Abstract
Parkinson’s disease (PD) is a progressive neurodegenerative disorder primarily associated with motor dysfunctions. By the time of definitive diagnosis, about 60% of dopaminergic neurons have already been lost; moreover, even if dopaminergic drugs are highly effective in symptoms control, they only help maintaining a near-healthy condition when started as soon as possible. Therefore, interest in identifying early biomarkers of PD has grown in recent years, especially using neurophysiological techniques such as electroencephalography (EEG). This study aims to investigate brain complexity differences in PD patients compared to healthy controls, focusing on the beta band using approximate entropy (ApEn) analysis of resting-state EEG recordings. Sixty participants were recruited, including 25 PD patients and 35 healthy elderly subjects, matched for age and gender. EEG were recorded for each participant and ApEn values were computed in the beta 1 (13–20 Hz) and beta 2 (20–30 Hz) frequency bands for each EEG-channel and for ROIs. PD patients showed statistically lower ApEn values compared to controls in both beta 1 and beta 2 bands. Regarding electrodes analysis, beta 1 band alterations were found in frontocentral areas, while beta 2 band alterations were observed in centroparietal and frontocentral areas. Considering ROIs, statistically lower ApEn values for PD patients has been reported in central and parietal ROIs in the beta 2 band. Complexity reduction in these areas may underlie beta oscillatory activity dysfunction, reflecting impaired cortical mechanisms associated with motor dysfunction in PD. The results suggest that ApEn analysis of resting EEG activity may serve as a potential tool for early PD detection. Further studies are necessary to validate this approach in PD diagnosis and rehabilitation planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is the second most common progressive neurodegenerative disorder of the central nervous system after Alzheimer’s disease [1] and the most common neurodegenerative movement disorder [2]. Moreover, PD ranks among the most prevalent neurological diseases in the aging population and the risk of the disease rises steeply with aging [3,4,5,6]. Despite the clinical picture including other non-motor symptoms, such as cognitive impairments or psychiatric disturbance, the PD is primarily associated to motor dysfunctions, such as bradykinesia/akinesia, rigidity, tremor, and postural instability [7]. PD is pathologically characterized by the loss of dopaminergic neurons in the substantia nigra pars compacta and by the presence of Lewy bodies. Several studies on non-human primates [5, 8] reported that physiological aging and degeneration of dopaminergic neurons in PD are linked by the same cellular mechanisms arguing that aging induces a pre-parkinsonian state and that the cellular mechanisms of dopaminergic neuron breakdown during normal aging are accelerated or exaggerated in Parkinson’s disease through a combination of genetic and environmental factors. Moreover, recent studies [9,10,11] have shown that mitochondrial dysfunction and neuroinflammation, age-related alterations, have been identified as mechanisms implicated in the pathophysiology of PD contributing to the onset and progression of the disease.
PD clinical diagnosis is mainly based on individual’s history, symptoms observation including bradykinesia in combination with a resting tremor or rigidity [2, 7, 12] and physical exams. There is not a specific lab or imaging test that can diagnose PD. However, certain tests such as magnetic resonance imaging of the brain (MRI brain), specific single-photon emission computerized tomography (SPECT) scan called a dopamine transporter (DAT) scan, or blood work can be used to support the diagnosis of PD or to rule out other medical conditions that can mimic PD [13, 14]. PD diagnosis, especially in the early stages, is difficult and takes time, especially because it occurs when symptoms are already appearing. By the time of definitive diagnosis, an estimated 60% of dopaminergic neurons have already been lost making the major part of the interventions ineffective due to the high degree of neural damage already present. Currently available therapies, aimed at slowing the progression of the disease and preserving patients’ autonomy, appear to be not entirely effective given the high degree of neuronal damage already present at the time of diagnosis [15]. Therefore, the low efficacy of treating patients is due to the late diagnosis and start of therapy. It is believed that the development of early diagnosis and preventive treatment will delay the onset of specific symptoms [16, 17]. Because of that, in the last few years, there was an increasing interest in investigating possible biomarkers of early stages of the disease to intercept it earlier and make the pharmacological and rehabilitation treatments more effective.
In general, PD disorders were largely studied by structural and functional imaging methods [14, 18, 19]; however, recently, there were an increment of scientific interest in exploring the disease using neurophysiological techniques such as magnetoencephalography (MEG) or electroencephalography (EEG). In particular, EEG is a non-invasive technique able to represent brain electrical activity with high temporal resolution and high test–retest reliability [20, 21]. This technique is more easily disseminated, cheaper and could be used for a broader population screening than imaging methods, which are expensive, invasive, and not widely disseminated.
Many studies have focused their attention in detecting linear and non-linear EEG features alterations in PD patients by means of different analysis’s methods in time and frequency domains [19, 22, 23].
Since PD is a neurodegenerative disease that impacts on cortical activity recorded via EEG, many studies have focused on analyzing the alterations that occur in the EEG power spectral density (PSD), especially in the alpha and beta frequency ranges, which are those most involved in the sensorimotor activity. Mainly, the past literature found an increase of PSD of slower EEG frequency bands (delta and theta) and a decrease of faster bands (alpha and Beta), suggesting a global slowing of EEG activity in PD patients compared with normal subjects [24,25,26,27]. In particular, this global slowing of EEG activity was correlated to the severity of cognitive impairment and motor disability in both demented and non-demented PD patients compared to healthy subjects [24, 28, 29]. Moreover, Polverino et al. [30] highlighted similar behavior in alpha band between Alzheimer’s disease (AD) and PD-demented patients compared to healthy subjects and different behavior in beta band between demented PD patients respect to AD patients. The latter result in beta band was found also in non-demented PD group.
These results highlight how differences in the alpha band may be related to the patient’s cognitive state, regardless they were caused by AD or PD, while the beta band seems to be more related to motor processes, and thus more specifically to PD.
Accordingly, the beta band investigation could lead to an understanding of the pathophysiology of PD and to enhanced therapeutic/rehabilitative interventions [31].
Indeed, differences in beta band were reported both in resting state and during motor tasks during EEG recordings. Pollock et al. [32] reported increased sensorimotor cortical power in beta band during rest as well as during isometric contraction of the upper limbs in early PD compared to controls. Moreover, their results showed a significant positive correlation during isometric contraction between primary sensorimotor cortex power in beta frequency and the Unified Parkinson’s disease rating scale part III (UPDRS III), a validated scale used to assess the severity of PD motor complications [33].
