Abstract
Mental health conditions are common comorbidities seen in drug overdoses. Evidence has shown substance use disorder (SUD) and mental health conditions often share an origin cause and more successful treatment when addressed together, simultaneously (Buckley, Journal of Clinical Psychiatry, 67, 5, 2006). With fatal overdoses increasing annually and the large prevalence of mental health conditions in Tennessee (TN), our aim was to determine if lack of access to mental healthcare providers was associated with higher fatal overdoses with mental health comorbidities, particularly in rural TN. For our analyses, fatal drug overdoses in all of TN were captured by the State Unintentional Drug Overdose Surveillance System (SUDORS). Hospital Discharge Data System data was then linked to SUDORS cases for deaths among TN residents who had an autopsy between 2019 and 2021. Analysis was limited to decedents with a mental health condition determined through ICD-10 codes and autopsy reports. Descriptive statistics were calculated stratified by rural or urban and geographic mental health professional shortage area (MHPSA) or non-MHPSA based on county of residence. Chi-square tests were conducted to determine differences. Unadjusted and adjusted logistic regression were conducted to determine the relationship between living in a MHPSA and living in a rural county among drug overdose decedents with mental health conditions. We identified 2639 (48.4%) decedents with a mental health condition between 2019 and 2021 out of 5458 total overdoses. Overall, 30.2% of decedents with a mental health condition lived in a MHPSA and 18.6% lived in a rural county. Analyses found that a higher proportion of decedents with a mental health condition lived in a rural MHPSA (37.1%) compared to an urban MHPSA (10.6%). Decedents with a mental health condition in a rural county had greater odds of living in a MHPSA compared to decedents with a mental health condition in an urban county adjusting for age, sex, and race (aOR = 4.68; CI, 3.79, 5.78). Mental health conditions, drug overdoses, and SUDs are closely associated in TN. Rural residents of the state who live in a MHPSA are less likely to have sufficient access to providers to meet their needs. Future research should work to identify ways to reduce barriers to mental healthcare services throughout the state to ensure equity in healthcare access for all.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
According to the National Institute on Drug Abuse, about half of people who experience a mental health condition will also experience a substance use disorder (SUD) at some point in their lives. The reverse is also true; those with a SUD have a higher likelihood of experiencing a mental health condition during their lives (National Institute on Drug Abuse, 2022). In 2021, the Substance Abuse and Mental Health Services Administration (SAMHSA) estimated that 19.4 million adults over 18 years of age had both a SUD and any mental illness (AMI) (Substance Abuse & Mental Health Services Administration, 2022). As mental health diagnoses are common comorbidities seen in overdoses, limited access to mental healthcare services could contribute to higher overall death rates in this population. The US Health Resources & Services Administration (HRSA) defines a Health Professional Shortage Area (HPSA) as an area, population, or facility experiencing a shortage of healthcare services. HRSA estimates that 155 million people in the USA live in a HPSA for mental healthcare services (Health Resources & Services Administration, 2019). Rural areas have disproportionately lower access to mental healthcare services when compared to urban or suburban areas (Morales et al., 2020). It is estimated that as much as 60% of individuals in the rural USA live in designated mental healthcare provider shortage areas (Andrilla et al., 2018).
In 2021, the state of TN had approximately 1,328,000 adults who reportedly had a mental health condition within the last year (SAMHSA, 2023). Furthermore, in 2021, 43.5% of Tennesseans reported having anxiety or depression symptoms and 25.6% were unable to get the care they needed (Kaiser Family Foundation analysis of U.S., 2020). The Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics (NCHS) states that out of the 95 counties in Tennessee (TN), 53 counties (56%) are considered either “non-metropolitan” or rural areas (Ingram et al., 2013). As of 2019, HRSA reported that there were approximately 1,025,711 Tennesseans living in a Geographic Mental Healthcare Provider Shortage Area (MHPSA) (Health Resources & Services Administration, 2019). In 2021, the State Unintentional Drug Overdose Reporting System (SUDORS) recorded that there were 3754 fatal overdoses in the state of TN, a 53% increase from 2019 (Tennessee Department of Health Office of Informatics & Analytics, 2023).
