Abstract
Purpose
Coronary artery segmentation in coronary computed tomography angiography (CTA) images plays a crucial role in diagnosing cardiovascular diseases. However, due to the complexity of coronary CTA images and coronary structure, it is difficult to automatically segment coronary arteries accurately and efficiently from numerous coronary CTA images.
Method
In this study, an automatic method based on symmetrical radiation filter (SRF) and D-means is presented. The SRF, which is applied to the three orthogonal planes, is designed to filter the suspicious vessel tissue according to the features of gradient changes on vascular boundaries to segment coronary arteries accurately and reduce computational cost. Additionally, the D-means local clustering is proposed to be embedded into vessel segmentation to eliminate noise impact in coronary CTA images.
Results
The results of the proposed method were compared against the manual delineations in 210 coronary CTA data sets. The average values of true positive, false positive, Jaccard measure, and Dice coefficient were \( 0.9541\pm 0.0651 \), \( 0.0812\pm 0.1024 \), \( 0.8894\pm 0.1214 \), and \( 0.9318\pm 0.0833 \), respectively. Moreover, comparing the delineated data sets and public data sets showed that the proposed method is better than the related methods.
Conclusion
The experimental results indicate that the proposed method can perform complete, robust, and accurate segmentation of coronary arteries with low computational cost. Therefore, the proposed method is proven effective in vessel segmentation of coronary CTA images without extensive training data and can meet clinical applications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease is the most common type of cardiovascular disease. If a coronary artery becomes narrowed or occluded due to plaque build-up, a decrease in blood flowing to the myocardium may cause ischemia, leading to fatal consequences [1]. In recent years, coronary computed tomography angiography (CTA) images have become critical for cardiovascular disease filtering, diagnosis, and treatment. However, it is difficult and time-consuming for clinicians to track and analyze coronary arteries manually. Therefore, the accurate and automatic segmentation of coronary arteries in CTA images has an important practical significance and clinical value [2]. The state-of-the-art methods for the segmentation of coronary arteries can be divided into the following categories [3, 4].
Models that correspond to the prior assumption are applied to the target vessels, such as a vascular model, a geometric model, a hybrid model, and a specific model. Boskamp et al. [5] designed a series of procedures to segment vessels according to vessel intensity distributions and morphology features, but it is sensitive to the noise of the image. To address those problems, many scholars proposed geometric models to detect vessel boundaries. Huang et al. [6] designed a method for accurate vessel segmentation based on the cylinder model. Although the geometric model can naturally deal with topological structure changes, it is low efficient and sensitive to noise. Therefore, various hybrid models have been proposed to segment vessels. A hybrid model-based method was proposed to simulate the generation of the vascular tree by using constraint construction optimization and flow-related geometric constraints [7]. Except for normal vessels, vessel bifurcations and abnormal vessels will increase the difficulties of vessel segmentation. Thus, a specific vascular model was designed for specific vascular shapes [8].
Features based on vessel measures estimate the models in CTA images, which can be image features, structural features, and feature transformations. An intensity-based multi-level classification model was proposed to extract features. Zhuang et al. [9] proposed an improved super-pixel generation algorithm that incorporates both gray-level and luminosity-based information to improve simple linear iterative clustering algorithms. A popular method in detecting vessels is to use the second-derivative information to characterize the geometric shape of local images, such as Hessian matrix transformation (HMT) [10]. Ge et al. [11] proposed a two-step segmentation algorithm based on Hessian matrix and level set using Hessian matrix eigenvalues, feature vectors, and evolution of a level set function.
Either the model-based or feature-based methods require a suitable vascular segmentation scheme to achieve good segmentation results. Generally, a strategy of vascular segmentation is: first, pre-processing or pre-segmenting target images [12]; second, using a region-growing based method, an active contour model method, and a centerline tracking-based method to extract vessels and obtain the boundaries [13, 14]; finally, adopting a post-processing strategy to extract complete target vessels [3]. Du et al. [15] proposed a new segmentation framework for 3D coronary artery tress by integrating noise reduction, candidate region detection, geometric feature extraction, and coronary artery tracking techniques.
