Abstract
Purpose
The purpose of this study is to evaluate the Radiomics and Machine Learning Analysis based on MRI in the assessment of Liver Mucinous Colorectal Metastases.Query
Methods
The cohort of patients included a training set (121 cases) and an external validation set (30 cases) with colorectal liver metastases with pathological proof and MRI study enrolled in this approved study retrospectively. About 851 radiomics features were extracted as median values by means of the PyRadiomics tool on volume on interest segmented manually by two expert radiologists. Univariate analysis, linear regression modelling and pattern recognition methods were used as statistical and classification procedures.
Results
The best results at univariate analysis were reached by the wavelet_LLH_glcm_JointEntropy extracted by T2W SPACE sequence with accuracy of 92%. Linear regression model increased the performance obtained respect to the univariate analysis. The best results were obtained by a linear regression model of 15 significant features extracted by the T2W SPACE sequence with accuracy of 94%, a sensitivity of 92% and a specificity of 95%. The best classifier among the tested pattern recognition approaches was k-nearest neighbours (KNN); however, KNN achieved lower precision than the best linear regression model.
Conclusions
Radiomics metrics allow the mucinous subtype lesion characterization, in order to obtain a more personalized approach. We demonstrated that the best performance was obtained by T2-W extracted textural metrics.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most frequent world-wide cancer, accounting for 10% of new tumour cases in 2020[1]. Moreover, its prevalence is supposed to rise quickly to > 3 million cases per year by 2040 [2, 3]. Metastatic disease represents the main cause of death and the liver is the mainly metastasis site [4,5,6,7,8]. At the primary tumour diagnosis, liver metastases (CRCLM) are present in about 20% of patients, whereas almost 40–50% of patients will develop metastases during follow-up [8,9,10,11,12,13,14,15,16]. In addition, about 60% of patients will develop new liver lesions even after a R0 resection of the primary metastases. Several risk factors for liver recurrence have been recognised, as T3/T4 CRCs, node positive of the primary cancer, synchronous and more than 3 liver lesions [17, 18]. On the other hand, the adjuvant chemotherapy administration, with a complete or partial response of the CRCLM, has been associated a lower recurrence rate [19]. With regard to histological sub-types, there are few data on patient outcome. The most common sub-type is adenocarcinoma not otherwise specified (NOS), followed by mucinous one, which represents 5–15% of all CRCs. Mucinous adenocarcinoma is associated a greater burden of mutations in KRAS and BRAF genes, a higher rate of microsatellite instability and a higher rate of CpG island methylator phenotype high (CIMP-H) tumours [21, 22], so that mucinous sub-type causes an increased risk of metastases and worse overall survival (OS) so as a decreased response to conventional chemotherapy based on fluorouracil, oxaliplatin and irinotecan [20,21,22]. So, it is evident that a proper liver mucinous metastases characterization consents a better patient selection to avoid superfluous treatments [23,24,25,26,27,28,29].
Today, Radiomics analysis is a new tool in imaging setting, allowing to assess tissue at microscopic level, in order to obtain quantitative data that could be employed as biomarkers to increase diagnostic, prognostic and predictive accuracy in oncological setting [30,31,32,33,34,35,36,37,38,39]. The Radiomics key-targets are the rise of the tumour detection rate, a proper prognosis assessment and the detection of patients who are responsive to specific therapy [27, 40,41,42,43,44,45,46,47]. In this context, Radiomic is conceived to be applied in decision support of precision medicine, using standard of care images that are routinely acquired in clinical practice [38, 39, 48,49,50,51,52,53,54].
Although, several researches have assessed the role of Radiomics in CRCLM patients [55,56,57], at the best of our knowledge, no study have assessed the ability of Radiomics features, obtained by MRI, in mucinous liver metastases characterization. The purpose of this study is to evaluate the Radiomics and Machine Learning Analysis Based on MRI in the assessment of mucinous CRCLM.
Materials and methods
Local Ethical Committee board accepted this retrospective study renouncing to the patient informed consent.
Patients were selected by radiological database considering the period from January 2018 to June 2021, according to the following inclusion criteria: (1) Liver pathological proven metastases; (2) MRI study of high quality in pre-surgical setting and (3) A follow-up Computed Tomography (CT) study of at least six months after surgery. The exclusion criteria were: (1) Discordance among the imaging diagnosis and the pathological one, (2) No MRI study with hepatospecific contrast agent (EOB-MRI).
The patient cohort included a training set and an external validation set. The internal training set was formed by 51 patients (18 women and 33 men) with 61 years of median age (range 35–82 years) and 121 liver metastases. The validation cohort, from “Careggi Hospital”, Florence, Italy, was formed by 30 patients with single lesion (10 women and 20 men) and 60 years of median age (range 40–78 years). The patient characteristics are summarized in Table 1.
MR imaging protocol
MR studies were performed with two 1.5 T MR scanners: Magnetom Symphony (Siemens, Erlangen, Germany) and Magnetom Aera (Siemens). The images were acquired before and after an intravenous (IV) contrast agent (CA) injection.
The MRI study protocol included conventional sequences, T1 weighted (W), without contrast medium administration, and T2-W, Diffusion Weighted Imaging (DWI) with seven b values in order to obtain functional parameters with mono-exponential model, and T1-W sequences after the administration of contrast medium. In Table 2 we reported MR study protocol.
According to the different phase of patient management, our study protocol includes the possibility to administrate a liver-specific contrast (in pre-surgical setting) and a non-liver-specific contrast (in characterization and staging phase).
In this study, we assessed images obtained employing a liver-specific agent (0.1 mL/kg of Gd-EOB-BPTA-Primovist, Bayer Schering Pharma, Berlin, Germany). The VIBE T1-W sequence was acquired with two different flip angle (10 and 30 degrees). A power injector (Spectris Solaris® EP MR, MEDRAD Inc., Indianola, IA, USA) was used to administrate the CA at an infusion rate of 2 mL/s.
