Abstract
Background
The persistence and adherence to endocrine therapy (ET) in hormone receptor-positive (HR +) breast cancer patients remain far less than optimal.
Aim
This retrospective study aimed to evaluate adherence to ET and to identify influencing factors in early-stage HR + breast cancer patients.
Method
A stratified random sampling method was used to select patients admitted for breast cancer surgery at a university hospital in Shanghai, China. Patients who received ET medications in the hospital information system (HIS) were included. The primary outcomes were early discontinuation of and adherence to ET. Potential factors influencing the discontinuation and adherence were assessed using univariate and multivariate logistic regression analyses.
Results
In total, 706 patients were included, and 161 (22.8%) discontinued ET in less than five years from the first prescription. The discontinuation rates from the one-year to the five-year treatment were 5.38, 16.70, 32.27, 51.52, and 50.00%, respectively (P < 0.001). The rates of adherence (defined as medication possession ratio ≥ 80%) from the first to the fifth year were 85.18, 82.25, 82.18, 72.92, and 73.68%, respectively (P = 0.18). Age, insurance, and surgery type impacted ET discontinuation and adherence. However, the type of medication only impacted the adherence to ET.
Conclusion
Persistence and adherence to ET in patients with breast cancer remain far from optimal and decrease over time. More attention should be paid to patients aged ≥ 70 years and those without insurance who tend to have early discontinuation of ET.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact Statements
-
Persistence and adherence to endocrine therapy for Chinese patients with breast cancer remain far from optimal.
-
Studies have shown that persistence and adherence to endocrine therapy usually decrease over five years of treatment.
-
Clinical interventions must be implemented to improve the persistence and adherence to endocrine therapy, especially for high-risk patients.
Introduction
According to the World Health Organization’s 2020 global cancer burden data, breast cancer has surpassed lung cancer as the most substantially diagnosed cancer for the first time, with an estimated 2.26 million new cases. In China, breast cancer was the fourth most common cancer, with 420,000 new cases. It is the leading cancer type in Chinese women. Hormone receptor–positive (HR +) breast cancers accounts for most breast cancers worldwide. Approximately 60% to 75% of women with breast cancer have estrogen receptor-positive (ER +) breast cancer, and 65% of these cancers are also progesterone receptor positive (PR +) [1]. Adjuvant endocrine therapy (ET) with tamoxifen or aromatase inhibitors (AIs) for 5–10 years substantially reduces recurrence and mortality in patients with HR + breast cancer [1,2,3]. Nonetheless, previous studies reported that almost half of the patients with breast cancer do not receive ET as scheduled during their recommended treatment courses. The discontinuation rates beyond five-year period range from 31 to 73%, indicating poor medication adherence and persistence [4,5,6,7].
Non-adherence and non-persistence to ET have been associated with an increased risk of breast cancer recurrence, mortality, and healthcare costs [8,9,10,11,12]. According to previous studies conducted in western countries, adverse drug reactions (ADRs) were the most commonly reported barrier to adherence to endocrine medication [6]. Other factors included age, education level, social support, comorbidities, economic reasons, doctor-patient communication, therapy method, and longer prescription refill intervals [4, 6, 7]. Given the differences in social, cultural, economic situations, and health care systems between different countries and regions, caution should be exercised when applying this experience to China.
To date, only a limited number of studies in China have investigated patients’ adherence to ET for breast cancer [13, 14]. The findings help to take targeted measures to improve medication adherence and reduce recurrence and mortality among Chinese breast cancer patients. Therefore, exploring the underlying causes of poor adherence to ET is essential and urgent.
Aim
This retrospective study aimed to evaluate the adherence to ET among Chinese patients with HR + early-stage breast cancer and identify its influencing factors.
Ethics approval
The study was carried out following the Declaration of Helsinki, and was approved by the Ethics Committee of Ren Ji Hospital School of Medicine, Shanghai Jiao Tong University (KY2021-012). The approval date was May 11, 2021.
Method
Participants
All patients who were pathologically diagnosed with breast cancer and admitted for breast surgery to a university hospital in Shanghai, China, between January 2016 and December 2020 were identified from the hospital information system (HIS). Male and female patients aged < 35 years were included in this study. For female patients aged ≥ 35 years, 50% were selected using a stratified random sampling method. Prescribing information for ET medications (tamoxifen [TAM]/toremifene [TOR] or AIs) was obtained from the outpatient clinic HIS (prescribing data was current as of June 30, 2021).
