Abstract
Increasing evidence suggests an association between fine particulate matter (PM2.5) exposure and type 2 diabetes mellitus. However, there is still a lack of comparative evaluation regarding diabetes burden due to ambient and indoor PM2.5 pollution at a global scale. This study attempts to provide a systematic and comprehensive profile for PM2.5-attributable burden of diabetes and its spatiotemporal trends, globally and regionally. Comparative estimates of diabetes attributable to ambient PM2.5 and household air pollution (HAP) from solid fuels for 204 countries and territories were derived from the Global Burden of Disease Study 2019. Globally, 292.5 (95% uncertainty interval: 207.1, 373.4) thousand deaths and 13.0 (9.1, 17.2) million disability-adjusted life years (DALYs) from diabetes were attributed to PM2.5 pollution in 2019, wherein more than two-thirds (67.3% deaths and 69.7% DALYs) were contributed by ambient PM2.5. Compared to 1990, age-standardized DALY rate (ASDR) in 2019 attributable to ambient PM2.5 increased by 85.9% (APC: 2.21% [2.15, 2.27]), while HAP-associated ASDR decreased by 37.9% (APC: − 1.66% [− 1.82, − 1.50]). We observed a negative correlation between SDI and APC in ASMR (rs = − 0.5, p < 0.001) and ASDR (rs = -0.4, p < 0.001) among 204 countries and territories. HAP-related diabetes experienced a sharp decline during 1990–2019, while global burden of diabetes attributable to ambient PM2.5 was rising rapidly. The elderly and people in low-SDI countries suffered from the greatest burden of diabetes due to PM2.5 pollution. More targeted interventions should be taken by governments to reduce PM2.5 exposure and related diabetes burden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes is a chronic metabolic disease that poses a serious threat to global health. Type 2 diabetes is the most common type of diabetes, which occurs when the body is resistant to insulin or does not produce enough insulin (Paul et al. 2020). Diabetes and associated complications, such as heart disease, chronic kidney disease, retinopathy, and neuropathy, will reduce the quality of life, life expectancy and rise healthcare costs (Faselis et al. 2020; Lin et al. 2020). The Global Burden of Diseases Study 2019 (GDB 2019) estimated that diabetes ranked as the eighth leading cause of disability-adjusted life years (DALYs) in 2019 (Vos et al. 2020). According to the evaluation of the International Diabetes Federation, global direct health expenditure on diabetes in 2019 reached 760 billion dollars and is expected to grow (Williams et al. 2020). The incidence of diabetes has increased significantly and will continue to surge in the future. In 2021, it was reported that there were 537 million people with diabetes, and the number is estimated to go up to 643 million by 2030, more than three-quarters of whom live in low- and middle-income countries (Sun et al. 2022). Governments and international organizations are urged to figure out more causes and make targeted interventions to reduce diabetes.
Diabetes is generally related to behavioral (e.g., alcohol use and smoking), environmental and occupational (e.g., ambient particulate matter and occupational injury), and metabolic (e.g., high systolic blood pressure and high body-mass index) risk factors. Behavioural risk factors for diabetes have been well examined (Glechner et al. 2018). As the process of industrialization and urbanization was accelerated, environmental risk factors for diabetes recently popped into public view (Yang et al. 2020b). Air pollution, especially fine particulate matter (PM2.5), is an important environmental risk factor, resulting in many health problems and even death because of its adverse effect caused by toxic compounds (Kermani et al. 2021; Liu et al. 2022). A large body of studies indicated that long-term exposure to PM2.5 is related to chronic diseases, including hypertension, cognitive aging, and cardiovascular (Leili et al. 2021; Li et al. 2022; Yao et al. 2022). Growing epidemiological studies indicated that exposure to PM2.5 is linked to elevated mortalities (Farzad et al. 2020; Hajizadeh et al. 2021; Zhang 2021). These increased risks of diabetes caused by PM2.5 may be related to systemic inflammation and oxidative stress, which may ultimately lead to the development of insulin resistance and beta-cell dysfunction (Buxton et al. 2019; Gangwar et al. 2020).
The associations between air pollutants and the incidence of diabetes have been universally established. Systematic reviews and meta-analysis have established the association between short- and long-term exposure to ambient particulate air pollution and the risk of diabetes (Liu et al. 2019a; Yang et al. 2020a), and a limited number of studies have evaluated an association between indoor air pollution and diabetes (Juntarawijit and Juntarawijit 2020; Mishra et al. 2020). Existing epidemiological evidence conducted in several countries, consisting of Italy, Mexico, and China, reinforced this link (Cheng et al. 2022; Chilian-Herrera et al. 2021; Meroni et al. 2021). However, these individual disease evaluations for PM2.5-related diabetes may show great heterogeneities in exposure assessments and analytic strategies, thus resulting in substantial uncertainty when comparing estimates across study sites and periods (Suryadhi et al. 2020; Zhang et al. 2021). It is still warranted to utilize a uniform and standardized analytic strategy to provide a systematic and comprehensive profile for PM2.5-attributable burden of diabetes on the disease and its spatiotemporal trends, globally and regionally.
