Abstract
While substance use and substance use disorders (SUDs) are increasing in prevalence and severity throughout the United States, a minority of people with SUDs are in formal treatment. The ED is a key site of medical care for patients with SUDs and presents an important opportunity for SUD treatment initiation and linkage to care. Even in a brief clinical encounter, emergency clinicians can have a meaningful impact on patients’ lives through SUD screening and identification, provision of harm reduction services, initiation of and linkage to SUD treatment, and linkage to services to address unmet health-related social needs. SUDs have complex biopsychosocial components and a bidirectional relationship with social determinants of health. Therefore, a comprehensive approach to SUDs must include addressing health-related social needs. Partnering with community organizations, specialty societies, and policy makers, EDs and hospitals can work to address social determinants of health which are related to harmful substance use and present barriers to treatment initiation and retention. In this chapter, we describe a social emergency medicine approach to caring for people with SUDs in the ED, highlight model ED and health system initiatives to address SUD and social determinants of substance use, and outline key structural and social determinants of SUDs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Substance use disorders are complex, biopsychosocial diseases with high rates of morbidity and mortality.
-
Addressing how underlying social determinants of health impact substance use will have the greatest and longest-lasting impact on improving population health.
-
ED substance use initiatives include screening, motivational interviewing, initiation of and/or referral to treatment, and provision of harm reduction services.
-
Patients with substance use disorders may need assistance with health-related social needs in order to achieve successful clinical outcomes and long-term well-being.
-
Professional societies, departments of health, and lawmakers can be key partners to improving care within and across EDs and hospital systems.
Foundations
Background
Emergency medicine providers care for patients with problems related to substance use on a daily basis. Compared to patients in other healthcare settings, adult emergency department (ED) patients have higher rates of substance use, including tobacco, alcohol, non-medical use of prescription medications, and illegal substances [1]. Over the last decade, substance use-related ED visits have significantly increased. From 2006 to 2014, US alcohol-related ED visits rose 61.6%, from 3,080,214 to 4,976,136 annual visits [2]. US ED drug-related visits doubled from 2005 to 2014, in large part due to increasing rates of opioid overdose [3] which increased by 29.7% from 2016 to 2017 alone [4].
Rising substance use-related ED visits are due to increased overall ED utilization, growing prevalence of substance use disorders (SUDs), increased diagnosis and detection of SUDs, and increased SUD severity and lethality of substances used. Both binge drinking and alcohol use disorder (AUD), for example, have increased nationally over the last two decades, especially among older males [5, 6]. There are approximately 88,000 alcohol-related deaths in the US each year, making alcohol the third leading preventable cause of death [7]. From 1999 to 2017, drug overdoses quadrupled and over 700,000 people died [8, 9]. Since 2013, drug overdose deaths due to synthetic opioids other than methadone increased exponentially among people from all races, ethnicities, sexes, and age groups [10]. Most of these deaths involved potent synthetic opioids, specifically fentanyl [11, 12]. While crude overdose death rates have been highest among White people, the highest percent increase in mortality due to synthetic opioids other than methadone has been among non-Hispanic/Latinx Black people. From 2013 to 2017, non-Hispanic/Latinx Black people had an 18-fold increase in overdose mortality, people who identified as Hispanic/Latinx had a 12.3-fold increase, and non-Hispanic/Latinx White people had a 9.2-fold mortality increase [12].
Despite the increasing national prevalence and severity of SUDs, engagement in formal addiction treatment remains low [2, 3, 13,14,15]. In 2018, there were an estimated 21.2 million people over the age of 12—7.8% of the US population—who needed treatment for a SUD, but only about 11.3% of people with a SUD (2.4 million people) received specialty treatment [16]. This treatment gap is due to multiple factors, including stigma and discrimination, limited treatment availability, cost, un- and under-insurance, failure to perceive a treatment need, and unmet health-related social needs [17,18,19,20]. In this chapter, we describe how, as a key interface between the community and the healthcare system, emergency medicine providers have an important opportunity to help close the SUD treatment gap and improve public health by advocating for policies and programs to provide early treatment initiation, reduce treatment barriers, and address health-related social needs.
Evidence Basis
Historically, SUDs have been mischaracterized as moral failings resulting from bad “choices.” Neuroscience research on addiction has demonstrated the neuronal circuitry changes from exposure to alcohol or drugs that result in compulsive substance use despite adverse personal consequences [21]. Advancements in our neurobiological understanding of SUDs now support the treatment of SUDs as chronic diseases. However, SUDs also have complex psychosocial components; they often co-occur with psychiatric conditions and are deeply intertwined with social determinants of health (SDOH). These factors influence not only the development SUDs, but also use-related harm and treatment initiation and retention.
The social determinants of SUDs are complex and vary by individual, geography, and substance, but there are some common associated factors. Housing status, adverse childhood experiences, and exposure to trauma and violence are all associated with substance use and the development of SUDs [22,23,24,25]. ED patients experiencing homelessness, for example, have increased prevalence and severity of substance use compared to ED patients who are stably housed [26]. Other individual-level factors, such as lower level of educational attainment, having low income, and being unemployed, underemployed, or employed in a job with a high risk of injury, such as manual labor occupations, have also been associated with increased rates of substance use and opioid overdose [27, 28]. The rise in deaths among middle-aged, less-educated, working-class White people due to alcoholism, overdose, and suicide—the so-called “deaths of despair”—have been connected to high unemployment, poor job prospects, and widening social inequalities [29,30,31]. The relationship between SUDs and social determinants of SUD is bidirectional and cyclical. For example, just as substance use can result in loss of income, housing, or employment, lack of housing or employment can impair an individual’s ability to successfully engage in SUD treatment and sustained recovery. Due to structural racism, economic opportunities and SUD treatment access and maintenance are even more limited for Black people [32, 33].
Interventions to address SUD in the medical setting have typically focused on individual medical treatment and/or behavior changes. These are important, but addressing the social determinants that underlie substance use will have a greater impact on improving overall population health [34]. A comprehensive approach to addressing SUDs takes into account not only the medical treatment of SUDs, but also health-related social needs and “upstream” SDOH. The socioecological model in Fig. 10.1 outlines key substance use-related factors and multilevel interventions ranging from the individual and intrapersonal levels to organizational, community, and policy spheres. Using an upstream approach to understand SUDs can help inform ED strategies and practices at the bedside as well as broader system-level and community-engaged interventions.
Emergency Department and Beyond
Bedside
While addressing the social determinants of SUDs may have the greatest impact on reducing population-level SUD morbidity and mortality, ED clinicians can have a significant and long-term impact on the health and wellbeing of individuals with SUD even in a brief clinical encounter. A social emergency medicine approach to ED treatment of SUDs entails four basic components: (1) identification of harmful substance use; (2) treatment initiation and harm reduction; (3) referral to treatment; and (4) identifying and addressing health-related social needs.
Many people with SUDs have a prior history of trauma, including physical, emotional, and sexual assault and/or abuse [35,36,37]. Using a trauma-informed approach during the healthcare encounter is key to identifying patients with SUDs and successful patient engagement. This includes awareness of the widespread impact of trauma, recognizing the signs and symptoms of trauma, integrating knowledge about trauma into patient care, and preventing re-traumatization [38, 39]. Providers can avoid re-traumatizing patients by communicating with and caring for patients in a respectful, non-judgmental way that prioritizes a patient’s sense of safety; uses person-centered, de-stigmatizing language; demonstrates provider trustworthiness and transparency; encourages peer support, mutual self-help, and patient empowerment; and incorporates considerations about cultural and historical context, gender, race, sexuality, and economics [38, 40].
Identification of Substance Use Disorders
Many substance use-related ED visits are due to intoxication, acute overdose, injury, suicidality, or injection-related injuries or infections. Other reasons for seeking care include acute exacerbations of chronic conditions related to substance use, such as liver failure from alcoholic cirrhosis. For many ED patients, however, harmful substance use or the presence of a SUD may not be obvious. Given the high prevalence of tobacco, alcohol, and drug use among ED patients overall, many EDs have implemented either universal or targeted substance use screening [41].
Substance use screening, brief intervention, and referral to treatment (SBIRT) interventions have been widely studied for tobacco, alcohol, and other drugs [42]. ED SBIRT interventions can be done by ED clinicians, social work, or drug and alcohol counselors and typically take 5-30 minutes, depending on intervention scope and content [43]. While studies have yielded variable results [41], SBIRT interventions in ED and non-ED settings overall show efficacy for not only reducing consumption of alcohol, tobacco, marijuana, and other drugs (e.g., cocaine, methamphetamine, and heroin) [44], but also substance use-related risk behavior, such as driving while intoxicated [45]. More information about SBIRT can be found through the SAMHSA-HRSA Center for Integrated Health Solutions (https://www.integration.samhsa.gov/clinical-practice/sbirt).
Screening can be targeted or universal and there are several short screening tools that have been adapted for ED use, such as the AUDIT-C [46,47,48], CAGE [49], and NIAAA single-use question [50,51,52]. Early detection and intervention for harmful substance use can prevent SUD development. Screening is especially relevant for adolescents, who may have early or undetected harmful substance use [53]. SBIRT has been widely applied and recommended in pediatrics using the CRAFFT screening tool, which is validated, brief, and developmentally appropriate [54, 55].
Screening paired with motivational interviewing, a patient-centered approach that incorporates a patient’s preferences and choice [56], will inform the type of ED treatment and/or harm reduction services provided and subsequent treatment referral. A positive screen or identification of unhealthy alcohol and/or drug use can be followed by a brief conversation to elicit the patient’s perspective and any steps they might take to be safer and healthier.
