Abstract
The aim of this study was to evaluate the effect of obstructive sleep apnea syndrome on the cognitive performance of young and middle-aged patients. Patients were divided into two groups, one consisting of 30 patients less than 50 years of age and the other consisting of 28 patients 50 years and over. Normal subjects were similarly divided into two groups, composed of 17 younger and 24 older controls. Patients and controls were examined with all-night polysomnography and subsequently underwent cognitive testing via attention–alertness tests. Comparing young to middle-aged patients, there were statistically significant differences in cognitive performance, especially in attention tests. Younger patients’ cognitive performance was similar to their age-matched controls, while middle-aged patients showed cognitive decline in comparison with their age-matched controls. Although we studied only two age groups using 50 years of age as a cut-off, we could demonstrate that cognitive deterioration of untreated sleep apnea patients is age dependent, and several factors may contribute to this effect including brain hypoxia, sleep fragmentation, or comorbidities. Aging patients with sleep apnea demonstrate cognitive decline, while younger patients with the same disease severity are (somehow) able to compensate for this effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many manuscripts on the topic of sleep apnea syndrome begin with the following statement: “Four percent of adult men and 2% of adult women in general population random samples meet the clinical and polysomnographic criteria for the diagnosis of sleep apnea syndrome.” Until 1993, when Young et al. [1] wrote this article, sleep apnea prevalence was underestimated, and the syndrome was often misdiagnosed. Today, obstructive sleep apnea syndrome (OSAS) is a well-recognized disease entity with precise diagnostic criteria and well-described consequences.
It is quite difficult to identify when the syndrome begins and to determine the number of years a patient has been suffering from sleep apnea before a diagnosis is made. General population studies [2] would be required to detect the presence of early stage OSAS. The best we can do in daily clinical practice is to estimate the duration of disease by taking a detailed medical history. In general, patients seek medical help only when sleep apnea symptoms become severe enough to cause deterioration of normal daytime activities, or alternately when a bed partner recognizes the problem. Cognitive deterioration is one of the first signs leading a patient to seek help, and although cognitive decline might be a reversible phenomenon, other consequences may not be.
Many studies have investigated the cognitive consequences of untreated sleep apnea like excessive daytime sleepiness, impaired driving performance, decreased alertness, and attention deficits [3–8]. The vast majority of these studies have examined parameters that affect daily symptoms such as body mass index (BMI) [9], arousals, apnea hypopnea index (AHI) [10], minimum oxyhemoglobin saturation (minSaO2), mean oxyhemoglobin saturation (meanSaO2), minutes of oxyhemoglobin saturation below 90% per total sleep time (T < 90%), etc. Among them, age is a parameter that has been studied thoroughly. Using sleep disorders clinic criteria (AHI > 10 and daytime symptoms), the prevalence of sleep apnea changes with age increasing from 1% in young subjects to almost 5% in the middle-aged individuals [11]. When only laboratory criteria are used, the prevalence tends to increase monotonically with age [12]. Combining the observations above, sleep apnea seems to have an age-related severity with a peak at 55 years and age-dependent prevalence with a peak at 70 years [12, 13].
While severity, mortality, and cognitive performance of OSAS are well described in middle-aged [12, 14, 15] and elderly patients [16–18], there are not enough data to cover the transition from young to middle age. This study’s objective was to compare the daily consequences of OSAS in young and middle-aged individuals.
