Abstract
Introduction
Symptoms of obstructive sleep apnea (OSA) and poor sleep quality affect around one in ten people in India. We aimed to determine if OSA symptoms and poor sleep quality are independently associated with cognition in middle-aged and elderly urban Indian populations.
Methods
We studied the cross-sectional association between OSA symptoms (by Berlin Questionnaire), poor sleep quality (by Pittsburgh Sleep Quality Index), and cognitive function in adults ≥ 50 years. Using a standard neuropsychological battery for cognitive function, a G-factor was derived as the first rotated principal component assessing domains of information processing, memory, and executive function. The associations of exposures with cognitive measures were modeled using linear regression, adjusted for metabolic risk factors, lifestyle factors, and psychosocial problems, followed by stratified analysis by decadal age group.
Results
A total of 7505 adults were enrolled. Excluding those with MMSE < 26 (n 710), of 6795 individuals (49.2% women), mean (SD) age 64.2 (9.0) years, 38.3% had high risk of OSA symptoms, and 15.9% had poor sleep quality. OSA symptoms were negatively associated with cognitive domains of information processing (adjusted beta coefficient of z-score − 0.02, p-value 0.006), memory (− 0.03, 0.014), and G-factor (− 0.11, 0.014) in full-model. Stratified analysis by age group showed significant adverse effects of OSA symptoms on cognition for middle-aged people (50–60 years) (− 0.26, 0.001), but not in later age groups. Poor sleep quality was also associated with lower cognitive scores for G-factor (− 0.48, < 0.001), memory (− 0.08, 0.005), and executive domains (− 0.12, < 0.001), but not with information domain.
Conclusion
The findings suggest that both symptoms of OSA and poor sleep quality have a direct adverse impact on cognition in an Indian setting. A modest effect of age on the relationship of OSA and cognition was also observed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cognitive impairment is characterized by a decline in cognitive abilities including memory loss, difficulty learning new information, and decreased focus [1]. This decline can range from mild cognitive impairment to dementia. Cognitive impairment among elderly individuals negatively affects their quality of life, becomes a cause of their disability and dependence, and heightens risk of mortality [2]. As the global population is aging, the individual and societal burden of cognitive impairment among the elderly is becoming increasingly apparent.
The global prevalence of cognitive impairment among those over the age of 50 ranges from 5 to 41%, with a median of 19% [3]. Cognitive impairment in the elderly population is caused by a variety of risk factors, including hypertension, type 2 diabetes mellitus, coronary artery disease, dyslipidemia, obesity, and stroke [4,5,6]. Recent research has identified sleep-disordered breathing and poor sleep quality as additional modifiable risk factors of cognitive impairment [7,8,9,10,11].
Obstructive sleep apnea (OSA) is a condition characterized by the sudden collapse of the airway during sleep, leading to apneic episodes and repetitive arousals [12]. Symptoms of OSA include snoring and daytime sleepiness. The prevalence of OSA varies globally, with rates ranging from 6.5 to 17% in women and 17 to 34% in men [13, 14]. Studies have shown that individuals with OSA symptoms are more likely to develop impairments in attention, memory, executive functioning, and general intellectual functioning [8, 15,16,17,18]. These individuals also have a higher risk of developing mild cognitive impairment (MCI) and dementia. The underlying mechanisms are thought to be hypoxemia and sleep fragmentation [19]. Importantly, continuous positive airway pressure (CPAP) treatment can reverse some of the cognitive deficits associated with OSA, highlighting the importance of early identification and treatment of OSA in individuals [15]. There are also challenges associated with using self-reported screening questionnaires to identify individuals at risk of OSA, due to low specificity across OSA screening questionnaires [20].
Disturbed sleep, insomnia, or lack of sleep have also been associated with an increased risk of cognitive impairment and dementia [4,5,6, 9, 10]. In particular, poor self-reported sleep quality leads to cognitive impairment [7]. A meta-analysis has found that compared to middle ranges of sleep duration, both shorter and longer sleep duration can affect verbal memory, verbal fluency, and working memory [11].
In India, almost one in ten (over 139 million) people belong to the elderly age group (60 years or older) in whom high prevalence of chronic diseases, depression, and anxiety constitute a major public health challenge [21,22,23]. Population-based studies from India among the general population have reported prevalence estimates of OSA as 8.7% in rural [24], and 9.3% in urban areas [25], and that of poor sleep quality at 16% [26]. Studies from India that reported determinants of cognition have not specifically assessed if OSA symptoms or poor sleep quality is indeed independently associated with cognitive impairment [27,28,29,30]. Previous studies adjusted for only a limited set of covariates, for example, the Study on Global Ageing and Adult Health (SAGE) was conducted in six middle-income countries, of which India was one, and had adjusted for age, sex, and education [31]. Furthermore, limited assessment of the outcome variable of cognitive deficit in previous studies posed a challenge in appropriate interpretation. Instead of using the recommended battery of neuropsychological tests, the assessment of cognition in previous studies from India was performed using Mini-Mental State Examination (MMSE) screening method [28, 30] or MMSE followed by evaluation by DSM-IV criteria [29].
Thus, there was a need to assess the independent association of OSA symptoms and poor sleep quality with cognition that is adjusted for potential confounders, and in which the outcome measures have been appropriately assessed. The population-based LoCARPoN study of 7505 persons aged 50 years and above in India provided this unique opportunity to assess the following research questions: Are OSA symptoms associated independently with cognition? Is poor sleep quality associated independently with cognition when conditioned on OSA symptoms and other covariates? Additionally, we attempted to assess if the above associations would vary by age to explore possible effect modification by age.