Treatment Initiation and Harm Reduction
Medical treatment of toxidromes and withdrawal are routinely taught during residency training to meet basic emergency medicine clinical competencies [57]. As a result, ED clinicians have considerable expertise in the management of intoxication, alcohol withdrawal, and overdose. ED provision of medications for SUD includes nicotine replacement for tobacco cessation and buprenorphine for the treatment of opioid use disorder (OUD) [58,59,60,61]. Naltrexone and acamprosate are effective medications to treat AUD, but their initiation in the ED has not yet been described [62]. After alcohol, tobacco is the next most common substance used among ED patients. ED-provided motivational interviewing and nicotine replacement have been shown to be effective in reducing tobacco use, including among low-income ED patients [63]. In just a few minutes, ED providers can assess for tobacco use, provide smoking cessation counseling, and prescribe nicotine replacement while a person is awaiting admission or upon discharge with referral to outpatient resources [58, 64, 65].
Key ED OUD initiatives include naloxone distribution for overdose rescue, ED initiation of buprenorphine, and behavioral counseling with referral to treatment [66]. Treatment with agonist medications for OUD (MOUD)—specifically buprenorphine and methadone—decreases mortality by more than 50% [67] and has also been shown to reduce overdose and acute care utilization [68]. Currently, however, only a minority of people with OUD are treated with these medications [69]. Receipt of MOUD in the year following an ED visit for an opioid overdose is associated with reductions in all-cause and opioid-related mortality [70]. A single site study of ED-initiated buprenorphine demonstrated a greater likelihood of follow-up at 30 days, decreased self-reported opioid use, and cost-effectiveness [61, 71]. Any prescriber with a DEA license can order buprenorphine for administration in the ED. However, completion of required training and receipt of a Drug Addiction and Treatment Act of 2000 (DATA 2000) waiver is needed to provide patients with a discharge prescription [72]. If a provider does not have a waiver, patients may return to the ED for up to 72 hours to get additional doses of buprenorphine [73, 74]. Providing patients with a prescription for a short course of buprenorphine until they can be seen for outpatient follow-up is preferred. Some EDs use hospital-based bridge programs or low barrier access clinics that stabilize patients on MOUD and link patients to outpatient office-based or opioid treatment programs (OTPs) for ongoing treatment. Other EDs provide referral directly to community-based OTPs or office-based treatment providers [75,76,77]. Success of ED-initiated buprenorphine is dependent on the availability of outpatient office-based buprenorphine providers and OTPs. There is significant variability in access to providers, with large access gaps by geography [17, 78, 79] and race [32]. Telemedicine is one strategy used to try to address gaps in outpatient treatment access [80,81,82,83,84,85].
Harm reduction, an approach which seeks to reduce drug-related harm while respecting individuals’ autonomy, is an essential component of comprehensive SUD care. Intervention cornerstones include syringe services programs and overdose education and naloxone distribution programs. Recommended by the World Health Organization and the Centers for Disease Control and Prevention (CDC), syringe services programs provide sterile injection supplies and teach safe injection practices to individuals who inject drugs, including opioids and methamphetamine. These programs have been shown to reduce HIV and hepatitis C transmission without increasing substance use [86,87,88,89,90,91]. Syringe services programs also provide additional services including HIV and hepatitis C testing, naloxone distribution, personalized support, continuity, and linkage to care. Given these benefits, patients should be referred to syringe services programs for continued harm reduction and support services, if available.
Community overdose education and naloxone distribution programs have been shown to reduce overdose mortality [92,93,94,95]. Naloxone is an opioid antagonist that reverses the effects of an opioid overdose. Naloxone distribution has increased substantially in recent years through community-based harm reduction organizations, public health departments, pharmacies, and other medical and community settings. EDs are increasingly distributing naloxone to patients at risk of opioid overdose [96,97,98,99]. While the liberal distribution of naloxone in EDs is recommended, some particularly high-risk groups include people recently released from prison [100, 101], people who inject opioids or concurrently use opioids and other sedating substances (e.g., benzodiazepines, alcohol) [102], and people with significant co-morbidities such as liver and lung disease [103]. Naloxone can be prescribed by any ED prescriber. Some EDs distribute take-home naloxone kits that include a mouth barrier for rescue breathing and educational materials. All patients at risk of overdose, or who are around individuals at risk of overdose, should be offered naloxone. In states that allow for third party prescribing of naloxone, naloxone can also be provided to family and friends of individuals at risk for opioid overdose [104].
Referral to Treatment
ED SUD screening, motivational interviewing, and referral to treatment can be done by any ED provider. Training in these practices is short and can be easily incorporated into emergency medicine residency training [105,106,107]. Depending on availability, Health Promotion Advocates, peer recovery specialists, substance use navigators, health coaches, or social workers can provide not only treatment referral, but can also help address issues like transportation, insurance coverage, and food and housing insecurity, which are key factors in treatment initiation, engagement, and retention.
One of the earliest examples of these types of programs, Project ASSERT (Alcohol & Substance Use Services, Education, and Referral to Treatment), uses Health Promotion Advocates, who are licensed peer alcohol and drug counselors, to provide substance use assessments and linkage to care. The first Project ASSERT program was started at Boston Medical Center (BMC) ED in 1994. Similar programs have since been implemented at EDs across the US [108,109,110]. Project ASSERT Health Promotion Advocates provide bedside psychosocial assessments, determine the appropriate treatment level of care, and arrange for placement in a continuum of treatment services as well as referrals to community support services. Support services provided include placement in shelters, social peer support referrals, overdose education, and naloxone rescue kits, primary care linkage, transportation assistance, and referrals to the BMC’s food and clothing banks. Patients interested in MOUD or AUD treatment receive same or next-day appointments at the affiliated BMC Faster Paths low-barrier bridge clinic [108, 111].
Some EDs use community-based peer recovery specialists, also known as recovery coaches, to assist with treatment linkage. Peer recovery specialists complete training (and, in some states, a certification exam) about addiction, SUD treatment, trauma-informed care, and motivational interviewing. They use their personal experience to provide individualized peer support to help individuals with SUD identify and remove barriers to treatment, including health-related social needs such as housing, lack of insurance, and lack of sufficient employment or education. Peer specialists can be hired by community-based organizations, departments of health [112], or be hospital-affiliated or employed [113,114,115]. For example, the AnchorED program in Rhode Island [96, 113] is a partnership between hospitals and a community-based organization, Anchor Recovery Community Center. After a patient presents to an ED, consulted AnchorED peer recovery coaches assess patients for readiness for change and provide motivational interviewing, naloxone and overdose prevention education, treatment navigation, and follow-up after an ED visit. Similar models are being increasingly applied in other municipalities and states [112, 116], but effectiveness has yet to be fully assessed [97, 112, 117].
Referral to treatment is best provided by a multidisciplinary team but for EDs that do not have these resources, clinicians can still provide screening, counseling, and referral to treatment. Community treatment services can be found using SAMHSA’s National Helpline (1-800-622-HELP [4357]) or their online treatment locator: https://findtreatment.samhsa.gov/. Local peer support groups can also be found through Alcoholic Anonymous (www.aa.org), Narcotic Anonymous (www.na.org), or SMART Recovery (Self-Management and Recovery Training at www.smart.org)
Identifying and Addressing Health-Related Social Needs
Because social needs impact substance use and access to SUD treatment, comprehensive ED initiatives to address SUDs must simultaneously address unmet social needs. At the time of an ED visit, individual-level assistance with housing, food insecurity, transportation, or health insurance can be provided. As these may be key barriers to accessing addiction treatment, assistance with these factors from the ED can help facilitate successful outpatient treatment engagement and retention. This may include the provision of services from the ED or referral to community resources. In 2019, the American College of Emergency Physicians (ACEP) recognized the importance of addressing social needs in the ED by passing a resolution endorsing staffing EDs with social workers [118]. Furthermore, hospitals and healthcare systems can develop infrastructure to assist patients with insurance enrollment, healthcare, and social services navigation, providing any needed clothing, jackets, or shoes, and provision of transportation vouchers and/or assistance to help patients attend outpatient follow-up appointments [119, 120]. As is discussed in greater detail below, housing is a key area of need for many patients with SUDs. For individuals with SUDs, referrals to Housing First programs—housing for individuals experiencing homelessness without prerequisites around sobriety or completion of SUD treatment [121,122,123]—may be preferred to programs that require abstinence.
Hospital/Healthcare System
Health and hospital systems as well as professional societies can encourage departments of health and state and local governments to make systemic and policy changes to that would ultimately improve care for ED patients with SUDs and address their unmet social needs. Emergency physicians have led such efforts across the US. Parity for SUD treatment under the Affordable Care Act has improved access to care, but significant barriers remain, largely related to gaps in treatment availability, challenges in addressing concurrent unmet social needs, and pervasive stigma [124, 125]. Black, Indigenous, and people of color (BIPOC) [33, 126,127,128], women [129], residents of rural areas [17, 78, 130, 131], and low-income individuals [125, 132] have lower initiation and maintenance of addiction treatment. In areas with limited addiction medicine provider availability [32, 79], telemedicine is being used to fill treatment gaps by providing either direct services or behavioral interventions [81], patient to provider communications, or enhancing the capacity of local providers to provide treatment for SUDs [133, 134]. However, these services can require ongoing access to the internet and/or smartphones, which may be cost-prohibitive or unavailable for some low-income individuals and people living in rural areas, who may be in most need of these services [135,136,137,138].
Reimbursement metrics can be used to reward care quality and value rather than quantity. Some of these initiatives are driven by, or done in partnership with, payers. MassHealth, Massachusetts’ Medicaid program, for example, has developed a network of Accountable Care Organizations to improve care for patients with SUDs [139]. The growing emphasis on care quality has spurred some hospital systems to develop quality and population health initiatives [140] including housing programs, local workforce development initiatives, food pantries and gardens, and healthcare managers and navigation programs for patients with SUDs. Given the high prevalence of co-occurring substance use and unmet social needs among individuals who frequently use the ED [141,142,143], some initiatives designed to address frequent ED utilization have incorporated SUD treatment along with addressing health-related social needs [144]. Some programs use community health workers or offer intensive case management to provide individualized support and healthcare navigation [144,145,146,147].
