Abstract
Fipronil (FPN) is a relatively new and broad spectrum insecticide that induces toxic effects to animals and humans through induction of oxidative stress. Ginseng is a medicinal plant that has antioxidant, anti-inflammatory, and anti-apoptotic activities. Thus, the current study was conducted to evaluate the anti-toxic potential of ginseng aqueous extract (GAE) against FPN-induced hepatorenal toxicity in rats. Thirty-two male Wistar albino rats were randomly allocated into four equal groups. Rats of the control group received distilled water. The second group was administrated with GAE at a dose of 200 mg/kg b.w. orally day by day for 6 weeks. The third group was intoxicated with FPN at a dose of 4.85 mg/kg b.w. orally day by day for 6 weeks. The fourth group was administrated with GAE 2 h before FPN intoxication. Intoxication of rats with FPN significantly elevated the activities of serum alanine aminotransferase and aspartate aminotransferase and serum levels of urea and creatinine, as well as increased malondialdehyde level and protein expressions of caspase-3 and cyclooxygenase-2 in hepatic and renal tissues. However, it significantly decreased hepatic and renal GSH content and catalase activity. In addition, it induced histopathological alterations in hepatic and renal tissue architectures. Conversely, concomitant oral administration of GAE ameliorated the FPN-induced biochemical, pathological, and histochemical alterations in both hepatic and renal tissues. This study indicated that ginseng attenuates FPN-induced hepatorenal toxicity, possibly via its antioxidant, anti-apoptotic, and anti-inflammatory properties.

CAL ABSTRACTPHIRAG
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The indiscriminate use of insecticides and the resistance of insects mainly to organochlorines, organophosphates, and pyrethroids lead to the widespread use of other alternatives such as phenylpyrazoles, new second-generation insecticides, which are more efficient and selective for insects control (Simon-Delso et al. 2015).
Fipronil (FPN), a member of the phenylpyrazoles, is a relatively recent and broad spectrum insecticide. Owing to its efficacy even at low concentrations, it gained popularity worldwide for several residential, agricultural, and veterinary applications (Magalhães et al. 2018). The wide dissemination or misuses of fipronil-based products lead to multiple avenues for animal and human exposure (Wang et al. 2016). Additionally, FPN has bioaccumulative effect when used in agriculture; thus, it affects animals and humans via the food chain (Qin et al. 2015). Fipronil acts as a noncompetitive blocker to the GABA-gated chloride channels resulting in neuronal hyperexcitation, paralysis, and death of the insects (Gunasekara et al. 2007). Despite its selective toxicity to insects, there are many evidences donated that the primary metabolites of FPN, fipronil sulfone and fipronil desulfinyl, have higher potency at mammalian GABA-gated chloride channels than those of insects, indicating a potential hazard of these metabolites to insects and non-target organisms than the parent compound (Das et al. 2006). Besides being a neurotoxin (Raquel et al. 2011), FPN induces hepatic, renal, mutagenic, carcinogenic, and endocrine-disruptive toxic effects (Silva et al. 2015; Badgujar et al. 2016; El-Ballal et al. 2019). Earlier studies indicated the implication of FPN in oxidative tissue damages through increasing the production of reactive oxygen species (ROS) and decreasing the endogenous antioxidants (Abdel-Daim and Abdeen 2018; Abouelghar et al. 2020). Disturbance of cellular oxidant/antioxidant balance injuries cellular macromolecules, including nucleic acids, lipids, and proteins, resulting in cellular oxidative damage (Salminen and Paul 2014).
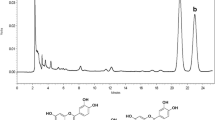
Antioxidants have been used to prevent and ameliorate the hazards of exposure to insecticides. Ginseng is a natural dietary supplement, belonging to panax genus and Araliaceae family, which is widely used as a medicinal plant (Wu et al. 2011). Among various ginseng species, American ginseng (P. quinquefolius), Chinese ginseng (P. notoginseng), and Korean ginseng (P. ginseng) are the most widespread worldwide (Lee and Kim 2014). Ginseng extracts contain various active constituents including, triterpene, saponins, essential oils, alkaloids, aminoglycosides, fatty acids, peptidoglycan, polysaccharides, vitamins, minerals, and phenolic compounds. Among them, ginsenosides are the major bioactive constituents of ginseng berry, leaf-stem, and root that are closely linked to the diverse physiological and pharmacological properties of ginseng (Yang et al. 2017). Ginseng is widely used as an alternative medicine and a natural remedy for the prevention and/or treatment of many diseases. It possesses anti-pyretic, anti-allergic, anti-aging, and immunostimulant properties (Kim et al. 2016). As well as, it has therapeutic potential in treatment of diabetes, hyperlipedemia, hypertension, cancer, and neurological and endocrine disorders (Yang et al. 2017; Ahuja et al. 2018). In addition, numerous studies spotlighted on the potential radioprotective (Mansour 2013), hepatoprotective (Abdel-Fattah et al. 2014), and nephroprotective (Raheem et al. 2017) effects of ginseng may be related to its anti-inflammatory, anti-apoptotic, and antioxidant properties (Youssef 2016; Raheem et al. 2017).
Set against the background of the risk of continuous exposure of animals and humans to FPN and the beneficial role of antioxidants against various toxic insults, this study was performed to evaluate the protective value of ginseng aqueous extract against fipronil-induced hepatorenal toxicity in rats with respect to its anti-inflammatory, anti-apoptotic, and antioxidant activities.