Recently, since PD is a neurodegenerative disease involving disconnections between and within multiple brain areas and basal ganglia, brain connectivity analysis has been applied to investigate the pathophysiology of this disease, focusing the attention on the study of beta band. Moreover, because PD is characterized by an excess of subcortical beta oscillations [34, 35], connectivity analyses have focused on studying mainly the beta band.
Leviashvili et al. [36] found reduced connectivity in the central-executive network and dorsal-attention network, and increased connectivity in the ventral-attention network in beta band of PD patients compared to healthy subjects demonstrating that reported results on resting-EEG data are in line with other functional magnetic resonance imaging (fMRI) studies on the same networks [37,38,39]. In a recent study, functional connectivity and spectral analysis were analyzed in the early stages of PD, showing a reduction in connectivity in beta frequency band [40]. A recent longitudinal study [41] reported a gradual connectivity impairment in high-frequency alpha and beta bands correlating the global assessment of PD patients with the level of the networks’ disconnection.
These studies report how EEG data analysis may be useful in describing the modifications due to PD. However, it would be still necessary to use new analysis methods to explore EEG signals of PD patients and to reveal other features of brain organization crucial information underlying brain dysfunctions. In recent years, with the possibility of applying advanced analysis and considering EEG non-linear and non-stationary signals, there has been a focus on the study of non-linear features by applying different parameters such as Fractal connectivity, correlation dimension, delay differential equations, higher Lyapunov exponent and complexity parameters in order to detect differences existing both in physiological state, and in diseases such as Alzheimer’s and Parkinson’s [25, 42,43,44,45,46,47,48,49,50,51].
One method that is still in its infancy but is revealing important results is the complexity or entropy analysis of the EEG signals. Entropy is a non-linear approach representing the irregularity, complexity, or unpredictability of a signal [52]. Because neural systems have been exhibited non-linear chaotic behavior, entropy measures can be successfully applied to the EEG signal to detect its variability or complexity. Entropy analysis has been reported as a powerful method for EEG in order to quantify brain functions related to altered state due to neurodegenerative diseases [53,54,55,56].
Pezard et al. [25] have investigated the EEG complexity of PD patients brain dynamics by the means of local entropy. The local entropy index shows a significant increase in patients compared to healthy subjects.
Recently, Pappalettera et al. [56] applied approximate entropy (ApEn) analysis to EEG signals in order to explore the brain resting state differences between PD patients and healthy controls in terms of complexity of the signals. They found statistically higher ApEn values in PD in the whole brain respect to the control group, highlighting differences in EEG signal complexity between healthy subjects and PD patients.
Although ApEn is an interesting analysis to investigate further, there are not many studies in the literature regarding the exploration of the EEG of Parkinson’s patients through this index. With the aim to fill this gap and further investigate the analysis done previously by our group [56, 57], here we investigated the modulation of ApEn in the beta band, which is reported as specifically affected by PD [31, 58]. During resting-state recordings, ApEn index was computed in the beta frequency range on each electrode first and splitting the scalp electrodes into regions of interest (ROIs), then comparing PD patients and healthy subjects’ outcomes.
Participants and methods
Participants
A total of 60 participants were involved in the study and divided into two groups, the CTRL group consisting of healthy elderly subjects (n = 35) and the PD group consisting of Parkinson’s patients (n = 25), matched for age and gender as reported in Table 1. In particular, the PD group consisted of 11 non-demented PD patients already included in a previous article [56] and 14 non-demented PD patients extracted from a public database [59]. All experimental procedure were undertaken with the signed consent of each participant, according to the World Medical Association Code of Ethics (1997) and carried out conforming to the Declaration of Helsinki and standards set by the Author’s Institutional Review Board.
For each PD patient, the disease was diagnosed considering the medical history and physical and neurological examinations as well as the response to levodopa drugs. Exclusion criteria were atypical Parkinsonism, neuroleptic drug use, dopamine blocking agents, alcohol abuse, presence of other neurological or psychiatric conditions, and any other severe illness. The Unified Parkinson’s Disease Rating Scale III (UPDRS) was used as measure of severity of motor disability [33]. The UPDRS score was 15.1 ± 1.2 (mean ± standard error (SE)). All PD patients underwent the MMSE scales, showing a mean score of 28.2 ± 0.3 (mean ± standard error (SE)).
For the healthy elderly control group, the subjects enrolled were physically and intellectually healthy with no symptoms or history of any neurological or psychiatric disorder.
Data recordings and preprocessing
Resting-state EEG were recorded from each participant, in both the PD and CTRL groups, for at least 4 min. In our laboratory, the EEG data were collected using 19-channels clinical headset for PD group of our clinical center and 32-channels headset for CTRL, positioned according to the International 10–20 system. All channels’ impedance was kept below 5 KΩ and the sampling rate was set up at 256 Hz. Electro-oculographic vertical and horizontal signals were recorded from two separate channels to monitor ocular movements and blinking.
EEG data of the online dataset were recorded with a sampling rate of 512 Hz, using a 32-channels BioSemi ActiveTwo system (Fp1, AF3, F7, F3, FC1, FC5, T7, C3, CP1, CP5, P7, P3, Pz, PO3, O1, Oz, O2, PO4, P4, P8, CP6, CP2, C4, T8, FC6, FC2, F4, F8, AF4, Fp2, Fz, Cz), performed off-medication, in resting-state condition.
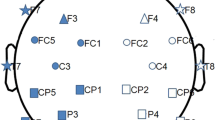
In order to make all records consistent, the same 19-channels obtained from our PD database were selected according to the International 10–20 system (Fp2, F4, C4, P4, O2, F8, T8, P8, Fp1, F3, C3, P3, O1, F7, T7, P7, Fz, Cz, Pz) for each recording, specifically in EEG data of public database and in CTRL group. Moreover, the EEG data of public database were downsampled to 256 Hz.
The participants were seated in a comfortable armchair, placed in a dimly lit, sound-damped, and electrically shielded room.
EEG data were processed in MATLAB (MathWorks, Natick, MA, USA) employing already used in-home scripts based on the EEGLAB toolbox (Swartz Center for Computational Neurosciences, La Jolla, CA, USA) [60,61,62]. Firstly, the data were band-pass filtered from 0.2 to 47 Hz using a finite impulse response (FIR) filter. Then, EEG recordings were processed segmenting the signal in 2-s duration non-overlapped epochs in order to remove artifactual activity, such as eye movements, scalp muscle contraction, and cardiac activity first by an EEG expert visual inspection. The Infomax ICA algorithm, which allows the separation of statistically independent sources from multichannel EEG recordings as implemented in the EEGLAB, was applied to remove significant artifacts [63,64,65]. ICA-based artifact removal has been done via visual inspection, considering the localization on the scalp, the spectrum, and the time pattern of the single components. At the end of the artifact removal procedure, at least 3-min EEG recordings, so about 100 2-s epochs remained for each subject.
