Abstract
Cutaneous melanoma (CM) poses a therapeutic challenge due to its aggressive nature and often limited response to conventional treatments. Exploring novel therapeutic targets is essential, and natural compounds have emerged as potential candidates. This study aimed to elucidate the impact of curcumin, a natural compound known for its anti-inflammatory, antioxidant, and anti-tumor properties, on metastatic melanoma cells, focusing on the purinergic system and immune responses. Human melanoma cell line SK-Mel-28 were exposed to different curcumin concentrations for either 6 or 24 h, after which we assessed components related to the purinergic system and the inflammatory cascade. Using RT-qPCR, we assessed the gene expression of CD39 and CD73 ectonucleotidases, as well as adenosine deaminase (ADA). Curcumin effectively downregulated CD39, CD73, and ADA gene expression. Flow cytometry analysis revealed that curcumin significantly reduced CD39 and CD73 protein expression at specific concentrations. Moreover, the A2A receptor’s protein expression decreased across all concentrations. Enzymatic activity assays demonstrated that curcumin modulated CD39, CD73, and ADA activities, with effects dependent on concentration and duration of treatment. Extracellular ATP levels increased after 24 h of curcumin treatment, emphasizing its role in modulating hydrolytic activity. Curcumin also displayed anti-inflammatory properties by reducing NLRP3 gene expression and impacting the levels of key inflammatory cytokines. In conclusion, this study unveils the potential of curcumin as a promising adjuvant in CM treatment. Curcumin modulates the expression and activity of crucial components of the purinergic system and exhibits anti-inflammatory effects, indicating its potential therapeutic role in combating CM. These findings underscore curcumin’s promise and warrant further investigation in preclinical and clinical settings for melanoma management.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cutaneous melanoma (CM) stands as one of the most lethal skin cancers, characterized by its aggressive nature and surging incidence rates. Recent statistics signal a concerning trend, with a projected 510,000 new cases and 96,000 CM-related deaths by 2040 [1]. The prognosis for CM remains unfavorable, primarily due to late-stage diagnosis and limited responses to systemic treatments. Even with the introduction of immunotherapy, long-term survival rates in advanced stages of the disease (III and IV) are estimated to be around 20% [2, 3]. Given this reality, novel therapeutic strategies have come under scrutiny, particularly those targeting inflammatory responses and purinergic signaling, which have implications for tumorigenesis, progression, angiogenesis, and metastasis across diverse malignancies [4, 5].
The purinergic system encompasses a complex cell signaling network involved in a range of physiological processes, including tumor development and progression [6, 7]. Adenosine plays a pivotal role in tumor progression. Within the extracellular environment, ectonucleoside triphosphate diphosphohydrolase-1 (CD39) transforms eATP into adenosine diphosphate (ADP) and adenosine monophosphate (AMP). Additionally, ecto-5′-nucleotidase (CD73) further metabolizes AMP into adenosine. Consequently, heightened adenosine levels within the tumor microenvironment (TME) foster an immunosuppressive milieu, thereby facilitating tumor growth [7, 8].
Similarly, the inflammatory response, particularly the inflammasome, has garnered attention as a promising neoplastic therapy, with the nucleotide-binding domain of the leucine-rich family containing pyrin-3 domain (NLRP3) inflammasome being the most extensively studied [9]. In CM, NLRP3 is of great interest since it is expressed in melanoma cell lines, and polymorphisms related to this gene are linked to disease susceptibility [10]. Furthermore, NLRP3 participates in the inflammatory cascade and plays a pivotal role in the inflammatory cascade and tumor progression [11].
Considering the discovery of new therapeutic targets for CM and the low effectiveness of available treatments, the exploration of bioactive compounds with in vitro and in vivo antineoplastic potential i has increased since they can become adjuvant options in systemic treatment due to their cost-effectiveness [12]. Among these compounds, curcumin, a polyphenol derived from Curcuma longa, is a pleiotropic molecule exhibiting anti-inflammatory, antioxidant, and antineoplastic effects [13]. The chemical structure of curcumin is shown in Fig. 1.
In CM cells, curcumin has demonstrated an ability to hinder cell growth, angiogenesis, and metastasis, and induce cytotoxicity and prompt cell death [14]. While several pathways are influenced by curcumin, its specific actions concerning the purinergic system and CM have remained largely unexplored. However, purinergic signaling holds considerable relevance in CM due to its involvement in melanogenesis and immune response dysfunction [15, 16].
Understanding how curcumin influences the purinergic system and the NLRP3 inflammasome in metastatic melanoma cells is the primary objective of this study. Despite curcumin’s recognized potential in inhibiting CM cell growth, angiogenesis, and metastasis, the specific molecular mechanisms related to the purinergic system and CM remain largely uncharted. These mechanisms represent pivotal targets due to their relevance in melanogenesis and immune response dysfunction.
Material and methods
Chemicals and reagents
All chemicals and reagents used for this study were of analytical grade and purchased from Sigma-Aldrich (Sigma-Aldrich et al., USA) and Merck (Darmstadt, Germany). Cell culture plates and flasks used for the culture procedures were obtained from Gibco™ Thermo Fisher Scientific (Grand Island, NY, USA) and Invitrogen Life Technologies (Carlsbad, CA, USA).
Cell culture and exposure to curcumin
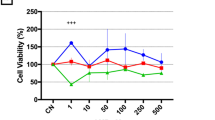
The human melanoma cell line SK-Mel-28 was purchased from the Rio de Janeiro Cell Bank (BCRJ), Brazil. Cells were cultured in flasks with Dulbecco’s modified Eagle medium (DMEM — high glucose and L-glutamine) containing antibiotic and antifungal (penicillin/streptomycin) and supplemented with 10% fetal bovine serum. Cells were cultured under suitable conditions using a humidified and controlled atmosphere with 5% carbon dioxide (CO2) at 37 °C. Curcumin was dissolved in 0.2% dimethylsulfoxide (DMSO) and in an appropriate culture medium to obtain different concentrations, and the cells were treated for 6 or 24 h with 0.1, 1, and 10 µM, based on a previous study [14]. Cells in the negative control group (CT) received only the culture medium. All experiments were performed 3 times independently.