Therefore, in this study, we attempt to systematically and comprehensively estimate the global burden of diabetes caused by ambient and indoor PM2.5 from 1990 to 2019 by different ages, sex, regions, and SDI, which may help governments and international organizations make targeted interventions to reduce PM2.5-attributable diabetes burden.
Materials and methods
Study data
We derived the up-to-date estimates of diabetes burden due to particulate matter pollution on the GBD website (http://ghdx.healthdata.org/gbd-results-tool, assessed on February 17, 2022). The GBD 2019 conducted a systematic and comparative assessment of the global burden for 369 diseases and injuries and 87 risk factors in 204 countries and territories from 1990 to 2019. Here, this current study only focused on the trends of diabetes burden attributable to ambient PM2.5 and household air pollution (HAP). The GBD 2019 estimation methods for attributable burden of disease have been detailed elsewhere (Murray et al. 2020b; Vos et al. 2020). Briefly, GBD 2019 evaluated exposure comprised of ambient PM2.5 and HAP: (1) Ambient PM2.5 exposure was based on satellite data which was estimated at 0.1° × 0.1° (11 km × 11 km at the equator) resolution (Cohen et al. 2017) and (2) assessment of HAP exposure was calculated by the proportion of individuals who use a specific solid-fuel type (wood, coal, charcoal, agricultural residues, or dung) through the spatio-temporal Gaussian Process Regression (Bennitt et al. 2021). Type 2 diabetes mellitus is defined based on the International Statistical Classification of Diseases and estimated by using vital registration data, verbal autopsy, censuses, disease registries, and other sources (Vos et al. 2020).
Measures for diabetes burden
Burden of diabetes attributable to PM2.5 was assessed using metrics including numbers and population attributable fractions (PAF) of deaths and DALYs, socio-demographic Index (SDI), age-standardized mortality rate (ASMR), and age-standardized DALY rate (ASDR).
PAF defines the proportional reduction in population disease or mortality that would occur if exposure to a risk factor was reduced to an alternative ideal exposure scenario (Vos et al. 2020). DALYs were calculated as the sum of years of life lost (YLLs) due to premature death and years lived with disability (YLDs), based on a reference maximum observed life expectancy and standardized disability weights for each health state (Murray et al. 2020b; Vos et al. 2020). Disability weights adopted for YLL calculation were derived from general population-based surveys (Salomon et al. 2015). SDI comprehensively evaluates the development level and is strongly correlated with health outcomes. In summary, SDI ranges from 0 to 1 and encompasses three different aspects which combine information on a gross domestic product, average schooling years among individuals over 15 years old, and the total fertility rate among females under 25 years old (Murray et al. 2020a).
To eliminate the influence of heterogeneity caused by differences in population age structures, GBD 2019 calculated the percentage change based on the point estimates of the age-standardized rates (ASR, per 100,000 population). Estimates in this paper are presented in absolute numbers and ASR with 95% uncertainty intervals (95% UIs), which were defined as the ordinal 25th and 975th draws for each measure in the 1000 estimations (Lozano et al. 2020). All rates were age-standardized via the direct method applying the GBD global-age structure.
Stratified analyses
Diabetes burden due to ambient PM2.5 and HAP were performed by sex, age, 21 GBD regions, and 204 countries and territories during 1990–2019. Age groups were divided into 16 categories (all-ages, 5-year age intervals between 25 and 94 years, and ≥ 95 years). We described the ASMR and ASDR trends of diabetes attributable to ambient PM2.5 and HAP, respectively. In addition, all the countries and regions were grouped into 21 GBD regions according to a geographic hierarchy. According to SDI, 204 countries and territories were categorized into five regions: low SDI (< 0.46), low-middle SDI (0.46–0.60), middle SDI (0.61–0.69), high-middle SDI (0.70–0.81), and high SDI (> 0.81) (Roth et al. 2018).
Statistical analysis
Percentage change and annual percentage change (APC) were estimated to depict the spatiotemporal trends of the ASMR and ASDR (Liu et al. 2019b). The trend of ASR can be measured over a time interval by APC; it can be obtained from a log-linear model:
where X was the calendar year, β1 represents the annual change, and ε refers to the error term. ASR in log transformation is assumed to be normally distributed; APC was calculated as (exp(β1) − 1) × 100 (Hankey et al. 2000). If the lower boundary of the APC’s 95% UIs were > 0, the ASR was considered to increase. Conversely, if the upper boundary of the APC’s 95% UIs were < 0, the ASR was thought to decrease. Otherwise, it was considered to be steady. Finally, we used the Spearman correlation coefficient to examine the correlation between SDI and ASR, and APC.
All analyses were performed using the R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria). A 2-sided p-value less than 0.05 is considered to be statistically significant.
