Abstract
Background
Ectopic pituitary adenomas (EPAs) are rare, and the suprasellar cistern seems to be the most common location. At this time, no detailed original classification, diagnosis, or treatment protocols for suprasellar pituitary adenomas (SPAs) have been described.
Case description
A 19-year-old man showed visual disturbances and lack of libido for 3 years, he suffered a sharp decline in vision with only light perception in the last week. Magnetic resonance imaging scans revealed a large suprasellar cystic lesion with a normal pituitary in the sella turcica. Endocrinological findings showed an extremely high prolactin level of 1250 ng/mL. Because of the sharp decline in vision, the patient underwent total removal of the suprasellar lesion using a transfrontal interhemispheric approach. The tumor pedicle originated in the lower pituitary stalk without any connection to the anterior pituitary gland in the sella turcica, while the diaphragma sellae was incomplete. Clinical and endocrinological cure criteria were fulfilled and postoperative pathology confirmed a prolactin-secreting pituitary adenoma.
Conclusion
Ectopic suprasellar pituitary adenomas (ESPAs) are extremely rare intracranial extracerebral tumors. SPAs can be classified into three types according to their origin and their relationship with surrounding tissue. Only type III is theoretically a true ectopic, based on previous reports. Thus, ESPAs are uncommon compared to other EPAs. Our case is the first reported case of a type IIa ‘E’SPA and the first description of this subtype classification until now. The pars tuberalis may be different from the pars distalis, and each subtype of adenohypophyseal cells may have different migration characteristics, which leads to different proportions of each hormone-secreting subtype in SPAs and EPAs. Transsphenoidal surgery is minimally invasive, but transcranial surgery may remain a universal option for the treatment of suprasellar lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
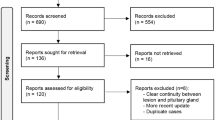
Pituitary adenomas are the most common lesion found in the sellar space, and ectopic pituitary adenomas (EPAs) are extremely rare. Their origin is identical to the adenohypophysis but they grow completely outside of the sella turcica [1], without any continuity with the intrasellar normal pituitary gland. Since Erdheim [2] reported the first case of EPA in 1909, about 100 cases have been reported in the literature [1, 3,4,5], with tumor sites including sphenoid sinus [1, 5,6,7,8,9,10,11], suprasellar cistern [1, 3, 10,11,12,13,14], cavernous sinus [3, 6, 12, 15], clivus [16], nasal cavity, sphenoid wing, petrous temporal bone, superior orbital fissure, temporal lobe [17], and the third ventricle [18]. Suprasellar cisterns are the most common ectopic location [1]. However, according to our understanding of the origin of suprasellar pituitary adenomas (SPAs), many adenomas previously considered ectopic, attached to the pituitary stalk above diaphragma sellae (DS), are misclassified as true ectopic adenomas originating from leptomeninges of the peri-infundibular region [1, 3, 5]. Thus, it is important to have a detailed classification of the origin of SPAs, and the true incidence of suprasellar cisterns among all ectopic locations should be reevaluated. Here, we report a case of ‘ectopic’ suprasellar subdiaphragmatic prolactinoma and report this subtype of ‘ectopic’ SPAs with a large size, clear intraoperative image, and satisfactory prognosis after craniotomy. A brief review of 36 ectopic suprasellar pituitary adenomas (ESPAs) are presented (including our case) (Table 1) to provide improved original classification, diagnosis, and treatment protocols.
