Abstract
Introduction
The laparoscopic omentopexy has been described for the prevention of peritoneal dialysis catheter obstruction due to omental wrapping of the catheter. As there are some controversies and limited data regarding the outcomes of prophylactic omentopexy, we designed a study to evaluate the efficacy of prophylactic omentopexy in preventing catheter dysfunction in patients undergoing laparoscopic catheter placement.
Materials and methods
In this randomized clinical trial, patients with end-stage renal disease during 3 months were divided into two groups of peritoneal dialysis catheter implants with and without omentopexy and subsequently evaluated regarding postoperative features.
Results
A total of 43 patients were evaluated, including 22 undergoing prophylactic omentopexies. There was no significant difference among the baseline features of the patients. There was also no significant difference regarding postoperative features, including peritonitis, leakage, reoperation, need for catheter removal, and mortality.
Conclusion
Prophylactic omentopexy did not cause any significant differences in complications. In addition, there was no benefit for decreasing postoperative outflow obstruction due to omental wrapping following peritoneal dialysis catheter insertion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peritoneal dialysis is a well-known treatment method for end-stage renal disease (ESRD) [1]. In this method, a catheter is placed into the peritoneal cavity allowing dialysis [2]. However, obstruction, leakage, migration, and infectious complications have remained some of the most common causes of peritoneal dialysis failure, leading to catheter removal [3,4,5,6].
Various approaches have been described for catheter insertion, including the surgical methods, which consist of open and laparoscopic procedures, and percutaneous techniques (2). These approaches may affect the occurrence of complications. Laparoscopy seems superior to open surgery by reducing complications, inserting the catheter under direct vision, and allowing additional procedures, such as omentopexy and catheter fixation (4, 19).
Obstructions cause dialysate flow problems in between 6.0 and 20.5% of cases (10–13). Omental wrapping is one of the most important reasons for mechanical flow obstruction of catheters. Omental wrapping has been reported to occur between 57 and 92% of the time after laparoscopic salvage procedures (7–9). Omental wrapping usually causes peritoneal dialysis malfunction in two ways, one is to close the catheter holes, and the other is to rotate the omentum around the catheter and pull it to the upper areas of the abdomen, which reduces the possibility of fluid going in and out. Simple relocation with or without catheter fixation, omentopexy, and omentectomy are currently used laparoscopically to save catheters [7,8,9,10,11,12,13].
In the open abdominal surgery method, omentum resection was performed to prevent the catheter from being blocked by the omentum, but during laparoscopy, omentopexy can be easily performed, but there are controversies regarding the necessity of performing omentopexy for all patients. Some surgeons perform prophylactic omentopexy for all laparoscopic insertion of peritoneal dialysis catheter [14], but others [15] believe it may be necessary for some percent of patients with long and large omentum. There are limited studies in the literature reporting the outcomes of prophylactic omentopexy as a method to prevent catheter dysfunction [14, 16,17,18]. In this procedure, the omentum is fixed to the abdominal wall as a possible way to avoid omental wrapping and obstruction, which can lead to catheter dysfunction [14]. Therefore, by designing a randomized clinical trial, we evaluated the efficacy of prophylactic omentopexy in patients undergoing laparoscopic catheter placement.
Materials and methods
Study design and participants
This study is a non-inferiority, double-blind randomized clinical trial on ESRD patients’ candidate for laparoscopic peritoneal dialysis for catheter placement in a quarterly period. The subjects were selected among patients referring to Imam Khomeini Hospital, the referral center of surgery affiliated with Tehran University of Medical Sciences, from August 2016 to July 2017. The patients were evaluated for a 3-month period. The inclusion criteria consisted of all patients referred to us for dialysis catheter insertion, while patients with a previous history of intra-abdominal surgery, and unstable conditions such as low ejection fraction, which required prompt intervention were excluded from our study. The total number of peritoneal dialysis patients was 67, which was considered the total sample population. Patients were divided into two groups of omentopexy (Intervention) and without omentopexy (Control) based on block randomization and were evaluated accordingly.