Results
Overall diabetes burden attributable to PM2.5 from 1990 to 2019
Globally, deaths and DALYs of diabetes attributed to ambient PM2.5 and HAP saw a continuous increase from 1990 to 2019 (Tables S1 and S2). In 2019, 292.5 (95% UI: 207.1, 373.4) thousand diabetes deaths were attributed to PM2.5 exposure, representing a 124% increase compared with 130.6 (91.4, 182.0) thousand in 1990. PM2.5-attributable DALYs rose substantially from 5.5 (3.7, 7.8) million in 1990 to 13.0 (9.1, 17.2) million in 2019. However, ASMR changed slightly from 3.6 (2.5, 4.9) in 1990 to 3.7 (2.6, 4.7) per 100,000 in 2019, and ASDR scaled up from 134.2 (92.0, 188.9) in 1990 to 156.1 (109.6, 207.3) per 100,000 in 2019.
The absolute numbers of diabetes deaths and DALYs due to ambient PM2.5 and HAP were higher in females, while males had larger ASMR and ASDR in 1990 and 2019. Deaths and DALYs were highly variable across regions, where estimates of ASDR were lowest in Australasia (18.5 [4.1, 39.1] per 100,000) and highest in Oceania (764.1 [499.7, 1073.8] per 100,000) in 2019.
Global diabetes burdens attributable to ambient PM2.5 and HAP
Figure 1 shows APC in ASDR of diabetes attributable to ambient PM2.5 and HAP by country between 1990 and 2019. Over 30 years, the numbers of diabetes deaths attributable to ambient PM2.5 surged 2.5-fold (55.8 thousand in 1990 versus 196.8 thousand in 2019), and DALYs followed a faster pattern of growth (2.3 versus 9.0 million). In terms of HAP-related diabetes, both deaths and DALYs exhibited an upward trend from 1990–2019. Deaths reach 95.7 thousand in 2019, rising 28.0% from 74.8 thousand in 1990, while DALYs soared by 25.4% from 3.1 to 3.9 million during the same period.
Annual percentage changes in age-standardized DALY rate of diabetes attributable to ambient PM2.5 and HAP by country between 1990 and 2019. A APC in ASDR of diabetes attributable to ambient PM2.5. B APC in ASDR of diabetes attributable to HAP. DALY disability-adjusted life years, ASMR age-standardized mortality rate, ASDR age-standardized DALY rate
Figure 2 reveals the ASDR distribution of diabetes due to ambient PM2.5 and HAP in 2019. ASMR due to ambient PM2.5 increased by 57.3% from 1.6 to 2.5 per 100,000, with an APC of 1.5% (1.4, 1.6); ASDR increased by 86.7% from 58.4 in 1990 to 109.0 per 100,000 in 2019, with an APC of 2.21% (2.15, 2.27). By contrast, HAP-related ASMR dropped dramatically by 39.9% from 2.0 in 1990 to 1.2 per 100,000 in 2019, with an APC of − 1.69% (− 1.89, − 1.49); ASDR scaled down from 75.9 in 1990 to 47.1 per 100,000 in 2019 on a slump by 37.9%, with an APC of − 1.66% (− 1.82, − 1.50). In 2019, ASMR and ASDR ascribed to ambient PM2.5 were 2.1- and 2.3-fold higher than those ascribed to HAP, respectively; (Figs. S1 and S2).
Age-standardized DALY rate of diabetes attributable to ambient PM2.5 and HAP by country in 2019. A Age-standardized DALY rate of diabetes attributable to ambient PM2.5. B Age-standardized DALY rate of diabetes attributable to HAP. DALY disability-adjusted life years, ASMR age-standardized mortality rate, ASDR age-standardized DALY rate
Diabetes burden attributable to ambient PM2.5 and HAP by sex and age
Figure 3 presents a different sex-specific tendency of diabetes attributable to ambient PM2.5 and HAP over the past three decades. Males suffered from greater ASMR and ASDR attributed to ambient PM2.5 over 30 years, with 2.8 and 122.2 per 100,000 in 2019, respectively. Males had larger HAP-related ASMR and ASDR in 1990 (2.1 versus 1.9, 77.0 versus 75.3 per 100,000), while females were at a slightly larger burden in 2019, with 1.2 and 48.6 per 100,000 ASMR and ASDR (versus 1.2 and 45.6 per 100,000 in males).
Sex-specific global burden of diabetes attributable to ambient PM2.5 and HAP from 1990 to 2019. A Age-standardized mortality rate of diabetes attributable to ambient PM2.5. B Age-standardized DALY rate of diabetes attributable to ambient PM2.5. C Age-standardized mortality rate of diabetes attributable to HAP. D Age-standardized DALY rate of diabetes attributable to HAP. ASMR age-standardized mortality rate, ASDR age-standardized DALY rate
Figure 4 illustrates PAF of DALYs for diabetes caused by ambient PM2.5 and HAP in age groups from 1990 to 2019. Generally, in all age groups, ambient PM2.5-related PAF of DALYs saw a considerable increase during the 30 years from 9.2% to 13.6%, while PAF of DALYs caused by HAP was off 52.0% from 12.3% to 5.9%. In 2019, people aged 25–49 years accounted for the largest PAF of DALYs related to ambient PM2.5 and HAP at respectively 14.1% and 6.9%, suggesting that PM2.5 pollution played as one of the leading risk factors of diabetes in young adults.