Materials and methods
Chemicals
Fipronil (Fipromex® 20% EC, MAC-GmbH, Company, Germany) was purchased from a local pesticide market. All kits used for biochemical analysis were obtained from Biodiagnostic Company (Giza, Egypt). Other chemicals were of analytical grade.
Preparation of ginseng aqueous extract
Korean red ginseng, Panax ginseng, root powder was obtained from Shannah Company, Egypt. Ginseng aqueous extract (GAE) was prepared following the method described by (King et al. 2006) with slight modification. Dry powdered ginseng roots were extracted in distilled water (1:9 w/v) at 90 °C for 1 h, cooled at room temperature for 30 min, and then centrifuged at 1200g for 15 min. The supernatant was collected and the pellets were re-suspended in distilled water at half the original volume. The extraction process was repeated twice. The supernatants obtained from all steps were collected and concentrated at 40 °C in hot air oven. The dried extract was kept at 4 °C and re-dissolved in distilled water immediately before administration.
Animals
Thirty-two adult male Wistar albino rats (130–150 g) were obtained from Al-Zyade Experimental Animals Production Center, Giza, Egypt. Rats were maintained in plastic cages on wood-chip bedding in well-ventilated animal house at 20 ± 3 °C temperature, 40–50% relative humidity, and daily natural dark/light cycle and provided with standard pellet feed and tap water ad libitum. Rats were acclimatized for 2 weeks prior to the beginning of the experiment. This study was ethically approved by the International Animal Care and Use Committee IACUC, Faculty of Veterinary Medicine, University of Sadat City, Egypt (Approval No.VUSC-007-1-17), which follows the Guide for the Care and Use of Laboratory Animals 8th edition. Washington (DC): National Academies Press (US); 2011.
Experimental animals and design
Rats were randomly allocated into four equal groups, 8 rats each.
Control group: Rats were given distilled water orally day by day for 6 weeks.
Ginseng aqueous extract group: Rats were administered ginseng aqueous extract (GAE) at a dose of 200 mg/kg b.w. orally day by day for 6 weeks (Al-Hazmi et al. 2015).
Fipronil group: Rats were administered fipronil (FPN) at a dose of 4.85 mg/kg b.w. orally day by day for 6 weeks (Tingle et al. 2003).
Ginseng aqueous extraxt and Fipronil group: Rats were given GAE as ginseng group 2 h before FPN administration as the fipronil group.
The selected dose of FPN was 1/20 of LD50 based on oral LD50 of FPN (97 mg/kg b.w.) in rats (Tingle et al. 2003).
Samples collection
Blood sampling
Twenty-four hours after the last administration, rats were fasted overnight and anesthetized by inhalation of isoflurane. Blood samples were collected without anticoagulant, centrifuged at 3000 rpm for 15 min, and sera samples were separated and stored at − 20 °C for further biochemical analysis.
Tissue sampling
After animals were euthanized by decapitation, the livers and kidneys of rats were immediately excised and divided into two parts. One part was washed with physiological saline then stored at − 80 °C for further tissue biochemical analysis. The other part was immediately kept in 10% neutral buffered formalin for histopathological and immunohistochemical examinations.
Assessment of serum liver and kidney functions biomarkers
Serum activities of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were measured according to the methods described by Reitman and Frankel, (1957). Urea and creatinine levels were measured according to Fawcett and Soctt (1960) and Schirmeister et al. (1964), respectively.
Assessment of oxidant/antioxidant status
Hepatic and renal tissue malondialdehyde (MDA) level, reduced glutathione (GSH) content, and catalase (CAT) activity were estimated by using commercial kits following the manufacturer’s instructions according to Ohkawa et al. (1979), Beutler et al. (1963), and Aebi (1984), respectively.
Histopathological examinations
The preserved liver and kidney specimens were routinely processed and stained by hematoxylin and eosin (H&E) stain for histopathological examination according to Bancroft and Gamble (2008).
Immunohistochemical investigations
The immunostaining method for localization of caspase-3 and COX-2 was performed following the method described by Liu et al. (2017) and Lin and Prichard (2015), respectively. The formalin-fixed liver and kidney sections were deparaffinized, hydrated in alcohol solutions, incubated in 3% H2O2, and then incubated with anti-caspase-3 (1:1000 dilution, Abcam, Ltd., USA) or anti-COX-2 (1:100 dilution, Abcam, Ltd., USA). The immune reactions were visualized by using diaminobenzidene (DAB; Sigma Chemical Co., USA) and semiquantitatively scored from 0 to 4, according to the percentage of positively immune stained cells (dark brown cytoplasm and nucleus) that were estimated in five random high-power fields (× 40), as previously described by (Rahman et al. 2001). Zero indicates negative staining, 1 indicates ˂ 25% of positive cells per field, 2 indicates 25–50%, 3 indicates 51–75%, and 4 indicates ˃ 75%.
Statistical analysis
Data are presented as mean ± standard error (SE). Statistical analysis was determined by one-way ANOVA followed by Duncan’s multiple range test for post hoc to determine the statistically significant (P < 0.05) differences among the experimental groups. All statistical analyses were performed by using SPSS (Statistical package for Social Sciences) Version 16 released on 2007.
Results
Ginseng aqueous extract ameliorated the toxic effects of FPN on general health condition of rats
Along the experimental period, no mortalities were recorded among different groups. No clinical manifestations were observed in either the control or GAE groups. However, rough hair coat, dullness, depression, and mild tremor were the apparent symptoms of toxicity observed in the FPN-intoxicated group. Rats of the GAE and FPN group showed apparent normal health conditions.
