Abstract
Since the 1950s, amnesia or memory impairment has been repeatedly reported in patients following surgical repair of anterior communicating artery (ACoA) aneurysms. Postoperative infarctions following surgical repair of ACoA aneurysms are classified as involvement of the subcallosal artery (the largest unpaired perforator of the ACoA), the recurrent artery of Heubner (RAH), or a combination of both. Postoperative amnesia can seriously affect the patient’s quality of life, thus prompting physicians to discuss the symptomatology of the three infarction patterns. We made the following speculations regarding the causal relationship between the infarction pattern and postoperative amnesia. First, postoperative amnesia is most likely caused by an infarction in the territory of the subcallosal artery, particularly in the column of the fornix, a constituent of the Papez neuronal circuit. Second, infarction in the RAH territory alone is unlikely to cause significant amnesia. Third, infarcted foci in the RAH territory, when associated with a subcallosal artery infarction, can cause considerable frontal dysfunction due to impaired frontostriatal circuits in patients with postoperative amnesia, with resultant worsening of the long-term outcome or quality of life.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postoperative infarctions following surgical repair of anterior communicating artery (ACoA) aneurysms are classified as involvement of the subcallosal artery (the largest unpaired perforator of the ACoA), the recurrent artery of Heubner (RAH), or a combination of both (Fig. 1). The subcallosal artery and its neighboring perforator, the RAH, are the vessels most commonly affected during treatment of ACoA aneurysms (Fig. 1c). The territory of the subcallosal artery includes the anterior cingulate gyrus, the anterior commissure, the column of the fornix, the paraterminal gyrus (including part of the septum pellucidum), the preoptic area, the rostrum and genu of the corpus callosum, and the subcallosal area (Fig. 2) [1]. The territory of the RAH includes the anterior limb of the internal capsule, the caudate nucleus, the globus pallidus, the nucleus accumbens, and the putamen (Fig. 2) [2].
Anatomy of the subcallosal artery and recurrent artery of Heubner and their supplying basal forebrain region. a Illustration of the subcallosal artery supplying the basal forebrain (reproduced from Mugikura et al. [1]). The subcallosal artery originates from the posterosuperior aspect of the anterior communicating artery (ACoA), ascends dorsally into the lamina terminalis (LT) cistern, and supplies the basal forebrain—the preoptic area (POpA), the paraterminal gyrus including part of the septum pellucidum (PTG), the subcallosal area (SbA), the anterior commissure (AC), and the column of the fornix (FxCo)—and then curves forward and upward to supply the rostrum (CCr) and genu (CCg) of the corpus callosum and the anterior cingulate gyrus (CGa). Thus, the artery exhibits a characteristic S-shaped curve and supplies these eight regions. FM foramen of Monro, MB mammillary body, OC optic chiasm, SP septum pellucidum, A2 A2 segment of the anterior cerebral artery, 3V third ventricle. b Specimen of the anterior cerebral artery and ACoA complex injected with methacrylic resin and viewed from posterior side (reproduced from Mugikura et al. [1]). The subcallosal artery (large arrowheads) is seen arising from the ACoA. A1 and A2, right and left A1 and right and left A2 segments, respectively, of the anterior cerebral arteries; RAH right and left recurrent arteries of Heubner. c Coronal microangiogram of the RAH on both sides and the unpaired subcallosal artery (reproduced from Takahashi et al. [2]). Both internal carotid arteries have been retracted inferiorly to demonstrate the cisternal course of the RAH (red arrows), which follows a curved or tortuous course along the A1 segment of the ACA (white arrows). The branches of the RAH are distributed to a part of the basal forebrain. The subcallosal artery (blue arrow) is also seen arising from the ACoA (yellow arrow)
Identification of the regions of the basal forebrain on magnetic resonance (MR) imaging using multiplanar reconstruction (MPR). All multiplanar reconstruction (MPR) images were generated from three-dimensional (3D) magnetization-prepared rapid gradient-echo (MPRAGE) images (reproduced from Mugikura et al. [1]). The abbreviations used in the figure are summarized in Table 1. a MPR sections passing through the anterior commissure (AC). The coronal image (middle) corresponds to the green line in the left panel (mid-sagittal), and the axial image (right) corresponds to the red line in the left panel, so that both images pass through the midline part of the anterior commissure (AC). b MPR sections passing through the paraterminal gyrus (PTG). The coronal image (middle) corresponds to the green line in the left panel (paramedian sagittal), and the axial image (right) corresponds to the red line in the left panel, so that both images pass through the superior part of the paraterminal gyrus (PTG)
Postoperative amnesia, which has been reported to occur in patients after the surgical clipping or coiling of ACoA aneurysms [1, 3], can seriously affect the patient’s quality of life, thus prompting physicians to discuss the symptomatology of the three infarction patterns. We made the following speculations regarding the causal relationship between the infarction pattern and postoperative amnesia in patients following surgical repair of ACoA aneurysms.
