Abstract
This study assessed trends in provision of trauma-specific services, defined as dedicated programming for persons with a history of trauma, in US Substance Use Disorder (SUD) and other Mental Health (MH) facilities. Facility level data from the National Survey of Substance Abuse Treatment Services and the National Mental Health Services Survey (2015–2019) were used to examine trends in provision of trauma specific-services. Trauma specific service provision trended up significantly between 2015 and 2019. In 2019, they were more commonly offered at MH facilities (49.9%) than SUD facilities (42.7%). Licensing by state SUD authorities were associated with provision of trauma-specific services at both MH (Adjusted Odds Ratio (AOR) = 1.23, 95% Confidence interval (CI) = 1.18–1.47, p < .001) and SUD (AOR = 1.19, 95% CI = 1.04–1.37, p = .012) facilities. The proportions of facilities that offer trauma-specific services were correlated within states (Pearson’s r = .44, p = .001). State policies to implement trauma screening at public facilities were associated with higher odds of offering trauma-specific services in MH (AOR = 1.31, 95% CI = 1.04–1.64, p = .021) and SUD (AOR 1.51, 95% CI = 1.19–1.12, p = .001) facilities; whereas, state implementation of trauma-specific CBT at public facilities was associated with higher odds of this outcome only in MH facilities (AOR = 1.23, 95% CI = 1.01–1.51, p = .043). Although trauma-specific services trended up significantly, fewer than half of treatment facilities offer such services nationally. Certain facility characteristics, such SUD authority certification, are associated with trauma-specific services. Variability among states in these services is linked to state policy. Increased efforts by states may be an effective point of intervention to further disseminate trauma-specific services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been an increase of awareness of the prevalence of and negative health impact of both childhood [1,2,3] and adult [1, 3,4,5,6] trauma, which can occur at individual, family, and community level. Childhood trauma can include physical, sexual, or emotional abuse, physical or emotional neglect [7], household dysfunction [1], and human trafficking [8]. Adult trauma can involve exposure to traumatic events, physical, sexual or emotional abuse [9], and can occur in the context human trafficking, including sex trafficking [10] and labor trafficking [8]. A variety of strategies to mitigate such effects have been proposed [11] and Substance Abuse and Mental Health Services Administration (SAMHSA) has taken a lead role at the federal level in disseminating these strategies [9, 12].
SAMHSA’s concept of trauma specific services was based on works by Fallot and Harris [11, 13] which differentiated trauma-specific services from trauma informed care in general [14]. Trauma-informed care is a treatment philosophy that takes traumatic experiences into account in all aspects of care, and promotes healing and recovery. While the trauma-informed approach highlights the importance of trauma in treatment, it does not explicitly mandate use of specific interventions.
Trauma-specific services focus on treating effects of trauma [14] and include evidenced based screening, assessment, treatment, and recovery aspects [13]. Examples of specific therapeutic approaches can include exposure therapy, therapy targeted at dissociative symptoms, and teaching coping strategies for dealing with powerful emotions [11, 14].
Prior research has shown that although there are effective ways to manage the impact of certain type of trauma [15, 16], survivors of trauma do not often seek trauma-specific services [17] due to a variety of barriers [18], including trouble finding such services [17]. Trauma is particularly common in individuals with SUD and other MH disorders [19]. Up to 75% of men and women in substance use disorder treatment and close to 90% of individuals in mental health treatment report a history of trauma [19]. Furthermore, 6% of the population develop PTSD at some point in their lives [20]. Trauma-specific services can be offered in both Substance Use Disorder (SUD) and other mental health (MH) treatment facilities. These two treatment systems have historically been separate in the US, and SUD facilities have served a different patient population than their MH counterparts [21]. Furthermore, SAMHSA maintains separate directories for the two types of facilities. Regardless of setting, relatively little is known about trends in availability of trauma-specific services among US treatment facilities.
