Abstract
We investigated the impact of suboptimal platelet reactivity on clinical outcomes after percutaneous coronary intervention (PCI). We enrolled 500 patients with stable coronary artery disease undergoing elective PCI. Platelet reactivity was measured before PCI using the VerifyNow P2Y12 assay. Primary endpoint was the incidence of ischemic or bleeding events at 1 month and 5 years. Patients with high platelet reactivity (HPR) showed significantly higher rates of ischemic events both during the 1st month after PCI (HR 2.06, 95% CI 1.02–4.06), and beyond 1 month compared with patients without HPR (HR 1.73, 95% CI 1.02–2.95). Conversely, compared with patients without low platelet reactivity (LPR), patients with LPR presented significantly higher rates of bleeding only during the 1st month (HR 3.67, 95% CI 1.68–8.02). In conclusion, pre-procedural HPR is associated with ischemic events even beyond the 1st month after PCI. The association of LPR with bleeding events seems to be confined to the periprocedural period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination of clopidogrel and aspirin is still the antiplatelet treatment of choice for patients with stable coronary artery disease (CAD) undergoing percutaneous coronary intervention (PCI) [1]. However, due to a large inter-individual variability in the response to antiplatelet agents [2], a significant proportion of these patients present suboptimal platelet reactivity at the time of PCI. We have previously shown that among clopidogrel-treated patients undergoing elective PCI, specific thresholds of platelet reactivity could be identified using the VerifyNow P2Y12 assay to define high platelet reactivity [HPR; P2Y12 reaction units (PRU) ≥ 240], which was associated with increased risk of ischemic events, and low platelet reactivity (LPR; PRU ≤ 178), which was associated with increased risk of bleeding events at 1 month follow-up [3]. These results were confirmed in a pooled analysis of > 20,000 patients, where, although using different thresholds for HPR and LPR definition (PRU > 208 and < 85, respectively), platelet reactivity was able to identify PCI-treated patients at higher risk of death and ST or at higher risk of bleeding [4]. The impact of suboptimal pre-PCI platelet reactivity, either high or low, on very long-term clinical outcomes is however largely unknown.
Methods
Patients population
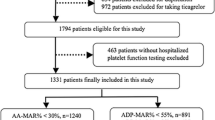
In this study we prospectively enrolled 500 consecutive patients with stable CAD undergoing elective PCI from 2010 to 2011 at Campus Bio-Medico University, Rome, Italy.
Treatment protocol
All patients received clopidogrel, either a 600-mg loading dose ≥ 6 h before intervention or a maintenance dose of 75 mg/day for at least 5 days. Patients on chronic treatment did not receive any further loading dose of clopidogrel. Technicalities of the procedure, including use of the radial approach, drug eluting stents, and glycoprotein IIb/IIIa inhibitors, were left to the operator’s discretion. Procedural anticoagulation consisted of unfractionated heparin administrated to achieve an activated clotting time of 250–300 s. Procedural success was defined as a reduction in percent diameter stenosis to below 30% in the presence of thrombolysis in myocardial infarction (TIMI) flow grade 3 in the main vessel and all side branches > 2 mm in diameter. After PCI, patients receiving bare-metal stents (BMS) received clopidogrel 75 mg/day for at least 4 weeks, whereas those receiving drug-eluting stents (DES) were prescribed clopidogrel for 12 months. All patients were on aspirin treatment before intervention and continued aspirin (80–100 mg/day) indefinitely. Patients with upstream use of glycoprotein IIb/IIIa inhibitors, treatment with oral anticoagulant drugs, platelet count < 70 × 109/L, high bleeding risk (active internal bleeding, history of hemorrhagic stroke, intracranial neoplasm, arteriovenous malformation or aneurysm, ischemic stroke in the previous 3 months), coronary artery bypass surgery in the previous 3 months, and severe renal failure (serum creatinine > 2 mg/dL) were excluded. This study was approved by the local ethics committee, with all patients giving written informed consent.