Ginseng aqueous extract normalized FPN-induced alterations in serum liver and kidney functions biomarkers of rats
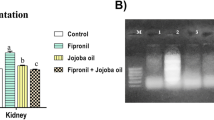
The effects of FPN and/or GAE on serum hepatic and renal functions biomarkers were presented in Fig. 1. Fipronil intoxication significantly (P ˂ 0.05) increased the activities of serum ALT and AST and serum levels of urea and creatinine compared to the control rats. Conversely, administration of rats with GAE 2 h before FPN intoxication normalized the serum activities of ALT and AST and serum levels of urea and creatinine. On the other hand, GAE had no significant effects on liver and kidney functions biomarkers compared to the control group.
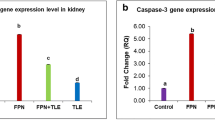
Ginseng aqueous extract prevented FPN-induced deterioration of hepatic and renal oxidant/antioxidant status of rats
Intoxication of rats with FPN significantly (P ˂ 0.05) increased hepatic and renal MDA levels, while it decreased GSH contents and CAT activity, compared to the control group. On the contrary, administration of rats with GAE 2 h before their intoxication prevented FPN-induced increase in MDA levels and decrease in GSH contents and CAT activity in hepatic and renal tissues. However, no significant changes in hepatic and renal MDA levels, GSH contents, and CAT activity were detected between GAE and the control groups (Fig. 2).
Ginseng aqueous extract modulated FPN-induced alterations of hepatic and renal tissue architectures of rats
Liver sections of control (Fig. 3a) and GAE (Fig. 3b) groups appeared normal with no definite histopathological alterations. Conversely, the liver of the FPN-intoxicated group revealed extensive vacuolization with marked ballooning of hepatocytes associated with focal sinusoidal congestion as well as apoptotic hepatocytes (Fig. 3c). However, marked attenuation of hepatocellular vacuolization with very mild cytoplasmic granulation in hepatic parenchyma were observed in GAE- and FPN-treated group (Fig. 3d).
Representative photomicrographs of liver sections of rats in different groups (H&E stain × 40). a Control group and b GAE group showing normal central vein (CV) and hepatocytes, c FPN group showing extensive vacuolization with marked ballooning of hepatocytes (black arrows) associated with focal sinusoidal congestion (yellow arrow), and d GAE and FPN group showing very mild cytoplasmic granulation (black arrows)
Renal tissue of control rats showed normal glomerular tuft and tubular epithelium (Fig. 4a). Also, kidneys of GAE-treated group appeared normal and identical to the control group (Fig. 4b). Marked histopathological lesions were demonstrated in the kidney of FPN-intoxicated rats. The main demonstrated lesions were focal necrosis of renal tubular epithelial cells intensely infiltrated by mononuclear infiltrates (Fig. 4c). Interestingly, the kidneys of GAE and FPN group appeared normal in all examined sections with few sporadic intertubular inflammatory cell infiltrates, and necrosis was restricted to sparse cells (Fig. 4d).
Representative photomicrographs of kidney sections of rats in different groups (H&E stain, × 40). a Control group and b GAE group showing normal glomerular and tubular epithelium, c FPN group showing focal necrosis of renal tubular epithelial cells intensely infiltrated by mononuclear infiltrates (black arrows), and d GAE and FPN group showing sporadic intertubular inflammatory cell infiltrates (yellow arrow)
Ginseng aqueous extract reduce FPN-increased protein expressions of caspase-3 and cyclooxygenase-2 in hepatic and renal tissues of rats
Negative immune reactivity for caspase-3 was demonstrated in the hepatic and renal tissues of the control and GAE groups (Figs. 5a, b and 6a, b, respectively). In contrast, significant increase of caspase-3 immune reactivity was recorded in the hepatic (Fig. 5c) and renal (Fig. 6c) tissues of the FPN-intoxicated group, and the percentages of positive cells were 3.40 ± 0.40 and 2.60 ± 0.50, respectively (Table 1). This immune reactivity was significantly reduced in the GAE and FPN group in both liver (Fig. 5d) and kidneys (Fig. 6d), and the percentages of positive cells were 1.80 ± 0.37 and 0.83 ± 0.37, respectively (Table 1).
Representative photomicrographs of caspase-3 (a–d) and COX-2 (e–h) immunohistochemically stained liver, × 40. a and e control group showing no caspase-3 (a) and no COX-2 immune reactive cells (e). b, f GAE group showing no caspase-3 (b) and no COX-2 immune reactive cells (f). c, g FPN group showing increase of positively immune reactive cells for caspase-3 (c) and COX-2 (g). d, h GAE and FPN group showing marked decrease of positively immune reactive cells for caspase-3 (d) and COX-2 (h)
Representative photomicrographs of caspase-3 (a–d) and COX-2 (e–h) immunohistochemically stained kidney, × 40. a, e control group showing no caspase-3 (a) and no COX-2 immune reactive cells (e). b, f GAE group showing no caspase-3 (b) and no COX-2 immune reactive cells (f). c, g FPN group showing strong positively stained cells for caspase-3 (c) and COX-2 (g). d, h GAE and FPN group showing weak positively stained cells for caspase-3 (d) and COX-2 (h)
Liver of the control (Fig. 5e) and GAE (Fig. 5f) groups showed no COX-2 immune reactive cells. Similarly, no COX-2 immune reactivity was demonstrated in the kidneys of the control (Fig. 6e) and GAE (Fig. 6f) groups. On the contrary, COX-2 immune reactivity was markedly increased in the liver and kidneys of FPN group (Fig. 5g and 6g, respectively) and the percentages of positive cells were 3.00 ± 0.31and 3.60 ± 0.24, respectively (Table 1). Pronounced reduction of COX-2 immune reactivity was recorded in the liver (Fig. 5h) and kidneys (Fig. 6h) of GAE and FPN group and the percentages of positive cells were 1.60 ± 0.40 and 1.60 ± 0.24, respectively (Table 1).