Entropy analysis
In the present study, we applied ApEn for complexity measures instead of other entropy measures because of ApEn that presents many advantages: it maintains a good reproducibility when used with time series [62, 66]; it is almost unaffected by noise, it is finite for composite, stochastic, and noisy deterministic processes [67]; and it detects the changes in underlying episodic behavior undetected by peak occurrences or amplitudes [68]. Moreover, ApEn has been extensively used in studies of time series of physiologic parameters to assess their degree of randomness [56, 57, 62, 69,70,71].
For all the presented reasons, ApEn would be extremely helpful in brain function understanding, given the complex and dynamical characteristics of the cerebral systems.
ApEn values were computed, in each participant, for each EEG channel and for beta 1 (13–20 Hz) and beta 2 (20–30 Hz) frequency bands using in-house developed MATLAB software and settings applied in other previously studies by our group. Firstly, a value of ApEn was computed for each channel and each epoch in each of the beta frequency bands. Finally, for each EEG recording, those values were averaged among the epochs to obtain a single ApEn value for each channel in each frequency band [56, 57, 62, 70, 71]. The software generates ApEn dimensionless values from 0 to 2: the higher the value of ApEn, the more irregular and less predictable the signal is; the lower this value, the more periodic and stable the signal tends to be [56].
The ApEn is computed using two input parameters: m, the model length, that was set equal to 2 and r, the tolerance factor, that was equal to 0.2*variance (x) [66, 72,73,74], where x is a 2-s long epoch of a specific channel. These well-established values are selected because they have been demonstrated to produce good statistical reproducibility for time series of length N > 60 [75]. Normalizing r in this manner gives ApEn a translation and scale invariance; in this way, it remains unchanged under uniform process magnification, reduction, or constant shift to higher or lower values [76]. In summary, the ApEn is calculated as \(\text{ApEn}={\Phi }_{m}-{\Phi }_{m+1}\):
where Ni represents the number of points that are within r of their corresponding point in the original sequence Y, at point i:
After electrode-by-electrode analysis was conducted, the scalp was subsequently divided into five ROIs (frontal: F3, Fz, F4; Central: C3, Cz, C4; parietal: P3, Pz, P4; temporal: F7, T7, P7, F8, T8, P8; occipital: O1, O2) and the entropy values of the electrodes belonging to a region were averaged with each other in order to have an ApEn value for each ROI considered.
Statistical evaluation
The two-tailed unpaired Student’s t-test was performed to highlight the statistical differences of the ApEn values of each channel comparing PD and CTRL groups in beta 1 and beta 2 frequency bands, setting the statistical threshold level at 0.05. Before the application of the statistical t-test, the distribution of ApEn values was checked for each channel by the Kolmogorov–Smirnov normality test for both PD patients and the control group. The test showed that each channel presented a normal distribution of ApEn values, thus allowing the application of the two-tailed unpaired Student’s t-test.
Moreover, a statistical one-way ANOVA and a post hoc analysis with the Duncan’s test were applied to the ROIs ApEn values to evaluate the statistical differences between the PD and CTRL groups for each ROI in beta 1 and beta 2 frequency bands.
Results
In order to investigate the differences between the PD and the CTRL group, ApEn values were computed for each participant in beta 1 and beta 2 frequency bands for each channel. Significant differences between PD and CTRL have been highlighted in beta 1 and beta 2 frequency bands. P-values of each studied channel are reported in the Supplementary Table 1. Considering the beta 1 band, the Fz channel highlights a statistically significant difference between the two groups. In fact, PD patients showed statistically lower ApEn values in the frontal, premotor areas, respect to CTRL group, whereas, regarding the beta 2 band, the PDs showed statistically lower ApEn values in the centroparietal, motor, and frontocentral, sensorimotor areas compared to the CTRL group, reporting statistical differences in F4, C4, P4, P3, Cz, Pz, channels. The topographical maps of the ApEn values of both groups and the distribution of the statistically significant differences between the two groups for each frequency band were reported in Fig. 1.
ApEn values of the CTRL and PD groups and the distribution of statistical differences between them, reported in the beta 1 and beta 2 bands, were plotted on the scalp in the first, second, and third columns, respectively. The significant p-values (< 0.05) are represented on the scalp by the red color
Subsequently, ApEn values for frontal, central, parietal, temporal, and occipital ROIs were calculated in order to demonstrate regional differences between groups in beta 1 and beta 2 frequency bands. While no statistical differences were reported in beta 1, in beta 2 the ANOVA showed a main effect F (degrees of freedom = 4, error degrees of freedom = 232) = 5.5604, p = 0.00027 and a significant reduction of PD ApEn values in the central (p = 0.043940) and in parietal (p = 0.036521) ROIs compared to CTRL group after the Duncan’s post hoc test was found (Fig. 2). P-values are reported in the Supplementary Table 2.
Discussion
Parkinson’s disease (PD) is a neurodegenerative disease widely known as a predominantly motor disorder produced by dopaminergic deficiency in the basal ganglia. In the last decades, considering the idea that the human brain can be modeled as a highly complex dynamical system, non-linear analysis has been applied to deeper pathological conditions in neurodegenerative processes and to identify characteristics of disturbed cortical mechanisms, mainly on motor frequency. Among these, entropy is applied to measure the complexity and therefore the unpredictability and randomness of a time series; in particular, higher entropy values has been associated with randomness and less regular system [70, 71, 75].
In this framework, in order to make interventions more effective and thus diagnose Parkinson’s early, the goal of the current study has been to investigate the brain complexity differences present in PD patients compared to healthy ones focusing on the beta band, the one most affected by PD and motor dysfunction, by the means of approximate entropy (ApEn).
The results of the current research highlighted the remarkable modifications of the signal complexity regarding the beta motor frequency band in the premotor and sensorimotor brain regions due to the PD in both electrode-by-electrode and per ROIs analysis.
Our results showed that PD patients presented statistically lower ApEn values than CTRL subjects. Regarding the beta 2 band, PD patients showed significantly lower ApEn values in the centroparietal, motor, and frontocentral, sensorimotor areas compared with the CTRL group confirming the differences in signal complexity and disease-related changes in sensorimotor regions and in the frequency band associated with motor dysfunction. These results were evident in both electrode-by-electrode analysis (Fig. 1) and ROIs (Fig. 2).
