Abstract
The fornix is a part of the Papez circuit and associated with memory formation. Pure fornix infarction is a very rare type of stroke that causes symptoms such as transient global amnesia (TGA); however, the degree of memory impairment varies. The cause of fornix infarction is often unknown. A right-handed 51-year-old female patient with a current smoking habit and a history of hypertension experienced an acute onset of anterograde amnesia marked by repetitive questions; this episode, which persisted for 24 h, appeared to be TGA. Diffusion-weighted imaging showed acute bilateral fornix column infarction. Fast imaging employing steady-state acquisition (FIESTA) revealed that the subcallosal artery (ScA) was responsible for the fornix column infarction. The etiology of the stroke remained indeterminable despite the comprehensive stroke workup; hence, this case was classified as an embolic stroke of undetermined source. ScA is the perforating branch from the anterior communicating artery. In general, minute perforating branches are not detected by ordinary MRI; however, FIESTA may be useful to detect the ScA. In the present case, FIESTA showed a relatively large ScA, potentially indicating a microembolic etiology. Although we evaluated our patient’s embolic source, it remained indeterminable. Acute amnesic symptoms occasionally occur due to bilateral fornix column infarction, and the resulting memory dysfunction sometimes persists. FIESTA may be useful for imaging the ScA to identify the etiology of stroke.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stroke is an emergency disease that should not be overlooked; however, it may not be a typical symptom, such as paralysis or speech impairment. The fornix is a part of the Papez circuit and is associated with memory formation. Pure fornix infarction is a very rare type of stroke that causes symptoms such as transient global amnesia (TGA); however, the degree of memory impairment varies. The cause of fornix infarction is often unknown because the subcallosal artery (ScA), responsible for fornix column infarction, is difficult to detect in the usual sequences of magnetic resonance imaging applied in acute stroke settings. Here, we report the case of a patient with bilateral fornix column infarction who experienced what appeared to be acute amnesic symptoms. Unlike usual TGA symptoms, her memory dysfunction persisted for 9 months after stroke onset. In this case, fast imaging employing steady-state acquisition (FIESTA) revealed a relatively large ScA. We speculate that the etiology of stroke is microembolic stroke, not small vessel occlusion, according to the size and shape of the ScA.
Case Report
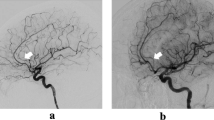
A right-handed 51-year-old female patient with a current smoking habit and a history of hypertension experienced an acute onset of anterograde amnesia marked by repetitive questions; this episode, which persisted for 24 h, appeared to be transient global amnesia (TGA). Four days after her symptoms arose, she visited the department of neurosurgery at another hospital. Diffusion-weighted imaging (DWI) showed acute bilateral fornix column infarction, and magnetic resonance angiography (MRA) showed no stenotic or occluded sites on the main trunks of the cerebral arteries (Fig. 1A, B). Two months after stroke, she was referred to our department without specific treatment, such as antithrombotic agents, and admitted for diagnostic workup to ascertain the etiology of the stroke. On admission, her neurological examination was normal except for tests of memory function. She scored 28 of 30 (delayed recall -2) on the Mini-Mental State Examination. The Wechsler Memory Scale-Revised (WMS-R) showed memory loss, including a remarkable reduction in delayed recall (Verbal Memory 72, Visual Memory 77, General Memory 69, Attention/Concentration 100, Delayed Recall less than 50). Blood tests related to anti-phospholipid antibody syndrome, collagen disease, and coagulation disorders were unremarkable. As time passes from the onset of stroke, MRI (T2-weighted image) cannot detect fornix column infarction (Fig. 1D), and FIESTA revealed that the ScA arose from the anterior communicating artery toward the back upward area. This artery was responsible for the infarction in the fornix column (Fig. 2A, B1, and B2). The etiology of the stroke remained indeterminable despite the comprehensive stroke workup, including transthoracic echocardiography, carotid sonography, Holter electrocardiography, and transesophageal echocardiography. This case was classified as an embolic stroke of undetermined source, and we selected aspirin for secondary stroke prevention. Nine months after stroke, the WMS-R showed remaining memory loss and a reduction in delayed recall (verbal memory 62, visual memory 85, general memory 64, attention/concentration 113, delayed recall less than 50). The patient is not in a condition necessitating outpatient language rehabilitation for her memory impairment, and she maintains independence in her daily life with some assistance from her family.
Diffusion-weighted imaging showed high signal intensity, and the apparent diffusion coefficient map showed low signal intensity in the bilateral fornix columns (A, B red arrow). Magnetic resonance angiography showed no stenotic or occluded sites on the main trunks of the cerebral arteries (C). Two months after stroke, T2-weighted imaging could not detect fornix column infarction (D)
Discussion
The Papez circuit, comprising connections among the hippocampus, fornix, mammillary body, mammillothalamic tracts, anterior thalamic nucleus, and cingulate gyrus, is important for episodic memory [1]. Acute amnestic symptoms occur with lesions of the Papez circuit, which are typically associated with damage to the medial temporal lobe, especially the hippocampus. Any infarction that compromises the Papez circuit will cause acute amnesia; however, pure fornix infarction is a very rare type of stroke 2. Bilateral fornix column infarction in particular causes severe anterograde and mild retrograde amnesia and various other forms of memory impairment. A review of 12 cases of isolated, noniatrogenic bilateral fornix column infarction is shown in Table 1 [2,3,4,5,6,7,8,9,10]. Almost all cases showed anterograde amnesia with clinical outcomes varying from case to case. In the present case, memory dysfunction persisted at 9 months after stroke onset. Although imaging in the chronic phase alone cannot pinpoint abnormalities, it is important to perform appropriate imaging studies in the acute phase to diagnose fornix infarction when a patient with memory impairment presents to the hospital.
