Abstract
Purpose
To establish an optimized ultralow-dose digital pulsed fluoroscopy (FP) protocol for upper gastrointestinal tract examinations and to investigate the radiation dose and image quality.
Materials and methods
An Alderson-Rando-Phantom with 60 thermoluminescent dosimeters was used for dose measurements to systematically evaluate the dose–area product (DAP) and organ doses of the optimized FP protocol with the following acquisition parameters: 86.7 kV; 77 mA; 0.9 mm3, automatic image noise and contrast adaption. Subjective image quality, depiction of contrast agent and image noise (5-point Likert scale; 5 = excellent) were assessed in 41 patients, who underwent contrast-enhanced FP with the aforementioned optimized protocol by two radiologists in consensus. A conventional digital radiograph (DR) acquisition protocol served as the reference standard for radiation dose and image quality analyses.
Results
Phantom measurements revealed a general dose reduction of approximately 96% per image for the FP protocol as compared to the DR standard. DAP could be reduced by 97%. Significant dose reductions were also found for organ doses, both in the direct and scattered radiation beam with negligible orbital (FP 5.6 × 10−3 vs. DR 0.11; p = 0.02) and gonadal dose exposure (female FP 2.4 × 10−3 vs. DR 0.05; male FP 8 × 10−4 vs. DR 0.03; p ≤ 0.0004). FP provided diagnostic image quality in all patients, although reading scores were significantly lower for all evaluated parameters as compared to the DR standard (p < 0.05).
Conclusion
Ultralow-dose FP is feasible for clinical routine allowing a significant reduction of direct and scattered dose exposure while providing sufficient diagnostic image quality for reliable diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dynamic fluoroscopic examinations of the upper gastrointestinal tract (UGI) are a comprehensive diagnostic tool to assess a variety of disorders and pathologies [1]. Although endoscopy has become the diagnostic gold standard for UGI examinations, fluoroscopy is still frequently used in clinical routine, as it provides additional functional and dynamic information [2,3,4,5,6]. This applies in particular to the evaluation of gastrointestinal passage disorders, dynamic evaluation of the swallowing process or leakage of oesophageal and gastric anastomoses, since fluoroscopy is more simple and cost-effective to perform than CT or MRI [6,7,8,9]. Furthermore, in paediatric radiology, fluoroscopy, often combined with ultrasound, serves as an alternative to CT to reduce dose exposure in both gastrointestinal and urogenital tract examinations [1, 10,11,12,13].
According to the ALARA principles, continuous optimization of examination protocols is demanded to reduce the cumulative dose exposure of the patient to minimize the risk of radiation effects [14, 15]. This is of particular interest, if frequent examinations are necessary, e.g. to evaluate the postoperative course or disease follow-up. Conventional DR acquisition was the examination of choice for the dynamic evaluation of UGI pathologies after changing from analogue to digital acquisition techniques, providing high-resolution images, however, at a considerable radiation dose [16, 17]. To account for this, several improvements of fluoroscopic hardware and dedicated post-processing software have been developed in recent years allowing for a substantial dose reduction [18,19,20,21]. However, focused research evaluating the benefits of these technical advances for fluoroscopic examinations of the upper gastrointestinal tract in adults are outstanding so far [16, 19]. Moreover, it is still difficult to estimate the actual organ dose applied during such examinations, since dose monitoring in fluoroscopy is commonly performed using the dose–area product (DAP) [22, 23]. Dedicated phantom studies investigating absorbed organ doses of radiosensitive organs are rare [1, 11, 24] although it is important to know in favour of patient safety [25].
Therefore, the aim of this study was to establish an optimized dynamic ultralow-dose digital pulsed fluoroscopy (FP) protocol for upper gastrointestinal tract examinations and to investigate the resulting organ doses and its clinical feasibility with conventional digital radiograph (DR) acquisitions as reference standard. We hypothesized that ultralow-dose digital pulsed fluoroscopy allows for sufficient diagnostic image quality to provide reliable diagnosis while significantly reducing direct and scattered dose exposure.
Materials and methods
The institutional review board approved this retrospective study and waived the requirement of written informed consent.