Discussion
Introduction of new insecticides into the environment has raised the concern for identification of their potential health hazards. Fipronil is widely used in agro-vet practices; however, it causes serious environmental and public health hazards (Tingle et al. 2003) through inducing oxidative stress in vivo and in vitro (Ki et al. 2012; Badgujar et al. 2015a,b). On the other hand, ginseng has been indicated to have anti-inflammatory, anti-apoptotic, and antioxidant properties (El-Bialy et al. 2020).
The current study indicated that FPN elicited an increment in serum levels of liver and kidney biomarkers, represented by elevated activities of ALT and AST and levels of urea and creatinine. The obtained results were in accordance with those reported by Mossa et al. (2015) and Abdel-Daim and Abdeen (2018). The marked increase in the serum ALT and AST activities observed in FPN-intoxicated rats indicates the injury of hepatocytes and alteration in its membrane permeability, thus, additional ALT and AST are released into the bloodstream (Kasarala and Tillmann 2016).The elevated urea level indicates impairment in renal tubular reabsorption, while the increase in serum creatinine level reflects impairment of glomerular filtration rate (Adedara et al. 2012). These alterations in the liver and kidney functions may be attributed to the ability of FPN to induce hepatic and renal tissue injuries. This assumption was confirmed by the histopathological findings in our study (Figs. 3 and 4), which were in line with previous studies that reported degenerative changes in hepatic and renal architectures following the exposure to FPN (Mossa et al. 2015; El-Ballal et al. 2019). The possible reason behind FPN-induced hepatic and renal tissue injuries may be the disturbance of oxidant/antioxidant status of the liver and kidney as our study demonstrated that oral administration of FPN induced hepatic and renal oxidative stress evidenced by the marked increase of MDA level with suppression of GSH content and CAT activity in hepatic and renal tissues, which were parallel with the previous findings reported by (Badgujar et al. 2015a, b; Mossa et al. 2015; El-Ballal et al. 2019). This disturbance in oxidant/antioxidant balance in the liver and kidneys is due to some xenobiotics induce toxicity via generation of ROS causing alterations in cellular antioxidants, and hence increase susceptibility to oxidative stress (OS) (Lopez et al. 2007). Lipid peroxidation (LPO) is an essential marker of OS and MDA is the end product of LPO that reflects the degree of cellular oxidative damage (Nabavi et al. 2012). Reactive oxygen species attack cellular components to generate peroxyl radicals, which undergo a cyclization reaction to produce endoperoxides, and finally MDA (Marnett 1999). GSH is a free radical scavenger and acts as a substrate for glutathione s-transferase and glutathione peroxidase for detoxification of free radicles (Parke and Piotrowski 1996). Catalase is a cellular antioxidant enzyme, which along with glutathione peroxidase rapidly converts H2O2 to water (Scibior and Czeczot 2006). Fipronil-induced injury of hepatic and renal tissues in our study may be due to oxidative stress-induced caspase-3 and Cox-2 protein expressions in these tissues (Figs. 5 and 6). These findings were in accordance with previous studies that reported an increase of caspase-3 immune reactivity in the hepatic and renal tissue of FPN-intoxicated rats (Abdel-Daim and Abdeen 2018) and increase of COX-2 expression in human neuroblastoma SH-SY5Y cells treated with FPN (Park et al. 2016). Caspase-3 and Cox-2 mediate apoptosis process, important for the maintenance and development of multicellular organisms, and participate in various physiological, pathological, and toxicological conditions (Majno and Joris 1995). Apoptosis is mediated by a proteolytic caspases essential for initiation, regulation, and execution of proteolytic processes (Thornberry 1999); among them, active caspase-3 is used for detection of apoptotic cells because it is the main executioner of apoptosis (Jakob et al. 2008). Cyclooxygenase-2, an immediate response protein, is upregulated in response to various stimuli, including environmental toxicants and proinflammatory cytokines (Narita et al. 2008). Moreover, COX-2 is implicated not only in inflammation but also in carcinogenesis, affecting cell proliferation, differentiation, apoptosis, angiogenesis, and metastasis (Williams et al. 1999). Oxidative stress is the main cause of cellular damage associated with xenobiotics and inflammatory stimuli. Reactive oxygen species produced during OS has been recorded to initiate signaling cascades resulting in apoptosis (Yu et al. 2004). Furthermore, ROS induce inflammatory response and mediate COX-2 expression (Barbieri et al. 2003). Induction of COX-2 in tissues initiates apoptosis by increasing prostaglandin-2 level (Hu et al. 2017). Thus, FPN induced the marked increases in the hepatic and renal MDA level which may indicate the development of OS in the tissues. Moreover, the observed reduction in the hepatic and renal GSH content and CAT activity may be due to the overutilization of the intracellular GSH and CAT to combat the increased ROS production after exposure to FPN, ultimately oxidative hepatic and renal tissue damages via induction of caspase-3 and COX-2 expressions in both hepatic and renal tissues.