Population attributable fractions of DALYs for diabetes caused by ambient PM2.5 and HAP in age groups from 1990 to 2019. A PAF of diabetes attributable to ambient PM2.5. B PAF on diabetes attributable to HAP. DALY disability-adjusted life years, ASMR age-standardized mortality rate, ASDR age-standardized DALY rate
Diabetes burden attributable to ambient PM2.5 and HAP by countries and regions
Figure 5 exhibits the burden of diabetes attributable to ambient PM2.5 and HAP between GBD regions in 1990 and 2019. As can be seen, ASMR and ASDR varied spatially in 2019. Southern Sub-Saharan Africa had the largest ASDR caused by ambient PM2.5 at 280.4 per 100,000, with an APC of 3.3% (2.9, 3.6) during 1990–2019, followed by Central Latin America (246.5 per 100,000), and North Africa and Middle East (220.6 per 100,000). By contrast, in 2019, the lowest ASDR attributable to ambient PM2.5 occurred in Australasia (18.3 per 100,000), with an APC of − 0.8% (− 1.0, − 0.5), followed by Eastern Europe (40.0 per 100,000) and Eastern Sub-Saharan Africa (40.2 per 100,000). ASMR attributed to ambient PM2.5 had a similar pattern (Fig. S3).
Age-standardized DALY rate of diabetes attributable to ambient PM2.5 and HAP in GBD regions in 1990 and 2019. A ASDR of diabetes attributable to paticulate matter in 1990. B ASDR of diabetes attributable to particulate matter in 2019. DALY disability-adjusted life years, ASMR age-standardized mortality rate, ASDR age-standardized DALY rate
In 2019, Bahrain was the top-ranked country in ambient PM2.5-related ASMR and ASDR, with estimates of 30.3 and 770.2 per 100,000, followed by Qatar (29.7 and 722.1 per 100,000), while ASMR and ASDR in Iceland were the lowest at 0.1 and 11.0 per 100,000. In parallel, the largest HAP-related ASDR were in Kiribati (1000.7 per 100,000) (Fig. 3), while United Arab Emirates occupied the lowest ASDR at 0.02 per 100,000.
Diabetes burden attributable to ambient PM2.5 and HAP by SDI
Figure 6 indicates ASDR of diabetes attributable to ambient PM2.5 and HAP, grouped by SDI quintiles from 1990 to 2019. Diabetes burden varied substantially from low SDI to high SDI, showing a gentle downward trend. In 2019, the largest ASMR and ASDR (3.8 and 150.1 per 100,000) due to ambient PM2.5 were observed in the middle SDI countries, while the lowest burden was estimated in countries with high SDI, at 0.9 and 58.6 per 100,000. From 1990 to 2019, ASMR and ASDR attributable to ambient PM2.5 in all countries increased slightly or remained still except for high SDI countries. HAP-related ASMR and ASDR showed a significant negative association with SDI from 1990 to 2019, suggesting high SDI countries shared the lowest ASMR and ASDR (0.01 and 0.4 per 100,000), while low SDI countries were experiencing the greatest diabetes burden from HAP (6.0 and 195.2 per 100,000).
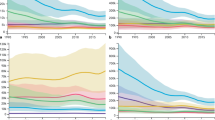
We observed a significant negative correlation between SDI and APC of ASR (ASMR [rs = -0.5, p < 0.001], ASDR [rs = -0.4, p < 0.001]) among 204 countries, suggesting high-SDI countries were associated with lower APC estimates in ASMR and ASDR (Fig. S4). Figure 7 describes the correlation between SDI and ASDR of diabetes attributable to ambient PM2.5 and HAP by region from 1990 to 2019. A nonlinear association was observed between SDI and ASR. Globally, ambient PM2.5-related ASMR and ASDR climbed slightly and then dipped sharply, showing an inverted U-shaped relation with a peak at middle SDI; while HAP-related ASMR and ASDR started at a gentle hill and then scaled down, presenting a near negative association between ASR and SDI (Figs. 7 and S5).
The correlation between SDI and age-standardized DALY rate of diabetes attributable to ambient PM2.5 and HAP by region from 1990 to 2019. A The correlation between SDI and ASDR attributable to ambient PM2.5. B The correlation between SDI and ASDR attributable to HAP. ASDR age-standardized DALY rate, DALY disability-adjusted life years, SDI social-demographic index. The solid blue line shows expected values across the spectrum of the socio-demographic index
Discussion
Based on GBD 2019, this study described the temporal and spatial distribution of diabetes burden due to ambient PM2.5 and HAP in 204 countries and territories, indicating a great discrepancy across regions from 1990 to 2019. The absolute number of deaths and DALYs caused by ambient PM2.5 and HAP were at a rapidly upward trend over the past three decades, while ASMR and ASDR attributed to ambient PM2.5 and HAP showed an opposite pattern. ASMR and ASDR attributed to ambient PM2.5 soared considerably from 1990 to 2019, and were more pronounced in males, the elderly, and middle SDI countries, while HAP-related ASMR and ASDR experienced a sharp decline at the same period. A negative association was found between SDI and APC of ASR from 1990 to 2019, and nonlinear correlations were observed between SDI and ASR.