Surgical intervention
Patients are fasted for 8 h before the operation. For prophylactic antibiotics, 1 g of Cefazolin is used. The patient is placed in a supine Trendelenburg position and placed under general anesthesia. Catheter incision is located in the area 2 to 3 cm outside and below the umbilicus (on the right or left) and should be on the inner edge of the rectus muscle to avoid possible damage to the epigastric arteries. CO2 gas is utilized for insufflation with an 80–100 mmHg pressure. The catheter exit site must be downward, with the smallest possible incision should be made so that the surrounding skin is firmly attached to it. The distance of the upper cuff from the exit of the catheter should not be less than 4 cm. Subsequently, Normal Saline with 1000 units of heparin enters the abdominal cavity to evaluate fluid evacuation. If the fluid circulation is satisfactory, the catheter head connections are connected, and dressing at the catheter site is applied to prevent the catheter and subcutaneous cuff from moving. For omentopexy, the omentum is fixed to the peritoneum of upper abdomen by one to three vicryl sutures, depending on the size of the omentum. The surgical method has been described in our previous reports. [18] All cases were subjected to the laparoscopic techniques and operated by a single experienced surgeon. Other than rectus sheet tunneling and omentopexy, no other inversion was performed.
Postoperative measures
On the day of the operation, a flat abdomen X-ray is taken from the patient for the evaluation of the catheter location in the first hours after the operation to be a criterion for comparison with the patient’s subsequent X-rays. Catheter washing with heparin-containing serum is performed by a peritoneal dialysis nurse on the day of surgery, the day after, and then once a week and 2 weeks later, peritoneal dialysis can be started. A dressing at the catheter exit site once a week for up to 2 weeks is sufficient if there is no fluid leakage.
Data collection
The present study included demographic and clinical information of the patient, such as age, sex, frequency of dialysis fluid inflow and outflow, length, size and volume of omentum, complications during catheter implantation, such as bleeding, and postoperative complications such as outflow obstruction, peritonitis, leakage, and primary malposition of the catheter. Follow-up evaluations included post-surgical complications, the need for catheter removal or rescue procedure, mortality, or transplantation. Each patient was followed for a period of at least 3 months. Furthermore, occurrence of any outcomes such as mortality or transplantation was documented till the end of our study period. In this study, both the patients and the researcher were blinded to the patients grouping, while only the surgeon was not blinded.
Statistics
The sample size was calculated based on the study of Crabtree et al. [15] with the predicted complication rate of 12.8% and 0.7% in the non-omentopexy and omentopexy arms, respectively, and with the non-inferiority margin of 7.5%, the sampling ratio of 1, power of 80%, and type 1 error of 5%, we calculated 20 patients needed in each arm. With the assumption of about a 10% drop-out rate, we enrolled 22 patients in each group. Measurement data were described by mean ± standard deviation (SD), and numerical data were described by number (%). Statistical differences were assessed using Pearson’s Chi-square or Fisher’s exact tests as categorical variables, as appropriate. The paired-sample t-test was used to evaluate the changes in clinical indices before and after the intervention. Data analysis is performed using SPSS software, and the significance level in this study was considered less than %5.
Ethical approval
The study was approved by the ethics committee of Tehran University of Medical Sciences (IR.TUMS.VCR.REC.1395.247), the institutional review board, and the Clinical Trial Registry (NCT02879734 at ClinicalTrials.gov). It was conducted in compliance with local regulatory requirements, Good Clinical Practice (GCP), and the Declaration of Helsinki. Written informed consent was obtained from all patients or their legally authorized representatives.
Results
In the present study, out of 67 patients, 24 were excluded based on the exclusion criteria; the remaining patients were divided into 2 groups, 21 patients without omentopexy and 22 patients with omentopexy during peritoneal dialysis catheter implantation (Fig. 1). There was no significant difference between the two groups regarding their gender, age, and cause of renal failure. In addition, there was no significant difference between the two groups regarding the potential risk factors for omental wrapping, including the length and bulk of omentum, intraoperative bleeding, color of outflow irrigating saline, and primary position of the catheter in the postoperative graph between the two groups (Table 1).
Regarding the postoperative complications, the omentopexy group had lower rates of peritonitis and dialysis fluid leakage from around the catheter compared to the control group; however, no statistically significant difference was observed (P = 0.345 and 0.108, respectively).
As demonstrated in Table 1, although the omentopexy group demonstrated higher rates of impaired inflow and outflow disorder compared to the control group, no statistical difference was achieved (P = 1.000 and 0.698, respectively).
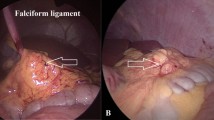
In both groups, five patients required catheter surgery reoperation and correction (P = 1.000). Out of five patients in the omentopexy group, three patients underwent reoperation due to adhesions caused by appendices epiploicae and fallopian tubes (one patient and two patients, respectively), and two patients underwent reoperation due to fibrin clot.
In the control group, out of five patients, one patient underwent reoperation due to adhesions caused by appendices epiploicae, and four underwent reoperation due to fibrin clot. However, none of the re-surgery cases was caused by omental wrapping.