Some municipalities have established respite programs where people without housing can stay while receiving treatment for medical problems that do not require hospitalization, but could not be safely addressed at a shelter or while living on the street [148]. Expanding indications to include beginning someone on SUD treatment is one potential strategy that could help improve SUD treatment initiation among patients experiencing homelessness.
Some municipalities and hospitals have invested in alternate sites of care for people who are intoxicated. One example is sobering centers, locations where uninjured and medically stable intoxicated individuals can safely regain short-term sobriety as an alternative to being brought to an ED or jail [149, 150]. Sobering centers have been implemented around the US and vary in their organizational affiliation, triage mechanism, and funding. Currently, there is no standardized scope of work or certification process for sobering centers. While they typically do not deliver onsite treatment for substance use, they can provide peer support and linkage to treatment.
To improve the quality of care within and across health systems, professional societies, public health departments, and state and federal governments have released treatment recommendations, guidelines, standards, and requirements for the treatment of SUDs in the ED. All trauma centers are required to screen, at a minimum, for alcohol use to maintain their trauma center certification [151]. Level I and Level II certified trauma centers must not only screen, but also provide interventions for all individuals who screen positive. The Colorado [152] American College of Emergency Physicians (ACEP) chapter has written treatment guidelines and California ACEP [59] has collaborated on and endorsed guidelines for ED buprenorphine initiation. Nationally, ACEP has not only supported ED naloxone distribution, but also the use of opioid prescribing guidelines and ED buprenorphine initiation. ACEP is also working to improve ED care of OUD at academic and community EDs. Through its Emergency Quality Network (E-QUAL) Opioid Initiative, ACEP provides online education and training resources and quality metric reporting and measurement for participating EDs nationwide [153].
Some states have begun to regulate and/or incentivize OUD treatment standards. After the passage of a substance use discharge planning law in 2016, the Rhode Island Department of Health released hospital treatment standards for the treatment of OUD and opioid overdose. These standards require EDs to provide standardized SUD screening; use peer recovery services; refer patients to treatment; and provide naloxone for overdose rescue, among other requirements [154]. These standards also include additional care recommendations for hospitals that can initiate and maintain patients on MOUD. Similarly, the city of Baltimore also released hospital standards of care [155], all New York City hospitals have agreed to treatment guidance put forward by the NYC Department of Health and Mental Hygiene [156], and last year the Massachusetts legislature passed a law requiring that EDs have protocols and capacity to possess, dispense, administer, and prescribe buprenorphine. To assist EDs with implementation, the Massachusetts Health and Hospital Association and the Massachusetts ACEP chapter released treatment guidelines [157]. Using financial incentives rather than regulation, the Pennsylvania Department of Human Services added an opioid-specific incentive to their Hospital Quality Improvement Program [158]. This program provides financial incentives for hospitals to develop clinical pathways to link Medicaid patients with OUD into treatment within 7 days of an ED visit [158, 159]. Moving beyond incentives, in February 2019, California passed legislation funding EDs to hire and pilot substance use disorder peer navigators and behavioral health peer navigators [160].
Societal Level
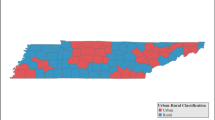
While substance use and SUDs are present among all genders, races, geographic regions, and social strata, they are not evenly distributed or equitably treated. Socioeconomic conditions have a significant impact on the development, progression, and treatment of SUDs. These conditions include, but are not limited to, housing conditions, healthcare access, availability of community resources, poverty, immigration status, employment, exposure to violence, neighborhood stressors, and discrimination [30, 161,162,163]. Many of the neighborhood-based inequalities we observe today are the direct result of historical housing policies known as “red-lining” which not only resulted in the segregation of US metropolitan areas, but also systematically limited Black people’s opportunities for economic advancement [164]. Widening income inequality, weakening social welfare and healthcare safety net programs, and diminishing social cohesion over the last 50 years all contribute to social distress that is associated with higher substance use severity and mortality [30, 31, 165, 166]. Areas with the lowest levels of social capital and socioeconomic status, for example, tend to have more liquor stores [169] and higher overdose rates [167, 168]. Conversely, wealthier counties and communities have fewer liquor retail outlets [170], lower levels of tobacco and alcohol use [171], and lower rates of opioid overdose [168]. Where people live and local demographics also impact what treatment options are available to them. For example, counties that are majority White are more likely to have access to buprenorphine, as compared to predominantly Black counties which are more likely to have access to methadone [32].
To support broader structural change and improvements in population health, emergency physicians can leverage their frontline experience, data, and knowledge to identify and advocate for programs, initiatives, policies, and legislation that address social determinants of SUDs. Societal level changes that will impact the development and treatment of SUDs can be divided into three general categories: (1) individual social factors; (2) public policy; and (3) the drug supply environment [172]. Each of these factors impacts not only substance use and addiction treatment, but also individual and population health and social outcomes.
Individual Social Factors
As previously discussed, structural inequities, SDOH, neighborhood exposures, and one’s living environment have an important impact on substance use and treatment engagement. In addition to addressing individual patient social needs as described earlier, ED providers and health systems can work on a larger community or structural level to improve the social determinants of SUDs. For example, stigma and discrimination toward drug use, people who use drugs, and people with SUDs present barriers to treatment access [173, 174]. To address this barrier, the Grayken Center for Addiction at Boston Medical Center has launched an anti-stigma campaign, which includes training and advocacy for use of non-stigmatizing language when talking about people with SUDs. This also includes employment initiatives that build workforce capacity for people with SUDs, public housing strategies to support people with SUDs, and educational programs and services for people with SUDs to get re-enrolled in school and gain higher education to help them improve their future job opportunities [175].
Housing is another key determinant of substance use that health systems can help address by screening patients for housing needs, referring patients to existing housing resources, and even providing funding or land for housing-related initiatives in conjunction with community and governmental stakeholders. There are two basic housing models to assist people with SUDs: Housing First permanent supportive housing and Recovery Housing (aka Sober Living Houses) [176]. Housing First is a model of permanent supportive housing not limited to people with SUDs. Residents are provided with permanent housing that uses a harm reduction approach to provide individuals with voluntary support and resources for their substance use [121]. These programs have demonstrated good efficacy in housing retention for people with SUDs [121,122,123]. Recovery Housing can range from independent, resident-run homes to staff-managed residences that provide clinical services [177]. Such programs are heterogeneous, and many use a model of peer-support with abstinence-based, Alcoholics Anonymous/Narcotics Anonymous type teachings. Some evaluations of Recovery Housing programs have shown decreased substance use, increased monthly income, and decreased incarceration [177]. While housing is essential for successful recovery, given the variability of Recovery Housing programs, some programs may not be well suited for patients with OUD if they do not accept individuals on MOUD.
Public Policy
Addressing socioeconomic determinants of SUDs requires changes in current public policy including expansion of social programs. Available transportation, education, health, addiction treatment, housing, social and legal advocacy services, and interactions with the criminal justice system, have significant impacts on SUD development and treatment. Medicaid expansion has improved treatment access in expansion states, but has not fully addressed overall treatment gaps or racial and gender disparities in care [32, 33, 70, 125, 127, 132, 178]. Addressing racial and gender disparities in treatment engagement and retention will require identifying and addressing systematic bias in treatment programs and the development of culturally competent, linguistically accessible, and/or specific treatment programs, including for pregnant people with SUDs [178,179,180]. Restrictive immigration policies, detention, deportations, anti-immigrant sentiments, and limited interpreter services are additional barriers faced by immigrants and refugees accessing mental health and substance use services [181].
Emergency physicians can be important advocates for the establishment or removal of laws to reduce drug use-related harm. Historically, the US has used a criminal justice policy strategy to address SUDs [182]. This has had important implications for SUD prevalence, morbidity, mortality, and public health. Rather than decreasing substance use, this approach has largely pushed substance use underground, resulting in increased use-related harm. In the case of witnessed opioid overdose, for example, many report fear of arrest as a primary cause of not calling 911 [183]. The passage of Good Samaritan Legislation offers some protection against prosecution to encourage utilization of emergency medical services in case of an overdose. Other state-specific legislation, specifically naloxone and syringe access laws, offer important opportunities to provide harm reduction services that can prevent opioid overdose as well as injection-related complications such as cellulitis, endocarditis, HIV, and hepatitis C [184,185,186]. The effectiveness of these laws is undermined, however, by the presence of paraphernalia laws, which criminalize possession of equipment for drug consumption, including sterile syringes, even if acquired from a syringe services program or purchased at a pharmacy [187]. Despite their public health utility, many states severely restrict syringe access at pharmacies or community-based syringe services programs, especially in rural communities and the Southeast and Midwest regions [187]. For more information about laws related to opioid prescribing, MOUD, Good Samaritan Legislation, naloxone access, and paraphernalia, see the Prescription Drug Abuse Policy System (PDAPS) at: http://pdaps.org.
Although all people who use illegal drugs face increased policing and scrutiny from the criminal justice system, communities of color and low-income communities are disproportionately impacted [188, 189]. Longer sentences for drug possession, including three-strikes laws and mandatory minimums, have not reduced the prevalence of substance use or rates of overdose [190] but have resulted in the mass incarceration of BIPOC communities [191]. These policy failures are related to the recurrent relapsing nature of SUDs, a high prevalence of trauma and post-traumatic stress disorder among incarcerated people, limited-to-no economic opportunities for those who have been incarcerated, and concurrent defunding of social welfare programs [190, 191, 192].
Furthermore, the use of evidence-based treatment in prison is limited and, where available, racial disparities persist, with decreased provision to Black people who are incarcerated [193]. Following release from prison, 77% of individuals with OUD return to opioid use and the risk of death increases threefold [194]. A minority of prisons and jails offer people with OUD evidence-based treatment with MOUD. Many prisons and jails even force individuals to stop their methadone and/or buprenorphine upon entry. Offering or continuing MOUD in prison can have a significant impact on overdose deaths. Studies from the US and internationally exploring prison buprenorphine programs have observed reductions in post-release opioid overdose death of up to 85% [195,196,197].