Detector system and protocols
A multifunctional fluoroscopy system (Artis Zee MP, Siemens Healthcare, Erlangen, Germany) with a flat-panel detector [amorphous silicon (a-Si) with caesium iodide (CsI) scintillator; size: 30 × 40 cm; pixel size 154 × 154 µm; spatial resolution of 3.25 LP/mm; digitization depth 14 bit] was used for all phantom and patient measurements.
The acquisition parameters of our optimized ultralow-dose digital pulsed protocol were as follows: 86.7 kV; 77 mA; 3.2 ms; a copper filter of 0.9 mm was applied for beam hardening; to compensate for the resulting decrease in image contrast, an automatic post-processing algorithm was implemented to improve contrast ratios; in addition, automatic noise reduction was used to balance the low mA–s product; a resolution of 512 × 512 was chosen with an acquisition pulse rate of 30/s for high temporal resolution. The conventional reference DR acquisitions were performed with 80.0 kV, 283 mA, 9.0 ms, a copper filtering of 0.2 mm, a resolution of 1024 × 1024 and a frame rate of 30/s.
For both protocols, the field of view was chosen as small as possible (refer to Fig. 1). The last image hold was used for table and collimator adjustments.
Phantom studies
To systematically investigate the potential of our optimized FP protocol to reduced radiation burden and to objectify organ dose exposure, we conducted a phantom study using an anthropomorphic male Alderson-Rando Phantom (Type RT200, Humanoid Systems, CA, USA) representing a male patient (175 cm height and 73.5 kg weight) with similar X-ray absorption and scattering as human body tissue. For dose measurements, 60 thermoluminescent dosimeters (TLD, LiF (lithium fluoride), TLD Type-100; Harshaw, Chemical Company, Ohio, USA) were placed in radiosensitive organs in the direct (bone marrow; lungs; oesophagus; stomach; thymus) and scattered (eyes; liver; gonads; thyroid) beam. To ensure reliable measures and taking into account the radiation absorption along the examined object in the p.a. direction, each organ was equipped with at least two (2–6) TLDs including the most ventral and most dorsal part to homogenously cover the whole organ. The final organ doses were than calculated by averaging the detected doses of all TLDs per organ. To consider the extremely low-dose exposure of the FP protocol and to allow for reliable dose detection by the TLD, images were acquired until the detector system indicated a cumulative dose of 500 mGy. Between FP and DR acquisition, all TLDs were recalibrated. The phantom–tube distance was 36 cm, while the distance between the phantom and the detector was 28.5 cm. The measured values for the DAP and the organ doses were normalized to the mean examination time in the patient study (see below) to provide a useful measure for clinical routine.
Patient study
To assess the image quality of the investigated FP protocol in clinical routine, we included 41 patients, who underwent clinically indicated contrast-enhanced (Imeron 400, Bracco, Konstanz, Germany; Peritrast 400, Dr. Franz Köhler Chemie GmbH, Bensheim, Germany) fluoroscopy with our optimized FP protocol and of whom a historical conventional DR acquisition was available in the PACS archive. Patients under the age of 18 years and incomplete examinations were excluded from the analysis. A summary with detailed patient demographics is given in Table 1.
Analysis of image quality
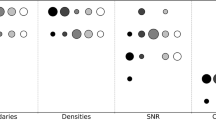
Image quality was subjectively evaluated on a dedicated workstation (syngoMMWP VE26A; Siemens Healthcare, Erlangen, Germany) by two radiologists in consensus with 3 (A.P.) and 6 years (M.N.) of experience in fluoroscopy. Readers were blinded to the acquisition protocol and the clinical diagnosis and images were presented in a random order. A five-point Likert scale was used to assess the following parameters: 1) overall image quality; 2) delineation of contrast agent; 3) image noise (5 = excellent image quality and delineation, no image noise; 4 = good image quality and delineation, subtle image noise; 3 = fair image quality and delineation, moderate image noise; 2 = poor image quality and delineation, severe image noise; 1 = non-diagnostic).