A deep learning-based method has been widely used in vascular segmentation in recent years. In contrast to traditional methods, it does not need to design models, features, or segmentation schemes [4, 16]. Gu et al. [17] proposed a global feature embedded network (GFE-Net) for coronary arteries segmentation in CTA images. The GFE-Net improves V-Net uses a noisy activating function to suppress CTA image noise during the network down-sampling process. Shen et al. [18] proposed a 3D fully convolutional network (FCN) integrating an attention gate for coarse segmentation of coronary arteries. The coarse segmentation is then optimized using the level set function to obtain a refined, smooth segmentation. Although the deep learning-based method has made some achievements in vascular segmentation, its application in vascular segmentation of coronary CTA images still presents great challenges [19, 20].
In this paper, we propose an automatic method for coronary artery segmentation. The main contributions are summarized as follows:
-
1.
We design a two-dimensional (2D) symmetrical radiation filter (SRF) which is applied to the tissue on three orthogonal planes (the axial, coronal, and sagittal planes) rather than a cross-sectional plane.
-
2.
We propose a D-means local clustering segmentation scheme that performs iterative local calculations on vascular tissue to avoid the influence of cardiac motion artifacts and unsteadiness of the contrast agent concentration.
-
3.
The proposed method has low complexity, low computational cost, a broad clinical application, and a low hardware requirement, which can fully meet the need of clinicians.
Method
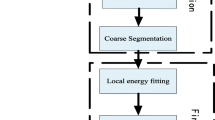
The framework of the leading segmentation procedures is depicted in Fig. 1. The proposed method has two new algorithms: the SRF used to filter the suspicious vessel regions and the D-means local clustering used to eliminate the impact of noise in coronary CTA images. Firstly, we describe the SRF-based vessel filtering method in “Vessel filtering” section, including the theory and application. Then, we describe the vessel segmentation method in “Vessel segmentation” section, including the use of SRF and D-means local clustering.
Framework of vessel filtering and segmentation of coronary CTA images. In the D-means local clustering stage, each step is composed of four views: axial view on the top left, sagittal view on the top right, VR view on the bottom left, and coronal view on the bottom right. At the image patch step, the non-coronary artery tissue marked in green is removed by the SRF; at the D-means clustering step, multicolored tissue is used to display the D-means clustering results
Vessel filtering
Theory of SRF
SRF is a vessel filter used to remove non-vessel tissue by calculating an intensity value of symmetrical vascular gradient and judging whether it meets a filtering threshold of gradient symmetry of vessels. Figure 2 depicts the SRF method.
Suppose that a point \( {x_0} \) in a vessel on a 2D plane emits ray pairs to the surroundings in a range of maximum distance \( D_{\max } \) and \(\pi \) angles. The ray pairs \(\pm u(\alpha )\) are two rays emitted from a point \( {x_0} \) in opposite directions. As well known, in coronary CTA images, vessels are brighter than the surrounding structures. The maximum gradient value will be at the inner and outer vessel boundary. Therefore, the vessel boundary should be detected first. b(x) denotes a boundary measure with a sign along a ray \( u(\alpha ) \) at a point x, defined as follows:
where I(x) denotes one-dimensional intensity distribution, and \({{\nabla }_{\sigma }}I(x)\) denotes a gradient of the point x. \(\sigma \) denotes a spatial scale of the vessel boundary determined according to a thickness of a vessel wall, set to 1.5mm. Considering the direction of the gradient, \( sign\left( {{\nabla }_{\sigma }}I(x) \right) \) is used to distinguish whether the change of vascular boundary is rising (from dark to bright) or falling (from bright to dark) [12]. The change from the inner to the outer vessel must present from bright to dark. Points inside the vessel are surrounded by falling boundaries except for two conditions: One is points outside the vessels are surrounded by bright tissue-like vessels and ventricles; the other is points belong to abnormal substances like calcified plaques and metal stents.