With increases in fatal drug overdoses annually and the relatively large proportion of Tennesseans living with mental health conditions, there is a need to elucidate which populations face the greatest shortage of mental healthcare providers and the impact this may have on fatal drug overdoses to better inform prevention efforts. The purpose of this study is to examine the association between lack of access to mental healthcare services and overdose death rates with mental health comorbidities in TN, with a focus on rural areas.
Methods
The TN Department of Health routinely conducts fatal drug overdose surveillance using SUDORS data. SUDORS uses death certificate data, autopsies, toxicology reports, and Prescription Drug Monitoring Program data (PDMP) to collect over 600 different variables relating to the overdose and the decedent. TN SUDORS, which collects information on the unintentional and undetermined manner of death drug overdoses occurring in TN, is nested within the National Violent Death Reporting System (NVDRS) and is funded by the Overdose Data to Action (OD2A) grant from the CDC. SUDORS overdoses are identified using the International Classification of Disease, Tenth Revision (ICD-10 CM) cause of death codes X40-44, Y10-14, and T36-50. Text search for cause of death fields looking for an overdose term such as “overdose,” or “intoxication,” and drug terms such as “fentanyl,” or “oxycodone” was also used to identify any deaths where codes were not available. All cases were manually reviewed to confirm inclusion (Tennessee Department of Health Office of Informatics & Analytics, 2023)10. Once cases are identified, SUDORS data is abstracted from death certificates, autopsies, toxicology reports, and PDMP and entered into NVDRS.
The purpose of this study was to examine whether there was or was not an association between lack of access to mental healthcare services and overdose death rates with mental health comorbidities in TN, with a focus on rural areas. We used the following methods to quantify an association, if any, and describe the characteristics of the decedents included in this study.
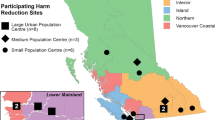
For this analysis, SUDORS data from January 1, 2019 to December 31, 2021 were obtained from our TN SUDORS internal Research Electronic Capture (REDCap) system and deterministically linked with Hospital Discharge Data System (HDDS) and PDMP data to capture more comprehensive information about decedents’ mental health diagnoses and prescription history (Harris et al., 2019; Harris et al., 2009). Demographic variables include age, race, sex, and rural/urban residence. Race, age, and sex were determined using death certificate information. Rural/urban residence was defined using the 2013 National Center for Health Statistics (NCHS) Urban–Rural Classification Scheme codes (Fig. 1). Urban counties were defined as metropolitan counties, subcategorized into large metro, medium metro, and small metro; these counties had populations greater than 50,000. Rural counties were defined as the non-metropolitan and non-core counties; these counties had populations of less than 50,000 (Ingram et al., 2013). The history of a mental health condition was determined through the linkage of HDDS data to SUDORS cases and descriptions of conditions on autopsy reports. Mental health conditions include mood disorders (F30-F39), anxiety disorders (F40-F49), schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders (F20-F29) and eating disorders (F50) coded for in HDDS data or described in SUDORS autopsy reports. These ICD-10 code groups were chosen as they represent a comprehensive number of conditions that develop throughout an individual’s life that may or may not be attributed to life events. SUD was determined using decedent history notated in the autopsy report as abstracted into the SUDORS database and linkage to HDDS data and codes (F11-F16, F18-F19). Prescription history for benzodiazepines and opioids was determined using PDMP data for several time points, including within 30 days of death, within 180 days of death, within 1 year of death, and “ever prescribed,” which includes prescription data back to 2012.
Tennessee NCHS Urban–Rural Classification Map (Ingram et al., 2013)
The US HRSA’s HPSA statistic uses three scoring criteria—population-to-provider ratio, percent of the population below 100% of the Federal Poverty Level, and travel time to the nearest source of care outside the HPSA designation area. HRSA’s geographic HPSA designation identifies a shortage of providers for a group of people within a defined geographic area (Health Resources & Services Administration, 2019). Geographic mental health provider shortage areas (MHPSA) were identified using HRSA geographic designations for the year of death. A county was considered a MPHSA if the county fell into a geographic shortage designated area.