Methods
Study population
We analyzed data from the baseline survey of the Longitudinal Cognition and Aging Research on Population of the National Capital Region—LoCARPoN (in Hindi means “dedication-to-people”) study. Detailed information on the LoCARPoN cohort profile is available [32]. In brief, LoCARPoN was a population-based cohort of middle-aged and older adults in New Delhi, India, that aimed to study India-specific risk factors for the incidence of stroke, dementia, and mental illness. Between the years 2016 and 2019, 8858 participants aged 50 years or older consented and were enrolled from two areas in South Delhi through household visits. A total of 7505 individuals attended the study center for in-person assessments including cognitive testing and cardiovascular examinations, and provided blood specimens for estimates of blood glucose and lipid profile. The MMSE (Hindi version) was used as a cognitive screening tool. Individuals with MMSE scores less than 26 (n = 710) were excluded, resulting in data of 6795 individuals for the present study (details in statistical analysis). The LoCARPoN study was approved by the Institutional Ethics Committee of All India Institute of Medical Sciences, New Delhi, India (reference number: IEC/NP-53/2014 RP-12/2014). Written informed consent was obtained from individual participants.
Outcome assessment
Several measures of cognition were assessed using a battery of neuropsychological tests at the research center by a clinical psychologist, and MMSE was performed as a screening tool. We constructed an overall measure of cognition as a general cognitive factor (G-factor) based on six cognitive tests: immediate recall, delayed recall, Purdue pegboard test-right hand, color trail test-B, digit span forward, and animal naming test. These tests assessed the following three cognitive domains: information processing, memory, and executive functioning. A principal component analysis was applied to the scores of the 6 cognitive tasks to derive a G-factor. For tests with multiple subtasks (Purdue pegboard test, color trail test-B, digit span forward), only one subtask was selected to prevent highly correlated tasks from distorting the factor loadings. The first rotated principal component accounted for 42.0% of the total test variance. Loadings on the principal components were as follows: immediate recall = 0.81, delayed recall = 0.81, Purdue pegboard test-right hand = 0.56, color trail test-B = − 0.51, digit span forward = 0.49, and animal naming test = 0.64. Other studies have reported that the G-factor explains 42.9 to 52.7% of the variance, which was consistent with our findings [33].
Exposure assessment
The OSA symptoms were determined using the Hindi version of the Berlin Questionnaire (BQ) [34]. The questionnaire comprises nine questions where five assess symptoms of snoring (category 1), three assess symptoms of sleepiness (category 2), and one assesses either hypertension or BMI ≥ 30 kg/m2 (category 3). Based on the summed scores (possible range 0 through 3), an individual was classified for the OSA symptoms as follows: “ ≥ 2” (high risk), “1” (low risk), and “0” (no risk).
Sleep quality characteristics were assessed using the Hindi version of the Pittsburgh Sleep Quality Index (PSQI) [35], a self-reported questionnaire consisting of 19 items grouped into seven components: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medication, and any daytime dysfunction. Each component score ranges from 0 to 3 (higher is worse). The responses are summed to derive the total score (global PSQI score); a participant with a global PSQI score “greater than 5” was categorized as having poor sleep quality. Sleep medication was defined as the reported use of any prescribed or “over-the-counter” medication to aid sleep at least once a week (yes/no). Sleep latency was defined as the duration it has taken to fall asleep each night, in the past 1 month (in minutes). Sleep duration (in hours) was self-reported, as hours of actual sleep that the person got at night. Total time in bed (hours) was calculated as the difference between bedtime and wake time in hours. Habitual sleep efficiency (HSE) (in percentage) was calculated as (Sleep duration/Total time in bed × 100). The scoring was ≥ 85 (score 0), 75– < 85 (score 1), 65– < 75 (score 2), and < 65 (score 3); where 0 is good, and 3 is poor. Since sleep duration and total time in bed were assessed separately, implausible values between 100 and 110% were recorded to 100%. Daytime dysfunction was scored if the participant endorsed any of the following: trouble staying awake while driving, eating meals, or engaging in social activity at least once a week, or a problem in keeping up enough enthusiasm to get things done.
Confounders
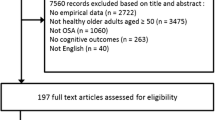
Both OSA symptoms and sleep quality are associated with socio-demographic characteristics and with a multitude of metabolic risk factors, lifestyle factors, and psychosocial problems. We selected confounders based on the directed acyclic graph (DAG) (Fig. 1).
Using pre-tested structured questionnaires, face-to-face interview with participants was conducted to collect information on socio-demographic characteristics and lifestyle factors. Socio-demographic characteristics included information on age, sex, and education (defined as completed years of schooling, used as a continuous variable). Lifestyle factors included alcohol intake (as ever took alcohol) and physical activity (assessed using the International Physical Activity Questionnaire (IPAQ), and categorized as mild, moderate, and high levels of physical activity). The IPAQ facilitates surveillance of physical activity based on global standard, and is a widely used questionnaire for such purposes [36]. We used the Hindi version of the IPAQ.
Metabolic factors included fasting glucose, total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), glycated hemoglobin, and the cardiovascular risk factors, i.e., blood pressure (BP) and body mass index (BMI). The cutoffs for BMI (in kg/m2) were set as underweight (< 18.5), normal (18.5 to < 25), pre-obese(25–30), and obese (> 30), according to the World Health Organization [37]. Overnight fasting blood specimens were used to estimate fasting blood glucose, HDL, LDL, and total cholesterol using Erba XL-640 Biochemistry Analyser. Glycated hemoglobin (HbA1C) was measured on the same blood specimen using the high-performance liquid chromatography (HPLC) method in a Biorad D-10-HbA1c Analyser. Dyslipidemia for each measure of lipid profile was defined as total cholesterol ≥ 200 mg/dL, LDL ≥ 130 mg/dL, and HDL ≤ 60 mg/dL. These cutoffs were based on the National Cholesterol Education Program guidelines, which also recommended that an ideal HDL level should be between 40 and 60 mg/dL [38].