Data collection and assessment of adherence to ET
Demographic and clinical variables were obtained through a review of clinical records, including age, sex, ethnicity, medical insurance, surgical method, and ET medications. Adherence to medications was defined as the process by which patients took their medications as prescribed and was further divided into three quantifiable phases: “initiation”, “implementation”, and “discontinuation” [15]. Nonadherence to medications occurred in one or a combination of the following situations: late or non-initiation of the prescribed treatment, suboptimal implementation of the dosing regimen, or early discontinuation of therapy. The initiation status was not reported in this retrospective study. The implementation of the dose regimen for ET was most commonly assessed based on the medication possession ratio (MPR), defined as the proportion of days covered by prescription refills over the entire period (this study: 1 year) after the initial prescription of ET. Adherence was defined as an MPR of ≥ 80% [16,17,18]. Patients were classified as having early discontinuation if 180 days had elapsed from the previous prescription without a refill within five years of treatment [4, 17, 18].
Study outcomes
The primary outcomes were early discontinuation and adherence to ET. The secondary outcomes were potential factors that affected discontinuation and adherence to ET.
Statistical analyses
Normally distributed continuous variables were expressed as mean ± standard deviation, and differences were assessed using an independent t-test. Nonnormally distributed continuous variables were expressed as medians (25th to 75th percentiles), and between-group differences were assessed using the nonparametric test. Categorical variables were expressed as frequencies and percentages. Differences between these variables were determined using the chi-square test or Fisher’s exact test. Univariate and multivariate logistic regression analyses were performed to assess factors influencing adherence to ET. The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. A P value of < 0.05 was considered significant. Data were analysed using SPSS 23.0 for Windows (IBM Corp., Armonk, NY).
Results
Patient characteristics
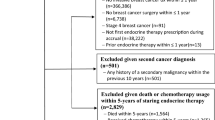
A total of 1,709 out of 3,313 patients were selected. After a match with the data in the outpatient clinic HIS, 976 patients who were prescribed ET medications were considered eligible participants. Among them, 270 patients were excluded (196 patients were not residing in Shanghai, 59 patients had only one prescription record, 25 patients had other malignant tumours or metastasis), and 706 patients were finally enrolled. All patients received at least two prescriptions for either TAM/TOR or AI after surgery.
The demographic, clinical, and medical characteristics of the patients are shown in Table 1. The median age at the time of diagnosis was 61 years (interquartile range 47–68 years). Most of them were women (99.2%), Han Chinese (99.4%), and had health insurance (89.0%). Of the 706 patients who received ET as adjuvant treatment, 525 (74.4%) were prescribed with AIs, 126 (17.8%) with TAM or TOR, and 55 (7.8%) with both TAM/TOR and AIs.
Discontinuation and adherence to ET
Among the 706 patients, 161 (22.8%) discontinued ET within 5 years of the first prescription (Fig. 1). The discontinuation rates from the one-year treatment to five-year treatment were 5.38, 16.70, 32.27, 51.52, and 50.00%, respectively (p < 0.001). The adherence rates from the first year to the fifth year were 85.18, 82.25, 82.18, 72.92, and 73.68%, respectively (P = 0.18) (Fig. 2).
Factors associated with discontinuation and adherence to ET
The results of the univariate and multivariate analyses of the potential factors affecting ET discontinuation and adherence (≤ 12 months or 12–24 months) are presented in Tables 2 and 3. Patients aged ≥ 70 years (OR: 2.11, 95% CI: 1.12–4.11, P = 0.024) or who underwent lumpectomy (OR 1.61; 95% CI 1.05–2.44; P = 0.027) were at high risk of premature discontinuation. In contrast, those with insurance were more likely to continue ET (OR: 0.54, 95% CI: 0.32–0.92, P = 0.020). Regarding the adherence rate in the first year, lumpectomy (OR: 1.75, 95% CI: 1.07–2.83, P = 0.024) and TAM/TOR + AIs (OR: 2.25, 95% CI: 1.14–4.24, P = 0.015) were the two influencing factors that decreased adherence to treatment in breast cancer patients. Regarding the adherence rate in the second year, patients taking TAM/TOR + AIs had poor adherence to ET (OR: 2.17, 95% CI: 1.06–4.28, P = 0.029). However, patients aged ≥ 70 years (OR: 0.33, 95% CI: 0.14–0.77, P = 0.012) or with insurance (OR: 0.40, 95% CI: 0.21–0.75, P = 0.004) had favourable adherence. However, the univariate analysis detected no significant association between factors and adherence in the third to fifth year.
Discussion
Statement of key findings
To our knowledge, this study was the first to evaluate long-term adherence to ET among patients with early-stage breast cancer in a first-tier city in China. The present study revealed that persistence and adherence to ET remained much less optimal and decreased over time. Almost 23% of patients discontinued ET within the 5-year treatment period. The discontinuation rates increased from 5.38% to 50.00% within five years, and the adherence rates decreased from 85.18% to 73.68%. Age, insurance, and type of surgery impacted discontinuation and adherence to ET. The type of medication had an impact only on adherence to ET medications.