To address this gap in research we examined data from the SAMHSA’s National Mental Health Services Survey (N-MHSS) and the National Survey of Substance Abuse Treatment Services Survey (N-SSATS) in order to assess the trends in, prevalence of, and correlates of trauma-specific services in the two treatment settings. We additionally examined the association of state characteristics in promoting trauma screening and treatment reflected in the state profiling data collected on behalf of SAMHSA, with offering trauma-specific services in SUD and other MH facilities across the states.
Methods
Data Sources
SUD facility data were obtained from SAMHSA’s N-SSATS [22]. The N-SSATS is a self-report national survey, completed by facility administrators, that assesses SUD health facility characteristics and available services. Facilities eligible for participation were “all facilities in the United States, both public and private, that provide substance abuse treatment” other than prisons and department of defense facilities [21] SAMHSA staff assists sites in completing surveys and to address inconsistent or missing data [21]. Respondents were asked to indicate whether their facility offers trauma-specific services, defined as programming specifically tailored or dedicated to individuals with a history of trauma. The response rate in 2019 was 91.4% (n = 16,275), although 15,961 facilities were included in the data as some facilities were ineligible, and 15,852 were included in the analyses due to missing data.
Facilities were identified as primary MH or primary SUD for the purposes of this survey to avoid double counting facilities.
Facility characteristics included treatment setting (inpatient, residential, partial hospitalization, outpatient), ownership (private-for-profit, non-profit, public), facility funding sources, and licensing/accreditation (including Joint Commission, state authorities, and health departments). Only facility characteristics available in both surveys were included in the analyses.
Questions regarding trauma-specific services were included in N-SSATS and N-MHSS starting in 2015. Therefore, only surveys for years 2015, 2016, 2017, 2018, and 2019 (the latest available data) were included. The following question was posed as part of the survey “Does this facility offer a mental health treatment program or group designed exclusively for clients in the following categories,” with available options for individuals who have experienced trauma. The survey further clarifies that if a facility treats clients in those categories, but does not offer tailored or exclusive programming, the respondent should not give a positive response to this question.
MH facility data were obtained from SAMHSA’s National Mental Health Services Survey (NMHSS) [23]. Similar to N-SSATS, the N-MHSS is a self-report nationwide survey of MH facility characteristics and available services. Facilities eligible to participate included “any facility that provide mental health services to people with mental illness” other than prisons and Department of Defense facilities, identified from a SAMHSA maintained facility inventory [22]. The questions were similarly worded in N-SSATS and N-MHSS, though the N-MHSS further broke down trauma-specific services into PTSD and non-PTSD. For the purposes of N-MHSS analyses, the two variables were merged to improve comparability to the N-SSATS variable. The data waves from the NMHSS corresponded to those of the NSSATS. The response rate in 2019 was 91% (n = 12,712), but 12,384 facilities were included in the analyses due to missing data. Facility characteristics mirrored those in the N-SSATS. Similar to the N-SSATS, trauma-specific service information was included starting in 2015.
State regulatory data were obtained from the state profiling system, which is a national system of annual standardized behavioral health data reported via survey by state behavioral health administrators, collected on behalf of SAMHSA [24]. Administrators were asked whether their states were implementing requirements related to screening for trauma at public facilities, and, if so, what instruments were being used. Administrators were additionally asked whether trauma-focused cognitive behavioral therapy was being implemented at public facilities in that state, and whether fidelity of implementation of trauma-focused cognitive behavioral therapy was being assessed by the state. The latest policy data available was from 2015, which was used for this study. These data were used to test for possible association of state initiatives, including implementation of screening for trauma and implementation of trauma-specific cognitive behavioral therapy (CBT) among public facilities in each state with trauma-specific service offerings in all facilities in that state in 2019.
All data used in this study are publicly available and no individuals or facilities were identified. As such, IRB approval was not required.
Statistical analyses
Analyses were conducted in 5 stages. First, trends in trauma-specific services at both SUD and MH facilities across multiple waves were assessed using linear regression with Newey-West standard errors, which correct for autocorrelation across survey waves [25].
Second, geographic distribution of available trauma-specific services at SUD and MH facilities was explored. Additionally, we tested for a possible correlation between proportion of trauma-specific services in MH and SUD facilities by state.