Diabetes mellitus was defined as HbA1c ≥ 6.5% (as per the American Diabetic Association- ADA International Expert Committee report) [39], or currently on medication for diabetes mellitus. High blood pressure was defined as either systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg (following recent recommendations [40]) or currently on medication for hypertension. Using an electronic blood pressure instrument, BP was measured on the right arm, 5 min apart. A mean of three readings was used to calculate SBP and DBP. Medication for diabetes mellitus and high blood pressure was self-reported. Sleep medication was defined as the reported use of any prescribed or “over the counter” medication to aid sleep, during the past month. The information was collected as never, less than once a week, once or twice a week, three or more times a week. We recorded sleep medication as never use or any use in past month. Anthropometric measures included body weight and height. Weight was recorded in kilograms by a digital weighing machine, using standing scales supported on a steady surface. Height was measured without shoes, in centimeters, with a stadiometer with the head in the Frankfurt plane positioned at a 90° angle against a metallic metric tape measure mounted on a wall.
Psychosocial problems: Symptoms of depression, based on the scores of 30-item geriatric depression scale, were categorized into normal (< 10), mild (10 to < 20), and moderate to severe (20 to 30) [41]. Symptoms of anxiety, based on the 11-item ACS anxiety scale, were categorized into normal (< 2), mild (2 to 5), and moderate to severe (6 to 11) [42].
Statistical analysis
We first presented a descriptive analysis (for n = 6795) of participants’ socio-demographic characteristics, exposure, outcome, and confounder variables as frequencies and percentages for categorical variables, or as mean (S.D.) for continuous variables. All 4 cognitive outcome measures, i.e., G-factor, information processing speed, memory, and executive functions were converted into z-scores. An association of socio-demographic, lifestyle, and metabolic factors with cognition using univariable linear regression models, adjusted for age and sex, is presented. We separately deployed a series of models for each outcome. In model 1, we assessed the association of OSA symptoms with cognitive measures, adjusted for age and sex, using linear regression. Model 2 was additionally adjusted for education, alcohol, and physical activity. Model 3 was model 2 plus the interaction term of OSA with age, where age was entered as a continuous variable. After assessing the significance of the interaction term, we re-ran the full model (model 2) in four strata of decadal age groups: 50–59 years, 60–69 years, 70–79 years, and ≥ 80 years to undertake the stratified analysis. We did not adjust for BMI or hypertension in the above models since they were used in defining the exposure (OSA symptoms).
To assess the independent association of poor sleep quality with the four measures of cognition, the above analyses were repeated with poor sleep quality as the exposure variable. Model 2 was adjusted for age, sex, education, alcohol, physical activity, symptoms of depression, symptoms of anxiety, diabetes mellitus, high blood pressure, body mass index, high-density lipoprotein (≤ 60 mg/dL), OSA symptoms, and interaction term of OSA with age, (both as continuous variables), and stroke history (yes/no). The presence of OSA can significantly impact sleep quality; hence, we statistically adjusted for that in the full model. We had controlled for the history of stroke using statistical adjustment. We used the variable hypertension as a measure of stroke risk. Since hypertension was a component of the scoring method for evaluating OSA symptoms, we could not evaluate hypertension as a covariate in the model assessing the association of OSA symptoms with cognition. Model 3 was model 2 plus the interaction term of PSQI with age (both as continuous variables). Associations with p < 0.05 were considered statistically significant in multivariable analysis. All analyses were performed in R.
Several sensitivity analyses were undertaken to (a) assess the effect of adding diabetes mellitus type 2 as a covariate in model 2, model 3, and the age-stratified analysis of the association between OSA symptom and cognition; (b) assess the interaction of sex with OSA symptoms by adding an interaction term with sex in model 3; (c) assess the interaction of sex with PSQI by adding an interaction term with sex in model 3; and (d) assess the effect of adding sleep medication as a covariate in model 2, model 3, and the age-stratified analysis of the association between sleep quality and cognition. We note that this likely constitutes overadjustment for a possible mediator unless sleep medication is seen more as an antecedent and not a consequence of sleep problems.
Missing data: We performed multiple imputations using chained equations to impute missing covariates with plausible values, so as to avoid reducing the number of observations in the analysis. We did not impute the G-factor. We used the mice package in R for multiple imputation using chained equation [43]. Predictive mean matching, logistic regression, and multinomial logit models were considered to impute missing values for continuous, binary, and categorical variables respectively, before considering a random sample from the imputed data. Glycated hemoglobin had the most missing values (22.5%), while other missing covariate values did not exceed 2%.
Results
Demographic characteristics of study population
After excluding participants having an MMSE score < 26 (n = 710), we analyzed data of 6795 individuals, mean (SD) age 64.2 (9.0) years, years of schooling 15.5 (3.3) years, 49.2% women. A total of 2530 (38.3%) participants were at high risk of OSA symptoms, while the prevalence of poor sleep quality was 15.9%. Almost half of all the participants (55.2%) had high blood pressure, while 38.4% had diabetes mellitus (HbA1C > 6.5 or on medication). More than half of all the participants (61.7%) had serum HDL ≤ 60gm/dL, while 28.8% had serum cholesterol ≥ 200 mg/dL. Other socio-demographic characteristics and comorbidity patterns are given in Table 1. An association of socio-demographic, lifestyle, and metabolic factors with cognition using univariable linear regression models adjusted for age and sex is presented in Supplementary Table S1.
OSA and cognition
More severe OSA symptoms, adjusted for age and sex, were negatively related to z-scores of G-factor and the cognitive domains of information processing speed and memory (Table 2). This pattern of association persisted in a fully adjusted model. More severe OSA symptoms were significantly negatively associated with the G-factor (adjusted beta coefficient of z-score − 0.11, 0.014), and the cognitive domains of information processing speed (− 0.02, p-value 0.006), and memory (− 0.03, 0.014) in the full model. However, OSA symptom was not associated with executive function in any model.