This study found that, globally, a continuous climb and a dramatic drop remained in the diabetes burden attributed to ambient PM2.5 and HAP, respectively. As prior epidemiological studies presented, people were more prone to suffer from diabetes when exposed to high concentrations of ambient PM2.5 (Wu et al. 2021). It is natural that substantial attributable burdens were caused by ambient PM2.5 with rapid acceleration of urbanization and fast growth in fossil fuel combustion (Shi et al. 2021). The increment in consumption of fossil fuels involved a role in the growth ambient PM2.5-related burden. HAP from solid fuels is one of the primary environmental health risks (Rosário Filho et al. 2021). Our study illustrated that low SDI countries was responsible for a large diabetes burden (e.g., ASMR and ASDR in 2019: 6.0 and 195.2 per 100,000). However, HAP-related ASMD and ASDR experienced a sharp decline by 39.9% and 37.9% during 1990–2019, respectively, which may be driven by energy transition toward clean fuels gradually (Snider et al. 2018).
Stratified analysis by sex illustrated that burden of diabetes attributable to ambient PM2.5 was considerably greater in males, which may be related to individual activity patterns or occupations (Shin et al. 2021). Males had more access to exposure in ambient PM2.5 and higher smoking rates (Peng et al. 2020), resulting in more diabetes risk caused by ambient PM2.5. We found females were at slightly larger HAP-related ASMR and ASDR in 2019. People spent roughly 90% of their lifetime indoors (Klepeis et al. 2001), and had great chances of being exposed to HAP. Given more time spent cleaning, cooking, and caring for children, women were usually at a high exposure to indoor residential emissions (James et al. 2020), thus suffering from a higher HAP-related burden (Mishra et al. 2020).
PAF of deaths and DALYs attributed to ambient PM2.5 or HAP varied greatly by age groups (e.g., DALYs in 2019: 14.3% in 30–34 yrs, 4.7% in 80 + years). Our analysis showed that in 2019, there are around one-seventh DALYs on diabetes attributed to ambient PM2.5 in 25–49 group, suggesting a great proportion of diabetes burden would diminish if concentration of PM2.5 were reduced (Murray et al. 2020b). The absolute numbers of deaths and DALYs were much higher in the elderly because of the high prevalence (Sun et al. 2022), while a greater PAF attributed to PM2.5 was observed in the young group than the elderly. The reason for relative low PAF of PM2.5 in older persons correlated to that they are more susceptible to cardiovascular diseases, which was closely interlinked with diabetes (Petrie et al. 2018). Therefore, PM2.5 accounted for a relatively less proportion in the old group with diabetes (Chen et al. 2016). Nevertheless, considering the biological degradation and ageing (e.g., a higher decline of immunologic and lung function) (Liu et al. 2018), the elderly are of high vulnerability to air pollution and should thus avoid PM2.5-related health loss by taking more protective measures (Qiu et al. 2018).
We found that, in 2019, ASMR and ASDR of diabetes attributable to ambient PM2.5 was highest in middle SDI countries (3.8 and 150.1 per 100,000), particularly in the Southern Sub-Saharan Africa, where residents were exposed to heavy ambient PM2.5 pollution (Shaddick et al. 2018). It may be caused by the fact that undeveloped countries are experiencing worse ambient air quality and have greater risks of PM2.5-related diseases (Hystad et al. 2020). Meanwhile, due to more solid fuels consumed (Rajkumar et al. 2018), and less ventilation used (Yu et al. 2020), low SDI countries contributed the largest HAP-related diabetes burden (with ASMR and ASDR of 6.0 and 195.2 per 100,000 in 2019) (McCarron et al. 2020). Stricter ambient air quality criteria promulgated by policymakers and energy transformation to cleaner fuels were needed in undeveloped and developing countries to reduce PM2.5-related health loss (Huang et al. 2018). The association between SDI and ASR presents an inverted U-shaped relation with a peak in middle SDI countries, suggesting that in low- and middle-SDI countries, rapid economic growth contributed to a significant amount of PM2.5 pollution (Shan et al. 2020). HAP-related ASR shows a nearly linear association with SDI, indicating that high-SDI countries, benefiting from cessation of solid fuel use or replacing them with cleaner fuels, had lower ASRs (Shaddick et al. 2018).