Subcallosal artery infarction
First, postoperative amnesia is most likely caused by an infarction in the territory of the subcallosal artery, particularly in the column of the fornix, a constituent of the Papez neuronal circuit (Fig. 3) [1]. We previously evaluated three-dimensional (3D) T2-weighted magnetic resonance (MR) images for the presence of infarcted foci in ten consecutive patients with postoperative amnesia. All patients had infarcts in the subcallosal artery, and most lesions were present bilaterally; five patients had additional infarcted foci in the RAH territory, all of which were present unilaterally (right side, 4; left side, 1).
A case of subcallosal artery infarction with persistent amnesia with a favorable long-term outcome. A 39-year-old man presented with amnesia immediately after the second clipping of a remnant of a ruptured aneurysm of the ACoA. Neuropsychological examination four months after the aneurysm clipping confirmed the amnesia (intelligence quotient (111) minus memory quotient (68) = 43 > 2 SD, 1 standard deviation [SD] = 15, delayed recall < 50) along with preserved frontal function (processing speed: 105). He continued to work in downgraded jobs ≥ 12 months following ACoA aneurysm repair (favorable long-term outcome), although he had persistent amnesia after 5 years (intelligence quotient (115) minus memory quotient (70) = 45 > 2 SD, delayed recall: 58) along with preserved frontal function (processing speed: 102). Axial (a and b) MPRAGE and coronal (c and d) T2WI-VISTA images taken 4 months after the second clipping bilaterally show infarcted foci in the column of fornix (red arrows) and anterior commissure (blue arrows). In axial image b, the central portion of the pars libera that is located at the posterior end of the paraterminal gyrus or septum pellucidum is missing, with only a circular margin remaining (red arrows). Note that on a and c, infarcted foci in the bilateral anterior commissure show a characteristic bowtie-like appearance, and are associated with the infarcted foci in the adjoining bilateral column of fornix. No infarcted lesions in the RAH were seen in this patient
Specifically, two MR signs appeared characteristic. The first, the bowtie-like appearance of infarcts that may be seen on both axial and coronal MR images, represents bilateral involvement of the anterior commissure associated with infarcted foci in the column of the fornix (Fig. 3).
The second sign, a sagittally elongated infarction along the medial aspect of the brain on axial or sagittal MR planes that involves the anterior cingulate gyrus, genu, and/or rostrum of the corpus callosum, should represent the sagittally elongated vascular distribution along the characteristic S-shaped course of the subcallosal artery (Fig. 5a, b and d). We believe that both signs could prove useful as MR indicators of amnesia associated with ACoA aneurysm treatment.
RAH territory infarction
Second, infarction in the RAH territory alone is unlikely to cause significant amnesia. Mizuta et al. reported the neuropsychological findings of five patients with computed tomography (CT)-documented infarction in the caudate nucleus, presumably in the RAH territory (left, 3; right, 2), following an operation for ACoA aneurysm. In their study, neurosurgeons confirmed vasospasm of the RAH intraoperatively in all patients; no patients showed a significant decrease in the memory quotient (MQ) < 85 as measured using the Wechsler Memory Scale, or reached significant amnesia, defined as the intelligence quotient measured using the Wechsler Adult Intelligence Scale (WAIS) minus the MQ > 15, although mild memory disturbance was noted in three patients with left caudate infarction [4]. In the study by Fukamachi et al. [5], two patients with bilateral RAH infarctions after an operation for ACoA aneurysm did not develop amnesia. We suppose that the subcallosal artery was intact in these patients, which explains why postoperative amnesia did not manifest. Among 14 patients with postoperative amnesia, including four with mild memory disturbance in our previous study [1], none had infarcted foci in the territory of the RAH alone without foci in the territory of the subcallosal artery. We also experienced a patient with unilaterally infarcted foci in the RAH territory but no foci in the subcallosal artery territory; she did not develop postoperative amnesia (Fig. 4).