Materials and methods
Subjects
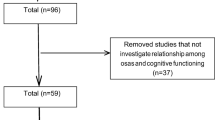
The study population consisted of patients with suspected sleep apnea syndrome, seen in an outpatient sleep clinic. Between October 2003 and June 2005, we approached 119 OSA patients and 81 healthy individuals to voluntarily participate in the study. Thirty four patients and 15 controls were excluded from the study according to the exclusion criteria listed below, and 27 patients and 25 controls declined to participate. Fifty-eight consecutive OSA patients and 41 controls were finally enrolled. Patients and controls were matched for age, ethnicity, gender, intelligence quotient (IQ), and years of education. Controls were questioned on medical issues/psychiatric illnesses and drug abuse. Inclusion criterion was the polysomnographic diagnosis of severe OSAS (AHI ≥ 30). Mild and moderate OSAS patients were excluded from the study to examine the major impact of sleep apnea on cognitive function. Other exclusion criteria were: subjects under medication (hypnotics, antidepressants, benzodiazepines) that could interfere with sleep and cognitive efficiency, those with depressive manifestations, cerebral insult, neurological disease, hypothyroidism, narcolepsy and daytime impairment of respiratory function (PO2 < 8 kPa and/or PCO2 > 6 kPa), alcohol or drug abuse, patients received no education, learning disabilities, age >65 years, insufficient total sleep time (<240 min), or no rapid eye movement (REM) sleep.
The mean age of our participants was near the age of 50 years. This age cut-off, which has been used in several similar studies [1–3, 12, 15, 19, 20], represented a dividing line to create a young age (30 patients, range 32 to 49 years) and a middle-aged patient group (28 patients, range 50 to 65 years). Controls were also divided with the same age criterion into two groups of 17 young and 24 older controls, respectively.
Study procedures
All patients and control subjects underwent a full-night diagnostic polysomnography (Embla, Flaga ht. Medical Devices, Iceland) with recordings of electroencephalogram (C4/A1, C3/A2), electrooculogram, chin electromyogram, electrocardiogram, oral and nasal flow (measured with thermistors), abdominal and thoracic movements (inductive plethysmography bands), oxyhemoglobin saturation, and snoring. For evaluation of subjective daytime sleepiness, all subjects answered the Epworth Sleepiness Scale (ESS) questionnaire [21]. The ethics committee of our institution approved the study, and all study patients and controls gave informed consent before their enrolment.
Cognitive evaluation took place on the day after the diagnosis of sleep apnea was made and before the second night of C-PAP titration. The cognitive functions evaluated included intellectual efficiency with Raven Progressive Matrices (RPM) IQ test, and attention–reaction time to visual and audio stimuli. Most of the attention tests are impaired in OSAS, and a single test could have underestimated impaired attention in some patients [3]. For that reason, we estimated attention with three different tests: selective attention (SA), permanent (or sustained) attention (PA), and target detection (TD) [22].
In our study, every patient and healthy individual underwent an attention/alertness battery test based on the Vienna Test System [22–24]. Cognitive testing was presented on a computer screen. After a tutorial lesson and a practice trial for each test, the final evaluation was performed.
Reaction time test to visual (RT-V) or acoustic (RT-A) stimuli
The subject places the forefinger on a detector, and when a colored flashlight appears in the center of the screen, the subject has to move the forefinger from the detector and push a matched-color button 10 cm ahead in the fastest possible way. Then the subject places the forefinger on the detector again, until the next flashlight appears. The series of flashlights are presented in a random way, and therefore, vary across trials minimizing the learning effect. The number of flashlights is 50, and the test lasts for approximately 15 min. Two parameters are recorded:
-
The period of time between the flash light and the moment the subject takes the forefinger away from the detector.
-
The period of time the subject takes to move the forefinger away from the detector and push the button ahead.
The sum of the two recorded times is called “reaction time to visual stimuli.” Reaction time test to acoustic stimuli is performed in a similar way, the only difference being that the flashlight is replaced by a sound presented to the subject via headphones. High and low frequency sounds are presented for 1 s and in random order so the subject has to push the predetermined high or low frequency buttons placed 10 cm ahead of the detector. The number of sounds is 30, and the test lasts for 8 min.
The results of the above tasks represented alertness.
SA test
The program presents four geometrical shapes on the top of a computer screen arranged in a horizontal row and asks from the subject to compare these shapes with a geometrical shape shown at the bottom of the screen. With every correct answer or after a fixed time interval, the next task follows automatically. At the beginning of the test, there is a maximum fixed time interval of 15 s between tasks. This gets shorter as the test continues and approaches a total time of 10 s, while the difficulty to find the right match increases (with more complex geometrical shapes). The number of tasks administrated is 80, and the duration of the test is approximately 20 min.