Descriptive statistics were calculated for all variables and stratified by rural or urban residential county and a geographic MHPSA or a non-MHPSA. Analysis was limited to TN residents who had an autopsy report and were able to be linked with HDDS data. Chi-square tests were conducted to determine differences between groups. We then performed unadjusted and adjusted logistic regression to determine the relationship between living in a geographic MHPSA and living in a rural county among drug overdose decedents with a mental health condition. Statistical significance was assessed at α = 0.05. This study was found exempt by the TN Department of Health Institutional Review Board. This analysis was not pre-registered on a publicly available platform and should be considered exploratory. The data that support our findings are available upon request from the Tennessee Department of Health.
Results
From 2019 to 2021, SUDORS captured 8730 fatal drug overdoses in TN. Of these, 8275 were TN residents, and of TN residents, 6230 had an autopsy report used for abstraction. We then identified the subset of 5458 decedents who were able to be linked to HDDS data. Using HDDS and SUDORS data, mental health conditions were seen in 2639 (48.4%) out of these 5458 decedents. All our analyses were limited to these 2639 decedents with mental health conditions (Tables 1, 2, and 3). In decedents with mental health conditions, 81.4% (2149) lived in an urban area and 18.6% (490) lived in a rural area (Table 1). Additionally, 30.2% (796) lived in an MHPSA and 69.8% (1843) did not (Table 2). Almost half of the decedents were female (46.1%) and a large proportion were White race (85.0%). When looking at the history of SUD, 89.6% of decedents with a mental health condition had a SUD (Table 1 and 2). When comparing decedents with a mental health condition in rural vs. urban areas, characteristics were relatively consistent; however, a slightly larger proportion were White race in rural areas (96.1% vs 82.4%) (Table 1). Additionally, when comparing decedents that lived in an MHPSA to those that did not, characteristics again were relatively consistent; however, a slightly larger proportion were White race (90.1% vs 84.0%) (Table 2).
In toxicology, opioids were the most commonly seen drug class in decedents with a mental health condition at 86.7%, followed by stimulants (55.1%), benzodiazepines (35.8%), and antidepressants (31.2%) (Table 1 and 2). Additionally, there were less opioids found on toxicology in decedents with a mental health condition who lived in rural areas when compared to those who lived in urban areas (79.8% vs. 88.3%) (Table 1). This pattern was consistent for decedents in a MHPSA (Table 2). All other drug classes were relatively consistent among both those who lived in rural vs. urban areas and those who lived in an MHPSA vs. those who did not.
In decedents with a mental health condition, mood disorders were the most common at 78.6%, followed by anxiety (74.3%) and schizophrenia (18.8%). Diagnoses remained consistent among those who lived in both rural and urban areas and in both those who lived in a MHPSA and those who did not (Table 1 and 2).
During our prescription history analysis (Table 1 and 2), we were able to link 95% of all decedents with a mental health condition to PDMP data. We found that prescriptions for an opioid within the last 30 days before death were more common for decedents with a mental health condition who lived in a rural vs. an urban area (19.7% and 12.6%, respectively, p-value = 0.0001) (Table 1), as well as in a MHPSA vs. a non-MHPSA (18.6% and 11.9%, respectively, p-value = 0.0001) (Table 2). Prescriptions for opioids in all other time periods were relatively consistent among decedents with a mental health condition in rural and urban areas, as well as in those who lived in a MHPSA and those who did not. When assessing benzodiazepine prescriptions by rural and urban residence, more decedents in rural counties were prescribed benzodiazepines within the last 180 days before death or since 2012 (19.9% vs. 16.0% and 46.6% vs. 39.4%) (Table 1). This was consistent for decedents in a MHPSA vs. non-MHPSA (18.6% vs. 15.9% and 46.0% vs 38.5%) (Table 2).
While MHPSAs alone did not account for a higher proportion of fatal drug overdoses with known mental health conditions, when stratified by type of county (rural vs. urban), we found that the proportional increase of decedents in rural MHPSA’s was statistically significant (Table 3). Decedents with a mental health condition in a rural county have greater odds of living in a MHPSA compared to decedents with a mental health condition in an urban county adjusting for age, sex, and race (aOR = 4.68; CI, 3.79, 5.78).