The interaction term of OSA with age was significant for the domain of information processing speed (0.002, p-value = 0.022) in model 3, but neither for the G-factor nor for the rest of the cognitive domains. Stratified analysis by age group revealed significant adverse effects of OSA symptoms on G-factor (− 0.26, 0.001), information processing (− 0.04, 0.003), and memory (− 0.07, 0.004), but restricted only to middle-aged people (50–60 years). In the later age groups, none of the associations were significant. This suggested a possibility of a trend for an effect modification by age in the association of OSA symptoms with cognition.
Since OSA and diabetes mellitus share a bidirectional relationship, we had undertaken a sensitivity analysis by adding diabetes mellitus to the full model. The association of OSA symptom with G-factor was no longer significant, though OSA remained associated with information and memory domains of cognition (Supplementary Table S2). Sensitivity analysis showed no additional modification by sex, in the association of OSA symptoms with cognition (Supplementary Table S3).
Sleep quality and cognition
Poor sleep quality, adjusted for age and sex, was negatively related to the z-scores of the G-factor and the cognitive domains of information processing speed and memory as well as executive function (Table 3). This pattern of association persisted in a fully adjusted model except for the domain of information processing. Poor sleep quality was significantly negatively associated with cognitive domains of G-factor (adjusted beta coefficient of z-score − 0.45, p-value < 0.001), memory (− 0.07, 0.01), and executive function (− 0.12, < 0.001) in the full model.
In model 3, the interaction term of PSQI with age was significant only for the G-factor (− 0.003, p-value = 0.015). Stratified analysis by age group revealed there was an adverse effect of poor sleep quality on G-factor, and executive function for successive age groups of 50–59 years, 60–69 years, and 70–79 years. However, there was no discernible trend of this association by age suggesting thereby absence of effect modification by age in the association of sleep quality with cognition. Sensitivity analysis showed no additional modification by sex, in the association of poor sleep quality with cognition (Supplementary Table S3). Sensitivity analysis to assess the effect of sleep medication showed no changes in model 2, and model 3. However, in stratified analysis, the association of sleep quality with the executive domain was no longer significant in the age group 60 years and above. (Supplementary Table S6). Also, in stratified analysis, the association of sleep quality with G-factor was no longer significant, in the age group 70 years and above, but the significant effect was sustained in the age group 60–69 years (Supplementary Table S6).
Discussion
We report three salient findings in this study: (i) among the middle-aged and elderly urban population of India, the presence of more severe symptoms of OSA independently adversely affected the general cognitive G-factor, as well as the cognitive domains of information processing speed and memory; (ii) having a poorer sleep quality in this population made the participants more vulnerable to cognitive impairments in the domains of memory and executive function as well as the G-factor; (iii) stratified analysis suggested the possibility of effect modification by age in the association of OSA symptoms with cognition, which however, requires further exploration.
This investigation is the only large-scale population-based study from India exploring the association of OSA and cognition while adjusting for a range of covariates that could potentially confound this association. Similarly, our study is also one among few exploring the association of poor sleep quality with cognition by considering OSA symptoms as a confounder, along with a comprehensive list of covariates. The current study highlighted the the role of OSA and poor sleep quality as independent modifiable risk factors for cognitive deficits among the elderly in India.
Our study fills a gap since an understanding of the effects of OSA and poor sleep quality on cognition is lacking in the South Asian population. Moreover, establishing an association independent of the many contributing factors that might exacerbate cognitive deficits in individuals with OSA and poor sleep quality was a critical limitation of previous studies. These factors include comorbid conditions or lifestyle factors. We measured covariates spanning socio-demographic and metabolic as well as psychologic factors. The large sample size in our study allowed us to accommodate these variables in regression models. Another issue was the lack of accurate measurement of cognitive status since many previous studies have relied on MMSE as the only cognitive marker. We used a standardized set of neuropsychological battery of tests to evaluate cognitive function, and also derived a statistical common cognitive factor, the G-factor, thereby improving on the accuracy of the outcome measure.
Previous studies from India reporting determinants of cognition have not determined the independent effects of OSA symptoms and sleep quality on cognition, and unlike ours, only a few covariates were adjustments [28,29,30] [31]. Our study took into account the potential metabolic and lifestyle factors in addition to demographic factors. Another major limitation in previous studies from India (except [31]) was the method of assessment of the cognitive deficit. Instead of a standard battery of neuropsychological tests, studies defined them variously, e.g., MMSE < 25 [30], MMSE < 24 [28], or MMSE < 23 plus DSM-IV [29]. Being only a screening method, MMSE is not a valid measure of cognitive deficit. Moreover, using MMSE did not allow such studies to assess specific cognitive domains. Wave 1 of the WHO-SAGE study conducted in six middle-income countries including India used a composite z-score based on five cognitive tests namely, immediate and delayed verbal recall, forward and backward digit span, and verbal fluency [31]. Our study immensely improved the quality of the outcome measure by using an extensive battery of neuropsychological tests, allowing us to study the three domains of information, memory, and executive functions in detail, unlike the limitation in the WHO-SAGE study.
Association of OSA with cognition
Our findings support the association between OSA and cognitive decline seen in studies from high-income and middle-low-income countries. A previous meta-analysis of prospective studies showed a 26% increased risk of cognitive impairment among those with OSA [8]. In line with the meta-analysis [8] and others [18], the negative association between OSA symptoms and cognition in our study was prominent for the G-factor, and the domains of information processing speed and memory. However, unlike other studies, we did not find an association with executive function [8, 18]. This difference could be due to multiple reasons, e.g., not all studies might be examining the same cognitive domains, or using different measures for a given domain. The latter is especially pertinent to executive function assessment which measures the complex operations of reasoning and problem-solving that would involve the coordination of multiple sensory, perceptual, and attentional components; some of these components than others are reportedly affected more by OSA [18, 44]. Hence, a cautious approach is warranted while interpreting the absence of association with executive function.