The major advantage of this study was that we systematically and comprehensively estimated the global burden of diabetes caused by ambient PM2.5 and HAP from 1990 to 2019 by different ages, sex, regions, and SDI. This should significantly help to provide a comparable reference for policymakers to take targeted measures to diminish air pollution and related diabetes. Meanwhile, we acknowledged this analysis has a few limitations. First, we may underestimate burden of diabetes due to air pollution with regard to utilizing GBD data, which were highly relied on existing but insufficient epidemiological studies (Cohen et al. 2017; Murray et al. 2020b). Second, assessments for undeveloped countries with high levels of air pollution may be inaccurate, because sparse evidence based on prospective cohort studies was available in low SDI countries to date (Yin et al. 2020). Third, estimates of ambient PM2.5 exposure was still of great uncertainty at a global scale, and estimates of HAP from other sources was absent (such as estimates on heating and indoor second-hand smoke) (Deng et al. 2020), which may result in high possibility of exposure misclassification (Turner et al. 2014; Yang et al. 2018). Fourth, we only estimated the diabetes burden attributable to ambient PM2.5 and HAP additivity; however, burden may multiply or more complex interact regarding joint effects (Yin et al. 2020). Furthermore, high-quality epidemiological research in undeveloped countries with high ambient PM2.5 and HAP levels is still warranted.
Conclusions
In conclusion, this study illustrated that HAP-related diabetes experienced a sharp decline during 1990–2019, while global burden of diabetes attributable to ambient PM2.5 was rising rapidly. The elderly and people in low-SDI countries suffered from the greatest burden of diabetes due to PM2.5 pollution. Our study suggested that active interventions should be taken to get a further decline in PM2.5 exposure and related diabetes burden.
Data availability
The datasets generated and/or analyzed during the current study are available in the (GBD) repository (http://ghdx.healthdata.org/gbd-results-tool).
References
Bennitt FB, Wozniak SS, Causey K, Burkart K, Brauer M (2021) Estimating disease burden attributable to household air pollution: new methods within the Global Burden of Disease Study. Lancet Glob Health 9:S18
Buxton MA, Meraz-Cruz N, Sanchez BN, Gronlund CJ, Foxman B, Vadillo-Ortega F et al (2019) Air pollution and inflammation: findings from concurrent repeated measures of systemic and reproductive tract cytokines during term pregnancy in Mexico City. Sci Total Environ 681:235–241
Chen L, Zhou Y, Li S, Williams G, Kan H, Marks GB et al (2016) Air pollution and fasting blood glucose: a longitudinal study in China. Sci Total Environ 541:750–755
Cheng X, Ji X, Yang D, Zhang C, Chen L, Liu C et al (2022) Associations of PM2.5 exposure with blood glucose impairment in early pregnancy and gestational diabetes mellitus. Ecotoxicol Environ Saf 232:113278
Chilian-Herrera OL, Tamayo-Ortiz M, Texcalac-Sangrador JL, Rothenberg SJ, López-Ridaura R, Romero-Martínez M et al (2021) PM2.5 exposure as a risk factor for type 2 diabetes mellitus in the Mexico City metropolitan area. BMC Public Health 21:2087
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K et al (2017) Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389:1907–1918
Deng M, Li P, Ma R, Shan M, Yang X (2020) Air pollutant emission factors of solid fuel stoves and estimated emission amounts in rural Beijing. Environ Int 138:105608
Farzad F, Akram G, Abbas S, Ahmad Jonidi J, Ali A, Majid K et al (2020) Quantification of mortality and morbidity in general population of heavily-industrialized city of Abadan: Effect of long-term exposure. J Air Pollut Health 5:171–180
Faselis C, Katsimardou A, Imprialos K, Deligkaris P, Kallistratos M, Dimitriadis K (2020) Microvascular Complications of Type 2 Diabetes Mellitus. Curr Vasc Pharmacol 18:117–124
Gangwar RS, Bevan GH, Palanivel R, Das L, Rajagopalan S (2020) Oxidative stress pathways of air pollution mediated toxicity: Recent insights. Redox Biol 34:101545
Glechner A, Keuchel L, Affengruber L, Titscher V, Sommer I, Matyas N et al (2018) Effects of lifestyle changes on adults with prediabetes: a systematic review and meta-analysis. Prim Care Diab 12:393–408
Hajizadeh Y, Jafari N, Fanaei F, Ghanbari R, Mohammadi A, Behnami A et al (2021) Spatial patterns and temporal variations of traffic-related air pollutants and estimating its health effects in Isfahan city, Iran. J Environ Health Sci Eng 19:781–791
Hankey BF, Ries LA, Kosary CL, Feuer EJ, Merrill RM, Clegg LX et al (2000) Partitioning linear trends in age-adjusted rates. Cancer Causes Control 11:31–35
Huang J, Pan X, Guo X, Li G (2018) Health impact of China’s Air Pollution Prevention and Control Action Plan: an analysis of national air quality monitoring and mortality data. Lancet Planet Health 2:e313–e323
