Abstract
Purpose
Ectopic pituitary adenomas (EPA) are rare tumors thought to arise from embryological remnants along the route of normal pituitary migration. Clinically, these tumors vary in hormonal activity and can exert mass effect based on location and size.
Methods
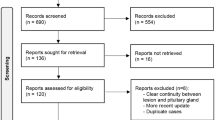
We performed a single-center retrospective analysis of patients with diagnosis of ectopic pituitary adenoma from 2001 to 2018.
Results
Five patients were identified with EPA: a 48-year-old woman with suprasellar EPA treated with transsphenoidal removal of the tumor, a 44-year-old woman with cavernous EPA treated with transsphenoidal removal of the tumor, a 48-year-old woman with sphenoid EPA treated with cabergoline, a 45-year-old man with clival EPA treated with cabergoline and transsphenoidal surgical resection, and a 54-year-old man with clival EPA treated with cabergoline therapy.
Conclusions
EPA should be considered as a differential diagnosis of juxta-sellar lesions. Appropriate hormonal testing may lead to early diagnosis, avoidance of unnecessary biopsy or surgery, and improved outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ectopic pituitary adenomas (EPA) are rare tumors described predominantly through case reports. With the routine use of cross-sectional imaging, familiarity with the radiological findings of this entity is critical in providing appropriate clinical management. Importantly, failure to consider the diagnosis pre-operatively may lead to unnecessary surgery.
Case presentations
Patient 1: suprasellar EPA
A 48-year-old woman with type 2 diabetes, hyperlipidemia, spontaneous bruising, hair loss, and facial hair growth was referred for multiple falls, including one that caused a right orbital fracture. Upon evaluation of the orbital fracture, the patient was noted to have a suprasellar mass. The morning serum cortisol following 1 mg overnight dexamethasone remained elevated at 21 mcg/dL (normal < 2 mcg/dL). The adrenocorticotropic hormone (ACTH) was also elevated at 77 pg/mL (normal 10–60 pg/mL). MRI confirmed the suprasellar mass impinging on the optic chiasm (Fig. 1). The pituitary gland, located within the sella, had a normal appearance. Transsphenoidal removal of the tumor was performed and histopathology revealed a corticotroph adenoma. Day 1 post-operative serum cortisol dropped to 13 mcg/dL.
Patient 2: cavernous sinus EPA
A 44-year-old woman was referred for weight gain and extremity striae. She had an elevated ACTH level of 103 pg/mL (normal 10–60 pg/mL) with suppression of aldosterone and renin levels. An outside MRI of the brain was reported as mild heterogeneity at the left aspect of the pituitary without a discrete mass. Upon presentation to our institution, a dynamic pituitary MRI was performed revealing an 8 mm left-sided intracavernous lesion adjacent to the sellar margin (Fig. 2). The pituitary gland was normal in appearance and no intrasellar lesion was seen. The inferior petrosal sinus sampling revealed a markedly increased ACTH level of 1369 pg/mL in the left inferior petrosal sinus (reference right inferior petrosal sinus ACTH was 43 pg/mL). The patient underwent successful transsphenoidal removal of the tumor histologically confirmed to be corticotroph adenoma.
Coronal (left) and axial (right) enhanced T1-weighted MRI demonstrates a well-marginated 8 mm ovoid non-enhancing mass (arrows) in the left cavernous sinus inferior and medial to the cavernous segment of the left internal carotid artery. The tumor effaces the left lateral margin of the normal appearing pituitary gland (asterisk)
Patient 3: sphenoid EPA
A 48-year old woman with type 2 diabetes was referred for fever, headache, and confusion. Lumbar puncture at an outside facility demonstrated an elevated opening pressure and growth of Streptococcus pneumoniae from CSF. Immediately following the IV antibiotic therapy, the patient developed CSF leak from her left naris. Upon transfer to our institution, CT and MRI demonstrated an enhancing juxta-sellar mass in the sphenoid sinus, clivus, and cavernous sinus (Fig. 3). Transsphenoidal biopsy revealed a prolactinoma. The patient was started on cabergoline. On follow-up, the patient had complete resolution of symptoms and normalization of prolactin levels.