Furthermore, our results indicated that administration of GAE 2 h before FPN intoxication protected rats from FPN-induced hepatorenal toxicity. These findings were evidenced by a significant decrease of serum ALT and AST activities and urea and creatinine levels as a result of the antioxidant properties of GAE, represented by marked reduction of hepatic and renal MDA level concomitantly with significant elevation of GSH content and CAT activity. These antioxidant activities of GAE reduced caspase-3 and COX-2 expression in hepatic and renal tissues that ameliorated FPN-induced alterations of hepatic and renal tissue architectures. Our findings were in line with the previous studies that indicate the hepatoprotective effect of ginseng against CCl4 (Bak et al. 2012), cadmium (Park et al. 2013), aflatoxins (Abdel-Fattah et al. 2014), and methotrexate (Youssef 2016). In addition, GAE has protective effect against cisplatin (Abdel-Wahhab and Ahmed 2004), streptozotocin (Hussein et al. 2011), ochratoxin (Morsy et al. 2012), gamma-irradiation (Mansour 2013), and gentamicin-induced (Raheem et al. 2017) nephrotoxicity. These hepatonephroprotective effects of GAE may be related to the antioxidant effect of ginseng that is closely linked to its ginsenoside content (Song et al. 2019) as it stimulates gene expression of antioxidant enzymes and enhances their activities, which play a crucial role for maintaining cell viability, by decreasing the oxygen radical produced by the intracellular metabolites (Zhang et al. 2008). Ginsenosides inhibit LPO by scavenging ROS, restoring GSH level, and inhibiting NO production (Kang et al. 2007; Zhu et al. 2009; Zhang et al. 2010). These antioxidant activities of ginseng may enable it to prevent the apoptosis of kidney tissue after exposure to gentamicin through its ability to reduce caspase-3 reactivity. (Raheem et al. 2017). In addition, Kang et al. (2006) stated that ginseng prevent renal damage in diabetic rats by reducing the overexpression of COX-2 confirming its anti-inflammatory properties that may be due to its ability to inhibit TNF-α-induced NF-κB transcription activity and NF-κB-dependent COX-2 and iNOS gene expressions (Song et al. 2012). Therefore, GAE exerted its protective effects against FPN-induced hepatorenal toxicity which may be via its antioxidant, anti-apoptotic, and anti-inflammatory activities.
Conclusion
Our findings provided evidences for the implication of oxidative stress, inflammation, and apoptosis to fipronil-induced hepatorenal toxicity and highlighted the ameliorative effect of ginseng, possibly via its antioxidant, anti-apoptotic, and anti-inflammatory properties. Therefore, the overall obtained data may be of crucial value in presenting ginseng as an effective therapeutic strategy against toxic effects of FPN and other phenylpyrazoles.
References
Abdel-Fattah SM, Safaa MA, Sanad MI, Helal AD, Sarfinaz S, Abd ElGhany Ragaa F, Ghanem F (2014) Biochemical and histochemical studies on white ginseng roots for ameliorating aflatoxicosis in rats. Int J Curr Microbiol App Sci 3(10):458–473
Abdel-Daim MM, Abdeen A (2018) Protective effects of rosuvastatin and vitamin E against fipronil-mediated oxidative damage and apoptosis in rat liver and kidney. Food Chem Toxicol 114:69–77. https://doi.org/10.1016/j.fct.2018.01.055
Abdel-Wahhab MA, Ahmed HH (2004) Protective effects of Korean Panax ginseng against chromium VI toxicity and free radical generation in rats. J Ginseng Res 28:11–17. https://doi.org/10.5142/JGR.2004.28.1.011
Abouelghar GE, El-Bermawy ZA, Salman HMS (2020) Oxidative stress, hematological and biochemical alterations induced by sub-acute exposure to fipronil (COACH®) in albino mice and ameliorative effect of selenium plus vitamin E. Environ Sci Pollut Res 27:7886–7900. https://doi.org/10.1007/s11356-019-06579-9
Adedara A, Teberen R, Ebokaiwe AP, Ehwerhemuepha T, Farombi EO (2012) Induction of oxidative stress in liver and kidney of rats exposed to Nigerian bonny light crude oil. Environ Toxicol 27(6):372–379. https://doi.org/10.1002/tox.20660
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126. https://doi.org/10.1016/s0076-6879(84)05016-3
Ahuja A, Kim JH, Kim JH, Yi YS, Cho JY (2018) Functional role of ginseng-derived compounds in cancer. J Ginseng Res 42(3):248–254. https://doi.org/10.1016/j.jgr.2017.04.009
Al-Hazmi MA, Rawi SM, Arafa NM, Wagas A, Montasser AO (2015) The potent effects of ginseng root extract and memantine on cognitive dysfunction in male albino rats. Toxicol Ind Health 31(6):494–509. https://doi.org/10.1177/0748233713475517