Polar coordinates used to illustrate the SRF. a The polar coordinates for any three points a, b, and c in the vessel used to illustrate the SRF. b The polar coordinates for point a in the vessel and points b, c in the right ventricle used to illustrate the SRF. The first column shows local axial planes of coronary CTA images. The red, green, and blue curves represent the maximum falling edge responses of a, b, and c points in each direction, respectively. The yellow circle represents the minimum threshold of the maximum falling edge responses
Since SRF is designed based on the gradient symmetry of vessels, the maximum falling edge response \( E\left( {{x}_{0}},u(\alpha ) \right) \) should be searched at the different locations x in a step size of 0.6mm along the ray \( u(\alpha ) \) within the maximum distance \( D_{\max } \). The step size is set according to the vessel diameter and the average physical size of coronary CTA images. The definition of function \( E\left( {{x}_{0}},u(\alpha ) \right) \) is given by:
where \( u(\alpha )=\sin (\alpha ){{u}_{1}}+\cos (\alpha ){u_2} \), and \({{u}_{1}}\) and \({{u}_{2}}\) are two directions of the 2D plane. \(\alpha \), \(\alpha \in \left[ 0,\pi \right) \), denotes an angle of the ray. The maximum distance \( D_{\max } \) is set to 8mm, which only needs to exceed the maximum vessel diameter according to the vascular physiology structure. For the ray pairs \(\pm u(\alpha )\), there are two maximum falling edge responses \( E\left( {{x}_{0}}, u(\alpha ) \right) \) and \( E\left( {{x}_{0}},-u(\alpha ) \right) \). When the two maximum falling edge responses both satisfy conditions, the ray pairs have gradient symmetry. Thus, the gradient symmetry function \( B\left( {{x}_{0}},\pm u(\alpha ) \right) \) is given by:
where \( {T_1} \) denotes a minimum threshold of the maximum falling edge responses, set to 70. The binary function P is equal to 1 when the expression condition inside the function is evaluated to be satisfied. Otherwise, it is equal to 0.
On a 2D plane, there are N ray pairs, set to 20 according to the size of coronary arteries and CTA images. Thus, the definition of the SRF function is given by:
where \({T_2}\) denotes a minimum threshold of a proportion of ray pairs that satisfy the gradient symmetry, set to 0.65. When the proportion of the ray pairs emitted from the point \( {x_0} \) to satisfy the gradient symmetry function \( B({{x}_{0}},\pm u(\frac{\pi i}{N})) \) is greater than the threshold \({T_2}\), the point \( {x_0} \) belongs to the vessels. The fixed parameters related to SRF are obtained by statistical methods, such as receiver operating characteristic (ROC) curves and histogram analysis.
2D planes and polar coordinates used to illustrate the SRF. The first column depicts the cross-sectional planes of the points obtained based on HMT and their corresponding polar coordinates. The second to the fourth columns depict the axial, coronal, and sagittal planes of the points and their corresponding polar coordinates. The red curve represents the maximum falling edge responses of the red point. The yellow circle represents the minimum threshold of the maximum falling edge responses. The points in a and b are in vessels. The point in c is not in the vessel
SRF is designed according to the feature of the descending boundary from the inner to the outer vessel on the 2D plane. Unlike the filter designed in the literature [12], SRF does not require the calculated point to be the center point of the vessel. As shown in Fig. 3a, as long as the points (like points a, b, and c) are in the vessel, their gradient of SRF is similar, and all have symmetry features of gradient change. Nevertheless, if the points are not in the vessel, they will not be similar and not have the symmetry feature like points b and c depicted in Fig. 3b.
Application of SRF
Compared with the state-of-the-art 3D vessel filter [21, 22], SRF is a 2D vessel filter designed based on the gradient symmetry of vessels on a 2D oblique plane, which is used to reduce the computational cost for clinical application. Generally, a 2D vessel filer is applied to a cross-sectional plane obtained based on the HMT, like the method used in the literature [12]. HMT is time-consuming and often inaccurate for week vessels [21, 22]. As we can observe from Fig. 4, whether in vascular or non-vascular cross-sectional planes, points have strong gradient symmetry (the first column of Fig. 4a and c). Even using multi-scales, the HMT has a deviation (the first column of Fig. 4b). However, the three orthogonal planes can effectively distinguish inside points (the second to fourth columns of Fig. 4a and b) from the outside points (the second to the fourth columns of Fig. 4c).