After contrast medium administration, VIBE T1-weighted FS (SPAIR) sequences were acquired in different phases: arterial (35 s delay), portal/venous (90 s), transitional phases (120 s), and hepatospecific phase (20 min).
MRI post-processing
For each volume of interest (VOI), 851 radiomics features were extracted as median values using open-source PyRadiomics python package [58] and as reported previously in [76]. The extracted features are in compliance with feature definitions as described by the Imaging Biomarker Standardization Initiative (IBSI) [59] and as reported in [https://readthedocs.org/projects/pyradiomics/downloads/ Accessed on 21 December 2021]. Median values of radiomics features were considered for each segmented VOI.
Reference standard
Histopathologic data, from routine report, were used as reference standard for determining metastasis histological subtype.
Statistical analysis
Statistical analysis includes both univariate and multivariate approaches performed considering a per-lesion analysis.
The assessment of observer variability was performed by calculating the intraclass correlation coefficient. A nonparametric Kruskal–Wallis test was performed to identify differences statistically significant of radiomics metrics of two groups (mucinous type versus non-mucinous type).
Receiver operating characteristic (ROC) analysis was performed using the Youden index to calculate the optimal cut-off for each metric and then the area under the ROC curve (AUC), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy.
Given the high number of textural features, a first selection of variables was made based on the results obtained from the univariate analysis: significant at nonparametric Kruskal–Wallis test and with an accuracy ≥ 80%. A linear regression modelling was used to assess the best linear combination of significant textural features.
Pattern recognition techniques including support vector machine (SVM), k-nearest neighbours (KNN), artificial neural network (NNET), and decision tree (DT)) were performed to calculate the diagnostic performance considering the significant features [60]. The best model was identified calculating the highest area under ROC curve and highest accuracy. Each classifier was trained with a 10-k fold cross validation. Moreover, an external validation cohort was used to validate the findings of the best classifier. McNemar test was used to evaluate that the results of the dichotomy tables were statistically significant. A p value < 0.05 was considered as significant. The statistical analyses were performed using the Statistics and Machine Toolbox of MATLAB R2021b (MathWorks, Natick, MA, USA).
Results
On univariate analysis, a variable number of metrics were statistically significant, which were distinctive when extracted from the diverse MR sequences: 15 significant predictors extracted from T2W SPACE; 13 significant predictors extracted from the arterial phase; 12 significant predictors extracted from the portal phase; 12 significant predictors extracted from the EOB-phase.
The best results at univariate analysis were reached by the wavelet_LLH_glcm_JointEntropy extracted by T2W SPACE sequence with accuracy of 92%, a sensitivity of 83%, a specificity of 94%, a PPV and a NPV of 78 and 95%, respectively, with a cut-off value of 4.61 (Table 3).
Linear regression model increased the performance obtained respect to the univariate analysis (see Table 4). The best results were obtained by a linear regression model of 15 significant features extracted by the T2W SPACE sequence with accuracy of 94%, a sensitivity of 92%, a specificity of 95%, a PPV and a NPV of 83 and 98%, respectively.
These results were statistically different from the results of univariate analysis and compared to the results of metrics extracted by other MR sequences (p value < 0.01 at McNemar test).
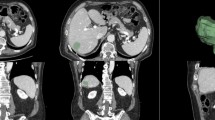
Table 5 reported the coefficients of metrics and intercept of the best linear regression model. The ROC of this linear regression model was reported in Fig. 1.
The best classifier among the tested pattern recognition approaches was KNN; however, KNN achieved lower precision than the best linear regression model (Table 5).
All results of the dichotomy tables were statistically significant (p value < 0.01 at McNemar test).
Discussion
To date, the prognosis of mucinous CRC remains highly debated, mainly because of the treatment strategy deviation for metastatic disease [20,21,22]. Although this sub-type lesion has a greater propensity for peritoneal dissemination, the liver is still the most common metastatic site and accounts for up to 50% of all metastases [2]. Management mucinous CRCLM has long been controversial. One important reason is that liver metastases are frequently accompanied by metastases of other sites, thus, a large proportion of these metastases are considered unfit for surgical resection. However, the relatively poor response to chemotherapy, indicates that surgery may occupy a more important role in the treatment of these patients, although the probability of recurrence remains high. In this context, it is evident that a proper lesions identification during pre-surgical imaging setting is the crucial element that should allow an appropriate treatment approach. Also, considering the idea that the mucinous subtype lesion has an adverse prognostic impact compared to non-mucinous subtype, since, mucinous subtype is correlated to the idea that it has a higher risk of metastases, worse overall survival (OS) and an impaired response to conventional chemotherapy [20,21,22], it is clear that radiologists should correctly recognize mucinous metastases. However, the presence of mucin substantially characterizes the lesions’ pattern on imaging studies that could suggest a diagnosis of benign lesions as hepatic cysts or haemangiomas, so that the correct diagnosis remains a challenging. At the best of our knowledge few studies have assessed the radiological features of mucinous colorectal metastases [55,56,57], and no one has evaluated the Radiomics and Machine Learning Analysis Based on MRI in the assessment of liver mucinous colorectal metastases.
In this study, we found that several metrics were statistically significant to characterize mucinous sub-type: 15 extracted from T2W SPACE; 13 from the arterial phase; 12 from the portal phase and 12 from the EOB-phase. The best results at univariate analysis were reached by the wavelet_LLH_glcm_JointEntropy extracted by T2W SPACE sequence with accuracy of 92%, a sensitivity of 83%, a specificity of 94%, a PPV and a NPV of 78 and 95%, respectively, with a cut-off value of 4.61. Also, linear regression model increased the performance obtained with a linear regression model of 15 significant features extracted by the T2W SPACE sequence with accuracy of 94%, a sensitivity of 92%, a specificity of 95%, a PPV and a NPV of 83 and 98%, respectively.