Case description
A 19-year-old man presented with decreased visual acuity and progressive visual field defects for 3 years, he suffered a sharp decline in vision with only light perception in the last week and was admitted to our department. He also complained of lack of libido over the past few years and a childish appearance, which was indicative of dysplasia of male secondary sexual characteristics. Physical examination was normal except for the visual disturbance. Visual acuity was only light perception in both eyes. Endocrinological findings showed an extremely high prolactin (PRL) level of 1250 ng/mL (normal, 2.1–17.7 ng/mL), while total testosterone (TT) level was slightly lower, 169.9 ng/dl (normal, 241.0–827.0 ng/dl); other pituitary hormone levels, including growth hormone (GH), insulin-like growth factor-1 (IGF-1), adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH) levels were within normal limits. Magnetic resonance imaging (MRI) scans revealed a large suprasellar cystic lesion with an enhanced surrounding capsule. It pushed the pituitary gland and stalk slightly to the left and the optic chiasm slightly upward (Fig. 1). Preoperative diagnoses mainly focused on suprasellar prolactinoma.
Pre- and postoperative magnetic resonance image (MRI). A large cystic lesion with an apparent boundary located in the suprasellar region. It appeared hypointense on T1-weighted images (T1WI) (a, d), while the capsule was significantly enhanced with gadolinium diethylenetriamine pentaacetic acid (Gd-DTPA) (b, e). The pituitary gland and stalk was pushed posterior to the left and the optic chiasm was compressed slightly upward. Post-op MRI showed that the lesion was completely resected from the suprasellar region and the pituitary gland and stalk were well-preserved (c, f)
Because of the sharp decline in vision, the patient was not accepted any medical treatment (such like cabergoline). Instead, he underwent a timely tumor resection of craniotomy through a right-sided transfrontal interhemispheric approach to decompress optic nerves completely. Intraoperative situations are shown in Fig. 2, and the tumor was located in the suprasellar cisterns with a dark red capsule and yellowish cyst fluid inside. A substantial part of the tumor was soft and reddish and could be easily aspirated. When isolating the tumor step by step, we could see that the tumor pedicle originated in the lower pituitary stalk without any connection to the anterior pituitary gland in the sella turcica, while the diaphragma sellae was incomplete. It pushed the pituitary gland and stalk posterior to the left, the optic nerves were displaced bilaterally, and the optic chiasm was compressed upward (Fig. 2). Histopathological examination (hematoxylin and eosin stain) of the tumor specimen revealed typical acidophilic or chromophobe adenoma cells with rich sinusoidal structures (Fig. 3). Immunohistochemical staining for hormones showed that the tumor was strongly positive for PRL, but was negative for GH, ACTH, FSH, LH, and TSH.
Intraoperative findings. The tumor was located in the suprasellar cisterns with a dark red capsule (a). When isolating the tumor step by step, a substantial part of the tumor was soft and reddish, with yellowish cyst fluid inside (b). The tumor pedicle originated in the lower pituitary stalk without any connection to the anterior pituitary gland in the sella turcica, and the diaphragma sellae is incomplete (c). It pushed the pituitary gland and stalk posterior to the left, the optic nerves were displaced bilaterally, and the optic chiasm was compressed upward. PA pituitary adenoma, PS pituitary stalk, PI pituitary, ON optic nerve
The patient’s postoperative course was satisfactoy. His vision returned to 0.2 (4.3) in both eyes and the visual field showed a bitemporal hemianopsia. He developed transient diabetes insipidus, but recovered quickly, within 1 week. The PRL level dropped to 8.8 ng/mL on the third postoperative day and was maintained for the next 2 months; the TT level increased gradually to normal limits during the next 3 months. Other endocrinological hormones including GH, IGF-1, ACTH, FSH, LH, and TSH were all within normal limits during follow-up. An MRI scan 6 months after operation showed that the tumor had been completely resected from the suprasellar region and the pituitary gland and stalk were well-preserved (Figs. 1, 2).