Taking the feature of SRF and coronary CTA images into account, we integrated SRF values from three orthogonal planes (axial, coronal, and sagittal planes) into one judgment to replace a judgment of SRF values from one cross-sectional plane. When two or more 2D orthogonal planes meet the intensity value, the point is considered to satisfy the gradient symmetry and belongs to vessels.
Vessel segmentation
In this paper, we integrate the designed SRF-based vessel filtering and D-means local clustering into coronary artery segmentation (as depicted in Fig. 1). Firstly, the initial seed points are obtained by state-of-the-art algorithms with the SRF to further ensure the initial seed points are effective for subsequent iterations of vessel segmentation. Secondly, the D-means local clustering is integrated into the iterative process to obtain image patches used to update vessel segmentation parameters. During each iteration, the SRF is used again to ensure that the image patches belong to the coronary arteries. Finally, the vessel segmentation is done when all the initial seed points and image patches are completed.
Initial seed points
The initial seed points that are generally starting points for region segmentation can be obtained in many ways, such as the methods described in the literature [10, 23, 24]. The initial seed points are coarse in this paper, i.e., only at least two effective seed points in each main coronary tree are enough, and numerous seed points and false seed points are tolerated. Therefore, to reduce the computational cost, two coarse thresholds, set to 130 Hounsfield units (HU) and 500 HU, are firstly used to extract a region of interest (ROI) for the initial seed points. Secondly, a Hessian matrix with a single scale determined by the average radius of coronary arteries and a tubular structure similarity function is adopted to get suspicious seed points with robust tubular structure features. Finally, the effective seed points are obtained by SRF.
D-means local clustering
Vessels in CT images appear unstable changes such as large changes in CT values, dislocation of coronary arteries, and blurry artifacts in coronary CTA images. Only in a small range of regions, the features are similar. Thus, the D-means local clustering algorithm is critical in the iterative segmentation process. It can divide a large region into multiple localized small image patches so that these small image patches can update the parameters required for the next iteration segmentation.
There are many state-of-the-art clustering algorithms such as K-means [25], K-medoids [26], density-based spatial clustering of applications with noise (DBSCAN) [27], and hierarchical clustering [28]. The D-means local clustering is the evolution of K-means and DBSCAN, which makes the distance between all target points in the clustering domain and the clustering center meet the defined conditions. Moreover, there is no need to specify the number of clusters before clustering.
Let us assume a data set X composed of m voxels from a region V. The process of the D-means clustering algorithm is to divide the data set X into N clusters \( {{C}_{i}} \) according to a distance D as defined in the following equation:
where \( {x}_{ij} \) is a voxel of the region V. D is set 4mm according to the maximum radius of the coronary artery. Each cluster \({{C}_{i}}\) has a cluster center \({{\mu }_{i}}\) defined as follows:
where \({{C}_{i}}\) is defined as:
the distance \( d({{x}_{ij}},{{\mu }_{i}}) \) is defined as follows:
By selecting Euclidean distance as the criterion of similarity and distance, the number of clusters N whose distance d from each point \({{x}_{ij}}\) to the cluster center \({{\mu }_{i}}\) is less than or equal to D is calculated. Figure 5 depicts the process of dividing a dataset X into three predefined clusters.