SA was also evaluated with TD test, where patients must identify within a presented picture specific predetermined objects and shapes [4].
PA test
This procedure is designed to examine the ability to perform multiple-choice reactions to quickly changing stimuli. The subject has to match several color figures presented on the computer screen with the corresponding color buttons on a keyboard, react to acoustic signs of high or low frequency by pushing predetermined corresponding buttons, and press foot pedals when the figure of a foot pedal appears on the screen. From the beginning to the end of the test, the period of time the subject has to match the figures and acoustic sign is progressively shortened. The total number of presented figures and sounds is 150, and the duration of the test is approximately 30 min.
Four parameters are recorded in both SA and PA tests:
-
Percentile of right answers
-
Percentile of wrong answers
-
Percentile of missed tasks
-
The total time spent for the completion of the test
According to the results of the tests, the subject is classified in a percentile of preexisting normal values of age-matched controls. Baseline data exist in adult populations from Europe and South Africa with different social-economic and educational levels, and with an age distribution of 18 to 65 years old [24].
Patients and control subjects were also evaluated according to intelligence with RPM test [25–27]. This widely applied nonverbal test evaluates the abstract–analytic reasoning of the subject using 60 items presented in five sets of increasing difficulty.
Data management and statistical analysis
We used SPSS statistical program (version 14) as a tool for our statistical analysis. Analysis of the collected data consisted of descriptive statistics followed by a simple t test (or Mann–Whitney test when normality failed) for sleep parameters and cognitive results. Most of our data did not follow a Gaussian distribution and failed normality tests; therefore, despite medium sample sizes, we performed nonparametric tests in most of the cases. We recognize that Mann–Whitney and other nonparametric tests work very well with large samples (more than 100), but they also can be a useful tool with medium-sized samples (around 30 in every group).
Before citing a number of tables and p values, we must explain the concept of our correlations between various parameters and different individual groups. We compared independent factors (polysomnography parameters, BMI, and age) with dependent factors (cognitive performance and ESS). We used multiple linear regression analysis and examined every dependent factor separately. We set the p value <0.05 as a limit for statistically significant findings.
Variance inflation factor (VIF), which measures the standard error of each regression parameter, was not above a value of 4 in any of our correlations (VIF must not exceed a value of 4 for the interaction to be reliable).
Results
Results are presented as the performance of patients and controls according to the specific cognitive tests used for their evaluation.
Table 1 summarized the general characteristics of all patients and controls, including their general sleep polysomnography results and cognitive testing. Patients combined as a single group demonstrated cognitive decline in comparison with normal subjects’ cognitive efficiency.
Attention tests revealed differences in performance between middle-aged and young age patient groups (Table 2). There were no statistically significant differences in reaction time tests between these groups.
Middle-aged patients had statistically significantly lower performance in attention tests not only in comparison with younger patients (Table 2) but also with their age-matched controls (Table 3). Reaction time tests also revealed statistically significant differences in performance between middle-aged patients and their age-matched controls. Reaction time test differences were of borderline statistical significance with p values under but near the threshold of 0.05.
Young patients performed quite well in attention tests (Table 2), as did their age-matched controls (Table 4). Young patients’ performance in attention and reaction time tests did not show statistically significant differences when compared to the performance of young controls.
We examined interactions between several sleep polysomnography paparements and attention–alertness tests in middle-aged and young patients. Middle age patients: We considered sleep polysomnography parameters, BMI, and age as independent factors, and by a multiple linear regression analysis, we examined interactions with attention tests. From the collected data, we found a positive linear correlation (Table 5) of meanSaO2 with attention tests (SA, PA, and TD).
Alertness (reaction time) tests were not correlated with meanSaO2 or other independent factors. There was also an expected finding of a negative linear correlation of age with attention–alertness tests.
Young patients
The same linear regression model was used to estimate interactions of independent factors (AHI, SaO2min/mean, T90, BMI, age) with attention–alertness tests as dependent factors. The analysis did not demonstrate any statistically significant interactions between independent and dependent factors. We found the same negative linear correlation (Table 6) of age with cognitive tests.