Discussion
The pituitary gland includes the adenohypophysis and neurohypophysis. The adenohypophysis originates extracranially and elongates upward, and it later becomes attached to the neurohypophysis, which is formed by the descent of the infundibular recess [3]. The adenohypophysis consists of the pars distalis, the pars intermedia, and the pars tuberalis. The pars distalis originates from the thickened anterior wall of Rathke’s pouch. It is the primary mass of the pituitary and synthesizes and secretes various hormones. The pars intermedia is a remnant of the posterior wall of Rathke’s pouch and is considered vestigial in humans [3]. The pars tuberalis is the upward extension from the pars distalis and surrounds the pituitary stalk anteriorly. The neurohypophysis consists of the pars nervosa, which is the inferior elongation of the hypothalamus, and adheres to pars intermedia forming the posterior lobe (neurohypophysis).
EPAs are rare intracranial extracerebral tumors. Their origin is identical with the adenohypophysis but they grow completely outside of the sella turcica [1]. The suprasellar cistern is the most common location for EPAs. However, not every SPA is an EPA; most of them are not. According to previous anatomical analyses, the origins of SPAs can be classified into three types (Table 2; Fig. 4). Type I are SPAs originating from pars distalis, the superior portion of the anterior pituitary tissue, and extending superiorly through the DS. Type II are SPAs originating from pars tuberalis, an elevated portion of the anterior pituitary tissue and mainly constituting the pituitary stalk, which is the most common source of SPAs in reported cases [8, 10, 12, 38]. Type III are SPAs originating from residual cells of Rathke’s pouch. When the pars tuberalis of Rathke’s pouch migrate upward to the hypothalamus at late stages, adenohypophyseal cells of pars tuberalis may migrate aberrantly to the suprasellar peri-infundibular region. These cells are not in continuity with the pars tuberalis (pituitary stalk) and are considered to be the source of ESPAs in this region [6, 40]. Type II SPAs can be further classified into a subdiaphragmatic subtype (Type IIa) and a supradiaphragmatic subtype (Type IIb), according to their relationship with DS. Furthermore, type I and type II SPAs cannot be called ectopic because of their continuity with anterior lobe tissue, only type III SPAs are real ectopic. Thus, ESPAs are less common than other EPAs.
The anatomic origin of suprasellar pituitary adenoma (SPA). It can be classified into three types. Type I are SPAs originating from pars distalis, the superior portion of the anterior pituitary tissue, and extending superiorly through the diaphragma sella (DS). Type II are SPAs originating from pars tuberalis, an elevated portion of anterior pituitary tissue and mainly constitute pituitary stalk. This type could further be classified into a subdiaphragmatic subtype (Type IIa) and a supradiaphragmatic subtype (Type IIb) according to the relationship with DS. Type III are SPAs originating from residual cells of Rathke’s pouch. When the pars tuberalis of Rathke’s pouch migrates upward to the hypothalamus in late stages, adenohypophyseal cells of pars tuberalis may migrate aberrantly to the suprasellar peri-infundibular region. These cells are not in continuity with the pars tuberalis (pituitary stalk)
Based on a retrospective review of all reported cases of ESPAs (Table 1), 28 could be found at their original location based on their description. However, the majority (17 cases) originated from pars tuberalis with complete DS (Type IIb), and only ten cases originated from ectopic adenohypophyseal cells of the suprasellar peri-infundibular region without any connection to the pituitary stalk (Type III). This is a theoretically real ectopic [41] and agrees with the results of Jouanneau et al. [42] Thus, the proportion of ESPAs among all EPAs may be over-estimated and we should correct the evaluation of SPAs according to their relationship with surrounding tissue (anterior pituitary, pituitary stalk and diaphragma sellae; Table 2). However, we report an SPA originating from the lower pituitary stalk with incomplete DS (Fig. 2), which is the first reported case of ‘ectopic’ suprasellar type IIa pituitary adenoma and the first description of this subtype classification.