Hystad P, Larkin A, Rangarajan S, AlHabib KF, Avezum Á, Calik KBT et al (2020) Associations of outdoor fine particulate air pollution and cardiovascular disease in 157 436 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet Planet Health 4:e235–e245
James BS, Shetty RS, Kamath A, Shetty A (2020) Household cooking fuel use and its health effects among rural women in southern India-A cross-sectional study. PLoS One 15:e0231757
Juntarawijit C, Juntarawijit Y (2020) Cooking with biomass fuel and cardiovascular disease: a cross-sectional study among rural villagers in Phitsanulok Thailand. F1000Res 9:307
Kermani M, Jonidi Jafari A, Gholami M, Taghizadeh F, Masroor K, Abdolahnejad A et al (2021) Characterisation of PM2.5 – bound PAHs in outdoor air of Karaj megacity: the effect of meteorological factors. Int J Environ Anal Chem 2021:1–19
Klepeis NE, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P et al (2001) The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Eposure Sci Environ Epidemiol 11:231–252
Leili M, Nadali A, Karami M, Bahrami A, Afkhami A (2021) Short-term effect of multi-pollutant air quality indexes and PM2.5 on cardiovascular hospitalization in Hamadan, Iran: a time-series analysis. Environ Sci Pollut Res 28:53653–53667
Li J, Dong Y, Song Y, Dong B, van Donkelaar A, Martin RV et al (2022) Long-term effects of PM2.5 components on blood pressure and hypertension in Chinese children and adolescents. Environ Int 161:107134
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X et al (2020) Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep 10:14790–14790
Liu J, Hou B, Ma X-W, Liao H (2018) Solid fuel use for cooking and its health effects on the elderly in rural China. Environ Sci Pollut Res 25:3669–3680
Liu F, Chen G, Huo W, Wang C, Liu S, Li N et al (2019a) Associations between long-term exposure to ambient air pollution and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Environ Pollut 252:1235–1245
Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C et al (2019b) The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol 70:674–683
Liu L, Luo S, Zhang Y, Yang Z, Zhou P, Mo S et al (2022) Longitudinal impacts of PM2.5 constituents on adult mortality in China. Environ Sci Technol. https://doi.org/10.1021/acs.est.1c04152
Lozano R, Fullman N, Mumford JE, Knight M, Barthelemy CM, Abbafati C et al (2020) Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1250–1284
McCarron A, Uny I, Caes L, Lucas SE, Semple S, Ardrey J et al (2020) Solid fuel users’ perceptions of household solid fuel use in low- and middle-income countries: a scoping review. Environ Int 143:105991
Meroni G, Valerio A, Vezzoli M, Croci E, Carruba MO (2021) The relationship between air pollution and diabetes: A study on the municipalities of the Metropolitan City of Milan. Diab Res Clin Pract 174:108748
Mishra S, McClure L, Golla V, Guddattu V, Lungu C, Sathiakumar N (2020) Relationship between diabetes mellitus and indoor air pollution: an exploratory analysis. Int J Noncommun Dis 5:165–170
Murray CJL, Abbafati C, Abbas KM, Abbasi M, Abbasi-Kangevari M, Abd-Allah F et al (2020a) Five insights from the Global Burden of Disease Study 2019. Lancet 396:1135–1159
Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M et al (2020b) Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1223–1249
Paul LA, Burnett RT, Kwong JC, Hystad P, van Donkelaar A, Bai L et al (2020) The impact of air pollution on the incidence of diabetes and survival among prevalent diabetes cases. Environ Int 134:105333
Peng L, Xiao S, Gao W, Zhou Y, Zhou J, Yang D et al (2020) Short-term associations between size-fractionated particulate air pollution and COPD mortality in Shanghai, China. Environ Pollut 257:113483
Petrie JR, Guzik TJ, Touyz RM (2018) Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol 34:575–584
Qiu H, Schooling CM, Sun S, Tsang H, Yang Y, Lee RS-y et al (2018) Long-term exposure to fine particulate matter air pollution and type 2 diabetes mellitus in elderly: a cohort study in Hong Kong. Environ Int 113:350–356
Rajkumar S, Clark ML, Young BN, Benka-Coker ML, Bachand AM, Brook RD et al (2018) Exposure to household air pollution from biomass-burning cookstoves and HbA1c and diabetic status among Honduran women. Indoor Air 28:768–776
Rosário Filho NA, Urrutia-Pereira M, D’Amato G, Cecchi L, Ansotegui IJ, Galán C et al (2021) Air pollution and indoor settings. World Allergy Org J 14:100499
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N et al (2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1736–1788
Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH et al (2015) Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health 3:e712–e723
Shaddick G, Thomas ML, Amini H, Broday D, Cohen A, Frostad J et al (2018) Data Integration for the assessment of population exposure to ambient air pollution for global burden of disease assessment. Environ Sci Technol 52:9069–9078
Shan A, Zhang Y, Zhang LW, Chen X, Li X, Wu H et al (2020) Associations between the incidence and mortality rates of type 2 diabetes mellitus and long-term exposure to ambient air pollution: a 12-year cohort study in northern China. Environ Res 186:109551