Controls
Both young and middle-aged controls demonstrated negative linear correlations of age with attention–alertness performance, but there was no correlation with other parameters.
Discussion
There is growing evidence [1, 12, 28] that age as a single parameter is somehow responsible for the severity of sleep apnea. Cross-sectional studies of prevalence do show an effect of age, independent of an increase in BMI with age. In our study, age was examined as an independent factor affecting cognitive performance of OSA patients, and these correlations were tested after controlling for BMI. We excluded subjects older than 65 years because cognitive deterioration with aging is a multifactorial process, and we could not consider OSA as the only contributing factor. Sleep changes in older people include a decline in REM sleep time, total sleep time, sleep efficiency, percentage of slow wave sleep, and there is an increase in sleep latency, increase in percentage of stage 1 and 2 sleep, and wake after sleep [29]. All the sleep changes listed above might have influenced cognitive testing.
We found statistically significant differences in cognitive performance between middle-aged patients and controls as well as between middle-aged patients and young patients. There were no such differences between young patients and controls.
The normal aging process could explain cognitive differences between young and middle-aged patients, but if only the aging process was the culprit, we should have detected cognitive differences between the control groups of different ages as well. However, young and middle-aged controls had similar, good performances in cognitive testing. We conclude that, in patients with sleep apnea, there are other factors besides aging affecting cognitive function. Significant cognitive differences could be the result of several factors, including brain damage due to sleep apnea hypoxic conditions for many years, or sleep fragmentation and/or comorbidities. Hypoxemia has already been studied as a predictive factor for cognitive impairment and excessive daytime sleepiness [6, 30–34]. Currently, there is no consensus as to whether sleep fragmentation or hypoxemia is a better predictive factor for cognitive performance. It seems that both factors contribute to these effects [33, 35, 36]. These factors can interfere with cognitive function and alter patient performance especially in aging patients.
Young patients exhibited cognitive performance comparable to the one achieved by their age-matched controls. This finding suggests that, at a young age, there is a compensation of the expected sleep apnea cognitive decline, or alternately, that cognitive tests are not sensitive enough to detect small changes in cognitive status. Regarding the fact that OSAS is a metabolic disease and hypoxic-metabolic changes take place from the beginning of the disease, we can hypothesize that young patients counterbalance these complications by mechanisms related to their young age like brain plasticity [37] or the nonexistence of comorbidities.
Correlations of hypoxia with cognitive impairment have been well described by many authors [6, 17, 30, 38]. Our study showed that meanSaO2 correlated positively only with the cognitive performance of middle-aged patients (a drop in oxyhemoglobin saturation corresponds to a drop in cognitive decline) and not with that of the younger patients despite all-night hypoxic conditions being similar between the two patient groups. We did not find significant correlations between minSaO2 or T < 90% and cognitive impairment. A literature review does not address the question of which of the oxyhemoglobin saturation parameters (meanSaO2, minSaO2, or T < 90%) best predicts cognitive function. Most of the studies use minSaO2 and T < 90% as predictive parameters of excessive daytime sleepiness and cognitive function [20, 23, 39]. Findley et al. [6] published results with a great correlation of meanSaO2 and cognitive impairment. Whether or not one is better than the other, we can assume that this varies according to patient population, presence or absence of co-morbidities, and disease severity. However, in our patient population (severe OSAS without serious comorbidities), meanSaO2 was better correlated with cognitive impairment.
Previously described increases in OSAS disease severity after age 55 [12] and age-related increases in mortality and morbidity after the age of 50 years [40, 41] combine with our findings of measurable cognitive decline over the age of 50 years. These observations suggest that OSAS patients are particularly in danger when they reach middle age. The consequences of this hypoxic-metabolic disease, especially the associated cardiovascular complications, contribute to increased morbidity and mortality, occurring mostly during middle age [14, 40, 41]. Measurable cognitive decline occurring at a relatively young age can be interpreted as an ominous sign of deterioration. Early detection of patients with OSAS and early treatment may prevent permanent consequences of the disease.