Gene expression of CD39, CD73, ADA, and NLRP3
Total RNA from melanoma cells was extracted using TRIzol® according to the manufacturer’s instructions. RNA quantification was performed using a μDrop™ spectrophotometer (Varioskan LUX™, Thermo Fisher Scientific, USA), and RNA purity was assessed by the 260/280 nm absorption ratio. Initially, the RNA was treated with DNAse (Thermo Scientific, USA) following the manufacturer’s recommendations. For the preparation of the cDNA, the cDNA synthesis kit High Capacity cDNA Reverse Transcription Kit (Thermo Scientific, USA) was used, where 10 µl of 2X RT master mix and 10 µl of the RNA sample (approximately 20 ng) were used, according to the manufacturer’s instructions. Molecular assay was performed using 5 µl of cDNA sample, 10 µl of 2X Power SYBR™ Green PCR Master Mix (Thermo Scientific, USA), 2 µl of F primer (500 nM), 2 µl of R primer (500 nM), and 1 µl of ultrapure water for a final volume of 20 µl. The temperature parameters of the PCR program were: preheating at 95 °C for 3 min, followed by 60 cycles of denaturation at 95 °C for 15 s, and annealing at 60 °C for 1 min. Melting curve analysis was performed to verify product identity. Samples were run in triplicates, and results were expressed regarding GAPDH levels. The data were then normalized to a calibrator sample using the ΔΔCq method. The forward and reverse sequences of oligos (5′–3′) used for each gene are described in Table 1.
Detection of CD39, CD73, and A2AR protein expression by flow cytometry
Melanoma cells were maintained in culture flasks until the confluence phase, followed by dissociation with trypsin, and immediately counted in a hemocytometer. Then, 1 × 106 cells were centrifuged for 5 min at 400 g and washed twice with phosphate-buffered saline (PBS) with 10% fetal bovine serum (FBS). The pellets were suspended and incubated for 30 min with 5 µl of the respective purified mouse antibody anti-human CD39 (catalog number 555464 BD Pharmingen™), anti-human CD73 (catalog number 550257 BD Pharmingen™), and anti-human A2AR (catalog number MA5-31611 Invitrogen™). The same number of cells was incubated without antibodies (negative control). All samples were washed with PBS, and 10,000 events were immediately acquired by flow cytometry (BD ACCURI C6) and analyzed by FlowJo V10 software. The results were expressed as the percentage of CD39, CD73, or A2AR positive cells compared to control and MFI.
Evaluation of CD39, CD73, and ADA
The enzymatic activities of CD39 and CD73 were performed according to Pilla et al. [17] and Lunkes et al. [18]. A reaction system for CD39 was prepared containing 5 mM CaCl2, 100 mM NaCl, 5 mM KCl, 6 mM glucose, and 50 mM Tris–HCl buffer, pH 7.4. The reaction system for CD73 was the same as for CD39, except 10 mM MgCl2 instead of CaCl2. Briefly, cells were suspended in saline solution (NaCl, 0.9%), and 20 µl of sample cells was added to each enzyme reaction mixture and pre-incubated at 37 °C for 10 min. The enzymatic reaction was started by adding specific substrates for each enzyme, ATP and ADP for CD39 and AMP for CD73 and incubated at 37 °C for 70 min. Finally, reactions were stopped by adding 150 µl of 15% TCA. Of the total contents of the well, 30 µl was transferred to a new plate; 300 µl of malachite green was added as a colorimetric reagent, and the released inorganic phosphate was determined at 630 nm. All samples were performed in triplicates. Control wells were performed to correct for non-enzymatic hydrolysis. A standard curve was prepared with KH2PO4, and the results were expressed in nmol/Pi released/min/mg protein [17].
Furthermore, ADA activity was evaluated based on adenosine (Ado) deamination, measuring the amount of ammonia released in the reaction following previously published general guidelines [18]. Finally, absorbance was read at 620 nm, and values were expressed in units/liter (U/l).
Determination of extracellular ATP levels
Molecular Probes® ATP Determination Kit (Invitrogen™), an extremely sensitive bioluminescence assay, was used with recombinant firefly luciferase and its substrate D-luciferin. The assay is based on the requirement of luciferase for ATP in light production — maximum emission ~ 560 nm at pH 7.8 [19]. We combined the reaction components to make a standard reaction solution. We adjusted the volumes to specific requirements: each reaction contained 1.25 µg/ml firefly luciferase, 50 µM D-luciferin, and 1 mM of DTT in 1 × reaction buffer. After 15 min of incubation, the luminescence was measured. An ATP standard curve was prepared at 1 nM to 1 µM concentrations.
Inflammatory profile
To investigate the participation of inflammation in curcumin responses, the levels of IL-2, IL-6, IL-10, and TNF were evaluated in the supernatant with flow cytometry using the commercial kit Cytometric Bead Array (CBA) (BD Human Th1/Th2 Cytokine Kit II) following the manufacturer’s guidelines. For this, 25 µl of supernatant, 25 µl of mixed suspension of capture beads, and 25 µl of phycoerythrin (PE) detection reagents were mixed and incubated at room temperature, in the dark, for 3 h. Then, data acquisition was performed with a BD ACCURI C6 flow cytometer and evaluated in appropriate software. The results were expressed in pg/ml.
Protein determination
The Bradford method [20] was employed for protein determination using bovine serum albumin as a standard, and the protein samples were adjusted according to each assay in mg/ml.
