.
Shimizu H, Kimura F, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, Furukawa K, Miyazaki M. Aggressive surgical resection for hilar cholangiocarcinoma of the left-side predominance: radicality and safety of left sided-hepatectomy. Ann Surg 2010; 251:281–286.
Liu F, Li Y, Wei Y, Li B. Preoperative biliary drainage before resection for hilar cholangiocarcinoma: whether or not? A systematic review. Dig Dis Sci 2011; 56(3):663–72.
Kloek JJ, van der Gaag NA, Aziz Y, Rauws EA, van Delden OM, Lameris JS, Busch OR, Gouma DJ, van Gulik TM. Endoscopic and percutaneous preoperative biliary drainage in patients with suspected hilar cholangiocarcinoma. J Gastrointest Surg 2010; 14(1):119–25.
Ferrero A, Lo Tesoriere R, Viganò L, Caggiano L, Sgotto E, Capussotti L. Preoperative biliary drainage increases infectious complications after hepatectomy for proximal bile duct tumor obstruction. World J Surg 2009; 33(2):318–25.
Kennedy TJ, Yopp A, Qui Y, Zhao B, Guo P, Liu F, Schwartz LH, Allen P, D’Angelica M, Fong Y, DeMatteo RP, Blumgart LH, Jarnagin WR. Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB 2009; 11(5):445–51.
Paik WH, Loganathan N, Hwang JH. Preoperative biliary drainage in hilar cholangiocarcinoma: when and how? World J Gastrointest Endosc 2014; 6(3):68–73.
Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg 2004; 240(4):698–708.
De Jong MC, Pulitanò C, Ribero D, Strub J, Mentha G, Schulick RD, Choti MA, Aldrighetti L, Capussotti L, Pawlik TM. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg 2009; 250(3):440–8.
Hosokawa I, Shimizu H, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, Miyazaki M. Surgical strategy for hilar cholangiocarcinoma of the left-side predominance. Current role of left trisectionectomy. Ann Surg 2014;259(6):1178–85.
Ribero D, Amisano M, Lo Tesoriere R, Rosso S, Ferrero A, Capussotti L. Additional resection of an intraoperative margin-positive proximal bile duct improves survival in patients with hilar cholangiocarcinoma. Ann Surg 2011;254(5):776–81.
Grendar J, Grendarova P, Sinha R, Dixon E. Neoadjuvant therapy for downstaging of locally advanced hilar cholangiocarcinoma: a systematic review. HPB (Oxford). 2014;16(4):297–303.
Soares KC, Kamel I, Cosgrove DP, Herman JM, Pawlik TM. Hilar cholangiocarcinoma: diagnosis, treatment options, and management. Hepatobiliary Surg Nutr. 2014 Feb;3(1):18–34.
Rosen CB, Heimbach JK, Gores GJ. Liver transplantation for cholangiocarcinoma. Transpl Int. 2010 Jul;23(7):692–7.
Gerhards MF, van Gulik TM, González González D, Rauws EA, Gouma DJ. Results of postoperative radiotherapy for resectable hilar holangiocarcinoma. World J Surg. 2003;27(2):173–9.
Sohal DP, Mykulowycz K, Uehara T, Teitelbaum UR, Damjanov N, Giantonio BJ, Carberry M, Wissel P, Jacobs-Small M, O’Dwyer PJ, Sepulveda A, Sun W. A phase II trial of gemcitabine, irinotecan and panitumumab in advanced cholangiocarcinoma. Ann Oncol. 2013;24(12):3061–5.
Park do H, Lee SS, Park SE, Lee JL, Choi JH, Choi HJ, Jang JW, Kim HJ, Eum JB, Seo DW, Lee SK, Kim MH, Lee JB. Randomised phase II trial of photodynamic therapy plus oral fluoropyrimidine, S-1, versus photodynamic therapy alone for unresectable hilar cholangiocarcinoma. Eur J Cancer. 2014;50(7):1259–68.
Conflict of Interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ratti, F., Cipriani, F., Piozzi, G. et al. Comparative Analysis of Left- Versus Right-sided Resection in Klatskin Tumor Surgery: can Lesion Side be Considered a Prognostic Factor?. J Gastrointest Surg 19, 1324–1333 (2015). https://doi.org/10.1007/s11605-015-2840-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2840-1