The periodic interruption in a person’s breathing causes periods of hypoxia, which in turn can lead to several pathologic changes in the cerebral microvascular and neurovascular systems, including decreased blood flow (hypoperfusion), decreased function of the inner lining of blood vessels (endothelial dysfunction), and an increase in inflammation in the nervous system (neuroinflammation). The resulting oxidative stress and inflammation can result in damage to the brain tissues, and changes in brain structure, leading to a range of cognitive problems [45] and the domains of vigilance, attention, reaction time, executive function, problem-solving, verbal recall, non-verbal recall, and episodic memory are particularly implicated therein. OSA is highly prevalent in patients with Alzheimer’s disease. By treating OSA and preventing these episodes of hypoxia, it may be possible to reduce the risk of developing early cognitive deficits and preserve cognitive and cardiovascular health. The symptoms of OSA, being a modifiable risk factor for the prevention of cognitive deficits, hence must be prioritized in a public health approach.
Differential effect of age in the association of OSA with cognition
The interaction term of age with OSA symptoms in our study was significant for the information domain, while the stratified analysis by age group showed significant adverse effects of OSA on cognition in persons aged 50–60 years. A similar finding was reported in the Reasons for Geographic And Racial Differences in Stroke (REGARDS) Study that assessed 2925 stroke-free individuals, aged between 47 and 93 years. In this study, individuals with a high risk of OSA in middle ages scored relatively lower than controls on executive functions than older persons with OSA compared to respective controls, indicating a significant OSA-age interaction, with negative effects on cognition attenuating after age 70 [46]. Two more studies demonstrated the age-dependency of the relation between OSA symptoms and cognitive impairment; they support the finding that middle age seems more crucial for cognitive impairment for individuals with OSA [47]. These studies compared individuals with OSA with controls, in both middle-aged and younger individuals. A small study of 99 patients reported a significant deterioration of cognitive attention alertness in middle-aged patients [48]. Another study found a reduced performance for immediate word recall and slower reaction time during sustained attention among middle-aged patients with OSA. Symptoms of OSA symptoms in middle-aged adults could provide a promising window of opportunity for an earlier intervention. However, a better characterization of the age-dependent association of OSA with cognition in different populations is necessary.
Alternate reason for association OSA with cognition in middle age in India
Although we did observe the association of OSA symptoms with cognition to be most pronounced in the middle ages, and which is in fact well in accordance with the literature [46,47,48], the observed association in the Indian setting could also be an effect of survival effect, since the pressure of high prevalence of co-morbidities (e.g., prevalence of diabetes mellitus or hypertension) in this age group and mortality can make this process much quicker in the India setting. Another possible explanation might be in the competing risks; the individuals in our study who potentially could have developed a cognitive deficit at later ages might have had already died with the advancing age cohorts, as per the life expectancy of India. This could lead to selection by higher mortality, i.e., people who were still alive at an advanced age were actually those who were relatively healthier, and thereby harboring a lower probability of developing a cognitive deficit at that age. This facet is more important for middle-income countries where the average life expectancy is 71 years (2020, World Bank, https://data.worldbank.org/indicator/SP.DYN.LE00.IN). The average life expectancy of an Indian is 70 years. Hence, elderly individuals who are alive beyond that age in India are different from their original birth cohort population, as a result of selection. This implies observations of a lack of significant association between OSA symptom and cognitive deficit for the advanced decadal age groups might be a function of inclusion in the study of healthier individuals who had a lesser probability of acquiring a cognitive deficit (Supplementary Tables S4 and S5).
Association of sleep quality with cognition
We found poor sleep quality to be associated with poorer z-scores of cognitive measures for the G-factor, as well as for the domains of information and executive function, in the full model. Like ours, most of the studies that assessed the association between sleep quality and cognition have been cross-sectional in design. With a cross-sectional design, our study cannot explain the direction of the observed associations between self-reported sleep quality and impaired cognition, although this direction was recently confirmed epidemiologically in a cohort study [49]. The Heinz Nixdorf Recall study, a population-based cohort study in Germany, reported that poor-quality sleep had a higher risk of incident cognitive impairment [49]. Various meta-analyses have also reported that poor sleep quality increases the risk of cognitive impairment [7], and all-cause dementia [10]. We however could not find studies from India addressing this question. Only wave 1 of the WHO-SAGE study conducted in six middle-income countries of India, also a part, found that those with moderate to high sleep quality had significantly better cognitive function. However, this study did not present the data separately for India. Moreover, unlike ours, they only adjusted for age, sex, and education while evaluating the impact of sleep quality on cognition [31].
Further support comes through evidence that poor sleep quality adversely impacts hippocampus-dependent memory consolidation [50]. We indeed found the memory domain of cognition being affected in this study. There are also reports that among older adults, inadequate sleep facilitates the accumulation of amyloid-β and cognitive decline [51]. Both short-duration sleep (≤ 6 h/night) and long-duration sleep (≥ 9 h/night) have been associated with worse cognitive outcomes [51]. It is still unclear whether certain cognitive functions are more impacted by extreme sleep duration, and if short and long sleep durations have different effects on the cognitive dysfunction in a particular domain. Persons with a short sleep duration performed worse in tests of memory, those with long sleep duration performed worse in an executive function task. In our study executive domain of cognition was also affected. The association of sleep quality with cognitive decline has also been linked through disruption of critical neurotrophins and neurogenesis [52], of sleep microarchitecture [53], and also of excessive daytime sleepiness [54].
Association of sleep quality with cognition independent of OSA symptoms
We have shown that the association of sleep quality and cognitive decline was independent of the OSA symptoms. There are limited studies that have teased out the effect of OSA symptom, while exploring the association of sleep quality with cognition in population-based studies. In line with our findings, Wang et al. [5] in a cross-sectional population-based (30,872) study from China reported that poor sleep quality negatively affected cognitive performance, even after adjusting for OSA symptoms They had defined OSA using the self-reported No-SAS (Neck Obesity Snoring Age Sex) scale, and sleep quality using PSQI, while cognitive status was assessed using only MMSE scores (< 24) [5]. An earlier cross-sectional study (N = 4157) based on the Heinz Nixdorf Recall Cohort, Germany, had emphasized the association between poor sleep quality and mild cognitive impairment, independent of OSA diagnosis [55]. Similar to our finding, the effect of poor sleep quality on cognition did not appear to vary by age group in those studies. The Cambridge Centre for Ageing and Neuroscience cohort (N = 2406) confirmed the adverse effect of poor sleep quality on cognition and also reported an absence of interaction between sleep quality and age for not only cognition, but also for other health outcomes [56].