According to a study by Dan Meila, the fornix column is in the territory of the ScA, the perforating branch from the anterior communicating artery (ACoA), and has multiple variants. The ScA is usually a single vessel and is typically the largest of the arteries arising from the ACoA [11]. The diameter of the ScA is 0.2–1.0 mm (average 0.67 mm), and its course is classified into three groups using 7-Tesla MRI: C-shaped (most common), straight, and S-shaped [12]. In the present case, the course of the ScA was visually classified as C-shaped on the basis of FIESTA via 3-Tesla MRI. In general, minute perforating branches are not detected by ordinary MRI; however, FIESTA may be useful for detecting the ScA, as in the present case. FIESTA can be performed with 3-Tesla MRI rather than 7-Tesla; FIESTA is also noninvasive, unlike digital subtraction angiography, and can be performed at almost any facility. FIESTA is a type of heavily T2-weighted image and is a useful technique for confirming the location of cranial nerves and small vessels. It offers excellent visualization of blood vessels and their anatomical details. The cause of isolated bilateral fornix column infarction is often difficult to identify in noniatrogenic cases [7, 9, 10]. In the present case, FIESTA showed a C-shaped and relatively large ScA, which might indicate a microembolic etiology. On C-shaped ScA, the bend from the mother vessel was small, and the thrombus might easily flow along the bloodstream, leading to the consideration of microembolic etiology. It was suspected that microemboli from upstream were flowing downstream of the artery and causing an occlusion, considering the shape or size of the vessel, and that the etiology was not lipohyalinosis or atheromatic changes. However, one of the limitations of this speculation is that we could not evaluate the current vascular flow of ScA using digital subtraction angiography because the patient declined to consent to the examination due to concerns about the risks of complications. In addition, we evaluated our patient’s embolic source, which remained indeterminable. We continue to undertake careful clinical management of this patient to detect any paroxysmal atrial fibrillation.
Conclusion
Acute amnesic symptoms occasionally occur as a result of bilateral fornix column infarction, and the resulting memory dysfunction sometimes persists. FIESTA may be useful for imaging the ScA to identify the etiology of stroke.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Papez JW. A proposed mechanism of emotion. J Neuropsychiatry Clin Neurosci. 1995;7(1):103–12. https://doi.org/10.1176/jnp.7.1.103.
Adamovich BL, Gualberto G, Roberts T, et al. Teaching NeuroImages: amnesia due to fornix infarction. Neurology. 2009;73(17): e86. https://doi.org/10.1212/WNL.0b013e3181bd80af.
Murr N, Thaisetthawatkul P, Helvey J, et al. Selective infarction of the anterior genu fornices associated with giant cell arteritis. J Stroke Cerebrovasc Dis. 2012;21(4):327–9. https://doi.org/10.1016/j.jstrokecerebrovasdis.2010.08.006.
Rizek P, Pasternak S, Leung A, et al. Acute-onset anterograde amnesia caused by isolated bilateral fornix infarction. Can J Neurol Sci. 2013;40(5):738–9. https://doi.org/10.1017/s0317167100015031.
Zhu QY, Zhu HC, Song CR. Acute amnesia associated with damaged fiber tracts following anterior fornix infarction. Neurology. 2018;90(15):706–7. https://doi.org/10.1212/WNL.0000000000005306.
Wang J, Ke J, Zhou C, et al. Amnesia due to the injury of Papez circuit following isolated fornix column infarction. J Stroke Cerebrovasc Dis. 2018;27(5):1431–3. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.12.040.
Salvalaggio A, Cagnin A, Nardetto L, et al. Acute amnestic syndrome in isolated bilateral fornix stroke. Eur J Neurol. 2018;25(5):787–9. https://doi.org/10.1111/ene.13592.
Ren C, Yuan J, Tong S, et al. Memory impairment due to a small acute infarction of the columns of the fornix. J Stroke Cerebrovasc Dis. 2018;27(7):e138–43. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.02.039.
Takano Y, Tatewaki Y, Mutoh T, et al. Isolated fornix infarction with damage to the limbic system as a cause of persistent amnesia: a case report. Am J Case Rep. 2018;19:1382–5. https://doi.org/10.12659/AJCR.912508.
Cho MJ, Shin DI, Han MK, et al. Acute amnesia during pregnancy due to bilateral fornix infarction: a case report. World J Clin Cases. 2020;8(19):4494–8. https://doi.org/10.12998/wjcc.v8.i19.4494.
Meila D, Saliou G, Krings T. Subcallosal artery stroke: infarction of the fornix and the genu of the corpus callosum. The importance of the anterior communicating artery complex. Case series and review of the literature. Neuroradiology. 2015;57(1):41–7. https://doi.org/10.1007/s00234-014-1438-8.
Matsushige T, Chen B, Dammann P, et al. Microanatomy of the subcallosal artery: an in-vivo 7 T magnetic resonance angiography study. Eur Radiol. 2016;26(9):2908–14. https://doi.org/10.1007/s00330-015-4117-1.
Funding
This study was supported by a research grant from the Japan Society for the Promotion of Science KAKENHI (Grant Number 20K16579).
Author information
Authors and Affiliations
Contributions
TA, attending physician: drafted and revised the manuscript for intellectual content.
TN, attending physician: drafted and revised the manuscript for intellectual content.
SA: revised the manuscript for intellectual content.
HM: revised the manuscript for intellectual content.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying data.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abe, T., Nezu, T., Aoki, S. et al. Acute Amnesic Symptoms Due to Bilateral Fornix Column Infarction: a Case Report. SN Compr. Clin. Med. 5, 238 (2023). https://doi.org/10.1007/s42399-023-01579-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01579-w