Limitations
Small number of participants is a limitation to this study. Perhaps a multicenter study might reveal with more accuracy the age effect on sleep apnea patients’ psychosocial level of functioning.
We only studied two age groups with 50 years of age as a dividing line, as insufficient data prevented us from examining what happens in other age groups. It is conceivable that major changes can occur when patients cross 60 years of age, or some other threshold, or perhaps the change is very gradual.
Another factor that might influence our results is the homogenous population of the participants, mainly citizens from Athens and high school graduates. The level of experience and education can play a role in cognitive test results, and have affected our data. A wider distribution of patients and controls would be more appropriate for better comparisons.
Conclusions
In this study, we have showed that cognitive decline appears and is detectable in aging OSA patients. This can be due to either a cumulative effect of the disease in middle age, after many years of existence, or to the fact that the aging brain is more sensitive to repeated episodes of oxyhemoglobin desaturation and sleep deprivation.
Younger patients have less comorbidity and are somehow able to compensate for the cognitive consequences of sleep deprivation and nocturnal hypoxia, perhaps through greater brain plasticity, thus showing normal brain function.
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Kim HC, Young T, Matthews CG, Weber SM, Woodward AR, Palta M (1997) Sleep-disordered breathing and neuropsychological deficits. A population-based study. Am J Respir Crit Care Med 156:1813–1819
Mazza S, Pepin JL, Naegele B, Plante J, Deschaux C, Levy P (2005) Most obstructive sleep apnoea patients exhibit vigilance and attention deficits on an extended battery of tests. Eur Respir J 25:75–80
Decary A, Rouleau I, Montplaisir J (2000) Cognitive deficits associated with sleep apnea syndrome: a proposed neuropsychological test battery. Sleep 23:369–381
Naegele B, Pepin JL, Levy P, Bonnet C, Pellat J, Feuerstein C (1998) Cognitive executive dysfunction in patients with obstructive sleep apnea syndrome (OSAS) after CPAP treatment. Sleep 21:392–397
Findley LJ, Barth JT, Powers DC, Wilhoit SC, Boyd DG, Suratt PM (1986) Cognitive impairment in patients with obstructive sleep apnea and associated hypoxemia. Chest 90:686–690
Findley L, Unverzagt M, Guchu R, Fabrizio M, Buckner J, Suratt P (1995) Vigilance and automobile accidents in patients with sleep apnea or narcolepsy. Chest 108:619–624
George CF, Nickerson PW, Hanly PJ, Millar TW, Kryger MH (1987) Sleep apnoea patients have more automobile accidents. Lancet 2:447
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, Kales A (2001) Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med 163:608–613
Harsch IA, Schahin SP, Radespiel-Troger M, Weintz O, Jahreiss H, Fuchs FS, Wiest GH, Hahn EG, Lohmann T, Konturek PC, Ficker JH (2004) Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Am J Respir Crit Care Med 69:156–162
Ferini-Strambi L, Fantini ML, Castronovo C (2004) Epidemiology of obstructive sleep apnea syndrome. Minerva Med 95:187–202
Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A (1998) Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med 157:144–148
Braghiroli A (1999) Who is Mr. Z. Sleep Breath 3:37–38
Lavie P, Lavie L, Herer P (2005) All-cause mortality in males with sleep apnoea syndrome: declining mortality rates with age. Eur Respir J 25:514–520
Telakivi T, Kajaste S, Partinen M, Koskenvuo M, Salmi T, Kaprio J (1988) Cognitive function in middle-aged snorers and controls: role of excessive daytime somnolence and sleep-related hypoxic events. Sleep 11:454–462
Shochat T, Pillar G (2003) Sleep apnoea in the older adult: pathophysiology, epidemiology, consequences and management. Drugs Aging 20:551–560