In the third stage, we tested for possible association of various available facility characteristics and availability of trauma-specific services at SUD and MH facilities in 2019.
In the fourth stages, we linked state profiling data to assess the relationship between state regulation that public facilities screen for trauma and availability of trauma-specific services in SUD and MH facilities in that state.
Finally, using linked state profiling data, we tested for possible associations of implementation of trauma-specific CBT and availability of trauma specific services at both facility types.
Analyses of correlates of offering trauma specific services were conducted using Generalized Estimating Equations regressions with a logit link and exchangeable correlation matrix, to account for clustering within states. Analyses were adjusted for facility characteristics. All analyses were conducted using SPSS version 23 software (IBM Corp. ©, 2015).
Results
Trend Analysis
Among SUD facilities, 42.7% offered trauma specific services in 2019, up from 32.4% in 2015 (Fig. 1). This trend was significant (Newey-West b = 2.46, 95%CI = 1.86–3.06, p = .001; data not shown). Among MH facilities, 49.9% offered trauma-specific services in 2019, up from 33% in 2015 (Fig. 1). This trend was similarly significant (Newey-West b = 4.36, 95% CI = 2.37–5.99, p = .003; data not shown).
Geographic Distribution
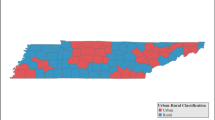
Geographic distribution of facilities offering trauma-specific services showed considerable variability between states. The proportion of SUD facilities offering trauma-specific services was under 50% in most states (Fig. 2a). Similarly, the proportion of MH facilities offering trauma-specific services was under 50% in most states (Fig. 2b). The proportion of SUD facilities offering trauma-specific services exceeded 60% in only 2 states; this rose to 5 states for MH facilities (Fig. 2a, Fig. 2b). There was a significant correlation between availability of trauma-specific services in SUD and MH facilities within states (Pearson’s r = .44, p = .001; data not shown).
a State proportion of Mental Health (MH) treatment facilities that offer trauma-specific services (Source: 2019 National Mental Health Services Survey; number of states in parentheses). b State proportion of Substance Use Disorder (SUD) treatment facilities that offer trauma-specific services (Source: 2019 National Survey of Substance Abuse Treatment; number of states in parentheses)
Facility Correlates
Among SUD treatment facilities, trauma-specific services were more commonly offered at residential (AOR = 2.27, 95% CI = 1.89–2.73, p < .001), partial hospitalization (AOR = 1.77, 95% CI = 1.50–2.09, p < .001), and outpatient (AOR = 1.57, 95% CI = 1.31–1.88, p < .001) setting (Table 1). Accepting state insurance (AOR = 1.21, 95% CI = 1.07–1.36, p = .003) and military insurance (AOR = 1.16, 95% CI = 1.04–1.29, p = .008) were associated with higher odds of offering trauma-specific services. State MH authority certification (AOR = 1.31, 95% CI = 1.19–1.48, p < .001) and State SUD authority certification (AOR = 1.19, 95% CI = 1.04–1.37, p = .012) were also associated with higher odds of offering trauma specific services (Table 1).
Among MH treatment facilities, trauma-specific services were more commonly offered in residential (AOR = 1.38, 95% CI = 1.16–1.64, p < .001) and outpatient (AOR = 1.53, 95% CI = 1.27–1.84, p < .001) settings and less commonly on the inpatient setting (AOR = .74, 95% CI = .60-.90, p = .003; Table 1). Non-profit (AOR = .78, 95% CI = .62-.98, p = .035) and public (AOR = .75, 95% CI = .58-.95, p = .019) facilities had lower odds of offering these services compared to private facilities. Facilities that accepted Medicare (AOR = .62, 95% CI = .53-.74, p < .001) and facilities that accepted self-pay (AOR = .75, 95% CI = .64-.89, p.001) also had lower odds of offering trauma-specific services. Accepting state insurance was associated with higher odds of offering trauma-specific services (AOR = 1.42, 95% CI = 1.23–1.63, p < .001). State SUD authority certification (AOR = 1.32, 95% CI = 1.18–1.47, p < .001) was significantly associated with trauma-specific services (Table 2).