Punishing substance use with incarceration has not reduced substance use, nor has it decreased substance-use related morbidity and mortality. Furthermore, criminal justice involvement has a detrimental impact on a person’s ability to obtain housing, employment, and education and a significant negative impact on the health and wellbeing of the families and communities of people who are incarcerated—all of which can undermine successful engagement in SUD treatment after incarceration [198]. Outside of drug legalization, policy changes to mitigate the impact of criminal justice drug policies would include job and education programs for people with criminal justice involvement, defelonization of drug possession, equitable access to SUD treatment, removal of screening for prior convictions on employment applications [199], and decoupling felony convictions from eligibility for housing and occupational licenses [200, 201].
Drug or diversion courts are one strategy used to reduce incarceration for drug-related charges and to improve access to addiction treatment. Some have shown effectiveness in reducing substance use and recidivism, but they vary in form, use, and provision of evidence-based treatment [202,203,204]. One study showed that only 53% of drug courts allowed MOUD to be part of an individual’s treatment plan [194]. Patient advocates have voiced concern about the role of coercion in acceptance of treatment, the efficacy of coerced treatment, and the persistence of racial discrimination in the courts, as treatment has been observed to be preferentially provided to White people facing criminal charges [205]. If implemented effectively, however, these programs could have the potential to reduce incarceration and improve treatment engagement.
A public health policy approach to SUD would entail a fundamental and radical change in drug policy. Drug and drug paraphernalia decriminalization and expansion of evidence-based addiction treatment could not only reduce the health consequences of drug use and incarceration but could also lower barriers to treatment and harm reduction services. In 2001, Portugal decriminalized drug consumption and expanded access to treatment and harm reduction services. Portugal had previously been considered the “heroin capital of Europe,” with an estimated 1% of its population using heroin. Since decriminalization, from 1999 to 2013, overdose deaths have decreased by 80%, treatment engagement increased over 60%, new diagnoses of HIV decreased by 94%, per capita social cost of drug misuse decreased by 18%, and the percentage of people in prison for drug law violations decreased by 45% [206,207,208].
Drug and Alcohol Supply
Many efforts to reduce substance use and substance use-related harm have focused on reducing and restricting the drug and alcohol supply. These efforts have ranged from total prohibition to legalization with government regulation and enforcement. Alcohol was previously prohibited and is now regulated through taxes and other restrictions by age, time, location, and types of beverage. Tobacco is similarly restricted through taxes, and restrictions on age and locations of consumption, which have contributed to reductions in tobacco use and in mortality from smoking-related illnesses [209, 210]. States are increasingly passing legislation to legalize and regulate recreational and medical marijuana consumption, despite federal restrictions [211, 212].
Drug supply strategies to address opioid overdose have focused on reducing opioid prescribing, use of prescription drug monitoring programs, and Drug Enforcement Administration responses to the global drug market. Reducing prescription supply without increasing the availability of SUD treatment and harm reduction services has shifted demand toward illegal drug use. Since the release of the CDC’s opioid prescribing guidelines in 2016, there has been a decline in opioid prescribing [213, 214]. However, despite decreasing prescriptions, overall overdose deaths remain high with many overdoses involving illegal opioid use alone and in combination with prescription opioids [9].
Successfully addressing the opioid epidemic, and substance use disorders more broadly, requires looking beyond biological and medical approaches of prevention, diagnosis, and treatment to strategies that address broader global structural issues that drive the drug trade, such as underdevelopment and poverty. As clinicians, we start at home, one patient at a time. But, by also advocating for hospital, health system, and societal changes in partnership with local communities and policy makers, ED providers can have a meaningful systemic impact to reduce SUD morbidity and mortality.
Recommendations for Emergency Medicine Practice
Basic
-
Identify patients with substance use disorders based on their clinical presentation or use a one-question or brief substance use disorder screening tool (https://www.integration.samhsa.gov/clinical-practice/screening-tools) [41].
-
Provide take-home naloxone for all patients who have presented after an opioid overdose or who are at risk for an overdose.
-
Treat opioid withdrawal in the ED with opioid agonists; methadone if the patient is on methadone, buprenorphine if the patient is not on long-acting opioids and has no contraindications [215].
-
Counsel patients on treatment options and refer patients requesting help to appropriate inpatient or outpatient treatment programs that offer medications for SUDs.
-
Offer rapid HIV testing to individuals who inject drugs.
-
Refer patients who use injection drugs to syringe services programs and provide them with education about sterile injection techniques to reduce soft tissue infections and transmission of HIV and hepatitis C.
Intermediate
-
For patients with moderate to severe OUD who are not in treatment or taking long-acting opioids (e.g., methadone), prescribe buprenorphine and provide referral to outpatient follow-up. While an “X-waiver” is required to write a discharge prescription for buprenorphine, any DEA-licensed ED provider can order a dose of buprenorphine to be administered in the ED (see ACEP’s Buprenorphine Use in the ED Tool [60] https://www.acep.org/patient-care/bupe/ or the ED Bridge Guide [216]: https://ed-bridge.org/guide).
-
Employ ED health navigators (peers or Health Promotion Advocates) to conduct substance use assessments, behavioral counseling, and linkage to treatment.
-
Identify and assess unmet social needs among patients with substance use disorders and refer to community resources as appropriate.
Advanced
-
Establish hospital-based programs or community partnerships to address patients’ unmet social needs as a key part of addressing SUDs.
-
Establish hospital workforce development programs for individuals with SUDs.
-
Advocate for changes in public policy that expand access to addiction treatment and harm reduction rather than punishment.
Teaching Case
Clinical Case
Ms. B is a 30-year-old Latina female with limited English proficiency and a past medical history of chronic low back pain, post-traumatic stress disorder secondary to sexual assault, and bipolar disease. She reports a history of heroin use and more recent use of opioid pills that she buys on the street. She presents to the ED experiencing opioid withdrawal symptoms and requesting Percocet. She receives one dose of 4mg buprenorphine/1mg naloxone by the ED attending and is referred to the ED’s Faster Paths to Treatment’s Bridge Clinic for further evaluation the next day.
At Faster Paths, she reports that one year prior to her visit her oxycodone prescription was abruptly discontinued by her primary care physician, who was concerned about the new state prescribing regulations and monitoring system. She began buying “Percocet 30mg” and tramadol on the street to prevent withdrawal and relieve her low back pain. The Faster Paths bridge clinic physician prescribes buprenorphine 4mg/naloxone 1mg twice daily, and a 4mg Naloxone HCL nasal spray to carry on her person. After a month of monitoring her cravings, negative urine drug testing for opioids except for buprenorphine, and dosage adjustments with frequent visits, she is transferred to the hospital’s Office-Based Addiction Treatment (OBAT) Maintenance Clinic.
During her last visit to Faster Paths, the patient reports extreme anxiety after receiving a letter notifying her to vacate her apartment by the end of the month. She reports that the landlord is selling the building in her gentrifying neighborhood and the new landlord intends to modernize the property and vastly increase rent. Ms. B voices worry about losing her low-rent apartment, which is within walking distance from her part-time job and addiction, medical, and psychiatric care at the same hospital. She reports poor credit, though she could afford first and last month’s rent for a new apartment. She is scared of becoming homeless, which would threaten her stable work, safety for herself, and the security of her medications. She was most concerned about triggering a relapse to heroin, which she has not used in more than 5 years. An emergency physician working in the Faster Paths low barrier bridge clinic wrote a letter to her landlord requesting an extension on her lease. The clinic coordinator consulted BMC THRIVE, an online resource guide developed for direct referrals, and provided Ms. B with information on the BMC medical-legal partnership services and a state program that offers financial assistance for moving costs. The physician’s letter helped Ms. B get a month’s extension. She applied to Boston Public Housing Authority for Section 8 housing without success; however, prior to eviction, because of her resilience, support system, and resources, she found low-cost housing in a suburb outside of Boston. One year later, Ms. B continues to take her prescribed buprenorphine and regularly attend her medical, addiction, and psychiatric appointments.
Teaching Points
-
1.
The relationship between substance use disorder and social needs is bidirectional. Addressing housing instability is a critical component for patient engagement and retention in substance use disorder treatment.
-
2.
Screening for substance use disorder, homelessness, and housing insecurity should be integrated into ED practice, documented in the electronic health record, and linked to a referral and/or consult for an ED social worker or peer advocate, as available.
-
3.
Emergency providers can write letters to landlords and government agencies and refer patients to local eviction prevention or legal services like the medical-legal partnership.
-
4.
ED providers can provide treatment for opioid withdrawal and opioid use disorder using medication for opioid use disorder. Beginning treatment in the ED and providing a warm handoff/referrals are especially important for patients with concurrent social needs, who may not have the resources or ability to access outpatient treatment options without assistance.
-
5.
EDs work within a system of care and cannot provide all needed services themselves. EDs should develop relationships with a referral network of substance use disorder treatment services and housing and other resources to help patients meet their social needs in their community. The SAMHSA practitioner locator guide is helpful to start the process of identifying referral sites for substance use disorder (https://www.samhsa.gov/medication-assisted-treatment/practitioner-program-data/treatment-practitioner-locator).
Discussion Questions
-
1.
The patient presented to the ED in opioid withdrawal. The ED physician effectively treated the patient with 4 mg of SL buprenorphine following ED protocol and state law. How does this compare to your ED’s current practice? What are some benefits, barriers, and enablers for providing buprenorphine in the ED? What mechanisms for outpatient follow-up are available in your local community?
-
2.
What is the impact of homelessness and housing insecurity on the behavioral and physical health of people with substance use disorders? How do substance use disorders contribute to homelessness and housing insecurity? How can ED physicians identify housing insecurity and homelessness? How can providers direct patients to appropriate community resources for unmet health-related social needs? How is this currently done at your institution? What are the ways this could be improved?
-
3.