Statistical analysis
All measurements were performed statistically by analysis of one-way variance (ANOVA) followed by appropriate post hoc testing using GraphPad Prism 9 software. All data were expressed as mean ± standard deviation. Differences between groups in relation to the studied variables were evaluated using one-way ANOVA analysis. Differences in the probability of rejecting the null hypothesis as < 5% (P < 0.05) were considered statistically significant. Statistical significance was defined for p values of *P < 0.05, **P < 0.01, ***P < 0.001, and ****P < 0.0001.
Results
Curcumin modulates the expression of CD39, CD73, ADA, and A2A in CM cells
We use RT-qPCR to evaluate CD39, CD73, and ADA gene expression in CM cells, as shown in Fig. 2 (A, D, and G). After 24 h of treatment, curcumin reduced CD39 gene expression at concentrations of 0.1 µM (P = 0.0211), 1 µM (P < 0.0001), and 10 µM (P = 0.0009). In alignment with the CD39 findings, curcumin also attenuated CD73 gene expression at concentrations of 0.1 µM (P = 0.0068) and 1 µM (P < 0.0001). In addition, ADA gene expression exhibited a substantial decline across all tested concentrations (P < 0.0001).
Expression of CD39, CD73, ADA, and A2AR genes and proteins. After 24 h of curcumin treatment, there was a reduction in CD39 gene expression in all tested concentrations (A). Curcumin promoted a decrease in CD39 protein expression at a concentration of 1 μM (B–D). Regarding CD73, a decrease in gene expression was observed at concentrations of 0.1 and 1 μM. E In relation to the protein expression of CD73, a decrease in the concentrations of 0.1 and 1 μM was verified and an increase at a concentration of 10 μM (F–H). A decrease in ADA gene expression was observed at all concentrations tested (I). Likewise, there was a decrease in the protein expression levels of the A2AR receptor in all curcumin concentrations after 24 h of treatment (J–L). Data are presented as mean ± SD. Statistical analysis: ANOVA. Values with P < 0.05 were considered statistically significant. *(P < 0.05), **(P < 0.01), ***(P < 0.001), ****(P < 0.0001). Dimethylsulfoxide (DMSO)
Flow cytometry is employed to analyze the protein expression of CD39, CD73, and the A2A receptor, as shown in Fig. 2 (B–D, F–H, and J–L). Consistent with gene expression results, curcumin elicited a significant decrease in CD39 protein expression at 1 µM concentration (P = 0.0357). Regarding the expression of the CD73 protein, it was possible to observe a reduction when cells were treated with curcumin contractions of 0.1 µM (P = 0.0056) and 1 µM (P < 0.0001). Nonetheless, at a higher concentration of 10 µM, curcumin upregulated CD73 protein expression (P = 0.0105). Thus, it was evident that curcumin at 1 µM concentration can decrease gene and protein expression of CD39 and CD73 ectonucleotidases (Fig. 2). About the A2A receptor, we observed a decrease in protein expression at all concentrations of curcumin tested (P < 0.0001) when compared to CT (Fig. 2J–L).
In addition to the percentages of positive cells, we also checked the median fluorescence intensity (MFI). MFI levels showed no difference between CD39 levels (Fig. 2D). In the same way, as found in the percentages of cells positive for CD73, the MFI revealed that there is a decrease in the levels of CD73 protein expression after treatment with 0.1 µM (P = 0.0093) and 1 µM (P = 0.0114) (Fig. 2H). The MFI of A2AR only showed a significant reduction at a concentration of 10 µM (P = 0.0089) (Fig. 2L).
Modulation of CD39, CD73, and ADA enzymatic activities in CM cells by curcumin
Figure 3 presents the enzymatic activity results for CD39, CD73, and ADA after 6 h (Fig. 2A–D) and 24 h (Fig. 2E–H) of curcumin treatment. After 6 h of curcumin treatment, we observed increased ATP hydrolysis by CD39 at all concentrations tested, with the most pronounced effect observed at 1 µM concentration (P < 0.0001) and a comparatively milder effect at 0.1 µM (P = 0.0023) and 10 µM (P = 0.0041) (Fig. 3A). Regarding AMP hydrolysis by CD73, we observed a decrease in enzymatic activity at 1 µM concentration of curcumin (P = 0.0269) (Fig. 3C). Concerning the deamination of Ado by ADA, we observed a significant increase in this enzymatic activity induced by curcumin at concentrations of 1 µM (P = 0.0113) and 10 µM (P = 0.0082). No significant difference was observed in ADP hydrolysis among groups (Fig. 3B).
CD39 activity (ATP and ADP hydrolysis), CD73 activity (AMP hydrolysis), and adenosine deaminase (ADA) activity. At all curcumin concentrations tested, the treatment increased ATP hydrolysis after 6 h (A). AMP hydrolysis after 6 h of treatment was reduced at a concentration of 1 μM (C). ADA activity after 6 h of treatment increased at concentrations of 1 and 10 μM (D). After 24 h of treatment, there was an increase in AMP hydrolysis at concentrations of 0.1 and 1 μM (E). It was not possible to observe a significant difference in ADP levels after 6 h (B) and 24 h of treatment (F). The levels of ATP hydrolysis (E) and ADA activity (H) did not show significant differences after 24 h of treatment. Data are presented as mean ± SD. Statistical analysis: ANOVA. Values with P < 0.05 were considered statistically significant. *(P < 0.05), **(P < 0.01), ***(P < 0.001), ****(P < 0.0001). Dimethylsulfoxide (DMSO)
After 24 h of curcumin treatment, there were no differences in the ATP and ADP hydrolysis levels by CD39 activity (Fig. 2E–F). Conversely, we observed that curcumin caused an increase in the hydrolytic activity of CD73 ectonucleotidase, which corresponds to AMP hydrolysis, at concentrations of 0.1 µM (P = 0.0008) and 1 µM (P = 0.0303) (Fig. 3G). Concerning ADA activity, no significant difference was observed compared to CT (Fig. 3H). Furthermore, as presented in Fig. 4 (A and B), 6 h of curcumin treatment do not alter extracellular ATP levels in relation to CT (Fig. 4A). In contrast, after 24 h, we observed an increase in extracellular ATP levels at curcumin concentrations of 1 µM (P = 0.0185) and 10 µM (P = 0.0006) (Fig. 4B). The results collectively attest the role of curcumin in modulating hydrolytic activity of CD73 and CD79 and consequently regulate extracellular ATP levels in CM cells.