Discussion
For individuals with a known mental health condition, our analyses found a more than fourfold increase in the odds of a fatal drug overdose when living in a MHPSA in a rural county compared to an urban county in TN. A possible explanation for the difference between urban and rural MHPSAs may be that urban counties are clustered together around the state, potentially making it easier to reach mental healthcare providers in these areas. Even though one urban county may be considered a MHPSA, its distance to other urban counties that are not MHPSAs may be closer when compared to rural counties that are often more isolated and sprawling.
Demographic results of our analysis were intriguing. When not limited to decedents with a mental health condition, a higher proportion of drug overdose decedents in TN are generally males (Tennessee Department of Health Office of Informatics & Analytics, 2023); however, in our analysis, limited to decedents with a mental health condition, the proportion of females and males was relatively equal in both rural and urban areas and MHPSAs and non-MHPSAs. A possible explanation is that females are more likely to seek care for mental health conditions than males. Additionally, this could also indicate a gender disparity in mental healthcare for females, as many studies show an unmet need for health services for women when compared to men (Manuel, 2018). When considering race, non-Hispanic Black decedents tended to live in urban areas and non-MHPSAs. This corresponds with data showing Black individuals more often live in urban areas (Johnson & Lichter, 2020). Non-Hispanic Black decedents comprised a small proportion of decedents with mental health conditions in our data; however, non-Hispanic Black individuals have more barriers to care when compared to White individuals (Manuel, 2018). The protective effect of non-Hispanic Black decedents with a mental health condition in our study could be due to inequity in access to care.
Evidence was found in the literature that shows co-occurrence of mental health conditions and SUD, both in the USA and internationally (Buckley, 2006). This comorbidity has shared indicators, such as Adverse Childhood Events (ACE), which has been a predictor of both SUD and mental health conditions alone and in tandem (Merrick et al., 2017). Additionally, evidence exists suggesting self-medication is a factor in individuals with mental health conditions whereby illicit substances and non-prescribed pharmaceuticals are used in lieu of professional treatment for their conditions (Merrick et al., 2017). In 2021, the Substance Abuse and Mental Health Services Administration (SAMHSA) estimated that 19.4 million adults over 18 years of age had both a SUD and any mental illness (AMI) (Substance Abuse & Mental Health Services Administration, 2022). SAMHSA defines AMI as having any mental, behavioral, or emotional disorder in the past year of sufficient duration to meet criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV), excluding developmental disorders and SUDs (Substance Abuse & Mental Health Services Administration, 2022). Their evidence suggests that nearly 80% of individuals with a SUD had AMI. These comorbidities are tightly interconnected, both in origin cause and over the life of the conditions, highlighting how crucial access to mental healthcare services can be in aiding the treatment and sequalae, including overdoses, in those with SUDs (Buckley, 2006; Harris et al., 2019; Substance Abuse & Mental Health Services Administration, 2022; Tomko et al., 2022).
Few articles currently exist that examine the potential associations between access to mental healthcare providers and unintentional fatal drug overdoses. However, Tomko et al. examined the risk of unmet mental health need and the risk of non-fatal overdoses in individuals who use opioids non-medically (Tomko et al., 2022). The National Survey on Drug Use and Health (NSDUH) defines an unmet mental health need as an individual feeling a perceived need for mental healthcare but being unable to access it. They found that nearly 50% of the individuals they assessed reported an unmet mental health need. Geographic barriers are included in their definition of potential limitations to accessing mental healthcare services (Tomko et al., 2022). Our analyses further suggest that lack of geographic access to mental healthcare may serve as an indicator for fatal drug overdoses in individuals with known mental health conditions.