To date, several researches have evaluated the Radiomics in liver metastases, focussing attention on mutational status, prognosis and recurrence [32, 33, 47, 61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77]. The study by Andersen et al. demonstrated a correlation between homogeneity features and worse overall survival (OS) [62]. Lubner et al. showed that the skewness degree was inversely correlated to KRAS status while the entropy with OS [64]. The possibility of stratifying patients for recurrence in liver remnants has been shown BY Ravanelli et al. [69]. In our previous studies, we showed that radiomics features obtained by EOB-MRI phase, arterial and portal phase so as by T2-W sequences, allow to predict clinical outcomes following liver resection in Colorectal Liver Metastases [19, 76,77,78,79,80,81,82,83].
Radiomics is an evolving research field that enables quantitative metrics to be obtained within medical images in order to acquire lesion characteristics such as heterogeneity and shape and which can, alone or in combination with other relevant data, be used for the resolution of clinical questions.
Ours results confirmed the capacity of radiomics and machine learning analysis to identify as biomarkers, several features that could guide the treatment choice in patients with liver metastases, in order to obtain a more personalized approach. In fact, the possibility to correlate radiomics parameters to mucinous sub-type offers notable advantages over qualitative assessment, allowing one to tailor cancer therapy to the patient, to predict response to treatment, to distinguish favourable subsets of patients from those with poor prognosis, to select patients that may benefit of surgical treatment.
Although many studies have shown that radiomics is very promising, there has been little standardization and generalization of radiomics analysis, which limits the use of this approach in the clinical setting. Clear limitations regarding data quality control, repeatability, reproducibility, generalizability of results and issues related to model overfitting [61,62,63,64,65,66,67,68,69,70, 84,85,86]. In fact, it is known that different aspects of data heterogeneity are due to variations in acquisition parameters (e.g. numbers of iterations and subsets, reconstruction type and algorithm, and temporal and spatial resolution) and image processing methods (segmentation method and gray-level discretization). Consequently, to allow the repeatability, reproducibility, generalizability of results, protocol studies should be optimized to obtain the standardization of protocols. In addition, depending on the software package for extracting features and the number of filters applied, the number of features extracted varies from a few to unlimited; reducing the number of features to build statistical and machine learning models is of crucial importance for generating valid and generalizable results [84].
This study has several limitations: (1) The small sample size, although the analysis was done on a homogeneous group and on all single lesion; (2) The retrospective nature, (3) A manual segmentation. Furthermore, we not evaluated: (4) The impact of chemotherapy on our data, while we assessed all single study protocol phase demonstrating that the best performance was obtained by T2-W extracted metrics. These data open the opportunity to radiomics analysis also on abbreviated study protocol, when the patient is unfit for contrast administration [47, 72].
Conclusion
In the present study, radiomics metrics, obtained by EOB-MRI study, allow to characterize mucinous subtype lesion, in order to obtain a more personalized approach. However, we did not assess the impact of chemotherapy, while we evaluated all single study protocol phase demonstrating that the best performance was obtained by T2-W extracted metrics. These data open the opportunity to radiomics analysis also on abbreviated study protocol, when the patient is unfit for contrast administration.
Data availability
The data presented in this study are available at link https://zenodo.org/record/6589924#.YpI6vGhBy3A.
References
International Agency for Research on Cancer (IARC) (2020), GLOBOCAN 2020: colorectal cancer, Number of new cases in 2020, both sexes, all ages, vol 2020. https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf
Gunter MJ, Alhomoud S, Arnold M, Brenner H, Burn J, Casey G et al (2019) Meeting report from the joint IARC–NCI international cancer seminar series: a focus on colorectal cancer. Ann Oncol. https://doi.org/10.1093/annonc/mdz044
European Cancer Information System (ECIS) (2020) Incidence and mortality estimates. https://ecis.jrc.ec.europa.eu/explorer.php?0-01-AEE2-All4-1,23-All6-0,855-2008,20087-7CEstByCancerX0_8-3CEstRelativeCancX1_8-3X1_9-AE27CEstBySexByCancerX2_8-3X2_-1-1
Fusco R, Granata V, Sansone M, Rega D, Delrio P, Tatangelo F, Romano C, Avallone A, Pupo D, Giordano M, Grassi R, Ravo V, Pecori B, Petrillo A (2021) Validation of the standardized index of shape tool to analyze DCE-MRI data in the assessment of neo-adjuvant therapy in locally advanced rectal cancer. Radiol Med. https://doi.org/10.1007/s11547-021-01369-1