Statistical analysis
We performed statistical analysis using SPSS Statistics (Version 22, IMB, Armonk/NY, USA). The results of the DAP and the direct and scattered organ doses of FP and DR examinations were compared by conducting the paired sample t test. For the comparison of the qualitative reading scores, Wilcoxon signed-rank test was performed. Two-sided p values below 0.05 were considered as statistically significant.
Results
Phantom studies
Phantom dose measurements with the optimized FP protocol allowed for a general dose reduction of approximately 96% per picture as compared to the DR standard (0.004 and 0.12 mGy, respectively).
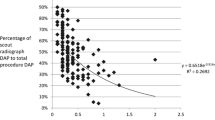
Time-adjusted measurements of the DAP for an examination time of 30 s (according to the mean examination time of 25 ± 12 in the patient study) revealed a dose reduction of approximately 97% for the FP protocol in comparison to the DR protocol (80.8 and 2794.6 μGym2, respectively). Significant dose reductions (FP vs. DR; p ≤ 0.03) were also found for the measured organ doses with negligible low exposure of radiosensitive organs in the scattered beam, such as the eyes (5.6 × 10−3 ± 0.00 and 0.11 ± 0.01; p = 0.02, respectively) and the male (8 × 10−4 ± 0.00 and 0.03 ± 0.00;p = 0.003, respectively) and female gonads (2.4 × 10−3 ± 0.00 and 0.05 ± 0.00; p = 0004, respectively). A summary of all organ dose measurements is given in Table 2.
Patient study
Optimized ultralow-dose digital pulsed fluoroscopy was successfully completed in all 41 patients (10 female, 31 male, age 65 ± 11 years, range 42–85 years) and all studies were considered to be of diagnostic value to allow for a reliable diagnosis. All FP examinations were performed by the same operator (A.P.) with a mean image acquisition time of 25 ± 12 s (range 9–56 s).
Analysis of image quality
The image quality of FP images was rated sufficiently good for a reliable diagnosis with the following reading scores: overall image quality: median 4, range 3–5; delineation of contrast agent: median 4, range 2–5; image noise: median 4, range 3–5 but significantly differing from the DR reference standard for all evaluated parameters (median 5; range 4–5; p < 0.05). Image examples of FP examinations in comparison to the historical DR acquisitions are provided in Figs. 2, 3, and 4.
Discussion
In this study, we investigated the dose exposure and image quality of an optimized ultralow-dose digital pulsed protocol for fluoroscopic examinations of the UGI. We found significantly reduced organ doses in both the direct field of view and in distant radiosensitive organs at a sufficient image quality to ensure a reliable diagnosis.
Due to frequent clinical use, dose saving strategies are mandatory for fluoroscopic examinations of the UGI. This applies in particular to paediatric and obese patients, both commonly undergoing UGI [1, 2]. The first are at particular risk for developing late radiation damage [11, 26, 27], whereas the latter inevitably receive a higher radiation exposure as compared to normal weight patients, due to the larger body profile and images are often of minor diagnostic quality, in particular when the radiation dose is limited to a reasonable extent [28, 29]. With the introduction of new image acquisition and reconstruction techniques (e.g. improved filtering, pulsed acquisition, last image hold) during the last decade, fluoroscopic examinations with a substantially reduced dose expose became possible [20, 21]. Several studies investigating these technical advances are available for diagnostic/interventional procedures of the vascular system [30,31,32] and for examinations of the GI and urogenital tract in paediatric radiology [1, 11, 13]. However, no dedicated research has been performed evaluating the quality standards for UGI examinations in adult patients. With the investigated ultralow-dose protocol comprising the latest hard- and software technologies in this study, we fill this gap by providing an analysis of the image quality and reference organ dose measures for an average adult fluoroscopic UGI examination in clinical routine.
Nevertheless, the results of this study need to be interpreted in the study setting. Although we consider that the presented organ doses as an overview for a standardized UGI examination in clinical routine using modern hard- and software techniques, it is important to remember that these results only apply for the specific protocol settings and detector system used. Other systems and acquisition parameters will affect the actual dose absorbed by radiosensitive organs; thus, our results may only serve as a general guideline and must not be seen as absolute values.