Extracellular ATP levels were assessed by a sensitive bioluminescent assay. Extracellular ATP levels showed no significant difference after 6 h of treatment with curcumin (A). After 24 h of treatment, there was an increase in the amount of ATP at concentrations of 1 and 10 μM (B). Data are presented as mean ± SD. Statistical analysis: ANOVA. Values with P < 0.05 were considered statistically significant. * (P < 0.05), ** (P < 0.01) *** (P < 0.001) **** (P < 0.0001). Dimethylsulfoxide (DMSO)
Curcumin decreases NLRP3 gene expression and cytokine levels
To evaluate the effect of curcumin on NLRP3 gene expression in CM cells, we use RT-qPCR, as shown in Fig. 5. All curcumin concentrations tested (0.1, 1, and 10 µM) decreased NLRP3 gene expression. Particularly, the effects of curcumin are more pronounced at concentrations of 0.1 and 10 µM (P < 0.0001) compared to the 1 µM concentration (P = 0.0008), as illustrated in Fig. 5 A.
Curcumin decreases NLRP3 inflammasome gene expression and levels of cytokines IL-6, IL-10, and TNF. At all tested concentrations, curcumin decreases NLRP3 inflammasome gene expression (A). After 24 h of treatment, there was an increase in IL-6 in the concentration of 0.1 μM and a decrease in the concentration of 10 μM (C). IL-10 levels decreased after treatment with 10 μM curcumin for 24 h (D). Curcumin at 1-μM and 10-μM concentrations significantly decreases TNF levels (E). IL-2 levels showed no significant difference after 24 h of curcumin treatment (B). Data are presented as mean ± SD. Statistical analysis: ANOVA. Values with P < 0.05 were considered statistically significant. * (P < 0.05), ** (P < 0.01), *** (P < 0.001), **** (P < 0.0001). Dimethylsulfoxide (DMSO)
The levels of inflammatory cytokines were evaluated in the cell culture medium of CM using a CBA kit. The results demonstrated an increase of IL-6 levels at 0.1-µM curcumin concentration (P = 0.0410) and a decrease at 10-µM concentration (P = 0.0137) when compared to the CT (Fig. 5C). Regarding IL-10, the results showed a significant reduction in these cytokine levels at curcumin concentration of 10 µM (P = 0.0029) (Fig. 5D). In addition, curcumin decreased TNF levels at concentrations of 1 µM (P = 0.0002) and 10 µM (P = 0.0004) (Fig. 5E). However, curcumin treatment did not alter IL-2 levels (Fig. 5B). Figure 6 presents a summary of the main results found in this study.
Curcumin induces tumor suppression of metastatic cutaneous melanoma cells via modulation of purinergic signaling and inflammatory response. The figure shows that treating SK-Mel-28 metastatic melanoma cells with curcumin reduced the hydrolysis of ATP, ADP, and AMP nucleotides. In agreement, a decrease in the gene and protein expression of the ectonucleotidases CD39 and CD73 was also observed, and consequently, an increase in the levels of extracellular ATP. With the decrease in adenosine levels in the extracellular environment and reduction in the expression of the A2A receptor, a less immunosuppressive environment is obtained, and, as a consequence, tumor suppression occurs. Abbreviations: ATP, adenosine triphosphate; ADP, adenosine diphosphate; AMP, adenosine monophosphate; E-NPPs, CD39/ENTPD-1, ectonucleoside triphosphate diphosphohydrolase 1; E-NT5/CD73, Ecto-5′-nucleotidase; ADA, adenosine deaminase; NLRP3, NLR family pyrin domain containing 3; IL-6, interleukin 6; TNF, tumor necrosis factor
Discussion
To increase the effectiveness of existing therapeutic approaches by modulating different pathways, researchers have verified an intimate relationship between purinergic signaling and the development and progression of CM. This linkage is primarily attributed to the interplay of extracellular ATP, known for its pro-inflammatory properties, with CD39 and CD73, as well as the involvement of Ado, recognized for its immunosuppressive actions. [6, 21]. In this study, we found that curcumin decreased gene and protein expression of CD39 and CD73 ectonucleotidases (Fig. 3). Similar results were found by Lui et al. [22] in a sepsis model, in which curcumin reduced the amount of CD39 + cells as a regulatory mechanism of inflammation and improvement of immune function.
In the case of CM, decreasing the expression of ectonucleotidases is positive since the extracellular synthesis of Ado is an important immunosuppression pathway in the tumor microenvironment (TME) [23]. Previously, Bagatini et al. [24] verified that 1α, 25-dihydroxyvitamin D3 is capable of modulating the expression and enzymatic activity of ectonucleotidases, preventing the immunosuppressive activity of Ado in melanoma cells. In this sense, Shevchenko et al. [25] suggested that immunotherapy with anti-programmed cell death 1 (anti-PD-1) antibodies with an anti-adenosinergic compound would be a new way to treat cancer. Other studies with mice observed a positive effect using combined anti-PD-1 therapy and an Ado A2A receptor inhibitor [26, 27]. Our study observed decreased A2A protein expression at all curcumin concentrations tested. This receptor is mainly responsible for the immunosuppressive activity of Ado, and its blockade, together with the use of the anti-PD-1 monoclonal antibody, resulted in greater effectiveness of the treatment and reduction of metastases [27]. In our case, curcumin would increase the effectiveness of the anti-melanoma treatment.