Segmentation procedures
Vessel segmentation is an iterative process. During the iterative process, the image patches are grown coarsely by two thresholds \({\text {Thre}}_{\text {low}}\) and \({\text {Thre}}_{\text {high}}\). \({\text {Thre}}_{\text {low}}\) and \({\text {Thre}}_{\text {high}}\) denote a low CT value threshold and a high CT value threshold, respectively. They are constantly updated during the growth of each image patches, which are defined by CT mean \( {\text {Mean}}_{\text {CT}} \) and standard deviation \({\text {SD}}_{\text {CT}}\) as follows:
where \( {\text {Mean}}_{\text {CT}} \) and \({\text {SD}}_{\text {CT}}\) denote CT value mean and standard deviation, respectively. They are calculated by the last image patches. For the first image patch, they are calculated by the 26 neighborhoods of the initial seed points. The image patch IP is defined as follows:
where \( {x}_{\text {CT}} \) denotes the CT value at x. The image patch IP will contain many false points which need to be removed. Thus, the SRF is applied to ensure that the reserved image patch RIP given by (11) is coronary arteries (see the “Vessel filtering” section).
where SRFV denotes a set of points that satisfies the condition of SRF. As described in “D-means local clustering” section, the image patch RIP should be clustered to ensure that the two thresholds \({\text {Thre}}_{\text {low}}\) and \({\text {Thre}}_{\text {high}}\) used for the next iterative segmentation are accurate. Thus, the D-means local clustering algorithm is used to get the regional cluster sets \( {C_N} \):
The cluster \({C}_{i}\) is the input image patch for the next iteration. When all seed points and image patches are completed, the segmentation is done.
Results
Materials
The proposed method was implemented in Visual Studio software (C/C++) and MATLAB software and executed on a desktop computer equipped with an Intel(R) Core (TM) i5-4590 HQ processor (3.30 GHz) and 16 GB of RAM.
Since there are no public data sets used for testing and verification in coronary artery segmentation, we randomly collected a total of 210 data sets of coronary CTA images from different manufacturers (GE, Philips, and Siemens), different equipment, and different hospitals. The average voxel size of images is 512 \( \times \) 512 \( \times \) 291 with an average physical size of 0.40 mm \( \times \) 0.40 mm \( \times \) 0.47 mm. There are 120 healthy data sets and 90 diseased data sets, of which 50 are significant stenosis (\( \geqslant 50\% \) luminal narrowing).
The manual delineation is time-consuming and energy-consuming because of the complex coronary artery structure, inconsistent image quality, and different expert requirements for coronary artery segmentation. Therefore, three senior cardiovascular experts have manually delineated the data based on the results of the proposed method by adding the missing coronary arteries and removing non-coronary arteries.
Examples of VR images of coronary artery segmentation results a, b. Red and green regions are the segmentation results of the proposed method, and especially green regions are the non-coronary artery tissue removed by experts. Blue regions are missing coronary artery tissue added by experts. Each row compares the segmented results of the proposed method and the manual delineations of experts 1, 2, and 3, respectively
Evaluation metrics
The results were compared with those manually delineated by experts to evaluate the accuracy of the segmentation results. Four metrics are used to evaluate the performance of the coronary artery segmentation methods: true positive (13), false positive (14), Jaccard measure (15), Dice coefficient (16):
where \({{S}_{{\text {auto}}}}\) and \({{S}_{{\text {label}}}}\) denote the coronary artery region obtained by automatic segmentation and manual delineation, respectively.
Performance
The examples of the segmentation results and corresponding manual delineations are shown in Fig. 6. We can observe from Fig. 6 that the segmented results in this paper are highly consistent with the tissue manually delineated by three experts. For some undersegmented tissue, the manual delineations vary considerably.
Figure 7 shows box plots of the four metrics obtained after quantitative evaluation of the segmented results and the results manually delineated by experts. We can observe from Fig. 7 that the results obtained by the proposed method are consistent with the results manually delineated by experts. Compared with the three experts, the mean medians of TP, FP, JM, and DC are 0.9837, 0.0258, 0.9558, and 0.9875, respectively.
We also evaluated the segmented results of diseased data and healthy data in the data sets separately. The mean value and standard deviation of four metrics are shown in Table 1. From Table 1, we can observe that the proposed method has good performance on the healthy data sets as well as the diseased data sets.
To illustrate the segmentation error of the proposed method, we compared the error between each of the manual delineations. The mean value and standard deviation of four metrics were calculated between the manual delineation results of two experts in Table 2. Table 3 shows the mean value and standard deviation of four metrics of our proposed method compared with the manual delineation results. From the results, we can observe that the error between each of the manual delineations is close to the results of the proposed method.