Considering the beta 1 band, the significant decrease in ApEn found in patients in the Fz channel of the premotor area (Fig. 1) is not confirmed in the analysis of ROIs, probably because the single channel information was smoothed in the averaging process of the frontal ROI while the result would appear to be more focal. However, a future study with higher numbers of subjects and electrodes could potentially confirm the observed beta 1 trend. In line with the results of the present study over the beta frequency band and the results of the previous study over the global frequency domain [56], Han et al. examined the complexity of the global frequency domain and of the different frequency sub-bands, including the beta one, reporting higher complexity values in the global frequency domain and lower values in the beta band of PD patients compared to healthy subjects [77]. These results are consistent with our evidence, and they revealed that, depending on the frequency band analyzed, there are different modulations made by PD.
Furthermore, our results are consistent with previous ApEn analysis of healthy elderly subjects that showed a reduction in complexity in the beta 2 frequency band compared to healthy younger subjects [57], highlighting a physiological reduction in entropy, which, based on our evidence, would seem to be more pronounced in the pathological condition of PD. However, in this case, our results are age unrelated, being balanced between the two groups, emphasizing that the decrease is closely related to the neurodegeneration of the pathology.
In the same framework, Chen et al. reported a reduced complexity in oscillatory beta band activity of PD using the Lempel–Ziv complexity analysis [78]. Even using the permutation entropy the complexity of beta band EEG resting-state was showed reduced in PD compared to healthy subjects [79].
Given that, it can be speculated that a loss of complexity appears when the nervous system becomes functionally compromised and that the lower ApEn values, namely the loss of signal complexity, reported in PD could be directed linked to the functional impairment of the nervous system elicited by the neurodegeneration and to the loss of complexity of the networks that generate the rhythm. Our results provide further support for the suggestion that a loss of complexity appears when the nervous system becomes functionally compromised [43, 80,81,82,83,84,85,86,87].
Concerning our evidences reported in beta 1 and beta 2, they may reflect the different activity of the beta sub-bands. The beta 1 and beta 2 different changes which we observed for the PD patients support the hypothesis of Marceglia et al. [88], that two distinct information channels in the cortico-basal ganglia–thalamo-cortical loop, involved in motor and non-motor information processing, are formed in the parkinsonian brain. The relative functional division between activities in the beta band might be supported by the evidence for different patterns of pharmacological sensitivity [89] and cortico-subthalamic coupling [90].
Our results are consistent even in the regions where we found significantly lower ApEn values in PD compared to CTRL. Specifically, for beta 1 the premotor and for beta 2 the sensorimotor areas, these areas are all directly affected by motor activity, as reported by numerous studies, thus being part of motor networks and are affected by the neurodegeneration implied in PD. Several studies based on fMRI have reported functional connectivity alterations of sensorimotor network in PD patients [91,92,93].
The reduction of complexity in the Beta band in the premotor (regarding beta 1) and sensorimotor (regarding beta 2) areas may underlie the beta oscillatory activity disfunction resulting in motor impairment, such as bradykinesia, rigidity, and tremor [78, 94].
Levy et al. [95] reported that beta oscillatory activity in the basal ganglia associated with the pathology that gave rise to tremor in PD. Beta band resting-state activity getting less complex, namely more ordered, detected in our study may be related to the motor symptoms, such as resting tremor, in PD patients.
In summary, our article expands and reinforces the existing literature both about the application of ApEn and about the differences in brainwave complexity Parkinson’s patients by reporting not only a loss of complexity in the beta band, which is related to sensorimotor processing and affected by the disease, but by finding these changes in specific sensorimotor areas, even considering the entire scalp.
Regarding the ApEn, although there are few applications in the literature to EEG data of patients with Parkinson’s disease, compared to other non-linear methods, it offers advantages such as straightforward interpretations, good reproducibility when applied to time series, scale invariance, and model independence. It is capable to detect changes in the underlying episodic behavior that are not reflected in the occurrences or amplitudes of spikes [51]. Applied to resting-state EEG data, either by analyzing electrodes or ROIs, ApEn emerges as a powerful and easily available tool to distinguish PD patients from healthy elderly controls.
Overall, based on these considerations, we can state that ApEn could provide a potential way to have an innovative biomarker to distinguish the pathological conditions, or intercept stages prior to the disease manifestation. Early diagnosis, through such a simple analysis, could potentially help delay the onset of symptoms and improve patients’ quality of life by applying early treatments.
Certainly, some methodological limitations should be considered, first of all the sample size of PD patients, which was increased from the previous published article [56] but still narrow, and that the EEG device has some technical limitations such as low spatial resolution which is counterbalanced by a very high temporal resolution. Moreover, the quality of the EEG recordings depends on the expertise of the technician, who must follow international guidelines for EEG headset application; it depends on the environmental noise, which can be minimized by conducting the recordings in a room that is as soundproofed and electrically shielded as possible and on the cooperation of the patients, who are undergoing recordings in a resting state to minimize any kind of movement.
Conclusions
Parkinson’s disease is a complex neurodegenerative disease primarily associated to motor dysfunctions. The ApEn analysis has been shown to be successful in detecting pathological features of activity in the beta band related to the nervous system functional impairments and to the disease development in early stages of PD.
In future studies, the results should be further deepened concerning disease progression, for instance by investigating the correlation between ApEn values and motor scores of UPDRS scale.
Moreover, for the purpose of validating this approach, it will be necessary to enroll a larger number of PD patients. In line with this, it might be interesting to use the ApEn as an input feature of a classifier for early detection of PD. Furthermore, although in this study we focused on resting EEG to demonstrate the potential of this simple recording analyzed with ApEn and to bring our research closer to a more clinical setting, it would be interesting to apply ApEn analysis on EEG recordings during cognitive and motor tasks to get a more complete picture of neurodegeneration implicated by PD from the early stage of the disease, highlighting the cognitive and motor changes brought about by Parkinson’s from the earliest stages of the disease.
Surely, as a step forward, the results of the present research showed that resting brain networks exhibit a different degree of complexity between Parkinson’s patients and control subjects in the beta bands and the related sensorimotor regions, suggesting that Parkinson modulates the underlying communications within these regions.
In conclusion, approximate entropy could be a useful index to support an early diagnosis, follow the progression of Parkinson’s disease and plan rehabilitation interventions.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015;386:896–912. https://doi.org/10.1016/s0140-6736(14)61393-3.