Platelet function analysis
Platelet reactivity was measured immediately before PCI using the VerifyNow P2Y12 assay, with results expressed as PRUs. HPR was defined in the presence of PRU values ≥ 240, whereas LPR was defined in the presence of PRU values ≤ 178. Consistently, normal platelet reactivity (NPR) was defined in the presence of PRU values between 179 and 239 [3].
Study endpoints
Clinical follow-up data were obtained up to 5 years by means of office visit, telephone interview, or chart review. All events were classified and adjudicated by a physician not involved in the follow-up process. Endpoint of this study was the incidence of ischemic or bleeding events [3] at 1 month and 5 years. Ischemic events were defined as death, myocardial infarction (MI), or target vessel revascularization (TVR). MI included both periprocedural and spontaneous events and were defined according to the third universal definition [5]. TVR was clinically driven and included bypass surgery or repeat PCI of the target vessel(s). Definite stent thrombosis (ST) was also recored and defined according to the Academic Research Consortium definition [6]. Bleeding events included TIMI major bleeding [7], or large entry-site hematoma (> 10 cm in diameter). Entry-site hematomas were repeatedly monitored throughout the hospitalization, and the largest size detected was used for the analysis.
Statistics
Statistical analysis was performed using STATA/IC software, version 13 (STATA Corp., College Station, Texas). Continuous variables are expressed as mean ± SD or median [interquartile range]. Categorical variables are reported as frequencies and percentages. Student’s t test or Mann–Whitney test were used to compare continuous variables, as appropriate. Comparisons between categorical variables were evaluated using two-tailed Fisher’s exact test or Pearson’s χ2 test, as appropriate. Event rates were evaluated by the Kaplan–Meier method and Cox proportional hazard analysis, adjusting for diabetes mellitus, multivessel disease, chronic kidney disease (defined as glomerular filtration rate < 60 mL/min/1.73 m2), total stent length, and GP IIb/IIIa antagonists. Landmark analyses (survival method) of the Kaplan–Meier estimates of clinical outcomes during the 1st year and from 1 month to 5 years were performed for different platelet reactivity groups. A p value < 0.05 was considered statistically significant.
Results
Patients population
A total of 170 (32.4%) patients presented with HPR, whereas 160 (30.0%) had LPR and 170 (32.4%) had NPR. Main clinical and procedural feature are reported in Table 1. Patients with HPR had higher body mass index compared with patients without HPR, and presented more frequently diabetes mellitus and multivessel disease. No major differences were observed between patients with and without LPR.
Follow-up data
Clinical follow-up was complete in 471 (94.2%). Patients experiencing ischemic and bleeding events at 5-year follow-up were 86 (17.2%) and 49 (9.8%), respectively. Ischemic events occurred in 41 (25.3%) patients with HPR and in 44 (14.2%) patients without HPR [hazard ratio (HR) 1.89; 95% confidence interval (CI) 1.21–2.90; p = 0.005; Fig. 1]. HPR was associated with significantly higher rates of MI (17.9 versus 7.8%; HR 2.22, 95% CI 1.28–3.85; p = 0.004) and definite ST (3.1 versus 0.3%; HR 9.75, 95% CI 1.21–2.90; p = 0.041), whereas no significant differences were observed in death and TVR rates between patients with and without HPR (Table 2). Bleeding events occurred in 25 (16.6%) patients with LPR and in 24 (7.5%) patients without LPR (HR 2.66; 95% CI 1.49–4.73; p = 0.001; Fig. 1). LPR was associated with significantly higher rates of entry site hematomas (9.9 versus 2.8%; HR 3.22, 95% CI 1.55–6.68; p = 0.002), whereas there were no differences in the rates of major bleeding between patients with and without LPR (Table 2). Table 3 reports the incidence of ischemic and bleeding events in the three groups of patients with LPR, NPR and HPR.