Patient 4: clival EPA
A 45-year-old man with hypertension and sleep apnea presented with episodes of headaches and hypertensive emergency. CT and MRI revealed a mass eroding the clivus and floor of the sella with extension into the sphenoid sinus (Fig. 4). Transsphenoidal biopsy of the lesion revealed a prolactinoma. Immediate postoperative prolactin level was elevated at 393 ng/mL (normal 4.0–15.2 ng/mL). On follow-up after cabergoline therapy, the patient had resolution headaches and marked decrease in prolactin levels (1.2 ng/mL).
Patient 5: spheno-clival EPA
A 54-year-old man was referred for a one-year history of intermittent tinnitus, ataxia, and vertigo. MRI obtained at an outside institution showed a large sphenoid sinus mass with clival invasion (Fig. 5a). The mass showed avid uptake on an otherwise unremarkable 18F-fluorodeoxyglucose(FDG) PET–CT performed at that facility (Fig. 5b). Laboratory evaluation revealed an elevated level of prolactin at 3436 mU/L. Based on the presumptive diagnosis of an ectopic prolactinoma, the patient was started on cabergoline therapy without biopsy. Subsequently, the prolactin levels normalized, symptoms improved, and the mass regressed on follow-up MRI (Fig. 5c).
Discussion
Anatomy
The pituitary gland is anatomically comprised of a posterior lobe (neurohypophysis) and an anterior lobe (adenohypophysis) [1,2,3]. The neurohypophysis is divided into the pars nervosa and infundibular stalk. The pars nervosa comprises the majority of the posterior lobe and is the storage site for oxytocin and vasopressin. The infundibular stalk forms a connection between the hypophyseal and hypothalamic systems [4,5,6].
The adenohypophysis is further delineated into the pars distalis, pars intermedia, and pars tuberalis [3, 7]. The pars distalis comprises the majority of the adenohypophysis and is responsible for the secretion of pituitary hormones including ACTH, thyroid-stimulating hormone (TSH), follicle-stimulating hormone, growth hormone, luteinizing hormone, and prolactin [3, 7]. The pars intermedia is only a few cell layers thick and forms the boundary between the anterior and posterior pituitary lobes [3]. The pars tuberalis is an extension from the pars distalis, which surrounds the infundibular stalk of the neurohypophysis [3].
Embryology
The neurohypophysis and adenohypophysis are derived from the neuroectoderm and ectoderm, respectively [8]. During the 4th week of gestation, the extracranial ectoderm from the primitive oral cavity forms a superiorly-oriented invagination, giving rise to the Rathke’s pouch which completely separates from the ectoderm during weeks 6–8 and joins with the inferiorly-oriented extension of the neuroectoderm. The union of these two invaginations forms the pituitary gland in the mesoderm-derived sella turcica of the sphenoid bone [6].
Ectopic pituitary adenomas
EPAs are thought to originate from the neoplastic proliferation of pituitary rests along the embryological path of the pituitary development [9, 10]. Approximately 60% of reported EPAs are seen in the sphenoid sinus and suprasellar region, and 30% can be located in the clivus, nasal cavity, cavernous sinus, parasellar region, and sphenoid wing [11]. The suprasellar EPA, located outside of the expected migrational tract, are thought to arise from ectopic suprasellar peri-infundibular pituitary cells [12]. Rare sites beyond the migrational tract have also been described, including those in the petrosal temporal bone,[13] superior orbital fissure,[14] third ventricle,[15] and temporal lobe [16].
Clinical manifestations of EPAs are variable. Overall, the symptomatology depends on involvement of adjacent structures and hormonal activity [17]. Visual disturbances (diplopia, visual activity loss, blurring, proptosis), and facial paresthesia may occur due to compression of the cranial nerves by tumor extending into cavernous sinus or clivus [18]. Sphenoid sinus EPA can also be present with nasal obstruction, headache, and cerebrospinal fluid leak [17]. The common hormonal manifestations include hyperprolactinemia, Cushing’s syndrome, and acromegaly [19]. Cross-sectional imaging with CT and MRI provides visualization of the juxta-sellar lesion. On CT, EPAs are often isodense to gray matter and enhance moderately after contrast. Evaluation of bone erosion may also be seen on CT. On MRI, EPAs are often low signal on T1WI, high signal on T2WI, and demonstrate mild-to-moderate gadolinium enhancement [17]. MRI offers superior contrast to allow accurate anatomic localization relative to the pituitary gland and adjacent structures such as cavernous sinus, cranial nerves and infundibulum. This anatomic information assists in the surgical planning for resection of the adenoma. While the transsphenoidal approach is a commonly utilized for resection, imaging may warrant alternative transsellar, transdiaphragmatic,[20] or pteronial approches [21].