Among the 18 cases of type II (a + b) SPAs, the majority (ten cases, 55.6%) were ACTH-secreting adenomas, four were PRL-secreting adenomas (22.2%), and four were nonfunctioning (22.2%). This differed from the proportion of each hormone-secreting subtype of intrasellar pituitary tumor. For the remaining ten cases of type III ESPAs, the hormonal distributions were as follows: three cases were PRL-secreting adenomas (30.0%), two were ACTH-secreting adenomas (20.0%), one was a GH-secreting adenoma (10.0%), one was a TSH-secreting adenoma (10.0%), and three were nonfunctioning (30.0%). This proportion is slightly different from the proportion of reported ectopic adenomas across all locations [1, 4]. It is possible that the pars tuberalis may differ from the pars distalis, and each subtype of adenohypophyseal cell may have different migration characteristics. Further embryological and histological studies are required to confirm our hypothesis.
The surgical strategy for suprasellar adenomas, unlike for intrasellar pituitary adenomas, remains controversial. Before the 2000s, although the resection of SPA through transsphenoidal surgery (TSS) was attempted [3, 25, 30, 35], transcranial surgery (TCS) was more acceptable. With the development of neuroendoscopic equipment and technology, as well as an increased understanding of saddle area anatomy, TSS is easier to perform. Mason et al. [30] described the transsphenoidal/transdiaphragmatic route through the posterior portion of the planum sphenoidale to reach suprasellar tumors. Fuminari et al. [38] considered the endoscopic view as lacking a steric sense, and they applied 3D endoscopy for suprasellar surgery to increase understanding of the 3D forms of these structures. We believe that this technology requires advanced training. Although it is minimally invasive and useful, it should not be applied to all cases of suprasellar lesions, particularly lesions with a hard texture, rich blood supply, and involving the cavernous sinus or carotid artery. The limited operating space, difficult hemostasis, and CSF fistula require improvement [24, 25, 32, 33, 35]. However, TCS may remain a universal option for the treatment of suprasellar lesions.
Conclusions
Ectopic suprasellar pituitary adenomas (ESPAs) are extremely rare intracranial extracerebral tumors. SPAs can be classified into three types according to their origin and their relationship with surrounding tissue (anterior pituitary, pituitary stalk, and diaphragma sella). Only type III is theoretically a true ectopic, based on previous reports. Thus, ESPAs are uncommon compared to other EPAs. Our case is the first reported case of a type IIa ‘E’SPA and the first description of this subtype classification until now. The pars tuberalis may be different from the pars distalis, and each subtype of adenohypophyseal cells may have different migration characteristics, which leads to different proportions of each hormone-secreting subtype in SPAs and EPAs. Transsphenoidal surgery is minimally invasive, but transcranial surgery may remain a universal option for the treatment of suprasellar lesions.
References
Guerrero CA, Krayenbühl N, Husain M, Krisht AF (2007) Ectopic suprasellar growth hormone-secreting pituitary adenoma: case report. Neurosurgery 61(4):E879
Erdheim J (1909) Über einen Hypophysentumor von ungewöhnlichem Sitz. Beitr Pathol Anat 46:233–240
Hou L, Harshbarger T, Herrick MK, Tse V (2002) Suprasellar adrenocorticotropic hormone-secreting ectopic pituitary adenoma: case report and literature review. Neurosurgery 50:618–625