Granata V, Fusco R, deLutiodiCastelguidone E, Avallone A, Palaia R, Delrio P, Tatangelo F, Botti G, Grassi R, Izzo F, Petrillo A (2019) Diagnostic performance of gadoxetic acid-enhanced liver MRI versus multidetector CT in the assessment of colorectal liver metastases compared to hepatic resection. BMC Gastroenterol 19:129
Rega D, Pace U, Scala D, Chiodini P, Granata V, Fares Bucci A, Pecori B, Delrio P (2019) Treatment of splenic flexure colon cancer: a comparison of three different surgical procedures: Experience of a high volume cancer center. Sci Rep 9(1):10953. https://doi.org/10.1038/s41598-019-47548-z
Schicchi N, Fogante M, Palumbo P, Agliata G, Esposto Pirani P, Di Cesare E, Giovagnoni A (2020) The sub-millisievert era in CTCA: the technical basis of the new radiation dose approach. Radiol Med 125(11):1024–1039. https://doi.org/10.1007/s11547-020-01280-1
Granata V, Grassi R, Fusco R, Izzo F, Brunese L, Delrio P, Avallone A, Pecori B, Petrillo A (2020) Current status on response to treatment in locally advanced rectal cancer: what the radiologist should know. Eur Rev Med Pharmacol Sci 24(23):12050–12062. https://doi.org/10.26355/eurrev_202012_23994
Park SH, Kim YS, Choi J (2021) Dosimetric analysis of the effects of a temporary tissue expander on the radiotherapy technique. Radiol Med 126(3):437–444. https://doi.org/10.1007/s11547-020-01297-6
Crimì F, Capelli G, Spolverato G, Bao QR, Florio A, Milite Rossi S, Cecchin D, Albertoni L, Campi C, Pucciarelli S, Stramare R (2020) MRI T2-weighted sequences-based texture analysis (TA) as a predictor of response to neoadjuvant chemo-radiotherapy (nCRT) in patients with locally advanced rectal cancer (LARC). Radiol Med 125(12):1216–1224. https://doi.org/10.1007/s11547-020-01215-w
Bertocchi E, Barugola G, Nicosia L, Mazzola R, Ricchetti F, Dell’Abate P, Alongi F, Ruffo G (2020) A comparative analysis between radiation dose intensification and conventional fractionation in neoadjuvant locally advanced rectal cancer: a monocentric prospective observational study. Radiol Med 125:990–998. https://doi.org/10.1007/s11547-020-01189-9
Fornell-Perez R, Vivas-Escalona V, Aranda-Sanchez J, Gonzalez-Dominguez MC, Rubio-Garcia J, Aleman-Flores P, Lozano-Rodriguez A, Porcel-de-Peralta G, Loro-Ferrer JF (2020) Primary and post-chemoradiotherapy MRI detection of extramural venous invasion in rectal cancer: the role of diffusion-weighted imaging. Radiol Med 125(6):522–530. https://doi.org/10.1007/s11547-020-01137-7
Cusumano D, Meijer G, Lenkowicz J, Chiloiro G, Boldrini L, Masciocchi C, Dinapoli N, Gatta R, Casà C, Damiani A, Barbaro B, Gambacorta MA, Azario L, De Spirito M, Intven M, Valentini V (2021) A field strength independent MR radiomics model to predict pathological complete response in locally advanced rectal cancer. Radiol Med 126(3):421–429. https://doi.org/10.1007/s11547-020-01266-z
Fusco R, Sansone M, Granata V, Grimm R, Pace U, Delrio P, Tatangelo F, Botti G, Avallone A, Pecori B, Petrillo A (2019) Diffusion and perfusion MR parameters to assess preoperative short-course radiotherapy response in locally advanced rectal cancer: a comparative explorative study among standardized Index of shape by DCE-MRI, intravoxel incoherent motion- and diffusion kurtosis imaging-derived parameters. Abdom Radiol (NY) 44(11):3683–3700. https://doi.org/10.1007/s00261-018-1801-z
Granata V, Caruso D, Grassi R, Cappabianca S, Reginelli A, Rizzati R, Masselli G, Golfieri R, Rengo M, Regge D, Lo Re G, Pradella S, Fusco R, Faggioni L, Laghi A, Miele V, Neri E, Coppola F (2021) Structured reporting of rectal cancer staging and restaging: a consensus proposal. Cancers (Basel) 13(9):2135. https://doi.org/10.3390/cancers13092135
Granata V, Fusco R, Reginelli A, Delrio P, Selvaggi F, Grassi R, Izzo F, Petrillo A (2019) Diffusion kurtosis imaging in patients with locally advanced rectal cancer: current status and future perspectives. J Int Med Res 47(6):2351–2360. https://doi.org/10.1177/0300060519827168
Petrillo A, Fusco R, Granata V, Filice S, Sansone M, Rega D, Delrio P, Bianco F, Romano GM, Tatangelo F, Avallone A, Pecori B (2018) Assessing response to neo-adjuvant therapy in locally advanced rectal cancer using Intra-voxel Incoherent Motion modelling by DWI data and Standardized Index Of Shape From DCE-MRI. Ther Adv Med Oncol 16(10):1758835918809875. https://doi.org/10.1177/1758835918809875
Fusco R, Granata V, Rega D, Russo C, Pace U, Pecori B, Tatangelo F, Botti G, Izzo F, Cascella M, Avallone A, Delrio P, Petrillo A (2019) Morphological and functional features prognostic factor of magnetic resonance imaging in locally advanced rectal cancer. Acta Radiol 60(7):815–825. https://doi.org/10.1177/0284185118803783
Fusco R, Petrillo M, Granata V, Filice S, Sansone M, Catalano O, Petrillo A (2017) Magnetic resonance imaging evaluation in neoadjuvant therapy of locally advanced rectal cancer: a systematic review. Radiol Oncol 51(3):252–262. https://doi.org/10.1515/raon-2017-0032
Rees M, Tekkis PP, Welsh FK, O’Rourke T, John TG (2008) Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: a multifactorial model of 929 patients. Ann Surg 247(1):125e135