The ED physician provided a warm handoff to colleagues in the ED low-barrier bridge clinic that provides buprenorphine prescriptions and case management. What are your thoughts on the role of ED physicians to identify and refer patients with substance use disorder? What are the best ways to do this?
-
4.
What institutional or other supports would be needed for the ED to provide comprehensive care for patients with substance use disorders who are unstably housed? What resources are available at your ED/hospital? How can ED physicians advocate for their hospital to engage with and support community agencies already involved with housing issues?
References
Bernstein SL, D'Onofrio G. A promising approach for emergency departments to care for patients with substance use and behavioral disorders. Health Aff (Millwood). 2013;32(12):2122–8.
White AM, Slater ME, Ng G, Hingson R, Breslow R. Trends in alcohol-related emergency department visits in the United States: results from the nationwide emergency department sample, 2006 to 2014. Alcohol Clin Exp Res. 2018;42(2):352–9.
Weiss A, Bailey M, O'Malley L, Barrett M, Elixhauser A, Steiner C. Patient characteristics of opioid-related inpatient stays and emergency department visits nationally and by state, 2014. Agency for Healthcare Research and Quality: Rockville; 2017.
Vivolo-Kantor AM, Seth P, Gladden RM, Mattson CL, Baldwin GT, Kite-Powell A, et al. Vital signs: trends in emergency department visits for suspected opioid overdoses – United States, July 2016–September 2017. MMWR Morb Mortal Wkly Rep. 2018;67(9):279–85.
Han BH, Moore AA, Sherman S, Keyes KM, Palamar JJ. Demographic trends of binge alcohol use and alcohol use disorders among older adults in the United States, 2005–2014. Drug Alcohol Depend. 2017;170:198–207.
Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE, et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: a meta-analysis of 6 national survey series. Alcohol Clin Exp Res. 2018;42(10):1939–50.
Centers for Disease Control and Prevention. Average for United States 2006–2010 alcohol-attributable deaths due to excessive alcohol use 2013. Available from: www.cdc.gov/ARDI.
Centers for Disease Control and Prevention. Multiple cause of death 1999–2017 on CDC WONDER online database: National Center for Health Statistics.; December 2018. Available from: https://wonder.cdc.gov/mcd.html.
NIDA. Overdose Death Rates 2019 [updated January 2019]. Available from: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates.
Spencer MR, Warner M, Bastian BA, Trinidad JP, Hedegaard H. Drug overdose deaths involving fentanyl, 2011–2016. Hyattsville: National Center for Health Statistics; 2019. Contract No.: 3.
Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths – United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–52.
Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths – United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419–27.
NIDA. Nationwide trends June 25, 2015. Available from: https://www.drugabuse.gov/publications/drugfacts/nationwide-trends.
Mack KA, Jones CM, Ballesteros MF. Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas – United States. MMWR Surveill Summ. 2017;66(19):1–12.
National Survey on Drug Use and Health 2018 [Internet]. 2020. Available from: https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health.
Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Rockville; 2019.
Andrilla CHA, Moore TE, Patterson DG, Larson EH. Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: a 5-year update. J Rural Health. 2019;35(1):108–12.
Haffajee RL, Lin LA, Bohnert ASB, Goldstick JE. Characteristics of us counties with high opioid overdose mortality and low capacity to deliver medications for opioid use disorder. JAMA Netw Open. 2019;2(6):e196373.
Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. 2019;76(9):979–81.
Kulesza M, Matsuda M, Ramirez JJ, Werntz AJ, Teachman BA, Lindgren KP. Towards greater understanding of addiction stigma: intersectionality with race/ethnicity and gender. Drug Alcohol Depend. 2016;169:85–91.
American Psychiatric Association. Substance-related and addictive disorders. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, D.C.: American Psychiatric Association; 2013.
Shin SH, McDonald SE, Conley D. Patterns of adverse childhood experiences and substance use among young adults: a latent class analysis. Addict Behav. 2018;78:187–92.
Svingen L, Dykstra RE, Simpson JL, Jaffe AE, Bevins RA, Carlo G, et al. Associations between family history of substance use, childhood trauma, and age of first drug use in persons with methamphetamine dependence. J Addict Med. 2016;10(4):269–73.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–e66.
Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111(3):564–72.
Doran KM, Rahai N, McCormack RP, Milian J, Shelley D, Rotrosen J, et al. Substance use and homelessness among emergency department patients. Drug Alcohol Depend. 2018;188:328–33.
Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154–63.
Rigg KK, Monnat SM. Urban vs. rural differences in prescription opioid misuse among adults in the United States: informing region specific drug policies and interventions. Int J Drug Policy. 2015;26(5):484–91.
Case A, Deaton A. Mortality and morbidity in the 21st century: Washington, DC. Brookings Institute; 2017.
Ulirsch JC, Weaver MA, Bortsov AV, Soward AC, Swor RA, Peak DA, et al. No man is an island: Living in a disadvantaged neighborhood influences chronic pain development after motor vehicle collision. Pain. 2014;155(10):2116–23.
Knapp EA, Bilal U, Dean LT, Lazo M, Celentano DD. Economic insecurity and deaths of despair in US Counties. Am J Epidemiol. 2019;188(12):2131–9.
Goedel WC, Shapiro A, Cerda M, Tsai JW, Hadland SE, Marshall BDL. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3(4):e203711.
Saloner B, Cook BL. Blacks and hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health Affairs. 2013;32(1):135–45.
Frieden TR. Shattuck lecture: the future of public health. N Engl J Med. 2015;373(18):1748–54.
Finkelhor D, Turner HA, Shattuck A, Hamby SL. Violence, crime, and abuse exposure in a national sample of children and youth: an update. JAMA Pediatr. 2013;167(7):614–21.
Finkelhor D, Turner HA, Shattuck A, Hamby SL. Prevalence of childhood exposure to violence, crime, and abuse: results from the national survey of children's exposure to violence. JAMA Pediatr. 2015;169(8):746–54.
Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow M, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 data brief – updated release. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention: Atlanta; 2018.
Center for Substance Abuse Treatment. Trauma-informed care in behavioral health services. Rockville: Substance Abuse and Mental Health Services Administration; 2014.
Substance Abuse and Mental Health Services Administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS Publication No. (SMA) 14-4884. Substance Abuse and Mental Health Services Administration: Rockville; 2014.
Corbin TJ, Purtle J, Rich LJ, Rich JA, Adams EJ, Yee G, et al. The prevalence of trauma and childhood adversity in an urban, hospital-based violence intervention program. J Health Care Poor Underserved. 2013;24(3):1021–30.
Hawk K, D'Onofrio G. Emergency department screening and interventions for substance use disorders. Addict Sci Clin Pract. 2018;13(1):18.
Bernstein E, Topp D, Shaw E. A preliminary report of knowledge translation: lessons from taking screening and brief intervention techniques from the research setting into regional systems of care. Acad Emerg Med. 2009;16:1225.
SBIRT: Screening, Brief Intervention, and Referral to Treatment Washington, D.C.: SAMHSA-HRSA Center for Integrated Health Solutions. Available from: https://www.integration.samhsa.gov/clinical-practice/sbirt.
Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99(1-3):280–95.
Barata IA, Shandro JR, Montgomery M, Polansky R, Sachs CJ, Duber HC, et al. Effectiveness of SBIRT for alcohol use disorders in the emergency department: a systematic review. West J Emerg Med. 2017;18(6):1143–52.
Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary care validation of a single-question alcohol screening test. J Gen Intern Med. 2009;24(7):783–8.
Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170(13):1155–60.
AUDIT-C Overview. Available from: https://www.integration.samhsa.gov/images/res/tool_auditc.pdf.
O'Brien CP. The CAGE questionnaire for detection of alcoholism: a remarkably useful but simple tool. JAMA. 2008;300(17):2054–6.
NIAAA. Helping patients who drink too much: a clinician’s guide. National Institute on Alcohol Abuse and Alcoholism; Washington, DC. 2005.
Bernstein E, Topp D, Shaw E, Girard C, Pressman K, Woolcock E, et al. A preliminary report of knowledge translation: lessons from taking screening and brief intervention techniques from the research setting into regional systems of care. Acad Emerg Med. 2009;16(11):1225–33.
Smith PC, Cheng DM, Allensworth-Davies D, Winter MR, Saitz R. Use of a single alcohol screening question to identify other drug use. Drug Alcohol Depend. 2014;139:178–80. https://doi.org/10.1016/j.drugalcdep.2014.03.027. Epub 2014 Apr 5. PMID: 24768061; PMCID: PMC4085274.
Committee on Substance A, Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128(5):e1330–40.
Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adoles Med. 2002;156(6):607.
The Center for Adolescent Substance Use Research. The CRAFFT 2.1 manual. Boston: The Center for Adolescent Substance Use Research; 2018.
Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: The Guilford Press; 2013.
Counselman FL, Babu K, Edens MA, Gorgas DL, Hobgood C, Marco CA, et al. The 2016 model of the clinical practice of emergency medicine. J Emerg Med. 2017;52(6):846–9.
Lemhoefer C, Rabe GL, Wellmann J, Bernstein SL, Cheung KW, McCarthy WJ, et al. Emergency department-initiated tobacco control: update of a systematic review and meta-analysis of randomized controlled trials. Prev Chronic Dis. 2017;14:E89.
CA BRIDGE. Resources. https://cabridge.org/tools/resources/. Accessed 26 Feb 2021.
Ketcham E, Ryan R. BUPE: buprenorphine use in the Emergency Department Tool Dallas, TX: American College of Emergency Physicians; 2018. Available from: https://www.acep.org/patient-care/bupe/.
D'Onofrio G, O'Connor PG, Pantalon MV, Chawarski MC, Busch SH, Owens PH, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. Jama. 2015;313(16):1636–44.
Mark T, Montejano L, Kranzler H, Chalk M, Gastfriend D. Comparison of healthcare utilization among patients treated with alcoholism medications. Am J Manag Care. 2010;16(12):879–88.