Mitsuya K, Nakasu Y, Nioka H, Nakasu S (2004) Ectopic growth hormone-releasing adenoma in the cavernous sinus-case report. Neurol Med Chir 44:380–385
Caranci F, Cirillo L, Bartiromo F, Ferraioli M, Del Basso De Caro ML, Esposito F, Cappabianca P, Brunetti A, Elefante R (2006) Ectopic suprasellar pituitary adenoma: a case report. Neuroradiol J 19:731–735
Pluta RM, Nieman L, Doppman JL, Watson JC, Tresser N, Katz DA, Oldfield EH (1999) Extrapituitary parasellar microadenoma in Cushing’s disease. J Clin Endocrinol Metab 84(8):2912–2923
Lindboe CF, Unsgård G, Myhr G, Scott H (1993) ACTH and TSH producing ectopic suprasellar pituitary adenoma of the hypothalamic region: case report. Clin Neuropathol 12(3):138–141
Hamada J, Seto H, Miura M, Kuratsu J, Ushio Y (1990) Suprasellar pituitary adenoma arising from the pars tuberalis: case report. Neurosurgery 27:647–649
Tamaki N, Shirakuni T, Kokunai T, Matsumoto S, Fujimori T, Maeda S (1991) Ectopic pituitary adenoma in the suprasellar cistern: case report. Surg Neurol 35:389–394
Flitsch J, Schmid SM, Bernreuther C, Winterberg B, Ritter MM, Lehnert H, Burkhardt T (2015) A pitfall in diagnosing cushing’s disease: ectopic ACTH-producing pituitary adenoma in the sphenoid sinus. Pituitary 18:279–282
Appel JG, Bergsneider M, Vinters H, Salamon N, Wang MB, Heaney AP (2012) Acromegaly due to an ectopic pituitary adenoma in the clivus: case report and review of literature. Pituitary 15:S53–S56
Mizutani A, Yamaguchi-Okada M, Yokota N, Namba H (2009) Asymptomatic non-functioning ectopic pituitary adenoma in the suprasellar region: a case report. Br J Neurosurg 23(3):321–323
Seltzer J, Lucas J, Commins D, Lerner O, Lerner A, Carmichael JD, Zada G (2015) Ectopic ACTH-secreting pituitary adenoma of the sphenoid sinus: case report of endoscopic endonasal resection and systematic review of the literature. Neurosurg Focus 38(2):E10
Ramírez C, Hernández-Ramirez LC, Espinosa-de-los-Monteros AL, Frano JM, Guinto G, Mercado M (2013) Ectopic acromegaly due to a GH-secreting pituitary adenoma in the sphenoid sinus: a case report and review of the literature. BMC Res Notes 6:411
Kohno M, Sasaki T, Narita Y, Teramoto A, Takakura K (1994) Suprasellar ectopic pituitary adenoma: case report. Neurol Med Chir 34:538–542
Ortiz-Suarez H, Erickson DL (1975) Pituitary adenoma of adolescents. J Neurosurg 43:437–439
Neilson K, de Chadaverian JP (1987) Ectopic anterior pituitary corticotropic tumour in a six-year-old boy. Histological ultrastructural and immunocytochemical study. Virchows Arch A 411:267–273
Kleinschmidt-Demasters BK, Winston KR, Rubinstein D, Samuels MH (1990) Ectopic pituitary adenoma of the third ventricle. Case report. J Neurosurg 72:139–142
Ogilvy KM, Jakubowski J (1973) Intracranial dissemination of pituitary adenomas. J Neurol Neurosurg Psychiatr 36(2):199–205
Rothman LM, Sher J, Quencer RM, Tenner MS (1976) Intracranial ectopic pituitary adenoma: case report. J Neurosurg 44:96–99
Iwai Y, Hakuba A, Katsuyama J, Nagata Y, Nishimura S, Abe K, Asakura T, Inoue Y (1990) A case of ectopic large pituitary adenoma [in Japanese]. No Shinkei Geka 18:71–75
Matsumura A, Meguro K, Doi M, Tsurushima H, Tomono Y (1990) Suprasellar ectopic pituitary adenoma: case report and review of the literature. Neurosurgery 26:681–685
Luk KH, Lam KS, Kung AW, Fung CF, Leung SY (1992) Suprasellar ectopic pituitary adenoma presenting as cranial diabetes insipidus. Postgrad Med J 68:467–469