Tysnes OB, Storstein A. Epidemiology of Parkinson's disease. J Neural Transm (Vienna). 2017;124:901–05. https://doi.org/10.1007/s00702-017-1686-y.
Bennett DA, Beckett LA, Murray AM, Shannon KM, Goetz CG, Pilgrim DM, Evans DA. Prevalence of parkinsonian signs and associated mortality in a community population of older people. N Engl J Med. 1996;334:71–6. https://doi.org/10.1056/nejm199601113340202.
Tanner CM, Goldman SM. Epidemiology of Parkinson’s disease. Neurol Clin. 1996;14:317–35. https://doi.org/10.1016/s0733-8619(05)70259-0.
Collier TJ, Kanaan NM, Kordower JH. Ageing as a primary risk factor for Parkinson’s disease: evidence from studies of non-human primates. Nat Rev Neurosci. 2011;12:359–66. https://doi.org/10.1038/nrn3039.
Riederer P, Lange KW. Pathogenesis of Parkinson’s disease. Curr Opin Neurol Neurosurg. 1992;5:295–300.
Kouli A, Torsney KM, Kuan WL. Parkinson’s disease: Etiology, neuropathology, and pathogenesis. In: Stoker TB, Greenland JC, editors. Parkinson’s Disease: Pathogenesis and Clinical Aspects. Brisbane (AU): Codon Publications; 2018.
Collier TJ, Kanaan NM, Kordower JH. Aging and Parkinson’s disease: different sides of the same coin? Mov Disord. 2017;32:983–90. https://doi.org/10.1002/mds.27037.
Liu JP. Molecular mechanisms of ageing and related diseases. Clin Exp Pharmacol Physiol. 2014;41:445–58. https://doi.org/10.1111/1440-1681.12247.
Cossu D, Hattori N. Influence of aging, mitochondrial dysfunction, and inflammation on Parkinson’s disease. Neural Regen Res. 2024;19:1197–8. https://doi.org/10.4103/1673-5374.385873.
Rango M, Bresolin N. Brain mitochondria, aging, and Parkinson’s disease. Genes (Basel). 2018;9. https://doi.org/10.3390/genes9050250.
Beitz JM. Parkinson’s disease: a review. Front Biosci (Schol Ed). 2014;6:65–74. https://doi.org/10.2741/s415.
Bidesi NS, Vang Andersen I, Windhorst AD, Shalgunov V, Herth MM. The role of neuroimaging in Parkinson’s disease. J Neurochem. 2021;159:660–89. https://doi.org/10.1111/jnc.15516.
Meijer FJ, Goraj B. Brain MRI in Parkinson’s disease. Front Biosci (Elite Ed). 2014;6:360–9. https://doi.org/10.2741/e711.
Adler CH. Premotor symptoms and early diagnosis of Parkinson’s disease. Int J Neurosci. 2011;121 Suppl 2:3–8. https://doi.org/10.3109/00207454.2011.620192.
Ugrumov M. Development of early diagnosis of Parkinson’s disease: illusion or reality? CNS Neurosci Ther. 2020;26:997–1009. https://doi.org/10.1111/cns.13429.
Schapira AH, Obeso J. Timing of treatment initiation in Parkinson’s disease: a need for reappraisal? Ann Neurol. 2006;59:559–62. https://doi.org/10.1002/ana.20789.
Pagano G, Niccolini F, Politis M. Imaging in Parkinson’s disease. Clin Med (Lond). 2016;16:371–5. https://doi.org/10.7861/clinmedicine.16-4-371.
Chen R, Berardelli A, Bhattacharya A, Bologna M, Chen KS, Fasano A, Helmich RC, Hutchison WD, Kamble N, Kühn AA, et al. Clinical neurophysiology of Parkinson’s disease and parkinsonism. Clin Neurophysiol Pract. 2022;7:201–27. https://doi.org/10.1016/j.cnp.2022.06.002.
Melgari JM, Curcio G, Mastrolilli F, Salomone G, Trotta L, Tombini M, di Biase L, Scrascia F, Fini R, Fabrizio E, et al. Alpha and beta EEG power reflects l-dopa acute administration in parkinsonian patients. Front Aging Neurosci. 2014;6:302. https://doi.org/10.3389/fnagi.2014.00302.
Miraglia F, Tomino C, Vecchio F, Alù F, Orticoni A, Judica E, Cotelli M, Rossini PM. Assessing the dependence of the number of EEG channels in the brain networks’ modulations. Brain Res Bull. 2020. https://doi.org/10.1016/j.brainresbull.2020.11.014.
Cozac VV, Gschwandtner U, Hatz F, Hardmeier M, Rüegg S, Fuhr P. Quantitative EEG and cognitive decline in Parkinson’s disease. Parkinsons Dis. 2016;2016:9060649. https://doi.org/10.1155/2016/9060649.
Nwogo RO, Kammermeier S, Singh A. Abnormal neural oscillations during gait and dual-task in Parkinson’s disease. Front Syst Neurosci. 2022;16:995375. https://doi.org/10.3389/fnsys.2022.995375.
Neufeld MY, Blumen S, Aitkin I, Parmet Y, Korczyn AD. EEG frequency analysis in demented and nondemented parkinsonian patients. Dementia. 1994;5:23–8. https://doi.org/10.1159/000106690.
Pezard L, Jech R, Růzicka E. Investigation of non-linear properties of multichannel EEG in the early stages of Parkinson’s disease. Clinical neurophysiology: official journal of the International Federation of Clinical Neurophysiology. 2001;112:38–45. https://doi.org/10.1016/s1388-2457(00)00512-5.
Soikkeli R, Partanen J, Soininen H, Pääkkönen A, Riekkinen P. Slowing of EEG in Parkinson’s disease. Electroencephalogr Clin Neurophysiol. 1991;79:159–65. https://doi.org/10.1016/0013-4694(91)90134-p.
Shirahige L, Berenguer-Rocha M, Mendonça S, Rocha S, Rodrigues MC, Monte-Silva K. Quantitative electroencephalography characteristics for Parkinson’s disease: a systematic review. J Parkinsons Dis. 2020;10:455–70. https://doi.org/10.3233/jpd-191840.
Kozak VV, Chaturvedi M, Gschwandtner U, Hatz F, Meyer A, Roth V, Fuhr P. EEG slowing and axial motor impairment are independent predictors of cognitive worsening in a three-year cohort of patients with Parkinson’s disease. Front Aging Neurosci. 2020;12:171. https://doi.org/10.3389/fnagi.2020.00171.