Cohen-Zion M, Stepnowsky C, Marler, Shochat T, Kripke DF, Ancoli-Israel S (2001) Changes in cognitive function associated with sleep disordered breathing in older people. J Am Geriatr Soc 49:1622–1627
Young T (1996) Sleep-disordered breathing in older adults: is it a condition distinct from that in middle-aged adults. Sleep 19:529–530
Lee MM, Strauss ME, Adams N, Redline S (1999) Executive functions in persons with sleep apnea. Sleep Breath 3:13–16
Naegele B, Thouvard V, Pepin JL, Levy P, Bonnet C, Perret JE, Pellat J, Feuerstein C (1995) Deficits of cognitive executive functions in patients with sleep apnea syndrome. Sleep 18:43–52
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Alchanatis M, Zias N, Deligiorgis N, Amfilochiou A, Dionellis G, Orphanidou D (2005) Sleep apnea-related cognitive deficits and intelligence: an implication of cognitive reserve theory. J Sleep Res 14:69–75
Kotterba S, Rasche K, Widdig W, Duscha C, Blombach S, Schultze-Werninghaus G, Malin JP (1998) Neuropsychological investigations and event-related potentials in obstructive sleep apnea syndrome before and during CPAP-therapy. J Neurol Sci 159:45–50
SCHUHFRIED GmbH. www.schuhfried.co.at
Golden C (1982) Clinical interpretation of objective psychological tests. Grune and Straton, University of Nebraska Medical Center
Lezac M (1995) Neuropsychological assessment, 3rd edn. Oxford University Press, New York
Raven J, Court J, Raven J (1976) Manual for Raven’s progressive matrices. HK Lewis, London
Bliwise DL (1994) Normal aging. Principles and practise of sleep medicine. In: Kryger MH, Roth TC, Dement WC (eds) WB Saunders, Philadelphia, pp 26–39
Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV (2004) Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 27:1255–1273
Bedard MA, Montplaisir J, Richer F, Malo J (1991) Nocturnal hypoxemia as a determinant of vigilance impairment in sleep apnea syndrome. Chest 100:367–370
Colt HG, Haas H, Rich GB (1991) Hypoxemia vs sleep fragmentation as cause of excessive daytime sleepiness in obstructive sleep apnea. Chest 100:1542–1548
Gottlieb DJ, Whitney CW, Bonekat WH, Iber C, James GD, Lebowitz M, Nieto FJ, Rosenberg CE (1999) Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am J Res Crit Care Med 159:502–507
Miliauskas S, Sakalauskas R (2005) [Peculiarities of nocturnal oxygen saturation in obstructive sleep apnea]. Medicina (Kaunas, Lithuania) 41:217–220
Morrell MJ, Twigg G (2006) Neural consequences of sleep disordered breathing: the role of intermittent hypoxia. Adv Exp Med Biol 588:75–88
Punjabi NM, O’Hearn DJ, Neubauer DN, Nieto FJ, Schwartz AR, Smith PL, Bandeen-Roche K (1999) Modeling hypersomnolence in sleep-disordered breathing. A novel approach using survival analysis. Am J Res Crit Care Med 159:1703–1709
Johns MW (1993) Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth sleepiness scale. Chest 103:30–36
Adams N, Strauss M, Schluchter M, Redline S (2001) Relation of measures of sleep-disordered breathing to neuropsychological functioning. Am J Res Crit Care Med 163:1626–1631
Engleman HM, Kingshott RN, Martin SE, Douglas NJ (2000) Cognitive function in the sleep apnea/hypopnea syndrome (SAHS). Sleep 23(Suppl 4):S102–S108
Quan SF, Wright R, Baldwin CM, Kaemingk KL, Goodwin JL, Kuo TF, Kaszniak A, Boland LL, Caccappolo E, Bootzin RR (2006) Obstructive sleep apnea-hypopnea and neurocognitive functioning in the Sleep Heart Health Study. Sleep Med 7:498–507
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Lavie P, Herer P, Peled R, Berger I, Yoffe N, Zomer J, Rubin AH (1995) Mortality in sleep apnea patients: a multivariate analysis of risk factors. Sleep 18:149–157
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alchanatis, M., Zias, N., Deligiorgis, N. et al. Comparison of cognitive performance among different age groups in patients with obstructive sleep apnea. Sleep Breath 12, 17–24 (2008). https://doi.org/10.1007/s11325-007-0133-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-007-0133-y