State Action
Only 5 states did not have some sort of policy to promote trauma screening at state facilities in 2015. The types of policies were quite variable. Only four states required a specific assessment tool. Texas and Idaho mandated the Adult Needs and Strengths Assessment, which contains a single question about trauma. Idaho used a tool specifically developed for this purpose called the Idaho Standard Assessment tool, which includes a question about trauma. Nevada required SAFE-T, which also includes a question about trauma. Most states simply require that providers inquire about trauma during intake and provide training for interested providers. There was a significant association between state policy to promote trauma screening in public facilities in 2015 and availability of trauma specific services in SUD facilities (AOR = 1.51, 95% CI = 1.19–1.82, p = .001; data not shown) and MH facilities (AOR = 1.31, 95% CI = 1.04–1.64, p.021) in that state.
In addition to trauma screening, in 2015, 27 states implemented trauma-specific CBT at state facilities, an evidence-based trauma-specific service. Implementation of trauma-specific CBT by states was associated with increased odds of offering trauma-specific services among MH facilities in that state (AOR = 1.23, 95% CI = 1.01–1.51, p = .043; data not shown). There was no association among SUD facilities. We additionally tested for any association of state fidelity monitoring of trauma-specific CBT and trauma-specific services in states offering those services, but found no such relationship.
Discussion
There has been a rapid expansion of trauma-specific services among US SUD and MH facilities between 2015 and 2019 and the rate of expansion is seemingly accelerating, particularly among MH facilities. While this is quite encouraging, even in 2019, less than half of facilities of either type offered such services, suggesting substantial room for growth.
Examination of facility characteristics reveals that trauma-specific services are more common among SUD and MH outpatient and residential facilities, which is encouraging as most care does occur in outpatient settings. The finding that trauma-specific services are common among residential SUD facilities is particularly encouraging given the relative importance of residential treatment in SUD treatment in general. The finding that trauma-specific services are less common among inpatient MH facilities is unfortunate, as there is evidence that early initiation of trauma-specific services can lead to improvement in patients with a history of trauma [26]. Fortunately, this finding was not present among inpatient SUD facilities. From a regulatory standpoint, efforts to increase availability of trauma-specific inpatient MH services may make a meaningful difference.
Among MH facilities, private ownership is most commonly associated with provision of trauma-specific services compared to other types of ownership, though more often than not, non-profit and public facilities also offer trauma-specific services. This finding is not replicated among SUD facilities.
The finding that accepting Medicare lowers the odds of providing trauma-specific services among MH facilities is puzzling given the focus of federal entities on enhancing trauma services 1 and efforts by SAMHSA to disseminate and enhance trauma specific services [12]. It could signal a need to expand trauma-specific services among Medicare recipients, especially persons with disabilities, who may be more likely to experience trauma [27]. Fortunately, this finding was not mirrored among SUD treatment facilities. Similarly puzzling was the lack of association between accepting military insurance and odds of providing trauma-specific services among MH facilities, given the widely understood increased exposure to trauma among military personnel. However, the direction of the association was positive, if not significant. It is plausible that some trauma-specific services are available to military personnel and their families in settings not captured by the N-MHSS. Encouragingly, accepting military insurance did increase the odds of provision of trauma-specific services among SUD facilities.
The results of this study highlight the wide variability in geographic distribution of trauma specific services by state, as well as the importance of states’ role in increased provision of trauma-specific services. The significant correlation in availability of trauma-specific services between SUD and MH facilities within states highlights the overall importance of state policies. State certification likely plays a substantial role in dissemination of trauma-specific services, particularly among MH facilities, which strongly suggests a connection to state regulatory environment. Furthermore, facilities that accept state insurance more commonly offer such services, suggesting a link to state funding.