Although there are no public gold standard data sets for evaluating coronary artery segmentation, the 3D Cardiovascular Imaging: a MICCAI (Medical Image Computing and Computer-Assisted Intervention) segmentation challenge workshop held in 2012 provides a framework for stenosis detection and evaluation. This evaluation framework provides 48 sets of CTA images, including 18 training sets and 30 test sets. \( 26\% \) and \( 32\% \) of the lesions are significant (\( \geqslant 50\% \) luminal narrowing) for training and test datasets, respectively [29]. The evaluation method uses the common delineation of three observers as the gold standard. Since the framework has been closed, we can only evaluate 18 training sets with the ground truth. The experimental results are shown in Table 4.
As deep learning has been widely used in segmentation and has achieved significant results, the proposed method was also compared with deep learning-based methods [17, 18]. The architectures are described in the fifth paragraph of the introduction section. According to the literature [17], the learning rate, optimizer, and number of epochs are \(1\times {10}^{-4}\), Adam, and 200, respectively. According to the literature [18], the learning rate, optimizer, and number of epochs are \(1\times {10}^{-5}\), Adam, and 500, respectively. The common manual delineations are used as ground truth to test 210 data sets. According to the general requirements of deep learning, 147 data sets were selected as the training sets, while 32 data sets were selected as the validation sets, and the others were used as the test sets. The experimental results are shown in Table 5.
The computational cost of the critical processes of the proposed method besides the HMT method was carried out on the 210 data sets (see Table 6). The most time-consuming procedure is obtaining the initial seed point, which accounts for \( 62.89\% \) of the total time, whereas the SRF and local clustering segmentation account for \(13.80\% \) and \( 15.91\% \), respectively. The execution time using the HMT to acquire cross-sectional planes is 5.27 times the total computational cost of the proposed method, which is indicated in the last column of Table 6.
Discussion
The proposed method has been tested on 210 randomly obtained data sets, and the results are promising. We can observe from Fig. 6 that the results are consistent with the manual delineations, which can fully include the left and right coronary arteries as well as branches. Although there may be local oversegmentation, they do not affect the overall structure of the coronary arteries. There may also be local undersegmentation mainly focused on the end of coronary arteries, but the manual delineations also have some disputes. As we can observe from the box plots of four metrics of segmentation results depicted in Fig. 7, the segmentation results have good clustering properties. The mean median of TP is 0.9837, which indicates that the results are relatively complete with less undersegmentation. The mean median of FP is 0.0258, which indicates that the error of oversegmentation is also within a small range.
To prove the segmentation error and clinical application, we conducted a comparative experiment, which results means that the proposed method is very close to the error of the manual delineations (see Table 2 and Table 3) and can fully meet clinical use. Furthermore, the proposed method was also tested and evaluated on the diseased and healthy data sets, respectively. The experimental results (see Table 1 and Table 4) are close to the results of the three observers, which means the proposed method has good adaptability to diseased data and can not be interfered with various factors such as calcified plaques, lipid plaques, hybrid plaques, and stents. For the healthy data, the segmented results are better than the diseased data, but there are still some poor segmented results. Although the healthy data are not affected by lesions, they are still easily affected by other factors, such as machine artifacts, motion artifacts, and unsteadiness of the contrast agent concentration, which result in poor image quality and seriously affect the segmented results.
We also compared our results with the related methods based on deep learning found in the literature. The experimental results (see Table 5) showed that our method is better than theirs. Although the methods based on deep learning have been widely used in vessel segmentation and have achieved good results, coronary artery segmentation in coronary CTA images is still not well. Since the coronary arteries are small with various shapes and lesions, they can be affected by various kinds of noise and imaging factors. In addition, coronary artery segmentation based on deep learning needs numerous training data to have good adaptability and generalization. However, it is difficult for us to obtain numerous training data in practice, which can lead to poor results.