In this case series, we demonstrate the importance of utilizing serum hormonal titers in the diagnosis and assessment of treatment response of EPAs. Nearly three-quarters of EPAs are hormonally active, of which ACTH and prolactin-secreting adenomas comprise the majority [11]. The possibility of EPA should always be kept in mind when dealing with lesions in juxtasellar locations i.e. the rostral clivus, cavernous sinus, sphenoid sinus, and suprasellar region. Obtaining hormonal levels in these cases may facilitate early diagnosis and potentially avert an unnecessary biopsy and/or surgical intervention. In the first two cases of ectopic prolactinoma, testing for elevated pre-operative prolactin levels coupled with the imaging findings may have been sufficient to suggest EPA and start the patient on appropriate therapy without biopsy. The final case of prolactinoma demonstrates appropriate laboratory testing based on the imaging interpretation, which indeed prevented biopsy and surgical intervention. This case, along with past reports [22, 23] of hormone-secreting ectopic pharyngeal pituitary adenoma successfully treated with octreotide and dopamine agonists, suggests that pharmacotherapy with hormonal analogs can not only help improve symptoms but may also eliminate the need for surgical resection.
Based on a PubMed case report search of EPA, we identified four case reports [24,25,26,27] in which laboratory reports of elevated pituitary hormones may have assisted in predicting EPA. In one case, a patient with a presumed chordoma at a clival lesion underwent partial surgical resection with pathology demonstrating a prolactin-secreting EPA [24]. Hormonal assessment may have prevented surgical intervention in this case, as a majority of prolactinomas responds well to dopamine analogs [28]. In another case, the surgery for a prolactin-secreting EPA was complicated by post-procedural cerebrospinal fluid leakage, which might have been avoided with pharmacotherapy [26]. Finally, in two patients who underwent surgery for asymptomatic prolactin-secreting [25] and TSH-secreting EPAs,[27] preoperative hormonal evaluation may have suggested the diagnosis of EPAs despite the absence of clinical manifestations.
In conclusion, although rare, EPA should be considered in the differential diagnosis of juxta-sellar lesions. Appropriate hormonal testing may not only lead to early diagnosis and improved outcomes, but may also help avoid unnecessary biopsy or surgery.
References
Nakane PK (1970) Classifications of anterior pituitary cell types with immunoenzyme histochemistry. J Histochem Cytochem 18(1):9–20. https://doi.org/10.1177/18.1.9
ElSayed SA, Bhimji SS (2018) Physiology, Pituitary Gland. StatPearls Publishing LLC, Treasure Island
Ilahi S, Ilahi TB (2018) Anatomy, Adenohypophysis (Pars Anterior, Anterior Pituitary). StatPearls Publishing LLC, Treasure Island
Stopa EG, LeBlanc VK, Hill DH, Anthony EL (1993) A general overview of the anatomy of the neurohypophysis. Ann N Y Acad Sci 689:6–15
Amar AP, Weiss MH (2003) Pituitary anatomy and physiology. Neurosurg Clin N Am 14(1):11–23 v
Larkin S, Ansorge O (2017) Development and microscopic anatomy of the pituitary gland. Endotext. https://www.endotext.org. Accessed 1 Feb 2019
Dorton AM (2000) The pituitary gland: embryology, physiology, and pathophysiology. Neonatal Netw 19(2):9–17. https://doi.org/10.1891/0730-0832.19.2.9
Patel H, Tiwari V (2018) Physiology, Posterior Pituitary. StatPearls Publishing LLC, Treasure Island
Ciocca DR, Puy LA, Stati AO (1985) Identification of seven hormone-producing cell types in the human pharyngeal hypophysis. J Clin Endocrinol Metab 60(1):212–216. https://doi.org/10.1210/jcem-60-1-212
Melchionna RH, Moore RA (1938) The pharyngeal pituitary gland. Am J Pathol 14(6):763–772 761
Hou L, Harshbarger T, Herrick MK, Tse V (2002) Suprasellar adrenocorticotropic hormone-secreting ectopic pituitary adenoma: case report and literature review. Neurosurgery 50(3):618–625