Bernstein SL, D'Onofrio G, Rosner J, O'Malley S, Makuch R, Busch S, et al. Successful tobacco dependence treatment in low-income emergency department patients: a randomized trial. Ann Emerg Med. 2015;66(2):140–7.
Bernstein SL, Boudreaux ED, Cydulka RK, Rhodes KV, Lettman NA, Almeida SL, et al. Tobacco control interventions in the emergency department: a joint statement of emergency medicine organizations. J Emerg Nurs. 2006;32(5):370–81.
Katz DA, Vander Weg MW, Holman J, Nugent A, Baker L, Johnson S, et al. The Emergency Department Action in Smoking Cessation (EDASC) trial: impact on delivery of smoking cessation counseling. Acad Emerg Med. 2012;19(4):409–20.
Duber HC, Barata IA, Cioe-Pena E, Liang SY, Ketcham E, Macias-Konstantopoulos W, et al. Identification, management, and transition of care for patients with opioid use disorder in the emergency department. Ann Emerg Med. 2018;18:S0196–644.
Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550.
Wakeman SE, Larochelle MR, Ameli O, Chaisson CE, McPheeters JT, Crown WH, et al. Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open. 2020;3(2):e1920622.
Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Rockville; 2019.
Larochelle MR, Bernson D, Land T, Stopka TJ, Wang N, Xuan Z, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a Cohort Study. Ann Intern Med. 2018;169(3):137–45.
Busch SH, Fiellin DA, Chawarski MC, Owens PH, Pantalon MV, Hawk K, et al. Cost-effectiveness of emergency department-initiated treatment for opioid dependence. Addiction. 2017;112(11):2002–10.
Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358–67.
Administering or dispensing of narcotic drugs., 21 CFR § 1306.07(b) (1998).
Davis CS, Carr DH. The law and policy of opioids for pain management, addiction treatment, and overdose reversal. Indiana Health Law Rev. 2017;14(1):1.
D'Onofrio G, McCormack RP, Hawk K. Emergency departments – A 24/7/365 option for combating the opioid crisis. N Engl J Med. 2018;379(26):2487–90.
Substance Abuse and Mental Health Services Administration. Use of medications for opioid use disorder in emergency departments. Rockville: National Mental Health and Substance Use Policy Laboratory; Bethesda, MD, 2019.
CA BRIDGE. Buprenorphine (Bup) Hospital Quick Start. Updated Sept 2020. https://cabridge.org/resource/buprenorphine-bup-hospital-quick-start/. Accessed 26 Feb 2021.
Joudrey PJ, Edelman EJ, Wang EA. Drive times to opioid treatment programs in urban and rural counties in 5 US states. JAMA. 2019;322(13):1310–2.
Grimm C. Geographic disparities affect access to buprenorphine services for opioid use disorder. Washington, D.C.: U.S. Department of Health and Human Services. Office of Inspector General; 2020. Contract No.: OEI-12-17-00240.
Eibl JK, Gauthier G, Pellegrini D, Daiter J, Varenbut M, Hogenbirk JC, et al. The effectiveness of telemedicine-delivered opioid agonist therapy in a supervised clinical setting. Drug Alcohol Depend. 2017;176:133–8.
Huskamp HA, Busch AB, Souza J, Uscher-Pines L, Rose S, Wilcock A, et al. How is telemedicine being used in opioid and other substance use disorder treatment? Health Aff (Millwood). 2018;37(12):1940–7.
Uscher-Pines L, Huskamp HA, Mehrotra A. Treating patients with opioid use disorder in their homes: an emerging treatment model. JAMA. 2020;324:39.
Yang YT, Weintraub E, Haffajee RL. Telemedicine's role in addressing the opioid epidemic. Mayo Clin Proc. 2018;93(9):1177–80.
Zheng W, Nickasch M, Lander L, Wen S, Xiao M, Marshalek P, et al. Treatment outcome comparison between telepsychiatry and face-to-face buprenorphine medication-assisted treatment for opioid use disorder: a 2-year retrospective data analysis. J Addict Med. 2017;11(2):138–44.
Samuels EA, Clark SA, Wunsch C, Keeler LAJ, Reddy N, Vanjani R, et al. Innovation during COVID-19: improving addiction treatment access. J Addict Med. 2020;14:e8.
Palmateer N, Kimber J, Hickman M, Hutchinson S, Rhodes T, Goldberg D. Evidence for the effectiveness of sterile injecting equipment provision in preventing hepatitis C and human immunodeficiency virus transmission among injecting drug users: a review of reviews. Addiction. 2010;105(5):844–59.
MacArthur GJ, van Velzen E, Palmateer N, Kimber J, Pharris A, Hope V, et al. Interventions to prevent HIV and Hepatitis C in people who inject drugs: a review of reviews to assess evidence of effectiveness. Int J Drug Policy. 2014;25(1):34–52.
Aspinall EJ, Nambiar D, Goldberg DJ, Hickman M, Weir A, Van Velzen E, et al. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(1):235–48.
Platt L, Minozzi S, Reed J, Vickerman P, Hagan H, French C, et al. Needle and syringe programmes and opioid substitution therapy for preventing HCV transmission among people who inject drugs: findings from a Cochrane Review and meta-analysis. Addiction. 2018;113(3):545–63.
Des Jarlais D, Perlis T, Arasteh K, Torian L, Hagan H, Beatrice S, et al. Reductions in hepatitis C virus and HIV infections among injecting drug users in New York City, 1990–2001. AIDS. 2005;19(Suppl 3):S20–5.
Nguyen TQ, Weir BW, Des Jarlais DC, Pinkerton SD, Holtgrave DR. Syringe exchange in the United States: a national level economic evaluation of hypothetical increases in investment. AIDS Behav. 2014;18(11):2144–55.
Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174.
Piper TM, Stancliff S, Rudenstine S, Sherman S, Nandi V, Clear A, et al. Evaluation of a naloxone distribution and administration program in New York City. Subst Use Misuse. 2008;43(7):858–70.
Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health. 2009;99(5):788–91.
Maxwell S, Bigg D, Stanczykiewicz K, Carlberg-Racich S. Prescribing naloxone to actively injecting heroin users: a program to reduce heroin overdose deaths. J Addict Dis. 2006;25(3):89–96.
Samuels E. Emergency department naloxone distribution: a Rhode Island department of health, recovery community, and emergency department partnership to reduce opioid overdose deaths. R I Med J. 2014;97(10):38–9.
Samuels EA, Baird J, Yang ES, Mello MJ. Adoption and utilization of an emergency department naloxone distribution and peer recovery coach consultation program. Acad Emerg Med. 2019;26(2):160–73.
Samuels EA, Hoppe J, Papp J, Whiteside L, Raja AS, Bernstein E. Naloxone distribution strategies needed in emergency departments. ACEPNow. American College of Emergency Physicians. March 16, 2016. https://www.acepnow.com/article/naloxone-distribution-strategies-needed-in-emergency-departments/.
Dwyer K, Walley AY, Langlois BK, Mitchell PM, Nelson KP, Cromwell J, et al. Opioid education and nasal naloxone rescue kits in the emergency department. West J Emerg Med. 2015;16(3):381–4.
Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600.
Bukten A, Stavseth MR, Skurtveit S, Tverdal A, Strang J, Clausen T. High risk of overdose death following release from prison: variations in mortality during a 15-year observation period. Addiction. 2017;112(8):1432–9.
Garg RK, Fulton-Kehoe D, Franklin GM. Patterns of opioid use and risk of opioid overdose death among medicaid patients. Med Care. 2017;55(7):661–8.
Nadpara PA, Joyce AR, Murrelle EL, Carroll NW, Carroll NV, Barnard M, et al. Risk factors for serious prescription opioid-induced respiratory depression or overdose: comparison of commercially insured and veterans health affairs populations. Pain Med. 2018;19(1):79–96.
Naloxone Overdose Prevention Laws: prescription drug abuse policy system; 2017. Available from: http://pdaps.org/datasets/laws-regulating-administration-of-naloxone-1501695139.
Ryan S, Pantalon MV, Camenga D, Martel S, D'Onofrio G. Evaluation of a pediatric resident skills-based screening, brief intervention and referral to treatment (SBIRT) curriculum for substance use. J Adolesc Health. 2018;63(3):327–34.
Duong DK, O'Sullivan PS, Satre DD, Soskin P, Satterfield J. Social workers as workplace-based instructors of alcohol and drug screening, brief intervention, and referral to treatment (SBIRT) for emergency medicine residents. Teach Learn Med. 2016;28(3):303–13.
Tetrault JM, Green ML, Martino S, Thung SF, Degutis LC, Ryan SA, et al. Developing and implementing a multispecialty graduate medical education curriculum on Screening, Brief Intervention, and Referral to Treatment (SBIRT). Subst Abus. 2012;33(2):168–81.
Improving the hospital and emergency department response to substance use disorders: a Project ASSERT Case Study: American Hospital Association; [cited 2019]. Available from: https://www.aha.org/system/files/content/17/project-assert-case-study.pdf.
Project ASSERT: Boston Medical Center. Available from: https://www.bmc.org/programs/project-assert.
The BNI ART Institute. Project ASSERT: SBIRT in Emergency Care: The Boston University School of Public Health. Available from: https://www.bu.edu/bniart/sbirt-experience/sbirt-programs/sbirt-project-assert/.
Faster Paths to Treatment: Boston Medical Center. Available from: https://www.bmc.org/programs/faster-paths-to-treatment.
Welch AE, Jeffers A, Allen B, Paone D, Kunins HV. Relay: a peer-delivered emergency department-based response to nonfatal opioid overdose. Am J Public Health. 2019;109(10):1392–5.
Addiction Policy Forum. Anchor ED. Washington, D.C. February 2017. www.addictionpolicy.org/post/anchored-rhode-island.