In both groups, four patients had signs and symptoms of peritonitis (including new onset of abdominal pain, fever, and cloudy effluent), all of them were controlled with antibiotic treatment.
The patients’ outcomes were documented after the 3-month follow-up period until the end of our study period, ranging till a maximum of 1 year. During the first 3-month follow-up of all patients, no cases of mortality or transplantation was observed. However, beyond this period, the mortality in our study was four cases, which were due to comorbid disease (ESRD and chronic heart disease); also, four patients in the omentopexy group and three patients in the control group underwent kidney transplantation during treatment.
Discussion
Various methods have been introduced for peritoneal catheter insertion without a consensus on the optimal procedure; however, the laparoscopic approach seems superior to other techniques [4]. Besides, laparoscopic catheter insertion itself can be divided into two methods: advanced laparoscopy, introduced by Crabtree and Fishman [19], may consist of rectus sheath tunneling and additional procedures, including omentopexy and adhesiolysis, while basic laparoscopy is just verifying the catheter position by laparoscope [20]. A meta-analysis by Shrestha et al. [20] compared the advanced laparoscopic catheter insertion with basic laparoscopy and open procedure, which showed a lower incidence of catheter obstruction and migration in advanced laparoscopy. Therefore, the superiority of advanced laparoscopy may be emphasized mainly due to the possible additional procedures.
Herein, we designed a clinical trial with 43 patients randomly divided into 2 groups to determine the effect of omentopexy as one of these additional procedures. We observed that the postoperative complications, the need for catheter removal, and inflow and outflow failure were not significantly different between the study and control groups. In addition, it is worth noting that none of the postoperative flow obstruction or complications was due to omentopexy features. Interestingly, none of the flow obstructions was due to omental wrapping. Obstructed cases in our study were primarily due to fibrin clots and adhesion of appendicular epiploica or fallopian tube to the holes of the catheter. The length and volume (or bulk) of omentum have not shown any direct effect on omental wrapping. The two groups were the same regarding some other risk factors that could cause flow obstruction such as intraoperative bleeding, and improper primary position of the catheter among catheter insertion.
We suggest that omentopexy should not be performed as prophylaxis in the initial operation, even for patients with long and bulky omentum. We believe if the patient develops catheter dysfunction, this procedure should be considered in the next operation; since our results demonstrated that postoperative outflow obstruction has some other important reasons such as appendicular epiploica and fallopian tube and fibrin clot, and we could not decrease the risk of them with omentopexy. There was no significant decrease in the rate of complications and flow obstruction and reoperation for patients with omentopexy versus without omentopexy.
Some studies compared the combination of rectus sheath tunneling and selective additional procedures with basic laparoscopy. Krezalek et al. [16] compared patients who underwent basic laparoscopy using selective adhesiolysis with advanced laparoscopy using rectus sheath tunneling, selective omentopexy, and adhesiolysis. In the advanced laparoscopy group, all patients underwent rectus sheath tunneling, while only 49 (53.3%) and 25 (27.2%) underwent omentopexy and adhesiolysis, respectively. The authors reported a significant difference in mechanical catheter dysfunction (4.4%) in the advanced laparoscopy compared to 14 (17.5%) in the basic laparoscopy, and that rectus sheath tunneling was shown to be notably effective as an independent preventive factor for catheter dysfunction [16]. Besides, in two similar studies by Attaluri et al. [21] and Crabtree and Fishman [19], similar results of lower complications and catheter dysfunction in advanced laparoscopy with selective additional procedures were achieved. These studies demonstrate the effective role of rectus sheath tunneling alongside selective procedures; however, the effect of omentopexy alone, as an additional procedure, cannot be statistically evaluated.
Limited studies have been designed among published literature to evaluate the efficacy of omentopexy compared to a control group without omentopexy. A study by Ogünç [14] introduced a technique for laparoscopic insertion of the peritoneal catheter as one of the first studies describing the omentopexy to prevent omental wrapping and catheter dysfunction. In the mentioned study, the omentum was fixed to the lateral abdominal wall on two points, and no catheter dysfunction was reported in the follow-up. In the study by Crabtree and Fishman [19], the authors described a criterion to perform omentopexy selectively. They performed omentopexy when the omentum was extended to the retrovesical space. As a result, in 9.2% of patients (14/153) in the omentopexy group, omentopexy was done, and only 0.7% of patients (1/153) in the omentopexy group had catheter obstruction compared to 12.8% rate (10/78) in the group without omentopexy. In another study by Cao et al. [17], prophylactic omentopexy was done by Hem-o-loks. They reported no obstruction, migration, and exit-site infection while two cases had leakage; they suggested that rectus sheath tunneling may prevent the leakage in those cases. However, there was no comparison with a control group to determine the efficacy of prophylactic omentopexy in these studies. In addition, in another study by van Laanen et al. [22], they added catheter fixation and omentopexy to their standard laparoscopic insertion, which included rectus sheath tunneling. In the advanced group (n = 32), in 7 patients, only catheter fixation, 5, only omentopexy, and 20 patients, both procedures were added to their standard method. The postoperative complications in the mentioned study were similar between the advanced (2/32, 6%) and standard (3/46, 7%) procedures (p value = 1.0). Although not all of the patients in the advanced group in the study by van Laanen et al. [22] underwent omentopexy, their results were relatively in line with our research.