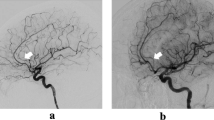
A case of recurrent artery of Heubner (RAH) infarction without amnesia. After operative treatment (titanium clipping) of the unruptured ACoA aneurysm, a 69-year-old woman had no evident neurological symptoms. Neuropsychological examination after the aneurysm clipping showed no evidence of amnesia and normal intellectual function (intelligence quotient: 102, memory quotient: 92). Coronal (a) preoperative MR angiogram shows the multiple unruptured aneurysms located in the ACoA (arrows), bifurcation of the middle cerebral artery on the right, the distal part of the internal carotid artery, and the middle cerebral artery on the left. Surgical clipping of the aneurysms of the ACoA and the bifurcation of the right middle cerebral artery was successfully performed. Postoperative computed tomography scan (b), and axial (c) and coronal (d) multiplanar reconstruction images of T2-weighted VISTA imaging show infarcts in the nucleus accumbens, anteroinferior part of the head of the caudate nucleus, and anterior limb of the internal capsule, which presumably represent the RAH distribution (c and d, asterisks). The midline part of the basal forebrain, including the paraterminal gyrus (c and d, red arrows) and column of the fornix (c, white arrow) on both sides perfused by the unpaired subcallosal artery, is preserved from infarction. Regarding the caudate nucleus (Fig. 1c), its inferior part perfused by the RAH is infarcted while its superior part, perfused by the lateral striate arteries, is not infarcted (Fig. 4d, #)[2]. The neuropsychological findings including memory may vary depending on the site involved with the head of the caudate nucleus
RAH infarction associated with subcallosal artery infarction
Third, infarcted foci in the RAH territory, when associated with a subcallosal artery infarction (Figs. 5, 6), can considerably worsen the long-term outcome of patients with postoperative amnesia. Our patients with involvement in both territories had worse outcomes than those with a subcallosal artery infarction alone and no involvement in the RAH territory [6]. When we re-examined the data from patients in our previous study, the processing speed measured using the WAIS representing frontal function decreased (> 15:1, standard deviation = 15, mean 100) in four of five patients with subcallosal artery and RAH involvement; all four patients abandoned their job or worked under full-time supervision ≥ 12 months following ACoA aneurysm repair (unfavorable long-term outcome), presumably due to frontal dysfunction associated with amnesia. Conversely, the processing speed decreased in only one of five patients with subcallosal artery involvement alone; all five patients returned to work or continued working in different or downgraded jobs ≥ 12 months following ACoA aneurysm repair (favorable long-term outcome), although they had persistent amnesia.
A case of subcallosal artery plus RAH infarction with persistent amnesia with an unfavorable long-term outcome. A 58-year-old man had a ruptured aneurysm of the anterior communicating artery. Surgical clipping was performed on the day after onset. Neuropsychological examination four months after the aneurysm clipping confirmed mild amnesia (intelligence quotient (80) minus memory quotient (68) = 12, delayed recall < 50) and decreased frontal function (processing speed: 81, score below − 1 SD of the normative data). He changed his job and worked under full-time supervision ≥ 12 months following ACoA aneurysm repair (unfavorable long-term outcome). Neuropsychological examination for 15 months after the aneurysm clipping confirmed persistent amnesia (intelligence quotient (94) minus memory quotient (67) = 27, delayed recall < 50) and persistent mildly decreased frontal function (processing speed: 84, score below − 1 SD of the normative data). The diffusion-weighted imaging scan on the day after clipping demonstrates acute infarction in the column of the fornix (a, blue arrows), paraterminal gyrus (white arrow), anterior commissure (yellow arrow), and the rostrum and genu of the corpus callosum (a and b, black arrows) on both sides. Axial MPRAGE imaging (c) and sagittal multiplanar reconstruction images from T2-weighted VISTA imaging (d) four months after clipping show infarcted foci in the column of fornix (blue arrows), anterior commissure (yellow arrows), paraterminal gyrus (white arrows), subcallosal area (white arrows), and the rostrum and genu of the corpus callosum (black arrows) on both sides. Infarction in the nucleus accumbens representing RAH territory infarction is seen on the right (c, red arrow). The entire extent of the lesions shows sagittally elongated bandlike infarctions along the medial aspect of the brain, which probably represent the distribution of the characteristic S-shaped course of the subcallosal artery (d)
A case of subcallosal plus RAH infarction with persistent amnesia with an unfavorable long-term outcome. A 52-year-old man presented with a ruptured anterior communicating artery (ACoA) aneurysm. Surgical trapping of the ruptured ACoA aneurysm was performed on the day of onset. Neuropsychological examination 2 months after rupture confirmed amnesia (intelligence quotient (82) minus memory quotient (58) = 24 > 15: delayed recall < 50, 1 standard deviation [SD] = 15) and impairment of the frontal function (processing speed: 63, score below − 2 SD of the normative data). Even after 2 years postoperatively, he could not return to work as a manager; his family supervised his full-time work as a physical laborer, although he often did his job poorly or ceased halfway through (unfavorable long-term outcome). Neuropsychological examination for 3 years after the aneurysm clipping confirmed persistent amnesia (intelligence quotient (93) minus memory quotient (61) = 32 > 2SD, delayed recall < 50) and persistent impairment of frontal function (processing speed: 72, score below − 1 SD of the normative data). Axial T1-weighted (a) and T2-weighted (b) images and axial multiplanar reconstruction images from T2-weighted VISTA imaging (c and d) showing the infarcted foci involving the anteroinferior part of the caudate nucleus on the right side, which presumably represents involvement of the recurrent artery of Heubner (a, b, and c, white arrows) and the basal forebrain on both sides (a and b, black arrows). The anterior commissure (c, black arrow), paraterminal gyrus and subcallosal area (c, asterisks), column of the fornix (d, black arrows), and genu of the corpus callosum on both sides (d, white arrow) are infarcted, all of which presumably represent involvement of the unpaired subcallosal artery
Some amnesic patients often show persistent frontal dysfunction, including executive dysfunction and reduced processing speed, after ACoA aneurysm repair [7, 8]. In another study of patients who received ACoA aneurysm clipping, postoperative amnesia and frontal dysfunction or reduced processing speed developed in those who had infarcts in the caudate nucleus, presumably representing the RAH territory, and in the basal forebrain, presumably representing the subcallosal artery territory [9]. We suspect that the association between RAH territory infarction and subcallosal artery involvement could cause considerable frontal dysfunction due to impaired frontostriatal circuits in patients with postoperative amnesia, leading to a worsening of the patient’s long-term outcome or quality of life.