Badgujar PC, Chandratre GA, Pawar NN, Telang AG, Kurade NP (2015a) Fipronil induced oxidative stress involves alterations in SOD1 and catalase gene expression in male mice liver: protection by vitamins E and C. Environ Toxicol 31(9):1147–1158. https://doi.org/10.1002/tox.22125
Badgujar PC, Pawar NN, Chandratre GA, Telang AG, Sharma AK (2015b) Fipronil induced oxidative stress in kidney and brain of mice: protective effect of vitamin E and vitamin C. Pestic Biochem Physiol 118:10–18. https://doi.org/10.1016/j.pestbp.2014.10.013
Badgujar PC, Selkar NA, Chandratre GA, Pawar NN, Dighe VD, Bhagat ST, Telang AG, Vanage GR (2016) Fipronil-induced genotoxicity and DNA damage in vivo: protective effect of vitamin E. Hum Exp Toxicol 36(5):508–519. https://doi.org/10.1177/0960327116655388
Bak MJ, Mira J, Woo-Sik J (2012) Antioxidant and hepatoprotective effects of the red ginseng essential oil in H2O2-treated HepG2 cells and CCl4-treated mice. Int J Mol Sci 13(2):2314–2330. https://doi.org/10.3390/ijms13022314
Bancroft JD, Gamble M (2008) Theory and Practice of histological techniques. 6th Edition. Churchill, Livingstone, New York, London. 440-450
Barbieri SS, Eligini S, Brambilla M, Tremoli E, Colli S (2003) Reactive oxygen species mediate cyclooxygenase-2 induction during monocyte to macrophage differentiation: critical role of NADPH oxidase. Cardiovasc Res 60(1):187–197. https://doi.org/10.1016/S0008-6363(03)00365-1
Beutler EK, Duron O, Kefly BM (1963) Improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Das PC, Cao Y, Cherrington N, Hodgson E, Rose RL (2006) Fipronil induces CYP isoforms and cytotoxicity in human hepatocytes. Chem Biol Interact 164(3):200–214. https://doi.org/10.1016/j.cbi.2006.09.013
El-Ballal SS, Amer HA, Tahoun EA, EL-Borai NB, Abuo Zahra MA (2019) Bee pollen alleviates fipronil and emamectin benzoate induced- hepatorenal toxicity in rats. Assiut Vet Med J 65(161):164–173
El-Bialy BES, Abd Eldaim MA, Hassan A, Abdel-Daim MM (2020) Ginseng aqueous extract ameliorates lambda-cyhalothrin-acetamiprid insecticide mixture for hepatorenal toxicity in rats: role of oxidative stress-mediated proinflammatory and proapoptotic protein expressions. Environ Toxicol 35:124–135. https://doi.org/10.1002/tox.22848
Fawcett JK, Soctt JE (1960) A rapid and precise method for the determination of urea. J Clin Pathol 13(2):156–159. https://doi.org/10.1136/jcp.13.2.156
Gunasekara AS, Truong T, Goh KS, Spurlock F, Tjeerdema RS (2007) Environmental fate and toxicology of fipronil. J Pestic Sci 32:198–199. https://doi.org/10.1584/jpestics.R07-02
Hu YP, Peng YB, Zhang YF, Wang Y, Yu WR, Yao M, Fu XJ (2017) Reactive oxygen species mediated prostaglandin E2 contributes to acute response of epithelial injury. 4123854:8 . https://doi.org/10.1155/2017/4123854
Hussein J, El-Khayat Z, Ramzy T, Ashour M, Oraby F (2011) Protective effect of Panax ginseng against Streptozotocin induced renal dysfunction in rats. J Appl Sci Res 7(10):1419–1423
Jakob S, Corazza N, Diamantis E, Kappeler A, Brunner T (2008) Detection of apoptosis in vivo using antibodies against caspase-induced neo-epitopes. Methods 44(3):255–261. https://doi.org/10.1016/j.ymeth.2007.11.004
Kang KS, Kim HY, Yamabe N, Nagai R, Yokozawa T (2006) Protective effect of sun ginseng against diabetic renal damage. Biol Pharm Bull 29(8):1678–1684. https://doi.org/10.1248/bpb.29.1678
Kang KS, Kim HY, Baek SH, Yoo HH, Park JH, Yokozawa T (2007) Study on the hydroxyl radical scavenging activity changes of ginseng and ginsenoside-Rb2 by heat processing. Biol Pharm Bull 30:724–728. https://doi.org/10.1248/bpb.30.724
Kasarala G, Tillmann HL (2016) Standard liver tests. Clin Liver Dis 8:13–18. https://doi.org/10.1002/cld.562
Ki YW, Lee JE, Park JH, Shin IC, Koh HC (2012) Reactive oxygen species and mitogen-activated protein kinase induce apoptotic death of SH-SY5Y cells in response to fipronil. Toxicol Lett 211:18–28. https://doi.org/10.1016/j.toxlet.2012.02.022
Kim JK, Tabassum N, Uddin MR, Park SU (2016) Ginseng: a miracle sources of herbal and pharmacological uses. Orient Pharm Exp Med 16:243–250. https://doi.org/10.1007/s13596-016-0246-6
King MS, Adler MD, Murphy LL (2006) Extraction-dependent effects of American ginseng (Panax quinquefolium) on human breast cancer cell proliferation and estrogen receptor activation. Integr Cancer Ther 5(3):236–243. https://doi.org/10.1177/1534735406291341
Lee CH, Kim JH (2014) A review on the medicinal potentials of ginseng and ginsenosides on cardiovascular diseases. J Ginseng Res 38(3):161–166. https://doi.org/10.1016/j.jgr.2014.03.001
Lin F, Prichard J (2015) Handbook of practical immunohistochemistry. Springer, New York