Tal A, Tenn JC (1993) Cushing’s disease caused by ectopic pituitary adenoma within the pituitary stalk. South Med J 86(2):249–250
Dyer EH, Civit T, Abecassis JP, Derome PJ (1994) Functioning ectopic supradiaphragmatic pituitary adenomas. Neurosurgery 34:529–532
Kohno M, Sasaki T, Narita Y, Teramoto A, Takakura K (1994) Suprasellar ectopic pituitary adenoma-case report. Neurol Med Chir 34:538–542
Tanaka T, Watanabe K, Nakasu S, Handa J (1994) Suprasellar ectopic pituitary adenoma: report of a case [in Japanese]. No Shinkei Geka 22:1141–1145
Akimoto J, Nagura M, Onodera Y (1995) Cystic ectopic pituitary adenoma: report of a case [in Japanese]. No To Shinkei 47:1092–1097
Takahata T, Katayama Y, Tsubokawa T, Oshima H, Yoshino A (1995) Ectopic pituitary adenoma occurring in the interpeduncular cistern: case report. J Neurosurg 83:1092–1094
Mason RB, Nieman LK, Doppman JL, Oldfield EH (1997) Selective excision of adenomas originating in or extending into the pituitary stalk with preservation of pituitary function. J Neurosurg 87:343–351
Nagatani T, Shibuya M, Suzuki Y, Saito K, Yoshida J (1997) Suprasellar ectopic pituitary adenoma. Acta Neurochir (Wien) 139:94–95
Jung S, Kim JH, Kim TS, Lee MC, Seo JJ, Park JW, Kang SS (2000) Supradiaphragmatic ectopic adrenocorticotropic hormone-secreting adenoma. Pathol Int 50:901–904
Ueda R, Katayama M, Yoshida K, Kawase T (2003) Suprasellar peri-infundibular ectopic prolactinoma-case report. Neurol Med Chir 43:51–54
Peker S, Sun I, Kurtkaya-Yapicier O, Elmaci I, Pamir MN (2005) Ectopic pituitary adenoma located at the pituitary stalk: case report. J Neurosurg Sci 49:25–29
Dam-Hieu P, Irthum B, Seizeur R, Roudaut N, Besson G (2007) Management of ACTH-secreting supradiaphragmatic adenomas. Clin Neurol Neurosurg 109:698–704
So G, Takeshita T, Morofuji Y, Iseki M, Hayashi T, Matsuo T, Suyama K, Nagata I (2008) Nonfunctioning suprasellar ectopic pituitary adenoma. A case report [in Japanese]. No Shinkei Geka 36:1121–1125
Kinoshita Y, Tominaga A, Arita K, Hama S, Sakoguchi T, Sugiyama K, Kurisu K (2012) Supra-diaphragmatic pituitary adenoma removed through the trans-tuberculum sellae approach. Case report. Neurol Med Chir 52:91–95
Fuminari K, Hideki A, Manabu O, Mitsunori M (2015) Extended endoscopic endonasal surgery using three-dimensional endoscopy in the intraoperative MRI suite for supra-diaphragmatic ectopic pituitary adenoma. Turk Neurosurg 25(3):503–507
Wang Q, Lu XJ, Sun J, Wang J, Huang CY, Wu ZF (2016) Ectopic suprasellar thyrotropin-secreting pituitary adenoma: case report and literature review. World Neurosurg 617:E13–E18
Colohan AR, Grady MS, Bonnin JM, Thorner MO, Kovacs K, Jane JA (1987) Ectopic pituitary gland simulating a suprasllar tumor. Neurosurgery 20:43–48
Rasmussen P, Lindholm J (1979) Ectopic pituitary adenomas. Clin Endocrinol 11:69–74
Jouanneau E, Perrin G, Trouillas J (2002) Corticotroph microadenomas of the pituitary stalk. Diagnosis and surgical removal. Neurochirurgie 48:215–222
Funding
This article is supported by a national clinical key specialty construction project in China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Rights and permissions
About this article
Cite this article
Zhou, HJ., Pan, DS., Ba, XQ. et al. ‘Ectopic’ suprasellar type IIa PRL-secreting pituitary adenoma. Pituitary 20, 477–484 (2017). https://doi.org/10.1007/s11102-017-0807-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-017-0807-9