Abdalla EK, Vauthey JN, Ellis LM et al (2004) Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 239(6):818e825
Vigano L, Capussotti L, Lapointe R et al (2014) Early recurrence after liver resection for colorectal metastases: risk factors, prognosis, and treatment. A LiverMetSurvey-based study of 6,025 patients. Ann Surg Oncol 21(4):1276e1286
Petralia G, Zugni F, Summers PE, Colombo A, Pricolo P, Grazioli L, Colagrande S, Giovagnoni A, Padhani AR (2021) Italian working group on magnetic resonance. Whole-body magnetic resonance imaging (WB-MRI) for cancer screening: recommendations for use. Radiol Med 126(11):1434–1450. https://doi.org/10.1007/s11547-021-01392-2
Petralia G, Summers PE, Agostini A, Ambrosini R, Cianci R, Cristel G, Calistri L, Colagrande S (2020) Dynamic contrast-enhanced MRI in oncology: how we do it. Radiol Med 125(12):1288–1300. https://doi.org/10.1007/s11547-020-01220-z
Granata V, Grassi R, Fusco R, Setola SV, Belli A, Ottaiano A, Nasti G, La Porta M, Danti G, Cappabianca S, Cutolo C, Petrillo A, Izzo F (2021) Intrahepatic cholangiocarcinoma and its differential diagnosis at MRI: how radiologist should assess MR features. Radiol Med 126(12):1584–1600. https://doi.org/10.1007/s11547-021-01428-7
Granata V, Bicchierai G, Fusco R, Cozzi D, Grazzini G, Danti G, De Muzio F, Maggialetti N, Smorchkova O, D’Elia M, Brunese MC, Grassi R, Giacobbe G, Bruno F, Palumbo P, Grassi F, Brunese L, Grassi R, Miele V, Barile A (2021) Diagnostic protocols in oncology: workup and treatment planning. Part 2: abbreviated MR protocol. Eur Rev Med Pharmacol Sci 25(21):6499–6528. https://doi.org/10.26355/eurrev_202111_27094
Gurgitano M, Angileri SA, Rodà GM, Liguori A, Pandolfi M, Ierardi AM, Wood BJ, Carrafiello G (2021) Interventional radiology ex-machina: impact of artificial intelligence on practice. Radiol Med 126(7):998–1006. https://doi.org/10.1007/s11547-021-01351-x
Granata V, Fusco R, Costa M, Picone C, Cozzi D, Moroni C, La Casella GV, Montanino A, Monti R, Mazzoni F, Grassi R, Malagnino VG, Cappabianca S, Grassi R, Miele V, Petrillo A (2021) Preliminary report on computed tomography radiomics features as biomarkers to immunotherapy selection in lung adenocarcinoma patients. Cancers (Basel) 13(16):3992. https://doi.org/10.3390/cancers13163992
Granata V, Fusco R, Barretta ML, Picone C, Avallone A, Belli A, Patrone R, Ferrante M, Cozzi D, Grassi R, Grassi R, Izzo F, Petrillo A (2021) Radiomics in hepatic metastasis by colorectal cancer. Infect Agent Cancer 16(1):39. https://doi.org/10.1186/s13027-021-00379-y
Fusco R, Piccirillo A, Sansone M, Granata V, Rubulotta MR, Petrosino T, Barretta ML, Vallone P, Di Giacomo R, Esposito E, Di Bonito M, Petrillo A (2021) Radiomics and artificial intelligence analysis with textural metrics extracted by contrast-enhanced mammography in the breast lesions classification. Diagnostics (Basel) 11(5):815. https://doi.org/10.3390/diagnostics11050815
Fusco R, Granata V, Mazzei MA, Meglio ND, Roscio DD, Moroni C, Monti R, Cappabianca C, Picone C, Neri E, Coppola F, Montanino A, Grassi R, Petrillo A, Miele V (2021) Quantitative imaging decision support (QIDS™) tool consistency evaluation and radiomic analysis by means of 594 metrics in lung carcinoma on chest CT scan. Cancer Control 28:1073274820985786. https://doi.org/10.1177/1073274820985786
Granata V, Fusco R, Avallone A, De Stefano A, Ottaiano A, Sbordone C, Brunese L, Izzo F, Petrillo A (2021) Radiomics-derived data by contrast enhanced magnetic resonance in ras mutations detection in colorectal liver metastases. Cancers (Basel) 13(3):453. https://doi.org/10.3390/cancers13030453
Granata V, Fusco R, Risi C, Ottaiano A, Avallone A, De Stefano A, Grimm R, Grassi R, Brunese L, Izzo F, Petrillo A (2020) Diffusion-weighted MRI and diffusion kurtosis imaging to detect RAS mutation in colorectal liver metastasis. Cancers (Basel) 12(9):2420. https://doi.org/10.3390/cancers12092420
Petralia G, Summers PE, Agostini A, Ambrosini R, Cianci R, Cristel G, Calistri L, Colagrande S (2020) Dynamic contrast-enhanced MRI in oncology: how we do it. Radiol Med 125:1288–1300. https://doi.org/10.1007/s11547-020-01220-z
Ria F, Samei E (2020) Is regulatory compliance enough to ensure excellence in medicine? Radiol Med 125:904–905. https://doi.org/10.1007/s11547-020-01171-5
Zhang A, Song J, Ma Z, Chen T (2020) Combined dynamic contrast-enhanced magnetic resonance imaging and diffusion-weighted imaging to predict neoadjuvant chemotherapy effect in FIGO stage IB2-IIA2 cervical cancers. Radiol Med 125:1233–1242. https://doi.org/10.1007/s11547-020-01214-x
Crimi F, Capelli G, Spolverato G, Bao QR, Florio A, Milite Rossi S, Cecchin D, Albertoni L, Campi C, Pucciarelli S et al (2020) MRI T2-weighted sequences-based texture analysis (TA) as a predictor of response to neoadjuvant chemo-radiotherapy (nCRT) in patients with locally advanced rectal cancer (LARC). Radiol Med 125:1216–1224. https://doi.org/10.1007/s11547-020-01215-w