During our prescription analysis, we found that prescriptions for an opioid within the last 30 days before death were more common for decedents with a mental health condition who lived in a rural vs. an urban area, as well as in a MHPSA vs. a non-MHPSA. This is consistent with prior research showing higher rates of opioid prescriptions and non-medical use of opioids in rural areas when compared to urban areas (Keyes et al., 2014; Oliva et al., 2023). However, our toxicology data showed lower proportions of opioids on toxicology in rural and MHPSAs. This was contrary to the other substance classes which were relatively even. Prescribing patterns in these areas could be impacting which substances people choose to use. Overlapping prescriptions for opioids and benzodiazepines were more prevalent in rural counties as well as MHPSAs. This is concerning given the known risk of overlapping prescriptions (Sprunger et al., 2022). However, the prescriber’s rationale or the venue in which they were prescribed is unknown. Given that the majority of cases with a mental health condition had a history of substance use disorder (89.6%) and that we found opioids in 86.7% of decedents’ toxicology, it was concerning to find over 60% of decedents in MHPSAs had ever been prescribed an opioid since 2012. The lower percentages for more recent prescriptions suggest that prescription drug monitoring programs may be helping to limit unnecessary prescribing. Lack of differences in the remaining prescribing patterns, except for those found in overlapping benzodiazepines and opioids between rural and urban counties and MHPSAs and non-MHPSAs, suggests that access to prescriptions may not be a factor in fatal overdoses among individuals with a mental health condition. Instead, results point to living in a MHPSA as a more substantial indicator of fatal overdose in a rural county. Future research should focus on eliminating barriers in access to care and evaluating appropriateness of overlapping benzodiazepine and opioid prescriptions. Continued monitoring and increasing prescriber awareness of commonly misused prescriptions in populations with known mental health conditions and SUD is crucial to help prevent overdoses in the future.
Mental health conditions are often associated with SUD. The treatment of both is often interconnected—mental healthcare providers can serve as crucial lifelines for those struggling with mental health conditions and SUD. Our analyses suggest that rural MHPSAs could serve as an indicator for fatal drug overdoses with mental health conditions, further highlighting the importance of access to mental health providers in combatting substance use and fatal drug overdoses.
Limitations
Our analysis had several limitations. The SUDORS variable that is coded for decedents with a mental health comorbidity relies on either next of kin’s reporting of the condition or known medical history found during autopsy investigation. To address this limitation, we linked SUDORS records to HDDS records to identify mental health diagnoses more comprehensively. Additionally, because TN is a decentralized state, there is a lack of autopsy standardization across our five regional forensic centers. This may lead to underreporting in both cases due to a lack of next of kin’s knowledge of a mental health condition or autopsy investigation not reporting mental health history. The deterministic linkage of HDDS to SUDORS data is not seamless and matches may be missed. Additionally, there is a vast underreporting of mental health conditions as not all individuals seek care for their condition. HDDS data is not inclusive of an individual’s entire medical record. Our analysis is limited to decedents who were able to be linked to HDDS data which may not be representative of all accidental or undetermined fatal drug overdoses in TN. Despite these limitations, evidence uncovered in our investigation should serve as a call to action for additional research into how lack of access to mental healthcare providers can affect trends in fatal drug overdoses.
Conclusion
Mental health conditions, drug overdoses, and SUDs are closely associated in TN. Rural residents of the state who live in a MHPSA are less likely to have sufficient access to providers to meet their needs. Future research should work to identify ways to reduce barriers to mental healthcare services throughout the state to ensure equity in healthcare access for all Tennesseans.
References
Andrilla, C., Holly A. et al. (2018). “Geographic variation in the supply of selected behavioral health providers.” American journal of preventive medicine 54.6 (2018): S199-S207. https://www.sciencedirect.com/science/article/pii/S0749379718300059
Buckley, P. F. (2006). Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. Journal of Clinical Psychiatry, 67, 5.
Catherine Tomko, Kristin E. Schneider, Saba Rouhani, Glenna J. (2022). Urquhart, Ju Nyeong Park, Miles Morris, Susan G. Sherman, Identifying pathways to recent non-fatal overdose among people who use opioids non-medically: How do psychological pain and unmet mental health need contribute to overdose risk?, Addictive Behaviors, 127 107215, ISSN 0306–4603, https://doi.org/10.1016/j.addbeh.2021.107215. (https://www.sciencedirect.com/science/article/pii/S0306460321004007)
Harris, P. A., Taylor, R., Minor, B. L., et al. (2019). REDCap Consortium, The REDCap consortium: Building an international community of software partners. Journal of Biomedical Informatics, 95(1), 103208.
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–81.
Health Resources and Services Administration. (2019). Designated health professional shortage areas statistics. Bureau of Health Workforce. U.S. Department of Health and Human Services [Internet].
Ingram, Deborah D., and Sheila J. Franco. (2013). NCHS urban-rural classification scheme for counties. No. 2014. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, 2014.