Perspectives
To clarify the clinical significance of such infarction patterns, further studies are needed that focus on a large number of consecutive patients treated surgically or interventionally for ACoA aneurysms. Formal neuropsychological examinations of the patients should be performed after the acute stage of illness, during which they show a state of confusion, disorientation, and intellectual disturbance. The long-term outcome should be evaluated. CT or two-dimensional thick-slice MR imaging, even diffusion-weighted, is likely to be insufficient to visualize small lesions [3]. We suggest that diffusion-weighted imaging should be used in the acute phase and 3D MR imaging in the chronic or stable phase.
Conclusion
The subcallosal artery, RAH, and a combination of the territories of these arteries are the three key infarction patterns following an operation for ACoA aneurysm. Postoperative amnesia is most likely caused by an infarction in the territory of the subcallosal artery, particularly in the column of the fornix. Infarction in the RAH territory alone is unlikely to cause significant amnesia. However, RAH territory infarction, when associated with a subcallosal artery infarction, can considerably worsen the long-term outcome or quality of life of patients with postoperative amnesia.
References
Mugikura S, Kikuchi H, Fujii T, Murata T, Takase K, Mori E, et al. MR imaging of subcallosal artery infarct causing amnesia after surgery for anterior communicating artery aneurysm. AJNR Am J Neuroradiol. 2014;35:2293–301.
Takahashi S, Goto K, Fukasawa H, Kawata Y, Uemura K, Suzuki K. Computed tomography of cerebral infarction along the distribution of the basal perforating arteries. Part I: Striate arterial group. Radiology. 1985;155:107–18.
Mugikura S, Takahashi S. Infarction in the pars libera of the column of fornix including pre (cholinergic)- and post (circuit of Papez fiber tracts)-commissural fibers causes “basal forebrain” amnesia. Neuroradiology. 2015;57:757.
Mizuta H, Motomura N. Memory dysfunction in caudate infarction caused by Heubner’s recurring artery occlusion. Brain Cogn. 2006;61:133–8.
Fukamachi A, Horikoshi T, Nagaseki Y, Sasaki H, Nukui H. Symmetrical bilateral low-density lesions in the areas of supply by Heubner’s arteries after aneurysm surgery. Acta Neurochir. 1987;84:89–92.
Kikuchi H. Long-term outcome of amnesic patients after surgery of anterior communicating artery aneurysm. Sendai: Tohoku University; 2014. http://hdl.handle.net/10097/58000.
Stenhouse LM, Knight RG, Longmore BE, Bishara SN. Long-term cognitive deficits in patients after surgery on aneurysms of the anterior communicating artery. J Neurol Neurosurg Psychiatry. 1991;54:909–14.
Ravnik J, Starovasnik B, Sesok S, Pirtosek Z, Svigelj V, Bunc G, et al. Long-term cognitive deficits in patients with good outcomes after aneurysmal subarachnoid hemorrhage from anterior communicating artery. Croat Med J. 2006;47:253–63.
Irle E, Wowra B, Kunert HJ, Hampl J, Kunze S. Memory disturbances following anterior communicating artery rupture. Ann Neurol. 1992;31:473–80.
Acknowledgements
This work was supported by JSPS KAKENHI grant number JP15K10290.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
All study participants provided informed consent, and the study design was exempt from ethics review board approval.
Conflict of interest
All authors declare that they have no competing interests.
About this article
Cite this article
Mugikura, S., Kikuchi, H., Fujimura, M. et al. Subcallosal and Heubner artery infarcts following surgical repair of an anterior communicating artery aneurysm: a causal relationship with postoperative amnesia and long-term outcome. Jpn J Radiol 36, 81–89 (2018). https://doi.org/10.1007/s11604-017-0703-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-017-0703-2