Kirienko M, Ninatti G, Cozzi L, Voulaz E, Gennaro N, Barajon I, Ricci F, Carlo-Stella C, Zucali P, Sollini M et al (2020) Computed tomography (CT)-derived radiomic features differentiate prevascular mediastinum masses as thymic neoplasms versus lymphomas. Radiol Med 125:951–960. https://doi.org/10.1007/s11547-020-01188-w
Zhang L, Kang L, Li G, Zhang X, Ren J, Shi Z, Li J, Yu S (2020) Computed tomography-based radiomics model for discriminating the risk stratification of gastrointestinal stromal tumors. Radiol Med 125:465–473. https://doi.org/10.1007/s11547-020-01138-6
Scapicchio C, Gabelloni M, Barucci A, Cioni D, Saba L, Neri E (2021) A deep look into radiomics. Radiol Med 126(10):1296–1311. https://doi.org/10.1007/s11547-021-01389-x
Wei J, Jiang H, Gu D, Niu M, Fu F, Han Y, Song B, Tian J (2020) Radiomics in liver diseases: Current progress and future opportunities. Liver Int 40(9):2050–2063. https://doi.org/10.1111/liv.14555
Saini A, Breen I, Pershad Y, Naidu S, Knuttinen MG, Alzubaidi S, Sheth R, Albadawi H, Kuo M, Oklu R (2018) Radiogenomics and radiomics in liver cancers. Diagnostics (Basel) 9(1):4. https://doi.org/10.3390/diagnostics9010004
Mathew RP, Sam M, Raubenheimer M, Patel V, Low G (2020) Hepatic hemangiomas: the various imaging avatars and its mimickers. Radiol Med 125(9):801–815. https://doi.org/10.1007/s11547-020-01185-z
Nardone V, Reginelli A, Grassi R, Boldrini L, Vacca G, D’Ippolito E, Annunziata S, Farchione A, Belfiore MP, Desideri I, Cappabianca S (2021) Delta radiomics: a systematic review. Radiol Med 126(12):1571–1583. https://doi.org/10.1007/s11547-021-01436-7
Brunese L, Brunese MC, Carbone M, Ciccone V, Mercaldo F, Santone A (2021) Automatic PI-RADS assignment by means of formal methods. Radiol Med. https://doi.org/10.1007/s11547-021-01431-y
van der Lubbe MFJA, Vaidyanathan A, de Wit M, van den Burg EL, Postma AA, Bruintjes TD, Bilderbeek-Beckers MAL, Dammeijer PFM, Bossche SV, Van Rompaey V, Lambin P, van Hoof M, van de Berg R (2021) A non-invasive, automated diagnosis of Menière’s disease using radiomics and machine learning on conventional magnetic resonance imaging: a multicentric, case-controlled feasibility study. Radiol Med. https://doi.org/10.1007/s11547-021-01425-w
Granata V, Fusco R, Avallone A, Cassata A, Palaia R, Delrio P, Grassi R, Tatangelo F, Grazzini G, Izzo F, Petrillo A (2020) Abbreviated MRI protocol for colorectal liver metastases: how the radiologist could work in pre surgical setting. PLoS ONE 15(11):e0241431. https://doi.org/10.1371/journal.pone.0241431
Santone A, Brunese MC, Donnarumma F, Guerriero P, Mercaldo F, Reginelli A, Miele V, Giovagnoni A, Brunese L (2021) Radiomic features for prostate cancer grade detection through formal verification. Radiol Med. https://doi.org/10.1007/s11547-020-01314-8
Agazzi GM, Ravanelli M, Roca E, Medicina D, Balzarini P, Pessina C, Vermi W, Berruti A, Maroldi R, Farina D (2021) CT texture analysis for prediction of EGFR mutational status and ALK rearrangement in patients with non-small cell lung cancer. Radiol Med. https://doi.org/10.1007/s11547-020-01323-7
Benedetti G, Mori M, Panzeri MM, Barbera M, Palumbo D, Sini C, Muffatti F, Andreasi V, Steidler S, Doglioni C, Partelli S, Manzoni M, Falconi M, Fiorino C, De Cobelli F (2021) CT-derived radiomic features to discriminate histologic characteristics of pancreatic neuroendocrine tumors. Radiol Med. https://doi.org/10.1007/s11547-021-01333-z
Granata V, Fusco R, Venanzio Setola S, Mattace Raso M, Avallone A, De Stefano A, Nasti G, Palaia R, Delrio P, Petrillo A, Izzo F (2019) Liver radiologic findings of chemotherapy-induced toxicity in liver colorectal metastases patients. Eur Rev Med Pharmacol Sci 23(22):9697–9706. https://doi.org/10.26355/eurrev_201911_19531
Granata V, Fusco R, Maio F, Avallone A, Nasti G, Palaia R, Albino V, Grassi R, Izzo F, Petrillo A (2019) Qualitative assessment of EOB-GD-DTPA and Gd-BT-DO3A MR contrast studies in HCC patients and colorectal liver metastases. Infect Agent Cancer 27(14):40. https://doi.org/10.1186/s13027-019-0264-3
Granata V, Fusco R, de Lutio di Castelguidone E, Avallone A, Palaia R, Delrio P, Tatangelo F, Botti G, Grassi R, Izzo F, Petrillo A (2019) Diagnostic performance of gadoxetic acid-enhanced liver MRI versus multidetector CT in the assessment of colorectal liver metastases compared to hepatic resection. BMC Gastroenterol 19(1):129. https://doi.org/10.1186/s12876-019-1036-7
Reynolds IS, Furney SJ, Kay EW, McNamara DA, Prehn JHM, Burke JP (2019) Meta- analysis of the molecular associations of mucinous colorectal cancer. Br J Surg 106(6):682e691
Reynolds IS, O’Connell E, Fichtner M et al (2020) Mucinous adenocarcinoma is a pharmacogenomically distinct subtype of colorectal cancer. Pharmacogenomics J 20(3):524e532
McCawley N, Clancy C, O’Neill BD, Deasy J, McNamara DA, Burke JP (2016) Mucinous rectal adenocarcinoma is associated with a poor response to neoadjuvant chemoradiotherapy: a systematic review and meta-analysis. Dis Colon Rectum 59(12):1200e1208
Granata V, Fusco R, Avallone A, Catalano O, Piccirillo M, Palaia R, Nasti G, Petrillo A, Izzo F (2018) A radiologist’s point of view in the presurgical and intraoperative setting of colorectal liver metastases. Future Oncol 14(21):2189–2206. https://doi.org/10.2217/fon-2018-0080