Waye KM, Goyer J, Dettor D, Mahoney L, Samuels EA, Yedinak JL, et al. Implementing peer recovery services for overdose prevention in Rhode Island: an examination of two outreach-based approaches. Addict Behav. Washington, D.C. 2019;89:85–91.
McGuire AB, Powell KG, Treitler PC, Wagner KD, Smith KP, Cooperman N, et al. Emergency department-based peer support for opioid use disorder: emergent functions and forms. J Subst Abuse Treat. 2020;108:82–7.
NYC Department of Health and Mental Hygiene. Information for Peers. Available from: https://www1.nyc.gov/site/doh/health/health-topics/alcohol-and-drug-use-information-for-peers.page.
Samuels EA, Bernstein SL, Marshall BDL, Krieger M, Baird J, Mello MJ. Peer navigation and take-home naloxone for opioid overdose emergency department patients: preliminary patient outcomes. J Subst Abuse Treat. 2018;94:29–34.
Summary of 2019 council resolutions: resolution 50 social work in the Emergency Department American College of Emergency Physicians; 2019. Available from: https://washingtonacep.org/wp-content/uploads/2019-Resolutions-Adopted-by-the-Council-Board.pdf.
Boston Medical Center. The preventive food pantry Boston, MA. Available from: https://www.bmc.org/nourishing-our-community/preventive-food-pantry.
Bridle-Fitzpatrick S. Hospital – food bank partnerships: a recipe for community health: hunger and health; April 25, 2018. Available from: https://hungerandhealth.feedingamerica.org/2018/04/hospital-food-bank-partnerships-recipe-community-health/.
Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651–6.
Urbanoski K, Veldhuizen S, Krausz M, Schutz C, Somers JM, Kirst M, et al. Effects of comorbid substance use disorders on outcomes in a Housing First intervention for homeless people with mental illness. Addiction. 2018;113(1):137–45.
Palepu A, Patterson ML, Moniruzzaman A, Frankish CJ, Somers J. Housing first improves residential stability in homeless adults with concurrent substance dependence and mental disorders. Am J Public Health. 2013;103(Suppl 2):e30–6.
Vuolo L, Oster R, Weber E. Evaluating the promise and potential of the parity act on its tenth anniversary, Health Affairs Blog October 10, 2018. Available from: https://www.healthaffairs.org/do/10.1377/hblog20181009.356245/full/.
Meinhofer A, Witman AE. The role of health insurance on treatment for opioid use disorders: evidence from the Affordable Care Act Medicaid expansion. J Health Econ. 2018;60:177–97.
Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. 2019;76:979.
Nowotny KM. Race/ethnic disparities in the utilization of treatment for drug dependent inmates in U.S. state correctional facilities. Addict Behav. 2015;40:148–53.
Guerrero EG, Marsh JC, Duan L, Oh C, Perron B, Lee B. Disparities in completion of substance abuse treatment between and within racial and ethnic groups. Health Serv Res. 2013;48(4):1450–67.
Gilbert PA, Pro G, Zemore SE, Mulia N, Brown G. Gender differences in use of alcohol treatment services and reasons for nonuse in a national sample. Alcohol Clin Exp Res. 2019;43(4):722–31.
Cerda M, Gaidus A, Keyes KM, Ponicki W, Martins S, Galea S, et al. Prescription opioid poisoning across urban and rural areas: identifying vulnerable groups and geographic areas. Addiction. 2017;112(1):103–12.
Amiri S, Lutz R, Socias ME, McDonell MG, Roll JM, Amram O. Increased distance was associated with lower daily attendance to an opioid treatment program in Spokane County Washington. J Subst Abuse Treat. 2018;93:26–30.
Guerrero EG, Garner BR, Cook B, Kong Y, Vega WA, Gelberg L. Identifying and reducing disparities in successful addiction treatment completion: testing the role of Medicaid payment acceptance. Subst Abuse Treat Prev Policy. 2017;12(1):27.
Komaromy M, Duhigg D, Metcalf A, Carlson C, Kalishman S, Hayes L, et al. Project ECHO (Extension for Community Healthcare Outcomes): a new model for educating primary care providers about treatment of substance use disorders. Subst Abus. 2016;37(1):20–4.
Tofighi B, Abrantes A, Stein MD. The role of technology-based interventions for substance use disorders in primary care: a review of the literature. Med Clin North Am. 2018;102(4):715–31.
Lord S, Moore SK, Ramsey A, Dinauer S, Johnson K. Implementation of a substance use recovery support mobile phone app in community settings: qualitative study of clinician and staff perspectives of facilitators and barriers. JMIR Ment Health. 2016;3(2):e24.
Anderson M, Kumar M. Digital divide persists even as lower-income Americans make gains in tech adoption: Pew Research Center; 2019. Available from: https://www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/.
Federal Communications Commission. 2019 Broadband Deployment Report. Federal Communications Commission. https://www.fcc.gov/reports-research/reports/broadbandprogress-reports/2019-broadband-deployment-report. Published May 29, 2019. Accessed August, 2020.
Perrin A. Digital gap between rural and nonrural America persists: Pew Research Center; [updated May 31, 2019]. Available from: https://www.pewresearch.org/fact-tank/2019/05/31/digital-gap-between-rural-and-nonrural-america-persists/.
MassHealth Launches Restructuring To Improve Health Outcomes for 1.2 Million Members [press release]. Boston: Executive Office of Health and Human Services; 2018.
Centers for Medicare and Medicaid Services Innovation Center. Accountable Health Communities Model [updated Nov 13, 2019]. Available from: https://innovation.cms.gov/initiatives/ahcm.
Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48(1):1–8.
LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data, and the policy implications. Ann Emerg Med. 2010;56(1):42–8.
Curran G, Sullivan G, Williams K, Han X, Allee E, Kotrla K. The association of psychiatric comorbidity and use of the emergency department among persons with substance use disorders: an observational cohort study. BMC Emerg Med J. 2008;8:17.
Moe J, Kirkland SW, Rawe E, Ospina MB, Vandermeer B, Campbell S, et al. Effectiveness of interventions to decrease emergency department visits by adult frequent users: a systematic review. Acad Emerg Med. 2017;24(1):40–52.
Kwan BM, Rockwood A, Bandle B, Fernald D, Hamer MK, Capp R. Community health workers: addressing client objectives among frequent emergency department users. J Public Health Manag Pract. 2018;24(2):146–54.
Bodenmann P, Velonaki VS, Ruggeri O, Hugli O, Burnand B, Wasserfallen JB, et al. Case management for frequent users of the emergency department: study protocol of a randomised controlled trial. BMC Health Serv Res. 2014;14:264.
Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771–8.
Doran KM, Ragins KT, Gross CP, Zerger S. Medical respite programs for homeless patients: a systematic review. J Health Care Poor Underserved. 2013;24(2):499–524.
Warren O, Smith-Bernardin S, Jamieson K, Zaller N, Liferidge A. Identification and practice patterns of sobering centers in the United States. J Health Care Poor Underserved. 2016;27(4):1843–57.
Jarvis SV, Kincaid L, Weltge AF, Lee M, Basinger SF. Public intoxication: sobering centers as an alternative to incarceration, Houston, 2010–2017. Am J Public Health. 2019;109(4):597–9.
American College of Surgeons Committee on Trauma. Resources for the optimal care of the injured patient. Chicago: American College of Surgeons; 2014.
Colorado ACEP. Opioid prescribing & treatment guidelines. Colorado ACEP: Northglenn; 2017.
American College of Emergency Physicians. E-QUAL Network Opioid Initiative 2019. Available from: https://www.acep.org/administration/quality/equal/emergency-quality-network-e-qual/e-qual-opioid-initiative/.
Rhode Island Department of Behavioral Healthcare Developmental Disabilities, and Hospitals, Rhode Island Department of Health. Levels of Care for Rhode Island Emergency Departments and Hospitals for Treating Overdose and Opioid Use Disorder. 2017 March.
Baltimore City Health Department. Levels of care for Baltimore City Hospitals responding to the opioid epidemic guide for Hospitals Baltimore, MD August 2018. Available from: https://health.baltimorecity.gov/sites/default/files/Levels%20of%20Care%20-%20Guide.pdf.
NYC Department of Health and Mental Hygiene. Guidance for the care of patients presenting to New York City Emergency Departments following a non-fatal opioid overdose New York City: NYC Department of Health and Mental Hygiene; May 31, 2019. Available from: https://www1.nyc.gov/assets/doh/downloads/pdf/basas/non-fatal-overdose-providers.pdf.
Massachusetts Health and Hospital Association. Guidelines for medication for addiction treatment for opioid use disorder within the emergency department: Massachusetts Health and Hospital Association; January 2019. Available from: https://www.mhalink.org/MHADocs/MondayReport/2019/18-01-04MATguidelinesNEWFINAL.pdf.
Kilaru AS, Perrone J, Kelley D, Siegel S, Lubitz SF, Mitra N, et al. Participation in a hospital incentive program for follow-up treatment for opioid use disorder. JAMA Netw Open. 2020;3(1):e1918511.
Pennsylvania Department of Human Services. Follow-up treatment after ED visit for opioid use disorder June 6, 2018. Available from: https://www.pamedsoc.org/docs/librariesprovider2/pamed-documents/new-opioid-measures-hqip.pdf?sfvrsn=8524485b_2.
Santiago. Health and Safety Code Section 11757: substance use disorder treatment: peer navigators: California State Legislature; Feb 5 2019. Available from: https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201920200AB389.
Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J Health Soc Behav. 2001;42(2)
Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52.
Galea S, Rudenstine S, Vlahov D. Drug use, misuse, and the urban environment. Drug Alcohol Rev. 2005;24(2):127–36.
Rothstein R. The Color of Law: a forgotten history of how our government segregated America. Liveright: New York; 2017.
US Census Bureau. 2018 American Community Survey February 13, 2020. Available from: https://www.census.gov/programs-surveys/acs/news/data-releases/2018/release.html#par_textimage_copy.