In terms of the computational cost, the average total time of the proposed method to process each of the 210 data sets was \( 3.5420\pm 0.9377 \)s, which can fully meet the clinical application.
The proposed method has achieved good results in coronary artery segmentation and can meet the clinical application. However, there are still two limitations.
-
1.
The initialization of parameters. Although the proposed method with the various parameters adopted in this paper can segment the coronary artery, a fully automatic segmentation without any empirical parameters increases the reliability and robustness of the method for abnormal data. Hence, future studies will be conducted to segment coronary arteries effectively without any empirical parameters.
-
2.
The initial seed points. Obtaining the initial seed points causes a high computational cost. Comparing the advantages and disadvantages of deep learning to the small number of data sets, we plan to combine the two methods in future work to reduce computing time and post-processing procedures.
Conclusion
In this study, a fully automatic method based on SRF and D-means local clustering for the segmentation of coronary CTA images is presented. The SRF is used to filter the vessel region to address the problem of segmentation caused by noise, artifacts, and non-coronary regions in the coronary CTA images. Furthermore, using the local clustering segmentation algorithm based on D-means can address the problem of large changes in CT values, dislocation of coronary arteries, and blurry artifacts in coronary CTA images, to quickly, stably, efficiently, and effectively segment the coronary artery. The experimental results of the quantitative analysis showed that the segmentation results of the proposed method are consistent with the three manual delineations within the error range, which also fit abnormal data and can meet the clinical applications.
References
Miller CL, Kontorovich AR, Hao K, Ma L, Iyegbe C, Björkegren JL, Kovacic JC (2021) Precision medicine approaches to vascular disease: Jacc focus seminar 2/5. J Am Coll Cardiol 77(20):2531–2550
Sharim J, Budoff M (2021) Efficacy of coronary computed tomography angiography in assessing regression of coronary artery disease. J Am Coll Cardiol 77(18):1283
Lesage D, Angelini ED, Bloch I, Funka-Lea G (2009) A review of 3d vessel lumen segmentation techniques: Models, features and extraction schemes. Med Image Anal 13(6):819–845
Li S, Kong X, Lu C, Zhu J, He X, Fu R (2021) Gca-net: global context attention network for intestinal wall vascular segmentation. Int J Comput Assist Radiol Surg 1–10
Boskamp T, Rinck D, Link F, Kummerlen B, Stamm G, Mildenberger P (2004) New vessel analysis tool for morphometric quantification and visualization of vessels in ct and mr imaging data sets. Radiographics 24(1):287–297
Huang X (2021) Intelligent algorithms-based ct image segmentation in patients with cardiovascular diseases and realization of visualization algorithms. Sci Program
Jaquet C, Najman L, Talbot H, Grady L, Schaap M, Spain B, Kim HJ, Vignon-Clementel I, Taylor CA (2019) Generation of patient-specific cardiac vascular networks: a hybrid image-based and synthetic geometric model. IEEE Trans Biomed Eng 66(4):946–955
Hammouche A, Cloutier G, Tardif JC, Hammouche K, Meunier J (2019) Automatic ivus lumen segmentation using a 3d adaptive helix model. Comput Biol Med 107:58–72
Zhuang S, Li F, Raj ANJ, Ding W, Zhou W, Zhuang Z (2021) Automatic segmentation for ultrasound image of carotid intimal-media based on improved superpixel generation algorithm and fractal theory. Comput Methods Programs Biomed 205:106084
Frangi AF, Niessen WJ, Vincken KL, Viergever MA (1998) Multiscale vessel enhancement filtering. In: International conference on medical image computing and computer-assisted intervention, Springer, pp 130–137
Ge S, Shi Z, Peng G, Zhu Z (2019) Two-steps coronary artery segmentation algorithm based on improved level set model in combination with weighted shape-prior constraints. J Med Syst 43(7):1–10