Neufeld MY, Inzelberg R, Korczyn AD. EEG in demented and non-demented parkinsonian patients. Acta Neurol Scand. 1988;78:1–5. https://doi.org/10.1111/j.1600-0404.1988.tb03609.x.
Polverino P, Ajčević M, Catalan M, Mazzon G, Bertolotti C, Manganotti P. Brain oscillatory patterns in mild cognitive impairment due to Alzheimer’s and Parkinson’s disease: an exploratory high-density EEG study. Clinical Neurophysiol: official journal of the International Federation of Clinical Neurophysiology. 2022;138:1–8. https://doi.org/10.1016/j.clinph.2022.01.136.
Little S, Brown P. The functional role of beta oscillations in Parkinson’s disease. Parkinsonism Relat Disord. 2014;20 Suppl 1:S44–8. https://doi.org/10.1016/s1353-8020(13)70013-0.
Pollok B, Krause V, Martsch W, Wach C, Schnitzler A, Südmeyer M. Motor-cortical oscillations in early stages of Parkinson’s disease. J Physiol. 2012;590:3203–12. https://doi.org/10.1113/jphysiol.2012.231316.
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, et al. Movement disorder society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23:2129–70. https://doi.org/10.1002/mds.22340.
Little S, Tan H, Anzak A, Pogosyan A, Kühn A, Brown P. Bilateral functional connectivity of the basal ganglia in patients with Parkinson’s disease and its modulation by dopaminergic treatment. PLoS One. 2013;8:e82762. https://doi.org/10.1371/journal.pone.0082762.
Boon LI, Hillebrand A, Olde Dubbelink KTE, Stam CJ, Berendse HW. Changes in resting-state directed connectivity in cortico-subcortical networks correlate with cognitive function in Parkinson’s disease. Clinical Neurophysiol: official journal of the International Federation of Clinical Neurophysiology. 2017;128:1319–26. https://doi.org/10.1016/j.clinph.2017.04.024.
Leviashvili S, Ezra Y, Droby A, Ding H, Groppa S, Mirelman A, Muthuraman M, Maidan I. EEG-based mapping of resting-state functional brain networks in patients with Parkinson’s disease. Biomimetics (Basel). 2022;7:231. https://doi.org/10.3390/biomimetics7040231.
Nachev P, Kennard C, Husain M. Functional role of the supplementary and pre-supplementary motor areas. Nat Rev Neurosci. 2008;9:856–69. https://doi.org/10.1038/nrn2478.
Brown CA, Schmitt FA, Smith CD, Gold BT. Distinct patterns of default mode and executive control network circuitry contribute to present and future executive function in older adults. Neuroimage. 2019;195:320–32. https://doi.org/10.1016/j.neuroimage.2019.03.073.
Cai S, Peng Y, Chong T, Zhang Y, M von Deneen K, Huang L Alzheimer’s Disease Neuroimaging Initiative. Differentiated effective connectivity patterns of the executive control network in progressive MCI: a potential biomarker for predicting AD. Curr Alzheimer Res. 2017;14:937–50. https://doi.org/10.2174/1567205014666170309120200.
Conti M, Bovenzi R, Garasto E, Schirinzi T, Placidi F, Mercuri NB, Cerroni R, Pierantozzi M, Stefani A. Brain functional connectivity in. Front Neurol. 2022;13:844745. https://doi.org/10.3389/fneur.2022.844745.
Yassine S, Gschwandtner U, Auffret M, Achard S, Verin M, Fuhr P, Hassan M. Functional brain dysconnectivity in Parkinson’s disease: a 5-year longitudinal study. Mov Disord. 2022;37:1444–53. https://doi.org/10.1002/mds.29026.
Stam CJ. Nonlinear dynamical analysis of EEG and MEG: review of an emerging field. Clin Neurophysiol : official journal of the International Federation of Clinical Neurophysiology. 2005;116:2266–301. https://doi.org/10.1016/j.clinph.2005.06.011.
Müller V, Lutzenberger W, Pulvermüller F, Mohr B, Birbaumer N. Investigation of brain dynamics in Parkinson’s disease by methods derived from nonlinear dynamics. Exp Brain Res. 2001;137:103–10. https://doi.org/10.1007/s002210000638.
Chang KH, French IT, Liang WK, Lo YS, Wang YR, Cheng ML, Huang NE, Wu HC, Lim SN, Chen CM, et al. Evaluating the different stages of Parkinson’s disease using electroencephalography with Holo-Hilbert spectral analysis. Front Aging Neurosci. 2022;14:832637. https://doi.org/10.3389/fnagi.2022.832637.
Rey M, Guillemant P. Contribution of non-linear mathematics (chaos theory) to EEG analysis. Neurophysiol Clin. 1997;27:406–28. https://doi.org/10.1016/s0987-7053(97)88807-7.
Fell J, Röschke J. Nonlinear dynamical aspects of the human sleep EEG. Int J Neurosci. 1994;76:109–29. https://doi.org/10.3109/00207459408985997.
Yuvaraj R, Murugappan M. Hemispheric asymmetry non-linear analysis of EEG during emotional responses from idiopathic Parkinson’s disease patients. Cogn Neurodyn. 2016;10:225–34. https://doi.org/10.1007/s11571-016-9375-3.
Lainscsek C, Hernandez ME, Weyhenmeyer J, Sejnowski TJ, Poizner H. Non-linear dynamical analysis of EEG time series distinguishes patients with Parkinson’s disease from healthy individuals. Front Neurol. 2013;4:200. https://doi.org/10.3389/fneur.2013.00200.
Lemoine É, Neves Briard J, Rioux B, Gharbi O, Podbielski R, Nauche B, Toffa D, Keezer M, Lesage F, Nguyen DK, et al. Computer-assisted analysis of routine EEG to identify hidden biomarkers of epilepsy: a systematic review. Comput Struct Biotechnol J. 2024;24:66–86. https://doi.org/10.1016/j.csbj.2023.12.006.
Kaposzta Z, Czoch A, Mukli P, Stylianou O, Liu DH, Eke A, Racz FS. Fingerprints of decreased cognitive performance on fractal connectivity dynamics in healthy aging. Geroscience. 2024;46:713–36. https://doi.org/10.1007/s11357-023-01022-x.
Natarajan K, Acharya UR, Alias F, Tiboleng T, Puthusserypady SK. Nonlinear analysis of EEG signals at different mental states. Biomed Eng Online. 2004;3:7. https://doi.org/10.1186/1475-925x-3-7.