Furthermore, studies have shown that curcumin is a potent A2A receptor antagonist, corroborating our results and confirming our initial hypothesis that curcumin acts mainly by blocking Ado production and antagonizing its receptors and may be a strong candidate for adjuvant use in the treatment of the CM [28, 29]. On the other hand, in our study, the highest concentrations of curcumin treatment increased gene, protein expression, and the enzymatic activity of CD39 and CD73 ectonucleotidases, especially after 24 h of treatment, and increased extracellular ATP levels. These events can be explained by considering the increase in ATP leakage caused by curcumin-induced apoptosis in CM cells [30, 31]. In our previous study, we demonstrated that curcumin significantly decreases the viability of SK-Mel-28 cells and increases the levels of apoptosis [14]. When apoptosis occurs, a series of events are associated, such as the rupture of cell organelles and permeabilization of the cell membrane, which leads to exocytosis of ATP, which previously had an energetic function in the intracellular environment [30]. Considering the increase in extracellular ATP, one way to maintain homeostasis is to increase the hydrolytic activity of ectonucleotidases that hydrolyze the nucleotide to transform it into Ado, since in the extracellular environment, this molecule acts as damage-associated molecular patterns (DAMPs) inducing cell death via P2X receptors [32,33,34]. In addition to inducing cell death, high levels of ATP can result in the activation of NLRP3, which is directly related to melanogenesis and metastasis [35].
Ju et al. [11] found that NLRP3 acts independently for the prognosis of CM and response to treatments, including immunotherapy, so it is essential to know the caspase pathways to modulate NLRP3. In CM, the NLRP3 is related to the suppression of antitumor immunity, leading to the generation of a permissive environment for the tumor via IL-1β, which culminates in tumor growth and progression [36, 37]. Inflammasome inhibition has shown to be promising, as it is related to increased metastases and decreased effectiveness of therapies [38]. In this study, we observed a decrease in NLRP3 gene expression after treatment with curcumin. In this sense, Theivanthiran et al. [39] found that genetic and pharmacological inhibition of this marker suppressed tumor infiltration, migration of the granulocytic subset of myeloid-derived suppressor cells (PMN-MDSC), and significantly increased the efficacy of anti-PD-1 immunotherapy.
The NLRP3 is also responsible for inducing IL-6 production [36]. This cytokine is considered the most important for sustaining tumor progression and acting on proliferation, apoptosis, angiogenesis, and differentiation [40]. In patients with CM, elevated levels of IL-6 were associated with poor prognosis [38] and distant metastases [41, 42]. Tengesdal et al. [43] verified that the inhibition of NLRP3 in CM cells decreases the production of IL-1β and IL-6 and consequently could inhibit immunosuppression and cell proliferation via disruption of the Janus kinase axis (JAK)/signal transducer and transcriptional activator 3 (STAT3). In addition to IL-6, another cytokine involved in modulating tumor progression and metastasis is TNF-α, which upregulates matrix metalloproteinases, leading to metastasis via epithelial-mesenchymal transition (EMT). The IL-6/STAT3 pathway has been suggested as an important therapeutic target for treating hepatocellular carcinoma [44]. In pancreatic cancer, curcumin inhibited cell invasion by blocking the IL-6/ERK/NF-κB axis [45]. In mice with CM, curcumin suppressed TNF-α-induced EMT, decreasing tumor growth and prolonging animal survival [46]. Similar results were observed in our study, in which curcumin decreased NLRP3 expression and IL-6, IL-10, and TNF-α levels. In agreement with the data obtained in this study, Bill et al. [47] found that a curcumin-analogue induced apoptosis of melanoma cells via IL-6/STAT-3.
Previous studies have reported that IL-10 is highly expressed in cutaneous melanoma cells and is involved in STAT3 pathway signaling [48]. A positive correlation was observed between IL-10 and tumor progression since it negatively regulates the immune response and consequently supports tumor immune escape [49]. Accordingly, Maruyama et al. [50] found that the curcumin-analog GO-Y030 inhibits IL-10 production and consequently increases the effectiveness of immune checkpoint inhibitors. In addition, it is essential for the survival of Treg, the main escape route of anti-PD-1 therapies [51]. Like curcumin, Yu et al. [52] observed that dihydroartemisinin also inhibits tumor progression via IL-6/IL-10/STAT-3, making these substances excellent options for therapeutic adjuvants.
Considering the evidence and results presented here, curcumin should be widely studied since it has an antitumor effect on several cell lines and can modulate antitumor immunity pathways, one of the main obstacles to successful treatment, and thus increasing the effectiveness of the therapies in use, mainly the anti-PD-1.
Studies with humans that test curcumin’s antineoplastic potential are scarce since the main obstacle encountered is low bioavailability [53]. Therefore, new formulations involving nanotechnology are being tested mainly on different types of cancer [54, 55].
Conclusion
In conclusion, our study underscores the potential of curcumin as a valuable subject for further investigation in the adjuvant treatment of CM. By modulating key components of the purinergic system and the NLRP3 inflammasome, curcumin demonstrates a multifaceted effect on CM cells. Notably, curcumin reduces the immunosuppressive potential of CM by decreasing the gene, protein, and enzymatic activity of CD39 and CD73 ectonucleotidases, which participate in the production of immunosuppressive Ado. These findings align with previous studies suggesting that curcumin, an A2A receptor antagonist, could potentially enhance anti-melanoma treatments.