Based on this study, it is suggested that omentopexy should not be performed prophylactically in the first surgery; if catheter malfunction occurs, it should be performed in the reoperation; since our results demonstrated that even with omentopexy, the rate of complications and reoperation did not decrease.
As in most of the studies that compared the outcomes of advanced with basic laparoscopy, omentopexy is not the only difference between the groups; further studies evaluating the effect of each additional procedure in the laparoscopic insertion of the peritoneal catheter are suggested. The results may lead to achieving the most efficient catheter insertion method.
Limitation of the study
We evaluated the effectiveness of omentopexy on catheter insertion in a randomized clinical trial with 43 cases. However, future multicentric studies with a larger sample size are suggested regarding this issue. In addition, our main follow-up duration was 3 months based on our experience that the main complications such as omental wrapping following omentopexy occurs during the initial weeks and during the short follow-up duration after surgery. Nevertheless, additional longitudinal studies with longer follow-up durations are required. Other factors such as the patient’s comorbidities, drug history, type of instrument used, and suture techniques can also vary among centers and surgeons, affecting the overall results. Further meta-analysis and randomized controlled studies are needed to determine the efficacy of other additional procedures to achieve an optimal laparoscopic approach for peritoneal catheter insertion.
Conclusion
We suggest that omentopexy should not be performed as a prophylaxis measure in the initial operation, and if the patient develops catheter dysfunction, this procedure should be considered in the next operation. Complications of peritoneal dialysis catheters may vary depending on the catheter insertion technique. Although it may be expected that omentopexy lead to lower rates of catheter dysfunction, especially by avoiding omental wrapping, our investigation did not show any significant differences between the groups, with and without omentopexy, concerning morbidity and mortality. In addition, further clinical trials to achieve an optimal laparoscopic approach for peritoneal catheter insertion are suggested.
Availability of data and materials
All data regarding this case report has been reported in the manuscript. Please contact the corresponding author in case of requiring any further information.
References
Mehrotra R, Devuyst O, Davies SJ, Johnson DW (2016) The current state of peritoneal dialysis. J Am Soc Nephrol 27(11):3238–3252
Esagian SM, Sideris GA, Bishawi M, Ziogas IA, Lehrich RW, Middleton JP, Suhocki PV, Pappas TN, Economopoulos KP (2021) Surgical versus percutaneous catheter placement for peritoneal dialysis: an updated systematic review and meta-analysis. J Nephrol 34(5):1681–1696
Crabtree JH, Chow KM (2017) Peritoneal dialysis catheter insertion. Semin Nephrol 37(1):17–29
Hagen SM, Lafranca JA, Steyerberg EW, JN IJ, Dor FJ (2013) Laparoscopic versus open peritoneal dialysis catheter insertion: a meta-analysis. PLoS ONE 8(2):e56351
Keshvari A, Fazeli MS, Meysamie A, Seifi S, Taromloo MK (2010) The effects of previous abdominal operations and intraperitoneal adhesions on the outcome of peritoneal dialysis catheters. Perit Dial Int J Int Soc Perit Dial 30(1):41–45
Javid MJ, Rahimi M, Keshvari A (2011) Dissociative conscious sedation, an alternative to general anesthesia for laparoscopic peritoneal dialysis catheter implantation: a randomized trial comparing intravenous and subcutaneous ketamine. Perit Dial Int J Int Soc Perit Dial 31(3):308–314
Amerling R, Maele DV, Spivak H, Lo AY, White P, Beaton H, Rudick J (1997) Laparoscopic salvage of malfunctioning peritoneal catheters. Surg Endosc 11(3):249–252
Lee M, Donovan JF (2002) Laparoscopic omentectomy for salvage of peritoneal dialysis catheters. J Endourol 16(4):241–244
Barone GW, Johnson DD, Webb JW (1998) A practical approach to laparoscopic surgery for malfunctioning peritoneal dialysis catheters. J Laparoendosc Adv Surg Tech A 8(1):19–23