A well-known fact of X-ray imaging regardless of the chosen modality, is to determine a reasonable trade-off between the required image quality for a reliable diagnosis and the radiation burden of the patient. The results of our phantom and patient study indicate that our FP protocol warrants these conditions, as all examinations were considered to be of sufficiently diagnostic image quality at significantly reduced organ doses. In particular, scattered radiation levels in distant organs such as the eyes and gonads were negligibly low, making radiation effects (e.g. cataract development) unlikely, even if repeated examinations are necessary. This dose distribution pattern is in line with Emigh et al., who also conducted a phantom study to investigate dose exposure in paediatric UGI examinations, although a direct comparison is not possible due to their different patient collective and fluoroscopy system [1].
Our study has the following limitations. Images in both protocols were acquired with the highest possible pulse/frame rate/s. This allows for a high temporal resolution, which is of importance to evaluate discreet and subtle findings during the contrast agent passage. On the other hand, depending on the acquisition time, this can result in a considerably high dose exposure, especially with the historical DR protocol. For indications, in which high temporal resolution is not the primary focus of interest, reducing the pulse/frame rate is advisable to further reduce cumulative radiation dose. Moreover, phantom measurements were only performed once for each examination protocol; thus, no information about retest reproducibility is available. In addition, no dedicated image quality phantom was used to compare the examination protocols. Finally, we did not perform a subgroup analysis of obese patients, due to the small number of the included patients.
In conclusion, we established an optimized ultralow-dose digital pulsed fluoroscopy protocol for UGI examinations allowing for a significant dose reduction and provided an analysis of the resulting organ doses and image quality to demonstrate its feasibility for clinical routine.
References
Emigh B, Gordon CL, Connolly BL, Falkiner M, Thomas KE (2013) Effective dose estimation for pediatric upper gastrointestinal examinations using an anthropomorphic phantom set and metal oxide semiconductor field-effect transistor (MOSFET) technology. Pediatr Radiol 43:1108–1116
Chandler RC, Srinivas G, Chintapalli KN, Schwesinger WH, Prasad SR (2008) Imaging in bariatric surgery: a guide to postsurgical anatomy and common complications. AJR Am J Roentgenol 190:122–135
Kulinna-Cosentini C, Schima W, Ba-Ssalamah A, Cosentini EP (2014) MRI patterns of Nissen fundoplication: normal appearance and mechanisms of failure. Eur Radiol 24:2137–2145
Bingham J, Shawhan R, Parker R, Wigboldy J, Sohn V (2015) Computed tomography scan versus upper gastrointestinal fluoroscopy for diagnosis of staple line leak following bariatric surgery. Am J Surg 209:810–814 discussion 814
Margulis AR (1994) The present status and the future of gastrointestinal radiology. Abdom Imaging 19:291–292
Pauli EM, Beshir H, Mathew A (2014) Gastrogastric fistulae following gastric bypass surgery-clinical recognition and treatment. Curr Gastroenterol Rep 16:405
Harmath C, Horowitz J, Berggruen S, Hammond NA, Nikolaidis P, Miller FH et al (2015) Fluoroscopic findings post-peroral esophageal myotomy. Abdom Imaging 40:237–245
Levine MS, Carucci LR (2014) Imaging of bariatric surgery: normal anatomy and postoperative complications. Radiology 270:327–341
LeBedis CA, Penn DR, Uyeda JW, Murakami AM, Soto JA, Gupta A (2013) The diagnostic and therapeutic role of imaging in postoperative complications of esophageal surgery. Semin Ultrasound CT MR 34:288–298
Glennie D, Connolly BL, Gordon C (2008) Entrance skin dose measured with MOSFETs in children undergoing interventional radiology procedures. Pediatr Radiol 38:1180–1187