Schaeffer K. 6 facts about economic inequality in the U.S. Washington, D.C.: Pew Research Center; February 7, 2020. Available from: https://www.pewresearch.org/fact-tank/2020/02/07/6-facts-about-economic-inequality-in-the-u-s/.
Zoorob MJ, Salemi JL. Bowling alone, dying together: the role of social capital in mitigating the drug overdose epidemic in the United States. Drug Alcohol Depend. 2017;173:1–9.
Pear VA, Ponicki WR, Gaidus A, Keyes KM, Martins SS, Fink DS, et al. Urban-rural variation in the socioeconomic determinants of opioid overdose. Drug Alcohol Depend. 2019;195:66–73.
LaVeist TA, Wallace JM. Health risk and inequitable distribution of liquor stores in African American neighborhood. Soc Sci Med. 2000;51(4):613–7.
Bluthenthal RN, Cohen DA, Farley TA, Scribner R, Beighley C, Schonlau M, et al. Alcohol availability and neighborhood characteristics in Los Angeles, California and southern Louisiana. J Urban Health. 2008;85(2):191–205.
Hamad R, Brown DM, Basu S. The association of county-level socioeconomic factors with individual tobacco and alcohol use: a longitudinal study of U.S. adults. BMC Public Health. 2019;19(1):390.
Saloner B, McGinty EE, Beletsky L, Bluthenthal R, Beyrer C, Botticelli M, et al. a public health strategy for the opioid crisis. Public Health Rep. 2018;133(1_suppl):24S–34S.
Ashford RD, Brown AM, Ryding R, Curtis B. Building recovery ready communities: the recovery ready ecosystem model and community framework. Addict Res Theory. 2019;28:1–11.
Cloud W, Granfield R. Conceptualizing recovery capital: expansion of a theoretical construct. Subst Use Misuse. 2008;43(12-13):1971–86.
Matthew DB. Un-burying the lead: public health tools are the key to beating the opioid epidemic. USC-Brookings Schaeffer Initiative for Health Policy; 2018.
Wittman FD, Polcin DL, Sheridan D. The architecture of recovery: two kinds of housing assistance for chronic homeless persons with substance use disorders. Drugs Alcohol Today. 2017;17(3):157–67.
Jason LA, Olson BD, Ferrari JR, Lo Sasso AT. Communal housing settings enhance substance abuse recovery. Am J Public Health. 2006;96(10):1727–9.
Schiff DM, Nielsen T, Hoeppner BB, Terplan M, Hansen H, Bernson D, et al. Assessment of racial and ethnic disparities in the use of medication to treat opioid use disorder among pregnant women in Massachusetts. JAMA Netw Open. 2020;3(5):e205734.
Guerrero EG, Marsh JC, Khachikian T, Amaro H, Vega WA. Disparities in Latino substance use, service use, and treatment: implications for culturally and evidence-based interventions under health care reform. Drug Alcohol Depend. 2013;133(3):805–13.
Valdez LA, Flores M, Ruiz J, Oren E, Carvajal S, Garcia DO. Gender and cultural adaptations for diversity: a systematic review of alcohol and substance abuse interventions for latino males. Subst Use Misuse. 2018;53(10):1608–23.
Perreira KM, Pedroza JM. Policies of exclusion: implications for the health of immigrants and their children. Annu Rev Public Health. 2019;40:147–66.
Alexander M. The New Jim Crow: mass incarceration in the age of colorblindness. New York: Jackson, Tenn New Press; 2010.
Koester S, Mueller SR, Raville L, Langegger S, Binswanger IA. Why are some people who have received overdose education and naloxone reticent to call Emergency Medical Services in the event of overdose? Int J Drug Policy. 2017;48:115–24.
Gonsalves GS, Crawford FW. Dynamics of the HIV outbreak and response in Scott County, IN, USA, 2011–15: a modelling study. The Lancet HIV. 2018;5(10):e569–e77.
Flath N, Tobin K, King K, Lee A, Latkin C. enduring consequences from the war on drugs: how policing practices impact HIV risk among people who inject drugs in Baltimore city. Subst Use Misuse. 2017;52(8):1003–10.
Goedel WC, King MRF, Lurie MN, Galea S, Townsend JP, Galvani AP, et al. Implementation of syringe services programs to prevent rapid human immunodeficiency virus transmission in rural counties in the United States: a modeling study. Clin Infect Dis. 2019;
Davis CS, Carr DH, Samuels EA. Paraphernalia laws, criminalizing possession and distribution of items used to consume illicit drugs, and injection-related harm. Am J Public Health. 2019;109(11):1564–7.
Fazel S, Yoon IA, Hayes AJ. Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction. 2017;112(10):1725–39.
The Drug Policy Alliance. The drug war, mass incarceration and race. The Drug Policy Alliance: New York; 2018.
Pew Charitable Trusts. More imprisonment does not reduce state drug problems: data show no relationship between prison terms and drug misuse. Washington, D.C.: Pew Charitable Trusts; 2018.
Wolff N, Huening J, Shi J, Frueh BC. Trauma exposure and posttraumatic stress disorder among incarcerated men. J Urban Health. 2014;91(4):707–19.
Hinton E. From the war on poverty to the war on crime: the making of mass incarceration in America. Cambridge, MA: Harvard University Press; 2016.
Rosenberg A, Groves AK, Blankenship KM. Comparing black and white drug offenders: implications for racial disparities in criminal justice and reentry policy and programming. J Drug Issues. 2017;47(1):132–42.
Substance Abuse and Mental Health Services Administration. Medication-Assisted Treatment (MAT) in the criminal justice system: brief guidance to the states: Substance Abuse and Mental Health Services Administration; March 2019. Available from: https://store.samhsa.gov/system/files/pep19-matbriefcjs.pdf.
Green TC, Clarke J, Brinkley-Rubinstein L, Marshall BDL, Alexander-Scott N, Boss R, et al. Postincarceration Fatal Overdoses After Implementing Medications for Addiction Treatment in a Statewide Correctional System. JAMA Psychiatry. 2018;75(4):405–7.
Marsden J, Stillwell G, Jones H, Cooper A, Eastwood B, Farrell M, et al. Does Exposure to Opioid Substitution Treatment in Prison Reduce the Risk of Death After Release? A National Prospective Observational Study in England. Addiction. 2017;112(8):1408–18.
Degenhardt L, Larney S, Kimber J, Gisev N, Farrell M, Dobbins T, et al. The impact of opioid substitution therapy on mortality post-release from prison: retrospective data linkage study. Addiction. 2014;109(8):1306–17.
Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. The Lancet. 2017;389(10077):1464–74.
Ban the Box Campaign. Available from: https://bantheboxcampaign.org.
Matthew DB. Un-burying the lead: public health tools are the key to beating the opioid epidemic. USC-Brookings Schaeffer Initiative for Health Policy; 2018.
Ordinance 125393: fair chance housing ordinance August 23, 2017. Available from: http://seattle.legistar.com/View.ashx?M=F&ID=5387389&GUID=6AA5DDAE-8BAE-4444-8C17-62C2B3533CA3.
Peters RH, Young MS, Rojas EC, Gorey CM. Evidence-based treatment and supervision practices for co-occurring mental and substance use disorders in the criminal justice system. Am J Drug Alcohol Abuse. 2017;43(4):475–88.
Tsai J, Flatley B, Kasprow WJ, Clark S, Finlay A. Diversion of veterans with criminal justice involvement to treatment courts: participant characteristics and outcomes. Psychiatr Serv. 2017;68(4):375–83.
The Center for Health and Justice at TASC. No entry: a national survey of criminal justice diversion programs and initiatives. Chicago: The Center for Health and Justice at TASC; 2013.
Nicosia N, Macdonald JM, Arkes J. Disparities in criminal court referrals to drug treatment and prison for minority men. Am J Public Health. 2013;103(6):e77–84.
Goncalves R, Lourenco A, Silva SN. A social cost perspective in the wake of the Portuguese strategy for the fight against drugs. Int J Drug Policy. 2015;26(2):199–209.
Ferreira S. Portugal’s radical drugs policy is working. Why hasn’t the world copied it? The Guardian. 2017 Dec 5.
Bajekal N. Want to win the war on drugs? Portugal might have the answer. Time. 2018 Aug 1.
Sharbaugh MS, Althouse AD, Thoma FW, Lee JS, Figueredo VM, Mulukutla SR. Impact of cigarette taxes on smoking prevalence from 2001-2015: a report using the Behavioral and Risk Factor Surveillance Survey (BRFSS). PLoS One. 2018;13(9):e0204416.
Frazer K, Callinan JE, McHugh J, van Baarsel S, Clarke A, Doherty K, et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2016;(2):CD005992.
National Conference of State Legislatures. State Medical Marijuana Laws June 5, 2019. Available from: http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx.
National Conference of State Legislatures. Marijuana Overview May 28, 2019. Available from: http://www.ncsl.org/research/civil-and-criminal-justice/marijuana-overview.aspx.
Kuehn B. Declining opioid prescriptions. JAMA. 2019;321(8):736.
Dowell D, Haegerich T, Chou R. CDC guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49.
Herring AA, Perrone J, Nelson LS. Managing opioid withdrawal in the emergency department with buprenorphine. Ann Emerg Med. 2019;73(5):481–7.
Herring A, Snyder H, Moulin A, Luftig J, Sampson A, Trozky R, et al. Buprenorphine Guide: ED-BRIDGE; 2018. Available from: https://ed-bridge.org/guide.
Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz KRB, Viswanath K, editors. Health behavior and health education. 4th ed. San Francisco: Wiley; 2008. p. 465–85.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Samuels, E.A., Xuan, Z., Bernstein, E. (2021). Substance Use: A Social Emergency Medicine Perspective. In: Alter, H.J., Dalawari, P., Doran, K.M., Raven, M.C. (eds) Social Emergency Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-65672-0_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-65672-0_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-65671-3
Online ISBN: 978-3-030-65672-0
eBook Packages: MedicineMedicine (R0)