Chao SH, Tsai TJ (1993) Laparoscopic rescue of dysfunctional Tenckhoff catheters in continuous ambulatory peritoneal dialysis patients. Nephron 65(1):157–158
Crabtree JH, Fishman A (1999) Videolaparoscopic implantation of long-term peritoneal dialysis catheters. Surg Endosc 13(2):186–190
Julian TB, Ribeiro U, Bruns F, Fraley D (1995) Malfunctioning peritoneal dialysis catheter repaired by laparoscopic surgery. Perit Dial Int J Int Soc Perit Dial 15(8):363–366
Ogunc G (2002) Malfunctioning peritoneal dialysis catheter and accompanying surgical pathology repaired by laparoscopic surgery. Perit Dial Int J Int Soc Perit Dial 22(4):454–462
Ogunc G (2001) Videolaparoscopy with omentopexy: a new technique to allow placement of a catheter for continuous ambulatory peritoneal dialysis. Surg Today 31(10):942–944
Crabtree JH, Fishman A (2003) Selective performance of prophylactic omentopexy during laparoscopic implantation of peritoneal dialysis catheters. Surg Laparosc Endosc Percutan Tech 13(3):180–184
Krezalek MA, Bonamici N, Lapin B, Carbray J, Velasco J, Denham W, Linn J, Ujiki M, Haggerty SP (2016) Laparoscopic peritoneal dialysis catheter insertion using rectus sheath tunnel and selective omentopexy significantly reduces catheter dysfunction and increases peritoneal dialysis longevity. Surgery 160(4):924–935
Cao W, Tu C, Jia T, Liu C, Zhang L, Zhao B, Liu J, Zhang L (2019) Prophylactic laparoscopic omentopexy: a new technique for peritoneal dialysis catheter placement. Ren Fail 41(1):113–117
Keramati MR, Abbaszadeh-Kasbi A, Keshvari A (2018) Laparoscopic omentopexy, rectus sheath tunneling and implantation of the peritoneal dialysis catheter using a peritoneal dialysis port. Perit Dial Int 38(3):187–191
Crabtree JH, Fishman A (2005) A laparoscopic method for optimal peritoneal dialysis access. Am Surg 71(2):135–143
Shrestha BM, Shrestha D, Kumar A, Shrestha A, Boyes SA, Wilkie ME (2018) Advanced laparoscopic peritoneal dialysis catheter insertion: systematic review and meta-analysis. Perit Dial Int: J Int Soc Perit Dial 38(3):163–171
Attaluri V, Lebeis C, Brethauer S, Rosenblatt S (2010) Advanced laparoscopic techniques significantly improve function of peritoneal dialysis catheters. J Am Coll Surg 211(6):699–704
van Laanen JHH, Litjens EJ, Snoeijs M et al (2022) Introduction of advanced laparoscopy for peritoneal dialysis catheter placement and the outcome in a University Hospital. Int Urol Nephrol 54:1391–1398. https://doi.org/10.1007/s11255-021-03020-4
Acknowledgements
This study was the subject of surgical residency speciality dissertation of Fakhroddin Kiani.
Funding
No financial support was received for this report.
Author information
Authors and Affiliations
Contributions
AK and MRK designed the study and carried out the therapeutic measures. FK, and SMMY collected the data and revised the manuscript. RS analyzed the data and HK and AM drafted the manuscript. AK and RS revised and proofread the manuscript. All the authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Amir Keshvari, Seyed Mostafa Meshkati Yazd, Mohammad Reza Keramati, Hooman Kamran, Reza Shahriarirad, Azam Miveforoshan, and Fakhroddin Kiani have no conflicts of interest or financial ties to disclose.
Ethical approval and consent to participate
The present study was approved by the Medical Ethics Committee of Tehran University of Medical Sciences. The purpose of this study was completely explained to the patient and was assured that her information will be kept confidential by the researchers. A written consent form was also obtained from the patient.
Consent for publication
Written informed consent was obtained from the patients for publication of this report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keshvari, A., Meshkati Yazd, S., Keramati, M.R. et al. Evaluation of the effectiveness of prophylactic omentopexy during laparoscopic insertion of peritoneal dialysis catheter: a case–control clinical trial. Int Urol Nephrol 55, 2083–2089 (2023). https://doi.org/10.1007/s11255-023-03522-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03522-3