Miksys N, Gordon CL, Thomas K, Connolly BL (2010) Estimating effective dose to pediatric patients undergoing interventional radiology procedures using anthropomorphic phantoms and MOSFET dosimeters. AJR Am J Roentgenol 194:1315–1322
Lee R, Thomas KE, Connolly BL, Falkiner M, Gordon CL (2009) Effective dose estimation for pediatric voiding cystourethrography using an anthropomorphic phantom set and metal oxide semiconductor field-effect transistor (MOSFET) technology. Pediatr Radiol 39:608–615
Linke SY, Tsiflikas I, Herz K, Szavay P, Gatidis S, Schafer JF (2015) Ultra low-dose VCUG in children using a modern flat detectorunit. Eur Radiol 26:1678–1685
Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB et al (2003) Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci USA 100:13761–13766
Kamiya K, Ozasa K, Akiba S, Niwa O, Kodama K, Takamura N et al (2015) Long-term effects of radiation exposure on health. Lancet 386:469–478
Axelsson B, Boden K, Fransson SG, Hansson IB, Persliden J, Witt HH (2000) A comparison of analogue and digital techniques in upper gastrointestinal examinations: absorbed dose and diagnostic quality of the images. Eur Radiol 10:1351–1354
Chawla S, Levine MS, Laufer I, Gingold EL, Kelly TJ, Langlotz CP (1999) Gastrointestinal imaging: a systems analysis comparing digital and conventional techniques. AJR Am J Roentgenol 172:1279–1284
Goodman BS, Carnel CT, Mallempati S, Agarwal P (2011) Reduction in average fluoroscopic exposure times for interventional spinal procedures through the use of pulsed and low-dose image settings. Am J Phys Med Rehabil 90:908–912
Barkhof F, David E, de Geest F (1996) Comparison of film-screen combination and digital fluorography in gastrointestinal barium examinations in a clinical setting. Eur J Radiol 22:232–235
Mahesh M (2001) Fluoroscopy: patient radiation exposure issues. Radiographics 21:1033–1045
Lin PJ (2008) Technical advances of interventional fluoroscopy and flat panel image receptor. Health Phys 95:650–657
Chau KH, Kung CM (2009) Patient dose during videofluoroscopy swallowing studies in a Hong Kong public hospital. Dysphagia 24:387–390
Schubert R (1995) What is dose area product? Radiol Technol 66:329–330
Staton RJ, Williams JL, Arreola MM, Hintenlang DE, Bolch WE (2007) Organ and effective doses in infants undergoing upper gastrointestinal (UGI) fluoroscopic examination. Med Phys 34:703–710
Samei E, Tian X, Segars WP (2014) Determining organ dose: the holy grail. Pediatr Radiol 44(Suppl 3):460–467
Frush DP, Donnelly LF, Rosen NS (2003) Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics 112:951–957
Brenner DJ (2002) Estimating cancer risks from pediatric CT: going from the qualitative to the quantitative. Pediatr Radiol 32:228–231 discussion 242-224
Carucci LR (2013) Imaging obese patients: problems and solutions. Abdom Imaging 38:630–646
Le NT, Robinson J, Lewis SJ (2015) Obese patients and radiography literature: what do we know about a big issue? J Med Radiat Sci 62:132–141
Nickoloff EL, Lu ZF, Dutta A, So J, Balter S, Moses J (2007) Influence of flat-panel fluoroscopic equipment variables on cardiac radiation doses. Cardiovasc Interv Radiol 30:169–176
Kuon E, Weitmann K, Hummel A, Dorr M, Reffelmann T, Riad A et al (2015) Latest-generation catheterization systems enable invasive submillisievert coronary angiography. Herz 40(Suppl 3):233–239
Heidbuchel H, Wittkampf FH, Vano E, Ernst S, Schilling R, Picano E et al (2014) Practical ways to reduce radiation dose for patients and staff during device implantations and electrophysiological procedures. Europace 16:946–964
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Local IRB approved this study and waived written informed consent.
Funding
This study received no funding.
Rights and permissions
About this article
Cite this article
Weiss, J., Pomschar, A., Rist, C. et al. Feasibility of optimized ultralow-dose pulsed fluoroscopy for upper gastrointestinal tract examinations: a phantom study with clinical correlation. Radiol med 122, 822–828 (2017). https://doi.org/10.1007/s11547-017-0793-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-017-0793-z