Our findings also highlight the marked variability in state efforts to improve trauma services and the work that is still needed. While most states support universal trauma screening, the nature of such screening varies widely among states. Identifying and training providers, especially in underserved rural areas, would be important first steps. This is supported by data from the Veterans Affairs health system, which began by training large numbers of providers in screening and delivery of care for individuals with a history of trauma, leading to significant increase in availability [28]. More work is needed to standardize the approach of screening for trauma and to imbed use of validated tools in such screening. State efforts to disseminate services also vary widely. For example, only about half of states implement trauma-specific CBT at state facilities, yet promoting such services affects many other facilities in that state. Promoting evidence-based practices with rigorous fidelity monitoring for most, if not all facilities in that state should be the goal for each state, and this can likely be achieved by direct state action. Standardization in psychotherapy training, including particular attention to populations who more commonly experience trauma (such as individuals with SUD), could also improve access to appropriate treatment.
There are notable limitations in this study. First, both the N-MHSS and the N-SSATS are self-report surveys, which may have affected the quality of the data. However, SAMHSA makes every effort to assist administrators in completing the surveys and addresses missing and inconsistent data. Furthermore, the wording of questions in the two surveys was similar, but not identical, necessitating separate analyses of the two datasets. Second, only 5 years of data regarding trauma-specific services were available, limiting the trend analysis. Third, SAMHSA uses broad and inclusive language in survey questions and informational materials, thus the true prevalence of trauma-specific services may be lower than reported here. Similarly, the N-MHSS and the N-SSATS did not assess the different trauma-specific modalities, opting for a broad overview of availability of such specialized services. Future research should focus on prevalence and correlates of different trauma-specific services. Fourth, the facility surveys do not assess the quality or exact method of delivery of services offered, the participation rate by patients, or the qualifications of providers. Finally, the present study only addresses dedicated and specialized services and does not examine trauma components of other types of mental health services (for example trauma therapy that can occur during typical treatment), nor does it assess facility capacity to provide trauma-informed care. Additionally, availability of trauma-specific services offered outside of the context of treatment facilities is unknown. However, this study includes close to 30,000 US facilities and is likely representative of the state of trauma-specific services nationwide.
Conclusion
Despite the rapid expansion of availability of trauma-specific services in the last 5 years, significant work remains as fewer than half of the treatment facilities of either type offered such services in 2019. The association of trauma-specific services with state licensing and state insurance funding, as well as with state policies regarding implementation of trauma screening and trauma-specific CBT among state facilities highlights the significance of the state action and funding in disseminating trauma-specific services and increasing the quality of such services. These findings call for action by state legislators and state behavioral health authorities to promote further dissemination of and enhancement in the quality of trauma-specific services.
References
Flitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experience (ACE) study. Am J Prev Med. 1998;14:245–58.
Chu DA, Williams LM, Harris AW, Bryant RA, Gatt JM. Early life trauma predicts self-reported levels of depressive and anxiety symptoms in nonclinical community adults: relative contributions of early life stressor types and adult trauma exposure. J Psychiatr Res. 2013;47(1):23–32.
Report of the Special Representative and Co-ordinator for Combating Trafficking in Human Beings, Organization for Security and Cooperation in Europe. Human Trafficking for Labour Exploitation/Forced and Bonded Labour: Identification—Prevention—Prosecution. Human Trafficking for Labour Exploitation/Forced and Bonded Labour: Prosecution of Offenders, Justice for Victims.
Lipschitz DS, Kaplan ML, Sorkenn JB, Faedda GL, Chorney P. Asnis, GM Prevalence and characteristics of physical an dsexual abuse among psychiatric outpatients. Psychiatr Serv. 1996;47(2):189–91.
Tsutsume A, Izutsu T, Poudyal AL, Kato S, Murui E. Mental health of female survivors of human trafficking in Nepal. Soc Sci Med. 2008;66(8):1841–7.
Bremner JD, Southwick SM, Darnell A. Charney, DS Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry. 1996;153:369–75.
Glaser D. Emotional abuse and neglect (psychological maltreatment): a conceptual framework. Child Abuse Negl. 2002;26:697714.
About Human Trafficking. Retrieved from https://www.state.gov/humantrafficking-about-human-trafficking/. 10/2020.
Ellsberg M, Jansen HAFM, Heise L, et al. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet. 2008;371(9619):1165–72.