Gülsün MA, Tek H (2008) Robust vessel tree modeling. In: International conference on medical image computing and computer-assisted intervention. Springer, pp 602–611
Wang C, Moreno R, Smedby Ö (2012) Vessel segmentation using implicit model-guided level sets. In: MICCAI Workshop“3D cardiovascular imaging: a MICCAI segmentation Challenge”, Nice France, 1st of October 2012
Shahzad R, van Walsum T, Kirisli H, Tang H, Metz C, Schaap M, van Vliet L, Niessen W (2012) Automatic stenoses detection, quantification and lumen segmentation of the coronary arteries using a two point centerline extraction scheme. In: MICCAI 2012 workshop proceedings
Du H, Shao K, Bao F, Zhang Y, Gao C, Wu W, Zhang C (2021) Automated coronary artery tree segmentation in coronary cta using a multiobjective clustering and toroidal model-guided tracking method. Comput Methods Programs Biomed 199:105908
Tan T, Wang Z, Du H, Xu J, Qiu B (2021) Lightweight pyramid network with spatial attention mechanism for accurate retinal vessel segmentation. Int J Comput Assist Radiol Surg 16(4):673–682
Gu J, Fang Z, Gao Y, Tian F (2020) Segmentation of coronary arteries images using global feature embedded network with active contour loss. Comput Med Imaging Graph 86:101799
Shen Y, Fang Z, Gao Y, Xiong N, Zhong C, Tang X (2019) Coronary arteries segmentation based on 3d fcn with attention gate and level set function. IEEE Access 7:42826–42835
Abdelrahman KM, Chen MY, Dey AK, Virmani R, Finn AV, Khamis RY, Choi AD, Min JK, Williams MC, Buckler AJ (2020) Coronary computed tomography angiography from clinical uses to emerging technologies: Jacc state-of-the-art review. J Am Coll Cardiol 76(10):1226–1243
Jodas DS, Pereira AS, Tavares JMR (2017) Automatic segmentation of the lumen region in intravascular images of the coronary artery. Med Image Anal 40:60–79
Wiemker R, Klinder T, Bergtholdt M, Meetz K, Carlsen IC, Bülow T (2013) A radial structure tensor and its use for shape-encoding medical visualization of tubular and nodular structures. IEEE Trans Visual Comput Graphics 19(3):353–366
Moreno R, Smedby Ö (2015) Gradient-based enhancement of tubular structures in medical images. Med Image Anal 26(1):19–29
Xiao R, Yang J, Ai D, Fan J, Liu Y, Wang G, Wang Y (2015) Adaptive ridge point refinement for seeds detection in x-ray coronary angiogram. Comput Math Methods Med
Sukanya A, Rajeswari R, Subramaniam Murugan K (2020) Region based coronary artery segmentation using modified frangi’s vesselness measure. Int J Imaging Syst Technol 30(3):716–730
Dubey AK, Gupta U, Jain S (2016) Analysis of k-means clustering approach on the breast cancer wisconsin dataset. Int J Comput Assist Radiol Surg 11(11):2033–2047
Yu X, Zhai J, Zou B, Shao Q, Hou G (2021) A novel acoustic sediment classification method based on the k-mdoids algorithm using multibeam echosounder backscatter intensity. J Mar Sci Eng 9(5):508
Jang HJ, Kim B (2021) Km-dbscan: density-based clustering of massive spatial data with keywords. Human Centric Comput Inf Sci 11
Lin Y, Chen S (2021) A centroid auto-fused hierarchical fuzzy c-means clustering. IEEE Trans Fuzzy Syst 29(7):2006–2017
Kirişli H, Schaap M, Metz C, Dharampal A, Meijboom WB, Papadopoulou SL, Dedic A, Nieman K, de Graaf MA, Meijs M (2013) Standardized evaluation framework for evaluating coronary artery stenosis detection, stenosis quantification and lumen segmentation algorithms in computed tomography angiography. Med Image Anal 17(8):859–876
Acknowledgements
This work was supported in part by National Natural Science Foundation of China (No. 61971118).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, Y., Yang, J., Sun, Q. et al. Vessel filtering and segmentation of coronary CT angiographic images. Int J CARS 17, 1879–1890 (2022). https://doi.org/10.1007/s11548-022-02655-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-022-02655-7