Landmark analysis
A landmark analysis of the Kaplan–Meier estimates of clinical outcomes during the 1st month and from 1 month to 5 years is provided in Fig. 2. Patients with HPR showed significantly higher rates of ischemic events both during the 1st month after PCI (HR 2.06, 95% CI 1.02–4.06; p = 0.045), and from 1 month to 5 years compared with patients without HPR (HR 1.73, 95% CI 1.02–2.95; p = 0.038). Conversely, patients with LPR presented significantly higher rates of bleeding during the 1st month (HR 3.67, 95% CI 1.68–8.02; p = 0.001) compared with patients without LPR, whereas similar rates of bleeding were observed from 1 month to 5 years (HR 1.37, 95% CI 0.57–3.26; p = 0.496). These results remained substantially unchanged when the PRU > 208 threshold was used for the definition of HPR and PRU < 85 threshold was used for the definition of LPR.
Discussion
This is the first study assessing the impact of pre-procedural platelet reactivity on long-term outcomes following elective PCI. Main findings of our study are that pre-PCI platelet reactivity is able to predict 5-year clinical outcomes of stable CAD patients treated with clopidogrel; however, while HPR is associated with increased risk of ischemic events even beyond the 1st month from PCI, with a continuous divergence between the Kaplan–Meier curves of patients with and without HPR, the association of LPR with bleeding events seems to be confined to the periprocedural period.
Our results corroborate the concept that HPR is a marker of risk for post-PCI ischemic events, retaining a negative prognostic value even long after the revascularization and beyond the period of treatment with clopidogrel. In this perspective, the known association of HPR on clopidogrel with increased baseline platelet aggregation, enhanced inflammatory status, and other clinical conditions that are intrinsically related to worse outcomes (e.g. diabetes mellitus, endothelial dysfunction, coronary microvascular impairment) [8,9,10,11,12], could in part explain its negative prognostic value. Moreover, HPR is associated with an increased risk of periprocedural myocardial injury [10, 13,14,15], which in turn has a detrimental impact on long-term clinical outcomes after PCI [16, 17]. Although previous clinical trials have failed to demonstrate a clinically relevant benefit of adapting antiplatelet therapy based on the presence of HPR [18,19,20], recent studies have shown the potential of more intensive antiplatelet agents to improve coronary microvascular function [21] and peripheral endothelial function in patients treated with PCI [22]. In this perspective, the selective use of prasugrel or ticagrelor in stable patients with HPR and other high-risk features might prove effective in improving clinical outcomes, and should therefore be the objective of specific investigation.
The persistent association of HPR with ischemic events over time could also provides the rationale for prolonging dual antiplatelet therapy beyond standard duration. Although the optimal duration of dual antiplatelet therapy is still a matter of debate, it is commonly accepted that the decision to withdraw or continue clopidogrel in association with aspirin in stable CAD patients treated with PCI should be based on a thorough evaluation of their risk profile, considering both clinical and procedural variables. At least in patients without an increased risk of bleeding, prolonging dual antiplatelet therapy based on the presence of HPR might confer protection from recurrent ischemic events, as it has already been proven in patients with prior MI [23]. The attempt to find the optimal trade-off between ischemic and bleeding events following PCI, and therefore to guide the duration of dual antiplatelet therapy, has led to the development of several prognostic models and scores, which may help to individualize therapeutic strategies [24, 25]. The addition of platelet reactivity to clinical and procedural variables may confer additional predictive value to these models [26].
Our results are reassuring with respect to the bleeding hazard in patients who over-respond to clopidogrel treatment, as LPR does not seem to imply an increased risk of major bleeding on the long run. Moreover, the excess of bleeding observed in our study within the 1st month after PCI was mainly driven by access site complications. It should be noted, however, that the vast majority of our patients underwent PCI via the femoral route; it is presumable that different results would be yielded with the adoption of radial approach as the standard access site strategy.