Hori A (1985) Suprasellar peri-infundibular ectopic adenohypophysis in fetal and adult brains. J Neurosurg 63(1):113–115. https://doi.org/10.3171/jns.1985.63.1.0113
Rasmussen P, Lindholm J (1979) Ectopic pituitary adenomas. Clin Endocrinol (Oxf) 11(1):69–74
Ortiz-Suarez H, Erickson DL (1975) Pituitary adenomas of adolescents. J Neurosurg 43(4):437–439. https://doi.org/10.3171/jns.1975.43.4.0437
Kleinschmidt-DeMasters BK, Winston KR, Rubinstein D, Samuels MH (1990) Ectopic pituitary adenoma of the third ventricle. Case report. J Neurosurg 72(1):139–142. https://doi.org/10.3171/jns.1990.72.1.0139
Neilson K, de Chadarevian JP (1987) Ectopic anterior pituitary corticotropic tumour in a six-year-old boy. Histological, ultrastructural and immunocytochemical study. Virchows Arch A Pathol Anat Histopathol 411(3):267–273
Yang BT, Chong VF, Wang ZC, Xian JF, Chen QH (2010) Sphenoid sinus ectopic pituitary adenomas: CT and MRI findings. Br J Radiol 83(987):218–224. https://doi.org/10.1259/bjr/76663418
Thompson LD, Seethala RR, Muller S (2012) Ectopic sphenoid sinus pituitary adenoma (ESSPA) with normal anterior pituitary gland: a clinicopathologic and immunophenotypic study of 32 cases with a comprehensive review of the english literature. Head Neck Pathol 6(1):75–100. https://doi.org/10.1007/s12105-012-0336-9
Langford L, Batsakis JG (1995) Pituitary gland involvement of the sinonasal tract. Ann Otol Rhinol Laryngol 104(2):167–169. https://doi.org/10.1177/000348949510400217
Mason RB, Nieman LK, Doppman JL, Oldfield EH (1997) Selective excision of adenomas originating in or extending into the pituitary stalk with preservation of pituitary function. J Neurosurg 87(3):343–351. https://doi.org/10.3171/jns.1997.87.3.0343
Guerrero CA, Krayenbuhl N, Husain M, Krisht AF (2007) Ectopic suprasellar growth hormone-secreting pituitary adenoma: case report. Neurosurgery 61(4):E879; (discussion E879). https://doi.org/10.1227/01.neu.0000298921.47495.42
Warner BA, Santen RJ, Page RB (1982) Growth hormone and prolactin secretion by a tumor of the pharyngeal pituitary. Ann Intern Med 96(1):65–66. https://doi.org/10.7326/0003-4819-96-1-65
Pugnale N, Waridel F, Bouzourene H, Boubaker A, Pugnale M, Gaillard RC, Gomez F (2003) Pharyngeal pituitary non-functioning adenoma with normal intra-sellar gland: massive tumor shrinkage on octreotide therapy. Eur J Endocrinol 148(3):357–364
Karras CL, Abecassis IJ, Abecassis ZA, Adel JG, Bit-Ivan EN, Chandra RK, Bendok BR (2016) Clival ectopic pituitary adenoma mimicking a Chordoma: case report and review of the literature. Case Rep Neurol Med. https://doi.org/10.1155/2016/8371697
Narese D, Virzi V, Virzi G, Narese F, Sciortino A, Culmone G, Virzi F, Maira G (2015) Ectopic prolactinoma in the clivus: a case report. La Clin Ter 166(4):176–178. https://doi.org/10.7417/ct.2015.1866
Sakakibara Y, Sekino H, Taguchi Y, Tadokoro M (2002) Unilateral exophthalmos caused by a prolactin producing ectopic pituitary adenoma: case report. No Shinkei Geka Neurol surg 30(6):623–628
Hanaoka Y, Ogiwara T, Kakizawa Y, Nagm A, Seguchi T, Aoyama T, Koyama J-i, Sato A, Hongo K (2018) Calcified ectopic TSH-secreting pituitary adenoma mimicking craniopharyngioma: a rare case report and literature review. Acta Neurochir 160(10):2001–2005. https://doi.org/10.1007/s00701-018-3638-1
Ballaux D, Verhelst J, Pickut B, De Deyn PP, Mahler C (1999) Ectopic macroprolactinoma mimicking a chordoma: a case report. Endocr Relat Cancer 6(1):117–122
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or non-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Agely, A., Okromelidze, L., Vilanilam, G.K. et al. Ectopic pituitary adenomas: common presentations of a rare entity. Pituitary 22, 339–343 (2019). https://doi.org/10.1007/s11102-019-00954-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-019-00954-y