We presented a cross-sectional association of OSA and poor sleep quality with cognition. Longitudinal studies are needed to better understand how OSA and poor sleep quality impact cognition over time. Second, there might be differences in how OSA, poor sleep quality, and cognitive impairment manifest in different age groups and between genders as implied by some prior authors. We explored these differentials in the age-stratified analyses. Third, our study has implications for public health intervention in terms of early identification and treatment. The findings of our study highlight the importance of identifying OSA and poor sleep quality among middle-aged adults, in whom a heightened risk of cognitive impairment was observed. This also paves the way to study if intervening early for OSA and/or poor sleep quality could indeed result in preventing cognitive decline in older adults.
Limitations and strengths
Several limitations must be acknowledged. We used the Berlin Questionnaire to assess the symptoms of OSA. While self-reported questionnaires such as the Berlin Questionnaire and the Epworth Sleepiness Scale are frequently used in population-based studies, due to inherent advantages, to identify individuals at high risk for OSAS, they suffer from low specificity for OSA leading to the possibility of false positives [20]. The large sample size would then improve the precision of the estimate which we believe brings confidence in the validity of the findings and its direction. Hence, the large number of participants in this study would have somewhat mitigated the effect of the lower diagnostic accuracy of the Berlin Questionnaire. Therefore, we believe that our estimate of the association of OSA with cognitive decline is likely to be valid. Future studies can further validate the findings using polysomnography-based diagnosis. There is a possibility that cardiovascular risk factors were differentially distributed among individuals with symptoms of OSA compared to those without those symptoms, which would have confounded the observed association between symptoms of OSA and the presence of cognitive impairment. We used a select set of metabolic and cardiovascular risk factors as covariates. Since hypertension and BMI were components of the scoring method, we could not evaluate them as covariates in the model assessing the association of OSA symptoms with cognition. A limitation remains due to the presence of residual confounding due to unmeasured or poorly measured cardiovascular factors. Future studies should attempt to include a comprehensive set of cardiovascular risk factors.
A cross-sectional study cannot determine the temporality of the association. A major advantage of our study was the sufficient number of individuals in each of the decadal age groups. Many previous studies that studied the age interaction and reported equivocal effect had used a cutoff at 50 years, perhaps due to the insufficient number of participants in separate age groups. Therefore, the previous studies may have missed the age-modifying effect that were averaged out due to the aggregation of individuals older than 50 years. Due to the sufficient number of individuals in each age group, we were able to evaluate effect modification by age. Due to adequate sample size, the study had the statistical power to perform simultaneous adjustment of many potential confounders. We did not adjust for the use of sleep medication in our study, as only 3.7% of the individuals reported a history of its usage, potentially limiting the model’s generalizability to this subgroup.
A strength of the study was that the participants were recruited from a population base of healthy adults. All data were collected in a uniform and standardized manner data. The demographic characteristics and often modest sample sizes of previous studies made the findings of those studies hard to generalize to healthy, community-dwelling populations.
Conclusion
The findings of the current study suggest that both symptoms of OSA and poor sleep quality may have a direct effect on cognition in the Indian population. There was a modest effect of age on this relationship, but further research is warranted about the effect on younger or older adults. The results have important implications for preventing dementia in middle-aged and older adults. Both OSA symptoms and poor sleep quality are modifiable risk factors that may be targeted for the prevention of cognitive deficit in middle-age and older adults. In the absence of awareness of OSA symptoms, its adverse effects, unwillingness to accept treatment, and dilemma among doctors on when/for whom to start treatment, many individuals who might benefit from treatment to possibly prevent neurodegeneration remain bereft.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
ICD-10. International Statistical Classification of Diseases and Related Health Problems 10th Revision. https://icd.who.int/browse10/2010/en#/F06.7. Accessed 7 Dec 2022
Park MH, Kwon DY, Jung JM et al (2013) Mini-Mental Status Examination as predictors of mortality in the elderly. Acta Psychiatr Scand 127:298–304. https://doi.org/10.1111/j.1600-0447.2012.01918.x
Pais R, Ruano L, Carvalho OP, Barros H (2020) Global cognitive impairment prevalence and incidence in community dwelling older adults—a systematic review. Geriatrics 5:84. https://doi.org/10.3390/geriatrics5040084
Yaffe K, Laffan AM, Harrison SL et al (2011) Sleep disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA J Am Med Assoc 306:613–619. https://doi.org/10.1001/jama.2011.1115
Wang Z, Heizhati M, Wang L et al (2022) Poor sleep quality is negatively associated with low cognitive performance in general population independent of self-reported sleep disordered breathing. BMC Public Health 22:3. https://doi.org/10.1186/s12889-021-12417-w