Shi K, Wu Y, Li L (2021) Quantifying and evaluating the effect of urban expansion on the fine particulate matter (PM2.5) emissions from fossil fuel combustion in China. Ecol Indic 125:107541
Shin HH, Parajuli RP, Gogna P, Maquiling A, Dehghani P (2021) Pollutant-sex specific differences in respiratory hospitalization and mortality risk attributable to short-term exposure to ambient air pollution. Sci Total Environ 755:143135
Snider G, Carter E, Clark S, Tseng J, Yang X, Ezzati M et al (2018) Impacts of stove use patterns and outdoor air quality on household air pollution and cardiovascular mortality in southwestern China. Environ Int 117:116–124
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB et al (2022) IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183:109119
Suryadhi MAH, Suryadhi PAR, Abudureyimu K, Ruma IMW, Calliope AS, Wirawan DN et al (2020) Exposure to particulate matter (PM2.5) and prevalence of diabetes mellitus in Indonesia. Environ Int 140:105603
Turner MC, Cohen A, Jerrett M, Gapstur SM, Diver WR, Pope CA 3rd et al (2014) Interactions between cigarette smoking and fine particulate matter in the Risk of Lung Cancer Mortality in Cancer Prevention Study II. Am J Epidemiol 180:1145–1149
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M et al (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1204–1222
Williams R, Karuranga S, Malanda B, Saeedi P, Basit A, Besancon S et al (2020) Global and regional estimates and projections of diabetes-related health expenditure: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diab Res Clin Pract 162:108072
Wu C, Yan Y, Chen X, Gong J, Guo Y, Zhao Y et al (2021) Short-term exposure to ambient air pollution and type 2 diabetes mortality: a population-based time series study. Environ Pollut 289:117886
Yang B-Y, Qian Z, Li S, Chen G, Bloom MS, Elliott M et al (2018) Ambient air pollution in relation to diabetes and glucose-homoeostasis markers in China: a cross-sectional study with findings from the 33 Communities Chinese Health Study. Lancet Planet Health 2:e64–e73
Yang BY, Fan S, Thiering E, Seissler J, Nowak D, Dong GH et al (2020) Ambient air pollution and diabetes: a systematic review and meta-analysis. Environ Res 180:108817
Yang M, Cheng H, Shen C, Liu J, Zhang H, Cao J et al (2020) Effects of long-term exposure to air pollution on the incidence of type 2 diabetes mellitus: a meta-analysis of cohort studies. Environ Sci Pollut Res Int 27:798–811
Yao Y, Lv X, Qiu C, Li J, Wu X, Zhang H et al (2022) The effect of China’s Clean Air Act on cognitive function in older adults: a population-based, quasi-experimental study. Lancet Health Longev 3:e98–e108
Yin P, Brauer M, Cohen AJ, Wang H, Li J, Burnett RT et al (2020) The effect of air pollution on deaths, disease burden, and life expectancy across China and its provinces, 1990–2017: an analysis for the Global Burden of Disease Study 2017. Lancet Planet Health 4:e386–e398
Yu K, Lv J, Qiu G, Yu C, Guo Y, Bian Z et al (2020) Cooking fuels and risk of all-cause and cardiopulmonary mortality in urban China: a prospective cohort study. Lancet Glob Health 8:e430–e439
Zhang S, Mwiberi S, Pickford R, Breitner S, Huth C, Koenig W et al (2021) Longitudinal associations between ambient air pollution and insulin sensitivity: results from the KORA cohort study. Lancet Planet Health 5:e39–e49
Zhang Y (2021) All-cause mortality risk and attributable deaths associated with long-term exposure to ambient PM2.5 in Chinese adults. Environ Sci Technol 55:6116–6127
Acknowledgements
The authors wish to acknowledge the contributions of Global Burden of Disease for assistance in providing data.
Funding
This study was financially supported by Scientific Research Program Funded by Hubei Provincial Department of Education (Grant No. Q20201104), Open Fund Project of Hubei Province Key Laboratory of Occupational Hazard Identification and Control (Grant No. OHIC2020Y01).
Author information
Authors and Affiliations
Contributions
Kai Wang: data curation, formal analysis, writing — original draft, writing — review and editing, visualization. Yunquan Zhang: conceptualization, methodology, data curation, writing — review and editing, visualization. Yaqi Wang: data curation, writing — review and editing. Jiaxin Liu: data curation, writing — review and editing. Peixuan Zhou: data curation, writing — review and editing. Zhouxin Yin: data curation, writing — review and editing. Shaocai Mo: data curation, writing — review and editing. Yang Yuan: data curation, writing — review and editing. Yong Yu: data curation, writing — review and editing. Minjin Peng: conceptualization, methodology, data curation, writing — review and editing, visualization.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, K., Zhang, Y., Wang, Y. et al. Secular trends in global burden of diabetes attributable to particulate matter pollution from 1990 to 2019. Environ Sci Pollut Res 29, 52844–52856 (2022). https://doi.org/10.1007/s11356-022-19510-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-022-19510-6