Johnson K, Lichter D. Growing racial diversity in rural America: Results from the 2020 census. University of New Hampshire Carsey School of Public Policy. https://carsey.unh.edu/publication/growing-racial-diversity-in-rural-america
Kaiser Family Foundation analysis of U.S. Census Bureau, [Household Pulse Survey, 2020, Phase 3: 1/20/2021–2/1/2021] (https://www.kff.org/statedata/mental-health-and-substance-use-state-fact-sheets/)
Keyes, K. M., Cerdá, M., Brady, J. E., Havens, J. R., & Galea, S. (2014). Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health, 104(2), e52–e59. https://doi.org/10.2105/AJPH.2013.301709
Manuel, J. I. (2018). Racial/ethnic and gender disparities in health care use and access. Health Services Research, 53(3), 1407–1429. https://doi.org/10.1111/1475-6773.12705
Morales, D. A., Barksdale, C. L., & Beckel-Mitchener, A. C. (2020). A call to action to address rural mental health disparities. Journal of Clinical and Translational Science, 4(5), 463–467. https://doi.org/10.1017/cts.2020.42
Melissa T. Merrick, Katie A. Ports, Derek C. Ford, Tracie O. Afifi, Elizabeth T. Gershoff, Andrew Grogan-Kaylor, Unpacking the impact of adverse childhood experiences on adult mental health, Child Abuse & Neglect, Volume 69, 2017, Pages 10–19, ISSN 0145–2134, https://doi.org/10.1016/j.chiabu.2017.03.016. (https://www.sciencedirect.com/science/article/pii/S0145213417301084)
National Institute on Drug Abuse (2022). Part 1: The connection between substance use disorders and mental illness. https://nida.nih.gov/publications/research-reports/common-comorbidities-substance-use-disorders/part-1-connection-between-substance-use-disorders-mental-illness
Oliva, A., González de Chavez, P., Dévora, S., & Abdala, S. (2023). Opioid prescription patterns in the province of Las Palmas, Canary Islands, Spain (2016–2020): Differences between urban and rural areas. Frontiers Pharmacology, 14, 1184457. https://doi.org/10.3389/fphar.2023.1184457
SAMHSA. (2023). 2021 National Survey on Drug Use and Health: Model-based estimated totals (in thousands) (50 states and the district of Columbia) (https://www.samhsa.gov/data/sites/default/files/reports/rpt39466/2021NSDUHsaeTotals121522/2021NSDUHsaeTotals121522.pdf)
Sprunger, J. G., Johnson, K., Lewis, D., Kaelber, D. C., & Winhusen, T. J. (2022). Five-year incidence of substance use and mental health diagnoses following exposure to opioids or opioids with benzodiazepines during an emergency department encounter for traumatic injury. Drug and Alcohol Dependence, 238, 109584. https://doi.org/10.1016/j.drugalcdep.2022.109584
Substance Abuse and Mental Health Services Administration. (2022). Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health (HHS Publication No. PEP22-07-01-005, NSDUH Series H-57). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/report/2021-nsduh-annual-national-report
Tennessee Department of Health Office of Informatics and Analytics. (2023). Tennessee State Unintentional Drug Overdose Reporting System (SUDORS) Report 2023. https://www.tn.gov/content/dam/tn/health/documents/pdo/sudors/SUDORS_Annual_Report_2023.pdf
Acknowledgements
The authors would like to thank Jenna S. Moses and Kate Durst for their insightful reviews of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kristi F. Hall has received the CDC Overdose Data to Action grant [5 NU17CE924899] from the Centers for Disease Control and Prevention.
Jessica Korona-Bailey has received the CDC Overdose Data to Action grant [5 NU17CE924899] from the Centers for Disease Control and Prevention.
Sutapa Mukhopadhyay has received the CDC Overdose Data to Action grant [5 NU17CE924899] from the Centers for Disease Control and Prevention.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hall, K.F., Korona-Bailey, J. & Mukhopadhyay, S. Access to Mental Healthcare Providers as an Indicator for Fatal Drug Overdoses in Rural Tennessee, 2019–2021. Int J Ment Health Addiction (2024). https://doi.org/10.1007/s11469-024-01244-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-024-01244-w