This study has a number of limitations that need consideration. First, platelet reactivity was only assessed prior to PCI; the prognostic impact of platelet reactivity at different timings remains therefore unknown. Second, nearly one-third of our patients received BMS, which is now an obsolete practice; it cannot be excluded that the use of new-generation DES might alternatively modulate the impact on platelet reactivity on clinical outcomes. Moreover, the presence of both patients treated with BMS and DES implies a different exposure length to dual antiplatelet therapy after PCI. Nevertheless, therapeutic adherence following stent type-based indications was > 80% for both patients receiving BMS and DES. Third, the use of the femoral route as the access site of choice might have led to higher bleeding rates compared to what would be expected with a routine radial approach.
Overall, our study suggests that, unlike LPR, HPR carries prognostic significance long after coronary revascularization. Whether modulating the type and duration of antiplatelet treatment based on this information could improve patients’ outcomes may become a matter of future investigation.
References
Authors/Task Force Members, Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A (2014) 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 35:2541–2619
Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Alfonso F, Macaya C, Bass TA, Costa MA (2007) Variability in individual responsiveness to clopidogrel: clinical implications, management, and future perspectives. J Am Coll Cardiol 49:1505–1516
Mangiacapra F, Patti G, Barbato E, Peace AJ, Ricottini E, Vizzi V, Gatto L, D’Ambrosio A, De Bruyne B, Wijns W, Di Sciascio G (2012) A therapeutic window for platelet reactivity for patients undergoing elective percutaneous coronary intervention: results of the ARMYDA-PROVE (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty-Platelet Reactivity for Outcome Validation Effort) study. JACC Cardiovasc Interv 5:281–289
Aradi D, Kirtane A, Bonello L, Gurbel PA, Tantry US, Huber K, Freynhofer MK, ten Berg J, Janssen P, Angiolillo DJ, Siller-Matula JM, Marcucci R, Patti G, Mangiacapra F, Valgimigli M, Morel O, Palmerini T, Price MJ, Cuisset T, Kastrati A, Stone GW, Sibbing D (2015) Bleeding and stent thrombosis on P2Y12-inhibitors: collaborative analysis on the role of platelet reactivity for risk stratification after percutaneous coronary intervention. Eur Heart J 36:1762–1771
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Joint ESCTFFUDOMI, Authors/Task FMC, Thygesen K, Alpert JS, White HD, Biomarker S, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman ECGS., Clemmensen BR, Johanson PM, Hod P, Imaging H, Underwood S, Bax R, Bonow JJ, Pinto JJ, Gibbons F, Classification RJ, Fox S, Atar KA, Newby D, Galvani LK, Hamm M, Intervention CW, Uretsky S, Steg BF, Wijns PG, Bassand W, Menasche JP, Ravkilde P, Trials J, Ohman RS, Antman EM, Wallentin EM, Armstrong LC, Simoons PW, Trials ML, Januzzi RS, Nieminen JL, Gheorghiade MS, Filippatos M, Trials G, Luepker RS, Fortmann RV, Rosamond SP, Levy WD, Wood D, Trials D, Smith RS, Hu SC, Lopez-Sendon D, Robertson JL, Weaver RM, Tendera D, Bove M, Parkhomenko AA, Vasilieva AN, Mendis EJ S, ESC Committee for Practice Guidelines CPG, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Document R, Morais J, Aguiar C, Almahmeed W, Arnar DO, Barili F, Bloch KD, Bolger AF, Botker HE, Bozkurt B, Bugiardini R, Cannon C, de Lemos J, Eberli FR, Escobar E, Hlatky M, James S, Kern KB, Moliterno DJ, Mueller C, Neskovic AN, Pieske BM, Schulman SP, Storey RF, Taubert KA, Vranckx P, Wagner DR (2012) Third universal definition of myocardial infarction. J Am Coll Cardiol 60:1581–1598