Furthermore, we observed the downregulation of NLRP3 inflammasome expression, leading to a decrease in critical inflammatory cytokines, such as IL-6, IL-10, and TNF-α, known for their roles in promoting tumor progression, metastasis, and immune evasion. The inhibition of the NLRP3 inflammasome and the associated cytokines suggests that curcumin may offer promise in augmenting the effectiveness of anti-CM therapies, particularly those targeting the PD-1 pathway. These findings not only affirm curcumin as a potential adjuvant therapy but also emphasize the importance of further research into its role in enhancing the treatment of CM. We recommend further in vivo studies since this substance is a strong candidate for adjuvant therapy in CM.
Data availability
No datasets were generated or analysed during the current study.
References
Arnold M, Singh D, Laversanne M, Vignat J, Vaccarella S, Meheus F et al (2022) Global burden of cutaneous melanoma in 2020 and projections to 2040. JAMA Dermatol 158(5):495
Rebecca VW, Somasundaram R, Herlyn M (2020) Pre-clinical modeling of cutaneous melanoma. Nat Commun 11(1):2858
Tangella LP, Clark ME, Gray ES (2021) Resistance mechanisms to targeted therapy in BRAF-mutant melanoma - a mini-review. Biochim Biophys Acta (BBA) - Gen Subj 1865(1):129736
McAllister SS, Weinberg RA (2010) Tumor-host interactions: a far-reaching relationship. JCO 28(26):4022–4028
Gouravani M, Khalili N, Razi S, Keshavarz-Fathi M, Khalili N, Rezaei N (2020) The NLRP3 inflammasome: a therapeutic target for inflammation-associated cancers. Expert Rev Clin Immunol 16(2):175–187
Huang Z, Xie N, Illes P, Di Virgilio F, Ulrich H, Semyanov A et al (2021) From purines to purinergic signaling: molecular functions and human diseases. Sig Transduct Target Ther 6(1):162
Di Virgilio F, Sarti AC, Falzoni S, De Marchi E, Adinolfi E (2018) Extracellular ATP and P2 purinergic signaling in the tumor microenvironment. Nat Rev Cancer 18(10):601–618
Allard B, Longhi MS, Robson SC, Stagg J (2017) The ectonucleotidases CD 39 and CD 73: novel checkpoint inhibitor targets. Immunol Rev 276(1):121–144
Ting JPY, Lovering RC, Alnemri ES, Bertin J, Boss JM, Davis BK et al (2008) The NLR gene family: a standard nomenclature. Immunity 28(3):285–287
Verma D, Bivik C, Farahani E, Synnerstad I, Fredrikson M, Enerbäck C et al (2012) Inflammasome polymorphisms confer susceptibility to sporadic malignant melanoma: inflammasome polymorphisms in melanoma. Pigment Cell Melanoma Res 25(4):506–513
Ju M, Bi J, Wei Q, Jiang L, Guan Q, Zhang M et al (2021) Pan-cancer analysis of NLRP3 inflammasome with potential implications in prognosis and immunotherapy in human cancer. Brief Bioinform 22(4):bbaa345
Hazafa A, Rehman KU, Jahan N, Jabeen Z (2020) The role of polyphenol (flavonoids) compounds in the treatment of cancer cells. Nutr Cancer 72(3):386–397
Kocaadam B, Şanlier N (2017) Curcumin, an active component of turmeric (Curcuma longa), and its effects on health. Crit Rev Food Sci Nutr 57(13):2889–2895
Manica D, Silva GBD, Silva APD, Marafon F, Maciel SFVDO, Bagatini MD et al (2023) Curcumin promotes apoptosis of human melanoma cells by caspase 3. Cell Biochem Funct 41(8):1295–304
Umansky V, Shevchenko I, Bazhin AV, Utikal J (2014) Extracellular adenosine metabolism in immune cells in melanoma. Cancer Immunol Immunother 63(10):1073–1080
Kazemi MH, Raoofi Mohseni S, Hojjat-Farsangi M, Anvari E, Ghalamfarsa G, Mohammadi H, Jadidi-Niaragh F (2018) Adenosine and adenosine receptors in the immunopathogenesis and treatment of cancer. J Cell Physiol 233(3):2032–2057
Pilla C, Emanuelli T, Frassetto SS, Battastini AM, Dias RD, Sarkis JJ (1996) ATP diphosphohydrolase activity (apyrase EC 3.6.1.5) in human blood platelets. Platelets 7(4):225–230
Lunkes GI, Lunkes D, Stefanello F, Morsch A, Morsch VM, Mazzanti CM, Schetinger MR (2003) Enzymes that hydrolyze adenine nucleotides in diabetes and associated pathologies. Thromb Res 109(4):189–194
Karamohamed S, Guidotti G (2001) Bioluminometric Method for Real-Time Detection of ATPase activity. Biotechniques 31(2):420–425
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72(1–2):248–254
Gourdin N, Bossennec M, Rodriguez C, Vigano S, Machon C, Jandus C, Bauché D, Faget J, Durand I, Chopin N, Tredan O, Marie JC, Dubois B, Guitton J, Romero P, Caux C, Ménétrier-Caux C (2018) Autocrine adenosine regulates tumor polyfunctional CD73+CD4+ effector T cells devoid of immune checkpoints. Abstract Cancer Res 78(13):3604–3618
Liu Y, Feng L, Hou G, Yao L (2022) Curcumin elevates microRNA-183-5p via Cathepsin B-mediated phosphatidylinositol 3-Kinase/AKT pathway to strengthen lipopolysaccharide-stimulated immune function of sepsis mice. Contrast Media Mol Imaging 2022:1–10