Protocol to prevent, suppress, and punish trafficking in persons, especially women and children, supplementing the United Nations convention against transnational organized crime. United Nations Convention Against Transnational Organized Crime and the Protocols TheretoNew York, United Nations. 2004:41–52
Berliner L, Kolko DJ. Trauma informed care: a commentary and critique. Child Maltreat. 2016;21(2):168–72.
Substance Abuse and Mental Health Services Administration, National Survey of Substance Abuse Treatment Services (N-SSATS): 2018. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration. 2019.
Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. HHS Publication No. (SMA) 14–4884. Rockville, MD: Substance Abuse and Mental Health Services Administration. 2014
Harris M, Fallot RD. Envisioning a Trauma-informed service system: a vital paradigm shift. New Dir Ment Health Serv. 2001;89:3–22.
Bradley R, Greene G, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005;162:214–227.
Friedman MJ. A guide to the literature on pharmacotherapy for PTSD. Res Q. 2000;11:1–8.
McChesney GC, Adamson G, Sheylin M. Service use patterns and mental health symptoms among adolescents exposed to multiple types of trauma. J Adolesc. 2015;40:1–10.
Kantor V, Knefel M, Lueger-Schuster B. Perceived barriers and facilitators of mental health service utilization in adult trauma survivors. Clin Psychol Rev. 2017;52:52–68.
Rosenberg L. Addressing Trauma in Mental Health and Substance Use Treatment. J Beh Health Serv Res. 2011;38:428.
National Center for Posttraumatic Stress Disorder. https://www.ptsd.va.gov/understand/common/common_adults.asp. Retrieved 31 Mar 2022.
Havassy BE, Alvidrez J, Owen KK. Comparisons of patients with comorbid psychiatric and substance use disorders: Implications for treatment and service delivery. Am J Psychiatry. 2004;161(1):139–45.
Substance Abuse and Mental Health Services Administration, National Survey of Substance Abuse Treatment Services (N-SSATS): 2019. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration. 2019
Substance Abuse and Mental Health Services Administration, National Mental Health Services Survey (N-MHSS). Data on Mental Health Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration. 2019.
NRI/Substance Abuse and Mental Health Services Administration, State profiling system. Available from https://www.nri-inc.org/our-work/projects/state-profiling-system/. Retrieved 9 Dec 2020
Newey WK, West KD. A simple, positive semi-definite, heteroskedasticity and autocorrelation consistent covariance matrix. Econometrica. 1987;1987(55):703–8.
Lampe A, Mitmansgruber H, Gast U, Schüssler G, Reddemann L. Treatment outcome of psychodynamic trauma therapy in an inpatient setting. Neuropsychiatrie : Klinik, Diagnostik, Therapie und Rehabilitation : Organ der Gesellschaft Osterreichischer Nervenarzte und Psychiater. 2008;22(3):189–97.
Young M, Nosek MA, Howland D, Chanpong G, Rintala DH. Prevalence of abuse of women with physical disabilities. Arch Phys Med Rehabil. 1997;78:34.
Rosen CS, Matthieu MM, Sitman Wiltsey S, Cook JM, Landes S, Bernadry NC, Chard LM, Crowley J, Eftekhari A, Filney EP, Hamblen JL, Harik JM, Keghe-Forbes SM, Meis LA, Osei-Bonsu PE, Rodriguez AL, Ruggiero KJ, Ruzek JI, Smith BN, Trent L. Watts BV. A review of studies on the system-wide implementation of evidence-based psychotherapies for posttraumatic stress disorder in the veterans health administration. Admin Policy Menthealth. 2016;43:957–977.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to Participate
No informed consent was necessary as no human subjects were included in the study.
Research Involving Human and Animal Participants
The research does not include human subjects.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Spivak, S., Spivak, A., Decker, M.R. et al. Availability of Trauma-Specific Services in US Substance Use Disorder and Other Mental Health Treatment Facilities: 2015–2019. Psychiatr Q 93, 703–715 (2022). https://doi.org/10.1007/s11126-022-09987-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-022-09987-2