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, McFadden E, Lansky A, Hamon M, Krucoff MW, Serruys PW, Academic RC (2007) Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 115:2344–2351
Rao AK, Pratt C, Berke A, Jaffe A, Ockene I, Schreiber TL, Bell WR, Knatterud G, Robertson TL, Terrin ML (1988) Thrombolysis in Myocardial Infarction (TIMI) Trial—phase I: hemorrhagic manifestations and changes in plasma fibrinogen and the fibrinolytic system in patients treated with recombinant tissue plasminogen activator and streptokinase. J Am Coll Cardiol 11:1–11
Hamilos M, Muller O, Ntalianis A, Trana C, Bartunek J, Sarno G, Mangiacapra F, Dierickx K, Meeus P, Cuisset T, De Bruyne B, Wijns W, Barbato E (2011) Relationship between peripheral arterial reactive hyperemia and residual platelet reactivity after 600 mg clopidogrel. J Thromb Thrombolysis 32:64–71
Mangiacapra F, Patti G, Peace A, Gatto L, Vizzi V, Ricottini E, D’Ambrosio A, Muller O, Barbato E, Di Sciascio G (2010) Comparison of platelet reactivity and periprocedural outcomes in patients with versus without diabetes mellitus and treated with clopidogrel and percutaneous coronary intervention. Am J Cardiol 106:619–623
Mangiacapra F, De Bruyne B, Muller O, Trana C, Ntalianis A, Bartunek J, Heyndrickx G, Di Sciascio G, Wijns W, Barbato E (2010) High residual platelet reactivity after clopidogrel: extent of coronary atherosclerosis and periprocedural myocardial infarction in patients with stable angina undergoing percutaneous coronary intervention. JACC Cardiovasc Interv 3:35–40
Mangiacapra F, Barbato E (2013) Clinical implications of platelet-vessel interaction. J Cardiovasc Transl Res 6:310–315
Muller O, Hamilos M, Bartunek J, Ulrichts H, Mangiacapra F, Holz JB, Ntalianis A, Trana C, Dierickx K, Vercruysse K, De Bruyne B, Wijns W, Barbato E (2010) Relation of endothelial function to residual platelet reactivity after clopidogrel in patients with stable angina pectoris undergoing percutaneous coronary intervention. Am J Cardiol 105:333–338
Mangiacapra F, Barbato E, Patti G, Gatto L, Vizzi V, Ricottini E, D’Ambrosio A, Wijns W, Di Sciascio G (2010) Point-of-care assessment of platelet reactivity after clopidogrel to predict myonecrosis in patients undergoing percutaneous coronary intervention. JACC Cardiovasc Interv 3:318–323
Mangiacapra F, Bartunek J, Bijnens N, Peace AJ, Dierickx K, Bailleul E, Di Serafino L, Pyxaras SA, Fraeyman A, Meeus P, Rutten M, De Bruyne B, Wijns W, van de Vosse F, Barbato E (2012) Periprocedural variations of platelet reactivity during elective percutaneous coronary intervention. J Thromb Haemost 10:2452–2461
Mangiacapra F, Cavallari I, Ricottini E, Pellicano M, Barbato E, Di Sciascio G (2015) High platelet reactivity and periprocedural myocardial infarction in patients undergoing percutaneous coronary intervention: a significant association beyond definitions. Int J Cardiol 190:124–125
Feldman DN, Kim L, Rene AG, Minutello RM, Bergman G, Wong SC (2011) Prognostic value of cardiac troponin-I or troponin-T elevation following nonemergent percutaneous coronary intervention: a meta-analysis. Catheter Cardiovasc Interv 77:1020–1030
Prasad A, Singh M, Lerman A, Lennon RJ, Holmes DR, Rihal CS (2006) Isolated elevation in troponin T after percutaneous coronary intervention is associated with higher long-term mortality. J Am Coll Cardiol 48:1765–1770