Brzecka A, Madetko N, Nikolenko VN et al (2021) Sleep disturbances and cognitive impairment in the course of type 2 diabetes-a possible link. Curr Neuropharmacol 19:78–91. https://doi.org/10.2174/1570159X18666200309101750
Bubu OM, Brannick M, Mortimer J, Umasabor-Bubu O, Sebastião YV, Wen Y, Schwartz S, Borenstein AR, Wu Y, Morgan D, Anderson WM (2017) Sleep, cognitive impairment, and Alzheimer’s disease: a systematic review and meta-analysis. Sleep 40(1). https://doi.org/10.1093/sleep/zsw032
Leng Y, McEvoy CT, Allen IE, Yaffe K (2017) Association of sleep-disordered breathing with cognitive function and risk of cognitive impairment: a systematic review and meta-analysis. JAMA Neurol 74:1237–1245. https://doi.org/10.1001/jamaneurol.2017.2180
Benedict C, Byberg L, Cedernaes J et al (2015) Self-reported sleep disturbance is associated with Alzheimer’s disease risk in men. Alzheimers Dement J Alzheimers Assoc 11:1090–1097. https://doi.org/10.1016/j.jalz.2014.08.104
Shi L, Chen S-J, Ma M-Y et al (2018) Sleep disturbances increase the risk of dementia: a systematic review and meta-analysis. Sleep Med Rev 40:4–16. https://doi.org/10.1016/j.smrv.2017.06.010
Bastien CH, Fortier-Brochu E, Rioux I et al (2003) Cognitive performance and sleep quality in the elderly suffering from chronic insomnia. Relationship between objective and subjective measures. J Psychosom Res 54:39–49. https://doi.org/10.1016/s0022-3999(02)00544-5
Young T, Hutton R, Finn L et al (1996) The gender bias in sleep apnea diagnosis: are women missed because they have different symptoms? Arch Intern Med 156:2445–2451. https://doi.org/10.1001/archinte.1996.00440200055007
Heinzer R, Vat S, Marques-Vidal P et al (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3:310–318. https://doi.org/10.1016/S2213-2600(15)00043-0
Peppard PE, Young T, Barnet JH et al (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014. https://doi.org/10.1093/aje/kws342
Lal C, Ayappa I, Ayas N et al (2022) The link between obstructive sleep apnea and neurocognitive impairment: an official American Thoracic Society workshop report. Ann Am Thorac Soc 19:1245–1256. https://doi.org/10.1513/AnnalsATS.202205-380ST
Sateia MJ (2003) Neuropsychological impairment and quality of life in obstructive sleep apnea. Clin Chest Med 24:249–259. https://doi.org/10.1016/s0272-5231(03)00014-5
Bubu OM, Andrade AG, Umasabor-Bubu OQ et al (2020) Obstructive sleep apnea, cognition and Alzheimer’s disease: a systematic review integrating three decades of multidisciplinary research. Sleep Med Rev 50:101250. https://doi.org/10.1016/j.smrv.2019.101250
Beebe DW, Groesz L, Wells C et al (2003) The neuropsychological effects of obstructive sleep apnea: a meta-analysis of norm-referenced and case-controlled data. Sleep 26:298–307. https://doi.org/10.1093/sleep/26.3.298
Abbasi A, Gupta SS, Sabharwal N et al (2021) A comprehensive review of obstructive sleep apnea. Sleep Sci 14:142–154. https://doi.org/10.5935/1984-0063.20200056
Bernhardt L, Brady EM, Freeman SC et al (2022) Diagnostic accuracy of screening questionnaires for obstructive sleep apnoea in adults in different clinical cohorts: a systematic review and meta-analysis. Sleep Breath Schlaf Atm 26:1053–1078. https://doi.org/10.1007/s11325-021-02450-9
Jana A, Chattopadhyay A (2022) Prevalence and potential determinants of chronic disease among elderly in India: rural-urban perspectives. PLoS ONE 17:e0264937. https://doi.org/10.1371/journal.pone.0264937
Sinha P, Hussain T, Boora NK et al (2021) Prevalence of common mental disorders in older adults: results from the National Mental Health Survey of India. Asian J Psychiatry 55:102463. https://doi.org/10.1016/j.ajp.2020.102463
Sahni B, Bala K, Kumar T, Narangyal A (2020) Prevalence and determinants of geriatric depression in North India: a cross-sectional study. J Fam Med Prim Care 9:2332–2336. https://doi.org/10.4103/jfmpc.jfmpc_357_20
Pinto AM, Devaraj U, Ramachandran P et al (2018) Obstructive sleep apnea in a rural population in South India: feasibility of health care workers to administer level III sleep study. Lung India Off Organ Indian Chest Soc 35:301–306. https://doi.org/10.4103/lungindia.lungindia_433_17
Reddy EV, Kadhiravan T, Mishra HK et al (2009) Prevalence and risk factors of obstructive sleep apnea among middle-aged urban Indians: a community-based study. Sleep Med 10:913–918. https://doi.org/10.1016/j.sleep.2008.08.011
Haldar P, Prasad K, Kant S et al (2022) Metabolic risk factors and psychosocial problems independently explain poor sleep quality and obstructive sleep apnea symptoms among adults in urban India. Sleep Breath Schlaf Atm. https://doi.org/10.1007/s11325-022-02725-9
Tiwari SC, Tripathi RK, Kumar A et al (2014) Prevalence of psychiatric morbidity among urban elderlies: Lucknow elderly study. Indian J Psychiatry 56:154–160. https://doi.org/10.4103/0019-5545.130496
Konda PR, Sharma PK, Gandhi AR, Ganguly E (2018) Correlates of cognitive impairment among Indian urban elders. J Gerontol Geriatr Res 7:489. https://doi.org/10.4172/2167-7182.1000489
Shaji S, Bose S, Verghese A (2005) Prevalence of dementia in an urban population in Kerala, India. Br J Psychiatry J Ment Sci 186:136–140. https://doi.org/10.1192/bjp.186.2.136
Sengupta P, Benjamin AI, Singh Y, Grover A (2014) Prevalence and correlates of cognitive impairment in a north Indian elderly population. WHO South-East Asia J Public Health 3:135–143. https://doi.org/10.4103/2224-3151.206729
Gildner TE, Liebert MA, Kowal P et al (2014) Associations between sleep duration, sleep quality, and cognitive test performance among older adults from six middle income countries: results from the Study on Global Ageing and Adult Health (SAGE). J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med 10:613–621. https://doi.org/10.5664/jcsm.3782
Prasad K, Dwivedi SN, Kant S et al (2022) Cohort profile: the LoCARPoN-a population-based prospective cohort study in middle-aged and older adults in India. Int J Epidemiol 51:29–30m. https://doi.org/10.1093/ije/dyab078