Liu PF, Hu YC, Kang BH, Tseng YK, Wu PC, Liang CC, Hou YY, Fu TY, Liou HH, Hsieh IC, Ger LP, Shu CW (2017) Expression levels of cleaved caspase-3 and caspase-3 in tumorigenesis and prognosis of oral tongue squamous cell carcinoma. PLoS One 12(7):e0180620. https://doi.org/10.1371/journal.pone.0180620
Lopez O, Hernandez AF, Rodrigo L, Gil F, Pena G, Serrano JL, Parron T, Villanueva E, Pla A (2007) Changes in antioxidant enzymes in humans with long-term exposure to pesticides. Toxicol Lett 171(3):146–153. https://doi.org/10.1016/j.toxlet.2007.05.004
Magalhães J, Sandini T, Berto Udo M, Fukushima A, Spinosa H (2018) Fipronil: uses, pharmacological and toxicological features. Revinter 11(1):67–83. https://doi.org/10.22280/revintervol11ed1.344
Majno G, Joris I (1995) Apoptosis, oncosis, and necrosis: an overview of cell death. Am J Clin Pathol 146(1):3–15
Mansour HH (2013) Protective effect of ginseng against gamma-irradiation-induced oxidative stress and endothelial dysfunction in rats. EXCLI J 12:766–777
Marnett LJ (1999) Lipid peroxidation-DNA damage by malondialdehyde. Mutat Res Fundam Mol Mech Mutagen 424(1–2):83–95. https://doi.org/10.1016/s0027-5107(99)00010-x
Morsy F, el Din A, Farrag A, Farrag H, Badawi M, Shaffie N (2012) Ochratoxin a toxic effect on rat kidneys and the potential protective effect of ginseng: histopathologic, histochemical, and image analysis morphometric studies. Maced J Med Sci 5(1):40–48. https://doi.org/10.3889/MJMS.1857-5773.2012.0195
Mossa AH, Swelam ES, Mohafrasha SMM (2015) Sub-chronic exposure to fipronil induced oxidative stress, biochemical and histopathological changes in the liver and kidney of male albino rats. Toxicol Rep 2:775–784. https://doi.org/10.1016/j.toxrep.2015.02.009
Nabavi SM, Nabavi SF, Eslami S, Moghaddam AH (2012) In vivo protective effects of quercetin against sodium fluoride-induced oxidative stress in the hepatic tissue. Food Chem 132(2):931–935. https://doi.org/10.1016/j.foodchem.2011.11.070
Narita M, Shimamura M, Imai S, Kubota C, Yajima Y, Takagi T, Shiokawa M, Inoue T, Suzuki M, Suzuki T (2008) Role of interleukin-1beta and tumor necrosis factor-alpha-dependent expression of cyclooxygenase-2 mRNA in thermal hyperalgesia induced by chronic inflammation in mice. Neuroscience. 152(2):477–486. https://doi.org/10.1016/j.neuroscience.2007.10.039
Ohkawa H, Ohishi W, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95(2):351–358. https://doi.org/10.1016/0003-2697(79)90738-3
Park SJ, Lee JR, Jo MJ, Park SM, Ku SK, Kim SC (2013) Protective effects of Korean red ginseng extract on cadmium-induced hepatic toxicity in rats. J Ginseng Res 37(1):37–44. https://doi.org/10.5142/jgr.2013.37.37
Park JH, Park YS, Lee JB, Park KH, Paik MK, Jeong M, Koh HC (2016) Meloxicam inhibits fipronil-induced apoptosis via modulation of the oxidative stress and inflammatory response in SH-SY5Y cells. J Appl Toxicol 36(1):10–23. https://doi.org/10.1002/jat.3136
Parke DV, Piotrowski JK (1996) Glutathione: its role in detoxication of reactive oxygen species and environmental chemicals. Toxicol 4:1–13
Qin F, Gao Y, Xu P, Guo B, Li J, Wang H (2015) Enantioselective bioaccumulation and toxic effects of fipronil in the earthworm Eisenia foetida following soil exposure. Pest Manag Sci 71(4):553–561. https://doi.org/10.1002/ps.3841
Raheem SA, Meselhy AR, Hafiez SA, Naby NA (2017) Evaluation of the protective effect of ginseng against gentamicine-induced nephrotoxicity in adult, albino rats: a histochemical and immunohistochemical study. Al Azhar Assiut Med J 15(1):35–42. https://doi.org/10.4103/AZMJ.AZMJ_4_17
Rahman MA, Dhar DK, Yamaguchi E, Maruyama S, Sato T, Hayashi H, Ono T, Yamanoi A, Kohno H, Nagasue N (2001) Coexpression of inducible nitric oxide synthase and COX-2 in hepatocellular carcinoma and surrounding liver: possible involvement of COX-2 in the angiogenesis of hepatitis C virus-positive cases. Clin Cancer Res 7(5):1325–1332
Raquel P, Tercariol G, Godinho AF (2011) Behavioral effects of acute exposure to the insecticide fipronil. Pestic Biochem Physiol 99(3):221–225. https://doi.org/10.1016/j.pestbp.2010.12.007
Reitman S, Frankel S (1957) Colorimetric determination of serum oxalacetic and glutamic pyruvic transaminase. Amer J Clin Pathol 28(1):56–63. https://doi.org/10.1093/ajcp/28.1.56
Salminen LE, Paul RH (2014) Oxidative stress and genetic markers of suboptimal antioxidant defense in the aging brain: a theoretical review. Rev Neurosci 25(6):805–819. https://doi.org/10.1515/revneuro-2014-0046
Schirmeister J, Willmman H, Kiefer H (1964) Plasma creatinine as rough indicator of renal function. Dtsch Med Wschr 89:1940–1947
Scibior D, Czeczot H (2006) Catalase: structure, properties, functions. Postepy Hig Med Dosw (Online) 60:170–180