Zhang XD. Entropy for the complexity of physiological signal dynamics. Adv Exp Med Biol. 2017;1028:39–53. https://doi.org/10.1007/978-981-10-6041-0_3.
Rosso OA. Entropy changes in brain function. Int J Psychophysiol : official journal of the International Organization of Psychophysiology. 2007;64:75–80. https://doi.org/10.1016/j.ijpsycho.2006.07.010.
Frantzidis CA, Vivas AB, Tsolaki A, Klados MA, Tsolaki M, Bamidis PD. Functional disorganization of small-world brain networks in mild Alzheimer’s disease and amnestic mild cognitive impairment: an EEG study using relative wavelet entropy (RWE). Front Aging Neurosci. 2014;6:224. https://doi.org/10.3389/fnagi.2014.00224.
Keshmiri S. Entropy and the brain: an overview. Entropy (Basel). 2020;22. https://doi.org/10.3390/e22090917.
Pappalettera C, Miraglia F, Cotelli M, Rossini PM, Vecchio F. Analysis of complexity in the EEG activity of Parkinson’s disease patients by means of approximate entropy. Geroscience. 2022;44:1599–1607. https://doi.org/10.1007/s11357-022-00552-0.
Pappalettera C, Cacciotti A, Nucci L, Miraglia F, Rossini PM, Vecchio F. Approximate entropy analysis across electroencephalographic rhythmic frequency bands during physiological aging of human brain. Geroscience. 2023;45:1131–1145. https://doi.org/10.1007/s11357-022-00710-4.
Waninger S, Berka C, Stevanovic Karic M, Korszen S, Mozley PD, Henchcliffe C, Kang Y, Hesterman J, Mangoubi T, Verma A. Neurophysiological biomarkers of Parkinson’s disease. J Parkinsons Dis. 2020;10:471–80. https://doi.org/10.3233/jpd-191844.
Rockhill AP, Jackson N, George J, Aron A, Swann NC. UC San Diego resting state EEG data from patients with Parkinson's disease. OpenNeuro [Dataset]. 2021. https://doi.org/10.18112/openneuro.ds002778.v1.0.5.
Vecchio F, Nucci L, Pappalettera C, Miraglia F, Iacoviello D, Rossini PM. Time-frequency analysis of brain activity in response to directional and non-directional visual stimuli: an event related spectral perturbations (ERSP) study. J Neural Eng. 2022;19. https://doi.org/10.1088/1741-2552/ac9c96.
Miraglia F, Vecchio F, Bramanti P, Rossini PM. Small-worldness characteristics and its gender relation in specific hemispheric networks. Neuroscience. 2015;310:1–11. https://doi.org/10.1016/j.neuroscience.2015.09.028.
Alù F, Miraglia F, Orticoni A, Judica E, Cotelli M, Rossini PM, Vecchio F. Approximate entropy of brain network in the study of hemispheric differences. Entropy (Basel). 2020;22:1220. https://doi.org/10.3390/e22111220.
Miraglia F, Vecchio F, Rossini PM. Searching for signs of aging and dementia in EEG through network analysis. Behav Brain Res. 2017;317:292–300. https://doi.org/10.1016/j.bbr.2016.09.057.
Vecchio F, Miraglia F, Alú F, Orticoni A, Judica E, Cotelli M, Rossini PM. Contribution of graph theory applied to EEG data analysis for Alzheimer’s disease versus vascular dementia diagnosis. J Alzheimers Dis. 2021;82:871–879. https://doi.org/10.3233/jad-210394.
Vecchio F, Miraglia F, Judica E, Cotelli M, Alù F, Rossini PM. Human brain networks: a graph theoretical analysis of cortical connectivity normative database from EEG data in healthy elderly subjects. Geroscience. 2020;42:575–584. https://doi.org/10.1007/s11357-020-00176-2.
Abásolo D, Escudero J, Hornero R, Gómez C, Espino P. Approximate entropy and auto mutual information analysis of the electroencephalogram in Alzheimer’s disease patients. Med Biol Eng Comput. 2008;46:1019–28. https://doi.org/10.1007/s11517-008-0392-1.
Pincus S. Approximate entropy (ApEn) as a complexity measure. Chaos. 1995;5:110–17. https://doi.org/10.1063/1.166092.
Pincus SM, Viscarello RR. Approximate entropy: a regularity measure for fetal heart rate analysis. Obstet Gynecol. 1992;79:249–55.
Sun R, Wong WW, Wang J, Tong RK. Changes in electroencephalography complexity using a brain computer interface-motor observation training in chronic stroke patients: a fuzzy approximate entropy analysis. Front Hum Neurosci. 2017;11:444. https://doi.org/10.3389/fnhum.2017.00444.
Alù F, Orticoni A, Judica E, Cotelli M, Rossini PM, Miraglia F, Vecchio F. Entropy modulation of electroencephalographic signals in physiological aging. Mech Ageing Dev. 2021;196:111472. https://doi.org/10.1016/j.mad.2021.111472.
Vecchio F, Miraglia F, Pappalettera C, Orticoni A, Alù F, Judica E, Cotelli M, Rossini PM. Entropy as measure of brain networks’ complexity in eyes open and closed conditions. Symmetry. 2021;13:2178. https://doi.org/10.3390/sym13112178.
Lee GM, Fattinger S, Mouthon AL, Noirhomme Q, Huber R. Electroencephalogram approximate entropy influenced by both age and sleep. Front Neuroinform. 2013;7:33. https://doi.org/10.3389/fninf.2013.00033.
Abásolo D, Hornero R, Espino P, Poza J, Sánchez CI, de la Rosa R. Analysis of regularity in the EEG background activity of Alzheimer’s disease patients with approximate entropy. Clin Neurophysiol: official journal of the International Federation of Clinical Neurophysiology. 2005;116:1826–34. https://doi.org/10.1016/j.clinph.2005.04.001.
Burioka N, Miyata M, Cornélissen G, Halberg F, Takeshima T, Kaplan DT, Suyama H, Endo M, Maegaki Y, Nomura T, et al. Approximate entropy in the electroencephalogram during wake and sleep. Clin EEG Neurosci. 2005;36:21–4. https://doi.org/10.1177/155005940503600106.
Pincus SM. Approximate entropy as a measure of system complexity. Proc Natl Acad Sci USA. 1991;88:2297–301. https://doi.org/10.1073/pnas.88.6.2297.
Pincus SM. Assessing serial irregularity and its implications for health. Ann N Y Acad Sci. 2001;954:245–67. https://doi.org/10.1111/j.1749-6632.2001.tb02755.x.