Hilal S, Tan CS, Adams HHH et al (2018) Enlarged perivascular spaces and cognition. Neurology 91:e832–e842. https://doi.org/10.1212/WNL.0000000000006079
Netzer NC, Stoohs RA, Netzer CM et al (1999) Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131:485–491. https://doi.org/10.7326/0003-4819-131-7-199910050-00002
Mollayeva T, Thurairajah P, Burton K et al (2016) The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev 25:52–73. https://doi.org/10.1016/j.smrv.2015.01.009
Craig CL, Marshall AL, Sjöström M et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35:1381–1395. https://doi.org/10.1249/01.MSS.0000078924.61453.FB
WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet Lond Engl 363:157–163. https://doi.org/10.1016/S0140-6736(03)15268-3
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2001) Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285(19):2486–2497. https://doi.org/10.1001/jama.285.19.2486
International Expert Committee (2009) International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 32:1327–1334. https://doi.org/10.2337/dc09-9033
Chobanian AV, Bakris GL, Black HR et al (1979) (2003) Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertens Dallas Tex 42:1206–1252. https://doi.org/10.1161/01.HYP.0000107251.49515.c2
Yesavage JA, Brink TL, Rose TL et al (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49. https://doi.org/10.1016/0022-3956(82)90033-4
Yadav AK (2020) Designing and validation of evidence-based questionnaire in English and Hindi for a population-based cohort study in North India. PhD thesis. Department of Neurology. ll India Institute of Medical Sciences
van Buuren S, Groothuis-Oudshoorn K (2011) Mice: multivariate imputation by chained equations in R. J Stat Softw 45:1–67. https://doi.org/10.18637/jss.v045.i03
Harvey PD (2019) Domains of cognition and their assessment. Dialogues Clin Neurosci 21:227–237. https://doi.org/10.31887/DCNS.2019.21.3/pharvey
Kerner NA, Roose SP (2016) Obstructive sleep apnea is linked to depression and cognitive impairment: evidence and potential mechanisms. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry 24:496–508. https://doi.org/10.1016/j.jagp.2016.01.134
Addison-Brown KJ, Letter AJ, Yaggi K et al (2014) Age differences in the association of obstructive sleep apnea risk with cognition and quality of life. J Sleep Res 23:69–76. https://doi.org/10.1111/jsr.12086
Alchanatis M, Zias N, Deligiorgis N et al (2008) Comparison of cognitive performance among different age groups in patients with obstructive sleep apnea. Sleep Breath Schlaf Atm 12:17–24. https://doi.org/10.1007/s11325-007-0133-y
Ayalon L, Ancoli-Israel S, Drummond SPA (2010) Obstructive sleep apnea and age. Am J Respir Crit Care Med 182:413–419. https://doi.org/10.1164/rccm.200912-1805OC
Brachem C, Winkler A, Tebrügge S et al (2020) Associations between self-reported sleep characteristics and incident mild cognitive impairment: the Heinz Nixdorf Recall Cohort Study. Sci Rep 10:6542. https://doi.org/10.1038/s41598-020-63511-9
Sippel D, Schwabedal J, Snyder JC et al (2020) Disruption of NREM sleep and sleep-related spatial memory consolidation in mice lacking adult hippocampal neurogenesis. Sci Rep 10:16467. https://doi.org/10.1038/s41598-020-72362-3
Winer JR, Deters KD, Kennedy G et al (2021) Association of short and long sleep duration with amyloid-β burden and cognition in aging. JAMA Neurol 78:1187–1196. https://doi.org/10.1001/jamaneurol.2021.2876
Sportiche N, Suntsova N, Methippara M et al (2010) Sustained sleep fragmentation results in delayed changes in hippocampal-dependent cognitive function associated with reduced dentate gyrus neurogenesis. Neuroscience 170:247–258. https://doi.org/10.1016/j.neuroscience.2010.06.038
Pace-Schott EF, Germain A, Milad MR (2015) Effects of sleep on memory for conditioned fear and fear extinction. Psychol Bull 141:835–857. https://doi.org/10.1037/bul0000014
Jaussent I, Bouyer J, Ancelin M-L et al (2012) Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep 35:1201–1207. https://doi.org/10.5665/sleep.2070
Dlugaj M, Weinreich G, Weimar C et al (2014) Sleep-disordered breathing, sleep quality, and mild cognitive impairment in the general population. J Alzheimers Dis JAD 41:479–497. https://doi.org/10.3233/JAD-132132
Gadie A, Shafto M, Leng Y, Kievit RA (2017) How are age-related differences in sleep quality associated with health outcomes? An epidemiological investigation in a UK cohort of 2406 adults. BMJ Open 7:e014920. https://doi.org/10.1136/bmjopen-2016-014920
Funding
The LoCARPoN cohort study was funded by the Department of Biotechnology, Ministry of Science and Technology (grant number BT/IN/Netherland/03/KP/2012 dated 14/02/2014), and the Department of Health Research, Ministry of Health and Family Welfare, Government of India (grant number R.11012/15/2018-HR, dated 09/08/2018). Technical support and training were provided by the Department of Epidemiology, Erasmus University Medical Centre, the Netherlands. The Erasmus component was funded through the Erasmus Medical Centre, Rotterdam, the Netherlands, and the Erasmus University, Rotterdam. MAI and HT received further support from Alzheimer Nederland (WE.15–2014–09).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Ethics Committee of All India Institute of Medical Sciences, New Delhi, India (reference number: IEC/NP-53/2014 RP-12/2014), and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The LoCARPoN study was approved by the Institutional Ethics Committee of All India Institute of Medical Sciences, New Delhi, India (reference number: IEC/NP-53/2014 RP-12/2014).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haldar, P., Tripathi, M., Prasad, K. et al. Association of obstructive sleep apnea and sleep quality with cognitive function: a study of middle-aged and elderly persons in India. Sleep Breath 28, 975–987 (2024). https://doi.org/10.1007/s11325-023-02953-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02953-7