Silva M, Pham N, Lewis C, Iyer S, Kwok E, Solomon G, Zeise L (2015) A comparison of ToxCast test results with in vivo and other in vitro endpoints for neuro, endocrine, and developmental toxicities: a case study using endosulfan and methidathion. Birth Defects Res B Dev Reprod Toxicol 104(2):71–89. https://doi.org/10.1002/bdrb.21140
Simon-Delso N, Amaral-Rogers V, Belzunces LP, Bonmatin JM, Chagnon M, Downs C, Furlan L, Gibbons DW, Giorio C, Girolami V, Goulson D, Kreutzweiser DP, Krupke CH, Liess M, Long E, McField M, Mineau P, Mitchell EAD, Morrissey CA, Noome DA, Pisa L, Settele J, Stark JD, Tapparo A, van Dyck H, van Praagh J, van der Sluijs JP, Whitehorn PR, Wiemers M (2015) Systemic insecticides (neonicotinoids and fipronil): trends, uses, mode of action and metabolites. Environ Sci Pollut Res Int 22:5–34. https://doi.org/10.1007/s11356-014-3470
Song SB, Tung NH, Quang TH, Ngan NTT, Kim KE, Kim YH (2012) Inhibition of TNF-α-mediated NF-κB transcriptional activity in HepG2 cells by Dammarane-type Saponins from Panax ginseng leaves. J Ginseng Res 36(2):146–152. https://doi.org/10.5142/jgr.2012.36.2.146
Song YN, Hong HG, Son JS, Kwon YO, Lee HH, Kim HJ, Park JH, Son MJ, Oh JG, Yoon MH (2019) Investigation of ginsenosides and antioxidant activities in the roots, leaves, and stems of hydroponic-cultured ginseng (Panax ginseng Meyer). Prev Nutr Food Sci 24(3):283–292. https://doi.org/10.3746/pnf.2019.24.3.283
Thornberry NA (1999) Caspases: a decade of death research. Cell Death Differ 6(11):1023–1027. https://doi.org/10.1038/sj.cdd.4400607
Tingle CC, Rother JA, Dewhurst CF, Lauer S, King WJ (2003) Fipronil: environmental fate, ecotoxicology, and human health concerns. Rev Environ Contam Toxicol 176:1–66. https://doi.org/10.1007/978-1-4899-7283-5_1
Wang X, Martínez MA, Wu Q, Ares I, Martínez-Larrañaga MR, Anadón A, Yuan Z (2016) Fipronil insecticide toxicology: oxidative stress and metabolism. Crit Rev Toxicol 46(10):876–899. https://doi.org/10.1080/10408444.2016.1223014
Williams CS, Mann M, DuBois RN (1999) The role of cyclooxygenases in inflammation, cancer, and development. Oncogene 18:7908–7916. https://doi.org/10.1038/sj.onc.1203286
Wu Y, Lu X, Xiang FL, Lui EM, Feng Q (2011) North American ginseng protects the heart from ischemia and reperfusion injury via up regulation of endothelial nitric oxide synthase. Pharmacol Res 64(3):195–202. https://doi.org/10.1016/j.phrs.2011.05.006
Yang Y, Ren C, Zhang Y, Wu X (2017) Ginseng: an non negligible natural remedy for healthy aging. Aging Dis 8(6):708–720. https://doi.org/10.14336/AD.2017.0707
Youssef GA (2016) Role of ginseng as hepatoprotective, antioxidant and anti-inflammatory against methotrexate induced liver injury in rats. Egypt J Hosp Med 62:105–108. https://doi.org/10.12816/0021419
Yu C, Rahmani M, Dent P, Grant S (2004) The hierarchical relationship between MAPK signaling and ROS generation in human leukemia cells undergoing apoptosis in response to the proteasome inhibitor Bortezomib. Exp Cell Res 295(2):555–566. https://doi.org/10.1016/j.yexcr.2004.02.001
Zhang QH, Wu CF, Duan L, Yang JY (2008) Protective effects of ginsenoside Rg (3) against cyclophosphamide-induced DNA damage and cell apoptosis in mice. Arch Toxicol 82(2):117–123. https://doi.org/10.1007/s00204-007-0224-3
Zhang HA, Wang M, Zhou J, Yao QY, Ma JM, Jiang CL (2010) Protective effect of ginsenoside against acute renal failure and expression of tyrosine hydroxylase in the locus coeruleus. Physiol Res 59(1):61–70
Zhu D, Wu L, Li CR, Wang XW, Ma YJ, Zhong ZY, Zhao HB, Cui J, Xun SF, Huang XL, Zhou Z, Wang SQ (2009) Ginsenoside Rg1 protects rat cardiomyocyte from hypoxia/reoxygenation oxidative injury via antioxidant and intracellular calcium homeostasis. J Cell Biochem 108(1):117–124. https://doi.org/10.1002/jcb.22233
Author information
Authors and Affiliations
Corresponding author
Additional information
Editorial Responsibility: Philippe Garrigues
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
Fipronil elevated liver and kidney functions biomarkers.
It induced oxidative stress, hepatic and renal tissue injuries, and apoptosis.
Ginseng normalized liver and kidney function biomarkers.
It modulated hepatic and renal tissue injury, inflammation and oxidative stress.
It ameliorated caspase 3 and COX-2 protein expression in hepatic and renal tissues.
Rights and permissions
About this article
Cite this article
Abd Eldaim, M.A.A., Abd El Latif, A.S., Hassan, A. et al. Ginseng attenuates fipronil-induced hepatorenal toxicity via its antioxidant, anti-apoptotic, and anti-inflammatory activities in rats. Environ Sci Pollut Res 27, 45008–45017 (2020). https://doi.org/10.1007/s11356-020-10306-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-020-10306-0