Van Griethuysen JJM, Fedorov A, Parmar C, Hosny A, Aucoin N, Narayan V, Beets-Tan RGH, Fillion-Robin JC, Pieper S, Aerts HJWL (2017) Computational radiomics system to decode the radiographic phenotype. Cancer Res 77:e104–e107. https://doi.org/10.1158/0008-5472.CAN-17-0339
Zwanenburg A, Vallières M, Abdalah MA, Aerts HJWL, Andrearczyk V, Apte A, Ashrafinia S, Bakas S, Beukinga RJ, Boellaard R et al (2020) The image biomarker standardization initiative: standardized quantitative radiomics for high-throughput image-based phenotyping. Radiology 295:328–338
Fusco R, Sansone M, Filice S, Carone G, Amato DM, Sansone C, Petrillo A (2016) Pattern recognition approaches for breast cancer dce-mri classification: a systematic review. J Med Biol Eng 36:449–459. https://doi.org/10.1007/s40846-016-0163-7
Beckers RCJ, Trebeschi S, Maas M, Schnerr RS, Sijmons JML, Beets GL, Houwers JB, Beets-Tan RGH, Lambregts DMJ (2018) CT texture analysis in colorectal liver metastases and the surrounding liver parenchyma and its potential as an imaging biomarker of disease aggressiveness, response and survival. Eur J Radiol 102:15–21
Andersen IR, Thorup K, Andersen MB, Olesen R, Mortensen FV, Nielsen DT, Rasmussen F (2019) Texture in the monitoring of regorafenib therapy in patients with colorectal liver metastases. Acta Radiol 60:1084–1093
Zhang H, Li W, Hu F, Sun Y, Hu T, Tong T (2018) MR texture analysis: potential imaging biomarker for predicting the chemotherapeutic response of patients with colorectal liver metastases. Abdom Radiol 44:65–71
Lubner MG, Stabo N, Lubner SJ, del Rio AM, Song C, Halberg RB, Pickhardt PJ (2015) CT textural analysis of hepatic metastatic colorectal cancer: pre-treatment tumor heterogeneity correlates with pathology and clinical outcomes. Abdom Imaging 40:2331–2337
Simpson AL, Doussot A, Creasy JM, Adams LB, Allen PJ, DeMatteo RP, Gönen M, Kemeny NE, Kingham TP, Shia J et al (2017) Computed tomography image texture: a noninvasive prognostic marker of hepatic recurrence after hepatectomy for metastatic colorectal cancer. Ann Surg Oncol 24:2482–2490
Ganeshan B, Miles KA, Young RC, Chatwin CR (2007) Hepatic enhancement in colorectal cancer: texture analysis correlates with hepatic hemodynamics and patient survival. Acad Radiol 14:1520–1530
Rahmim A, Bak-Fredslund KP, Ashrafinia S, Lu L, Schmidtlein C, Subramaniam RM, Morsing A, Keiding S, Horsager J, Munk OL (2019) Prognostic modeling for patients with colorectal liver metastases incorporating FDG PET radiomic features. Eur J Radiol 113:101–109
Dercle L, Lu L, Schwartz LH, Qian M, Tejpar S, Eggleton P, Zhao B, Piessevaux H (2020) Radiomics response signature for identification of metastatic colorectal cancer sensitive to therapies targeting EGFR pathway. J Natl Cancer Inst 112:902–912
Ravanelli M, Agazzi GM, Tononcelli E, Roca E, Cabassa P, Baiocchi GL, Berruti A, Maroldi R, Farina D (2019) Texture features of colorectal liver metastases on pretreatment contrast-enhanced CT may predict response and prognosis in patients treated with bevacizumab-containing chemotherapy: a pilot study including comparison with standard chemotherapy. Radiol Med 124:877–886
Taghavi M, Staal FC, Simões R, Hong EK, Lambregts DM, van der Heide UA, Beets-Tan RG, Maas M (2021) CT radiomics models are unable to predict new liver metastasis after successful thermal ablation of colorectal liver metastases. Acta Radiol 17:2841851211060437. https://doi.org/10.1177/02841851211060437
Granata V, Fusco R, Catalano O, Filice S, Amato DM, Nasti G, Avallone A, Izzo F, Petrillo A (2015) Early assessment of colorectal cancer patients with liver metastases treated with antiangiogenic drugs: the role of intravoxel incoherent motion in diffusion-weighted imaging. PLoS ONE 10(11):e0142876. https://doi.org/10.1371/journal.pone.0142876
Granata V, Fusco R, Petrillo A (2021) Additional considerations on use of abbreviated liver MRI in patients with colorectal liver metastases. AJR Am J Roentgenol 217(1):W1. https://doi.org/10.2214/AJR.21.25652
Esposito A, Buscarino V, Raciti D, Casiraghi E, Manini M, Biondetti P, Forzenigo L (2020) Characterization of liver nodules in patients with chronic liver disease by MRI: performance of the liver imaging reporting and data system (LI-RADS vol 2018) scale and its comparison with the likert scale. Radiol Med 125(1):15–23. https://doi.org/10.1007/s11547-019-01092-y
Bozkurt M, Eldem G, Bozbulut UB, Bozkurt MF, Kılıçkap S, Peynircioğlu B, Çil B, Lay Ergün E, Volkan-Salanci B (2021) Factors affecting the response to Y-90 microsphere therapy in the cholangiocarcinoma patients. Radiol Med 126(2):323–333. https://doi.org/10.1007/s11547-020-01240-9
Shin N, Choi JA, Choi JM, Cho ES, Kim JH, Chung JJ, Yu JS (2020) Sclerotic changes of cavernous hemangioma in the cirrhotic liver: long-term follow-up using dynamic contrast-enhanced computed tomography. Radiol Med 125:1225–1232
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Dell’Aversana F, Ottaiano A, Nasti G, Grassi R, Pilone V, Miele V, Brunese MC, Tatangelo F, Izzo F, Petrillo A (2022) EOB-MR based radiomics analysis to assess clinical outcomes following liver resection in colorectal liver metastases. Cancers 14(5):1239. https://doi.org/10.3390/cancers14051239