Collet JP, Cuisset T, Rangé G, Cayla G, Elhadad S, Pouillot C, Henry P, Motreff P, Carrié D, Boueri Z, Belle L, Van Belle E, Rousseau H, Aubry P, Monségu J, Sabouret P, O’Connor SA, Abtan J, Kerneis M, Saint-Etienne C, Barthélémy O, Beygui F, Silvain J, Vicaut E, Montalescot G, ARCTIC I (2012) Bedside monitoring to adjust antiplatelet therapy for coronary stenting. N Engl J Med 367:2100–2109
Price MJ, Berger PB, Teirstein PS, Tanguay JF, Angiolillo DJ, Spriggs D, Puri S, Robbins M, Garratt KN, Bertrand OF, Stillabower ME, Stillablower ME, Aragon JR, Kandzari DE, Stinis CT, Lee MS, Manoukian SV, Cannon CP, Schork NJ, Topol EJ, GRAVITAS I (2011) Standard- vs high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: the GRAVITAS randomized trial. JAMA 305:1097–1105
Trenk D, Stone GW, Gawaz M, Kastrati A, Angiolillo DJ, Müller U, Richardt G, Jakubowski JA, Neumann FJ (2012) A randomized trial of prasugrel versus clopidogrel in patients with high platelet reactivity on clopidogrel after elective percutaneous coronary intervention with implantation of drug-eluting stents: results of the TRIGGER-PCI (Testing Platelet Reactivity In Patients Undergoing Elective Stent Placement on Clopidogrel to Guide Alternative Therapy With Prasugrel) study. J Am Coll Cardiol 59:2159–2164
Mangiacapra F, Di Gioia G, Pellicano M, Di Serafino L, Bressi E, Peace AJ, Bartunek J, Wijns W, De Bruyne B, Barbato E (2016) Effects of prasugrel versus clopidogrel on coronary microvascular function in patients undergoing elective PCI. J Am Coll Cardiol 68:235–237
Mangiacapra F, Panaioli E, Colaiori I, Ricottini E, Lauria Pantano A, Pozzilli P, Barbato E, Di Sciascio G (2016) Clopidogrel versus ticagrelor for antiplatelet maintenance in diabetic patients treated with percutaneous coronary intervention: results of the CLOTILDIA study (Clopidogrel High Dose Versus Ticagrelor for Antiplatelet Maintenance in Diabetic Patients). Circulation 134:835–837
Bonaca MP, Bhatt DL, Cohen M, Steg PG, Storey RF, Jensen EC, Magnani G, Bansilal S, Fish MP, Im K, Bengtsson O, Oude Ophuis T, Budaj A, Theroux P, Ruda M, Hamm C, Goto S, Spinar J, Nicolau JC, Kiss RG, Murphy SA, Wiviott SD, Held P, Braunwald E, Sabatine MS, PEGASUS-TIMI SCAI (2015) Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med 372:1791–1800
Costa F, van Klaveren D, James S, Heg D, Räber L, Feres F, Pilgrim T, Hong MK, Kim HS, Colombo A, Steg PG, Zanchin T, Palmerini T, Wallentin L, Bhatt DL, Stone GW, Windecker S, Steyerberg EW, Valgimigli M, PRECISE-DAPT SI (2017) Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet 389:1025–1034
Pasea L, Chung SC, Pujades-Rodriguez M, Moayyeri A, Denaxas S, Fox KAA, Wallentin L, Pocock SJ, Timmis A, Banerjee A, Patel R, Hemingway H (2017) Personalising the decision for prolonged dual antiplatelet therapy: development, validation and potential impact of prognostic models for cardiovascular events and bleeding in myocardial infarction survivors. Eur Heart J 38:1048–1055
Mangiacapra F, Ricottini E, Barbato E, Demartini C, Peace A, Patti G, Vizzi V, De Bruyne B, Wijns W, Di Sciascio G (2015) Incremental value of platelet reactivity over a risk score of clinical and procedural variables in predicting bleeding after percutaneous coronary intervention via the femoral approach: development and validation of a new bleeding risk score. Circ Cardiovasc Interv 8:e002106
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Mangiacapra, F., Colaiori, I., Ricottini, E. et al. Impact of platelet reactivity on 5-year clinical outcomes following percutaneous coronary intervention: a landmark analysis. J Thromb Thrombolysis 45, 496–503 (2018). https://doi.org/10.1007/s11239-018-1630-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-018-1630-5