Muller-Haegele S, Muller L, Whiteside TL (2014) Immunoregulatory activity of adenosine and its role in human cancer progression. Expert Rev Clin Immunol 10(7):897–914
Bagatini MD, Bertolin K, Bridi A, Pelinson LP, da Silva Rosa Bonadiman B, Pillat MM, Gonçalves PBD, Ulrich H, Schetinger MRC, Morsch VM (2019) 1α 25-Dihydroxyvitamin D3 alters ectonucleotidase expression and activity in human cutaneous melanoma cells. J Cell Biochem 120(6):9992–10000
Shevchenko I, Mathes A, Groth C, Karakhanova S, Müller V, Utikal J, Werner J, Bazhin AV, Umansky V (2020) Enhanced expression of CD39 and CD73 on T cells in the regulation of anti-tumor immune responses. OncoImmunology 9(1):1744946
Leone RD, Sun IM, Oh MH, Sun IH, Wen J, Englert J, Powell JD (2018) Inhibition of the adenosine A2a receptor modulates expression of T cell coinhibitory receptors and improves effector function for enhanced checkpoint blockade and ACT in murine cancer models. Cancer Immunol Immunother 67(8):1271–1284
Mittal D, Young A, Stannard K, Yong M, Teng MW, Allard B, Stagg J, Smyth MJ (2014) Antimetastatic effects of blocking PD-1 and the adenosine A2A receptor. Cancer Res 74(14):3652–3658
Motawi TK, Sadik NAH, Hamed MA, Ali SA, Khalil WKB, Ahmed YR (2020) Potential therapeutic effects of antagonizing adenosine A2A receptor curcumin and niacin in rotenone-induced Parkinson’s disease mice model. Mol Cell Biochem 465(1–2):89–102
Naser AFA, Aziz WM, Ahmed YR, Khalil WKB, Hamed MAA (2022) Parkinsonism-like disease induced by rotenone in rats: treatment roleof curcumin dopamine agonist and adenosine A2A receptor antagonist. Curr Aging Sci 15(1):65–76
Martins I, Wang Y, Michaud M, Ma Y, Sukkurwala AQ, Shen S, Kepp O, Métivier D, Galluzzi L, Perfettini JL, Zitvogel L, Kroemer G (2014) Molecular mechanisms of ATP secretion during immunogenic cell death. Cell Death Differ 21(1):79–91
Dosch M, Gerber J, Jebbawi F, Beldi G (2018) Mechanisms of ATP release by inflammatory cells. Int J Mol Sci 19(4):1222
Denning NL, Aziz M, Gurien SD, Wang P (2019) DAMPs and NETs in sepsis. Front Immunol 30(10):2536
Yang D, He Y, Muñoz-Planillo R, Liu Q, Núñez G (2015) Caspase-11 requires the pannexin-1 channel and the purinergic P2X7 pore to mediate pyroptosis and endotoxic shock. Immunity 43(5):923–932
Ran Y, Su W, Gao F, Ding Z, Yang S, Ye L, Chen X, Tian G, Xi J, Liu Z (2021) Curcumin ameliorates white matter injury after ischemic stroke by inhibiting microglia/macrophage Pyroptosis through NF-κB suppression and NLRP3 inflammasome inhibition. Oxidative Med Cell Longev 30(2021):1552127
Ahmad I, Muneer KM, Tamimi IA, Chang ME, Ata MO, Yusuf N (2013) Thymoquinone suppresses metastasis of melanoma cells by inhibition of NLRP3 inflammasome. Toxicol Appl Pharmacol 270(1):70–76
Okamoto M, Liu W, Luo Y, Tanaka A, Cai X, Norris DA, Dinarello CA, Fujita M (2010) Constitutively Active inflammasome in human melanoma cells mediating autoinflammation via caspase-1 processing and secretion of interleukin-1β. J Biol Chem 285(9):6477–6488
Melnikova VO, Bar-Eli M (2009) Inflammation and melanoma metastasis. Pigment Cell Melanoma Res 22(3):257–267
Tengesdal IW, Menon DR, Osborne DG, Neff CP, Powers NE, Gamboni F, Mauro AG, D'Alessandro A, Stefanoni D, Henen MA, Mills TS, De Graaf DM, Azam T, Vogeli B, Palmer BE, Pietras EM, DeGregori J, Tan AC, Joosten LAB, Fujita M, Dinarello CA, Marchetti C (2021) Targeting tumor-derived NLRP3 reduces melanoma progression by limiting MDSCs expansion. Proc Natl Acad Sci U S A 118(10):e2000915118
Theivanthiran B, Evans KS, DeVito NC, Plebanek M, Sturdivant M, Wachsmuth LP, Salama AK, Kang Y, Hsu D, Balko JM, Johnson DB, Starr M, Nixon AB, Holtzhausen A, Hanks BA (2020) A tumor-intrinsic PD-L1/NLRP3 inflammasome signaling pathway drives resistance to anti–PD-1 immunotherapy. J Clin Invest 130(5):2570–2586
Zarogoulidis P, Yarmus L, Darwiche K, Walter R, Huang H, Li Z, Zaric B, Tsakiridis K, Zarogoulidis K (2013) Interleukin-6 cytokine: a multifunctional glycoprotein for cancer. Immunome Res 9(62):16535
Hoejberg L, Bastholt L, Johansen JS, Christensen IJ, Gehl J, Schmidt H (2012) Serum interleukin-6 as a prognostic biomarker in patients with metastatic melanoma. Melanoma Res 22(4):287–293
Vlaykova T, Kurzawski M, Tacheva T, Dimov D, Anastasov A, Vlaykova D, Miteva A, O’donoghue N, Drozdzik M (2020) Effects of the IL6 174G>C promoter polymorphism and IL 6 serum levels on the progression of cutaneous malignant melanoma. Oncol Lett 20(2):1781–1791
Tengesdal IW, Dinarello A, Powers NE, Burchill MA, Joosten LAB, Marchetti C, Dinarello CA (2021) Tumor NLRP3-derived IL-1β drives the IL-6/STAT3 Axis resulting in sustained MDSC-mediated immunosuppression. Front Immunol 31(12):661323