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, dell’ Aversana F, Ottaiano A, Avallone A, Nasti G, Grassi F, Pilone V, Miele V, Brunese L, Izzo F, Petrillo A (2022) Contrast MR-based radiomics and machine learning analysis to assess clinical outcomes following liver resection in colorectal liver metastases: a preliminary study. Cancers 14(5):1110. https://doi.org/10.3390/cancers14051110
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Dell’Aversana F, Belli A, Romano C, Ottaiano A, Nasti G et al (2022) Magnetic resonance features of liver mucinous colorectal metastases: what the radiologist should know. J Clin Med 11:2221. https://doi.org/10.3390/jcm11082221
Bimonte S, Leongito M, Barbieri A, Del Vecchio V, Barbieri M, Albino V, Piccirillo M, Amore A, Di Giacomo R, Nasto A, Granata V, Petrillo A, Arra C, Izzo F (2015) Inhibitory effect of (-)-epigallocatechin-3-gallate and bleomycin on human pancreatic cancer MiaPaca-2 cell growth. Infect Agent Cancer 29(10):22. https://doi.org/10.1186/s13027-015-0016-y
Avallone A, Pecori B, Bianco F, Aloj L, Tatangelo F, Romano C, Granata V, Marone P, Leone A, Botti G, Petrillo A, Caracò C, Iaffaioli VR, Muto P, Romano G, Comella P, Budillon A, Delrio P (2015) Critical role of bevacizumab scheduling in combination with pre-surgical chemo-radiotherapy in MRI-defined high-risk locally advanced rectal cancer: results of the BRANCH trial. Oncotarget 6(30):30394–30407. https://doi.org/10.18632/oncotarget.4724
Granata V, Fusco R, Setola SV, De Muzio F, Dell’ Aversana F, Cutolo C, Faggioni L, Miele V, Izzo F, Petrillo A (2022) CT-based radiomics analysis to predict histopathological outcomes following liver resection in colorectal liver metastases. Cancers (Basel) 14(7):1648. https://doi.org/10.3390/cancers14071648.PMID:35406419;PMCID:PMC8996874
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Grassi R, Grassi F, Ottaiano A, Nasti G, Tatangelo F, Pilone V, Miele V, Brunese MC, Izzo F, Petrillo A (2022) Radiomics textural features by MR imaging to assess clinical outcomes following liver resection in colorectal liver metastases. Radiol Med. https://doi.org/10.1007/s11547-022-01477-6
Petrillo A, Fusco R, Petrillo M, Granata V, Delrio P, Bianco F, Pecori B, Botti G, Tatangelo F, Caracò C, Aloj L, Avallone A, Lastoria S (2017) Standardized Index of Shape (DCE-MRI) and Standardized Uptake Value (PET/CT): two quantitative approaches to discriminate chemo-radiotherapy locally advanced rectal cancer responders under a functional profile. Oncotarget 8(5):8143–8153. https://doi.org/10.18632/oncotarget.14106
Fusco R, Granata V, Grazzini G, Pradella S, Borgheresi A, Bruno A, Palumbo P, Bruno F, Grassi R, Giovagnoni A, Grassi R, Miele V, Barile A (2022) Radiomics in medical imaging: pitfalls and challenges in clinical management. Jpn J Radiol. https://doi.org/10.1007/s11604-022-01271-4
Tagliafico AS, Campi C, Bianca B, Bortolotto C, Buccicardi D, Francesca C, Prost R, Rengo M, Faggioni L (2022) Blockchain in radiology research and clinical practice: current trends and future directions. Radiol Med 127(4):391–397. https://doi.org/10.1007/s11547-022-01460-1
Coppola F, Giannini V, Gabelloni M, Panic J, Defeudis A, Lo Monaco S, Cattabriga A, Cocozza MA, Pastore LV, Polici M, Caruso D, Laghi A, Regge D, Neri E, Golfieri R, Faggioni L (2021) Radiomics and magnetic resonance imaging of rectal cancer: from engineering to clinical practice. Diagnostics (Basel) 11(5):756. https://doi.org/10.3390/diagnostics11050756.PMID:33922483;PMCID:PMC8146913
Acknowledgements
The authors are grateful to Alessandra Trocino, librarian at the National Cancer Institute of Naples, Italy. Moreover, for the collaboration, authors are grateful for the research support to Paolo Pariate, Martina Totaro and Andrea Esposito of Radiology Division, Istituto Nazionale Tumori IRCCS Fondazione Pascale—IRCCS di Napoli, 80131 Napoli, Italy.
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
Each author has participated sufficiently to take public responsibility for the content of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have not disclosed any conflict of interest.
Ethical standard
Ethical standards This article does not contain any studies with human participants or animals performed by any of the authors.
Institutional review board statement
This study aligned with National appropriate guidelines and procedures. The Local Ethical Committee board approved this retrospective study.
Informed consent statement
This study aligned with National appropriate guidelines and procedures. Renouncing the need for informed patient consent given the study nature.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Granata, V., Fusco, R., De Muzio, F. et al. Radiomics and machine learning analysis based on magnetic resonance imaging in the assessment of liver mucinous colorectal metastases. Radiol med 127, 763–772 (2022). https://doi.org/10.1007/s11547-022-01501-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01501-9