Han CX, Wang J, Yi GS, Che YQ. Investigation of EEG abnormalities in the early stage of Parkinson’s disease. Cogn Neurodyn. 2013;7:351–9. https://doi.org/10.1007/s11571-013-9247-z.
Chen CC, Hsu YT, Chan HL, Chiou SM, Tu PH, Lee ST, Tsai CH, Lu CS, Brown P. Complexity of subthalamic 13–35 hz oscillatory activity directly correlates with clinical impairment in patients with Parkinson’s disease. Exp Neurol. 2010;224:234–40. https://doi.org/10.1016/j.expneurol.2010.03.015.
Yi GS, Wang J, Deng B, Wei XL. Complexity of resting-state EEG activity in the patients with early-stage Parkinson’s disease. Cogn Neurodyn. 2017;11:147–60. https://doi.org/10.1007/s11571-016-9415-z.
Darbin O, Adams E, Martino A, Naritoku L, Dees D, Naritoku D. Non-linear dynamics in parkinsonism. Front Neurol. 2013;4:211. https://doi.org/10.3389/fneur.2013.00211.
Stam KJ, Tavy DL, Jelles B, Achtereekte HA, Slaets JP, Keunen RW. Non-linear dynamical analysis of multichannel EEG: clinical applications in dementia and Parkinson’s disease. Brain Topogr. 1994;7:141–50. https://doi.org/10.1007/bf01186772.
Stam CJ, Jelles B, Achtereekte HA, Rombouts SA, Slaets JP, Keunen RW. Investigation of EEG non-linearity in dementia and Parkinson’s disease. Electroencephalogr Clin Neurophysiol. 1995;95:309–17. https://doi.org/10.1016/0013-4694(95)00147-q.
Akar SA, Kara B, Latifoğlu F. Bilgiç V. Analysis of the complexity measures in the EEG of schizophrenia patients. Int J Neural Syst. 2016;26:1650008. https://doi.org/10.1142/s0129065716500088.
Chenxi L, Chen Y, Li Y, Wang J, Liu T. Complexity analysis of brain activity in attention-deficit/hyperactivity disorder: a multiscale entropy analysis. Brain Res Bull. 2016;124:12–20. https://doi.org/10.1016/j.brainresbull.2016.03.007.
Gao J, Hu J, Tung WW. Complexity measures of brain wave dynamics. Cogn Neurodyn. 2011;5:171–82. https://doi.org/10.1007/s11571-011-9151-3.
Marsden JF, Limousin-Dowsey P, Ashby P, Pollak P, Brown B. Subthalamic nucleus, sensorimotor cortex and muscle interrelationships in Parkinson’s disease. Brain. 2001;124:378–88. https://doi.org/10.1093/brain/124.2.378.
Rowland NC, De Hemptinne C, Swann NC, Qasim S, Miocinovic S, Ostrem JL, Knight RT, Starr PA. Task-related activity in sensorimotor cortex in Parkinson’s disease and essential tremor: changes in beta and gamma bands. Front Hum Neurosci. 2015;9:512. https://doi.org/10.3389/fnhum.2015.00512.
Marceglia S, Fiorio M, Foffani G, Mrakic-Sposta S, Tiriticco M, Locatelli M, Caputo E, Tinazzi M, Priori A. Modulation of beta oscillations in the subthalamic area during action observation in Parkinson’s disease. Neuroscience. 2009;161:1027–36. https://doi.org/10.1016/j.neuroscience.2009.04.018.
Priori A, Foffani G, Pesenti A, Tamma F, Bianchi AM, Pellegrini M, Locatelli M, Moxon KA, Villani RM. Rhythm-specific pharmacological modulation of subthalamic activity in Parkinson’s disease. Exp Neurol. 2004;189:369–79. https://doi.org/10.1016/j.expneurol.2004.06.001.
Fogelson N, Williams D, Tijssen M, van Bruggen G, Speelman H, Brown P. Different functional loops between cerebral cortex and the subthalmic area in Parkinson’s disease. Cereb Cortex. 2006;16:64–75. https://doi.org/10.1093/cercor/bhi084.
Sharman M, Valabregue R, Perlbarg V, Marrakchi-Kacem L, Vidailhet M, Benali H, Brice A, Lehéricy S. Parkinson’s disease patients show reduced cortical-subcortical sensorimotor connectivity. Mov Disord. 2013;28:447–54. https://doi.org/10.1002/mds.25255.
Canu E, Agosta F, Sarasso E, Volontè MA, Basaia S, Stojkovic T, Stefanova E, Comi, Falini. Kostic, et al. Brain structural and functional connectivity in Parkinson’s disease with freezing of gait. Hum Brain Mapp. 2015;36:5064–78. https://doi.org/10.1002/hbm.22994.
Guimarães RP, Arci Santos MC, Dagher A, Campos LS, Azevedo P, Piovesana LG, De Campos BM, Larcher K, Zeighami Y, Scarparo Amato-Filho AC, et al. Pattern of reduced functional connectivity and structural abnormalities in Parkinson’s disease: an exploratory study. Front Neurol. 2016;7:243. https://doi.org/10.3389/fneur.2016.00243.
Rosin B, Nevet A, Elias S, Rivlin-Etzion M, Israel Z, Bergman H. Physiology and pathophysiology of the basal ganglia-thalamo-cortical networks. Parkinsonism Relat Disord. 2007;13 Suppl 3:S437–9. https://doi.org/10.1016/s1353-8020(08)70045-2.
Levy R, Ashby P, Hutchison WD, Lang AE, Lozano AM, Dostrovsky JO. Dependence of subthalamic nucleus oscillations on movement and dopamine in Parkinson’s disease. Brain. 2002;125:1196–209. https://doi.org/10.1093/brain/awf128.
Acknowledgements
This work was partially supported by the Italian Ministry of Health for Institutional Research (Ricerca corrente).
Author information
Authors and Affiliations
Contributions
Lorenzo Nucci: methodology, data curation, writing—review and editing. Francesca Miraglia: conceptualization, methodology, writing—original draft. Chiara Pappalettera: methodology, data curation, writing—review and editing. Paolo Maria Rossini: supervision, writing—review and editing. Fabrizio Vecchio: supervision, writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Nucci, L., Miraglia, F., Pappalettera, C. et al. Exploring the complexity of EEG patterns in Parkinson’s disease. GeroScience (2024). https://doi.org/10.1007/s11357-024-01277-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-024-01277-y