Xu J, Lin H, Wu G, Zhu M, Li M (2021) IL-6/STAT3 is a promising therapeutic target for hepatocellular carcinoma. Front Oncol 15(11):760971
Li W, Sun L, Lei J, Wu Z, Ma Q, Wang Z (2020) Curcumin inhibits pancreatic cancer cell invasion and EMT by interfering with tumor‑stromal crosstalk under hypoxic conditions via the IL‑6/ERK/NF‑κB axis. Oncol Rep 44(1):382–392
Jiang GM, Xie WY, Wang HS, Du J, Wu BP, Xu W, Liu HF, Xiao P, Liu ZG, Li HY, Liu SQ, Yin WJ, Zhang QG, Liang JP, Huang HJ (2015) Curcumin combined with FAPαc vaccine elicits effective antitumor response by targeting indolamine-23-dioxygenase and inhibiting EMT induced by TNF-α in melanoma. Oncotarget 6(28):25932–25942
Bill MA, Fuchs JR, Li C, Yui J, Bakan C, Benson DM Jr, Schwartz EB, Abdelhamid D, Lin J, Hoyt DG, Fossey SL, Young GS, Carson WE 3rd, Li PK, Lesinski GB (2010) The small molecule curcumin analog FLLL32 induces apoptosis in melanoma cells via STAT3 inhibition and retains the cellular response to cytokines with anti-tumor activity. Mol Cancer 9(1)
Mannino MH, Zhu Z, Xiao H, Bai Q, Wakefield MR, Fang Y (2015) The paradoxical role of IL-10 in immunity and cancer. Cancer Lett 367(2):103–107
Chhabra A, Chakraborty NG, Mukherji B (2008) Silencing of endogenous IL-10 in human dendritic cells leads to the generation of an improved CTL response against human melanoma associated antigenic epitope MART-127–35. Clin Immunol 126(3):251–259
MaruYama T, Kobayashi S, Shibata H, Chen W, Owada Y (2021) Curcumin analog GO-Y030 boosts the efficacy of anti-PD-1 cancer immunotherapy. Cancer Sci 112(12):4844–4852
Sawant DV, Yano H, Chikina M, Zhang Q, Liao M, Liu C, Callahan DJ, Sun Z, Sun T, Tabib T, Pennathur A, Corry DB, Luketich JD, Lafyatis R, Chen W, Poholek AC, Bruno TC, Workman CJ, Vignali DAA (2019) Adaptive plasticity of IL-10+ and IL-35+ Treg cells cooperatively promotes tumor T cell exhaustion. Nat Immunol 20(6):724–735
Yu R, Jin L, Li F, Fujimoto M, Wei Q, Lin Z, Ren X, Jin Q, Li H, Meng F, Jin G (2020) Dihydroartemisinin inhibits melanoma by regulating CTL/Treg anti-tumor immunity and STAT3-mediated apoptosis via IL-10 dependent manner. J Dermatol Sci 99(3):193–202
Giordano A, Tommonaro G (2019) Curcumin and cancer. Nutrients 11(10):23766
Bolger GT, Licollari A, Tan A, Greil R, Vcelar B, Greil-Ressler S, Weiss L, Schönlieb C, Magnes T, Radl B, Majeed M, Sordillo PP (2019) Pharmacokinetics of liposomal curcumin (Lipocurc™) infusion: effect of co-medication in cancer patients and comparison with healthy individuals. Cancer Chemother Pharmacol 83(2):265–275
FAqil F, Munagala R, Jeyabalan J, Agrawal AK, Gupta R (2017) Exosomes for the enhanced tissue bioavailability and efficacy of curcumin. AAPS J 19(6):1691–1702
Funding
This study was funded by grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (MDB; Grant: 310606/2021–7; AZ; Grant: 313311/2021–8), Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina (FAPESC) (MDB; Grant: 2021TR001726) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) (DM; Grant: Financial Code 001). MDB and AZ are 2 CNPq Research Fellows (PQ2). DM and GBS are supported by Fundo de Apoio à Manutenção e ao Desenvolvimento da Educação Superior and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for the scholarships. FAPESC, DECIT/CNPq/SES-SC, PPSUS, CAPES, CNPq-Brazil, CAPES, Federal University of Fronteira Sul (UFFS), Federal University of Santa Catarina (UFSC) and Biochemistry Graduate Course/UFSC-Brazil (PPGBQA/UFSC) supported grants and research scholarships. DM is registered as a PhD student on PPGBQA/UFSC.
Author information
Authors and Affiliations
Contributions
Conceptualization: DM, GBS, MDB, and MM.
Methodology: DM and GBS.
Investigation: DM, GBS, RAN, PDA, FM, JVC and LSM.
Visualization: DM, GBS, MDB and MM.
Funding acquisition: SFVOM, MDB and MM.
Project administration: MDB and MM.
Supervision: SFVOM, MDB, AZ and MM.
Writing – original draft: DM.
Writing – review and editing: DM, GBS, SFVOM, MDB, AZ and MM.
All authors reviewed and approved the final version.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Curcumin downregulates CD39 and CD73 ectonucleotidases in CM cells.
• Curcumin suppresses expression of A2A receptors in CM cells.
• Curcumin exerts regulatory effects on the immune response via the NLRP3 inflammasome and the inflammatory cascade.
• Curcumin demonstrates immunomodulatory properties by impacting adenosinergic signaling pathways.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Manica, D., da Silva, G.B., Narzetti, R.A. et al. Curcumin modulates purinergic signaling and inflammatory response in cutaneous metastatic melanoma cells. Purinergic Signalling (2024). https://doi.org/10.1007/s11302-024-10023-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11302-024-10023-0