Discontinuation and Adherence to ET
Studies conducted in developed countries reported the rates of discontinuation and adherence to ET in patients with HR + breast cancer ranged from 31 to 73% and from 41 to 72% over five years of treatment [4, 6, 8, 17]. Similar to these studies, we found that the 5-year discontinuation rate was 50%, while the fifth-year adherence rate was 73.68%. However, the adherence rate to ET was reported to be much higher in three other Chinese studies. A cross-sectional survey in Shenyang reported that only 13.4% of the patients discontinued adjuvant ET, and the non-persistence rates from the first year to the fifth year were 5.9, 9.1, 15.5, 16.9, and 22.6%, respectively [13]. In addition, 89.09% of the patients self-reported taking more than 80% of the medications each month. Another retrospective analysis conducted in Jilin province found that 63.1% of patients completed the 5-year ET [14]. A prospective, multi-centre, controlled, observational study (Shanghai, Beijing, Nanjing, Hangzhou) reported that the mean 1-year adherence rate (MPR ≥ 80%) was more than 95% [19].
The differences in outcomes were probably due to the way the data were obtained in different studies. The three Chinese studies used self-reported data, which were more likely to be over-reported since participants might be reluctant to admit their non-adherence to the prescribed regime. Furthermore, recall bias in older patients is another factor that can explain the overestimation of adherence in clinical and research encounters. Thus, adherence to ET derived from the self-reported survey is significantly higher than that obtained from prescription database [18, 20].
Factors associated with discontinuation and adherence to ET
We found that patients aged ≥ 70 years were more likely to be non-persistent, similar to the research conducted in Shenyang, China [13]. Regarding treatment adherence, older patients were more adherent to ET than younger patients in the second year of our study. The effects of age on discontinuation and adherence should be explored in future prospective studies. Furthermore, the previous study found that patients < 39 years had a higher discontinuation rate, possibly due to patient self-assessment of treatment benefits versus adverse drug events [13]. However, this was not observed in the present study. According to a systematic review, patients who switched to hormonal therapies were less likely to adhere to the treatment [17]. Similarly, we also found a low adherence rate among patients who switched to endocrine drugs in the first year and second year of the study. Women who used TAM had significantly higher odds of non-persistence than those who used AIs [13]. However, this was not observed in our study. TAM was not available for a relatively long period in our hospital. Many patients had to take TOR instead of TAM, and whether this affected the analysis results needs further investigation.
Financial restrictions, insurance coverage, and educational level, and previous radiotherapy and chemotherapy significantly influence adherence [14]. Furthermore, insurance and mastectomy had positive impacts on both discontinuation and adherence. ADRs are the most frequently reported barriers to ET adherence [6]. Other factors included comorbidities, doctor-patient communication, therapy method, or more prolonged prescription refill intervals [4, 6, 7]. Due to limitations in this retrospective study, several factors, such as ADRs and doctor-patient communication, were not analyzed. More prospective studies involving more potential factors are needed to investigate their association with persistence and adherence to ET.
Clinical implication
Our results provide evidence of the current situation and related factors for adherence to ET in breast cancer patients. The findings may have the following implications: recommending and implementing strategies to prevent the discontinuation of ET, attracting the attention of doctors and hospital administrators, and strengthening education on the adherence and persistence to ET among HR + breast cancer survivors, especially at-risk patients (≥ 70 years, uninsured, received lumpectomy, or underwent drug switch). Up to now, educational materials and text message reminders have been the most common interventions implemented to improve adherence to ET [21, 22]. Still, this non-personalized practice had limited effectiveness in improving adherence. More feasible and efficient interventions are urgently needed to strengthen ET adherence and extend long-term survival in HR + breast cancer patients.
Strengths and weaknesses
The strength of this study was the approach used to evaluate adherence to ET. Compared to the self-reported method used in other Chinese studies, we used MPR, a more objective way to assess medication adherence. Our study has several limitations. First, only 61 and 38 patients were followed up until the fourth and fifth-year treatment period, a small proportion of patients compared to those in the first three years. Therefore, studies with a larger sample size are warranted. Second, this was a retrospective study, and the data were collected from the HIS. We could not assess other potential factors that could affect medication adherence, such as ADR and physician–patient communication. Third, patients with breast cancer may visit different hospitals to obtain prescriptions. Data in this study were extracted from a single-centre based on the MPR, inevitably underestimating the medication adherence rate. Thus, a multi-centre trial with a more extended follow-up period should be conducted to validate the study findings.
Conclusion
The persistence and adherence to ET in patients with breast cancer in Shanghai, China, remains far from optimal and decrease over time. More attention should be paid to breast cancer patients aged ≥ 70 years and those without insurance who tend to discontinue ET early.
References
Burstein HJ, Temin S, Anderson H, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: american society of clinical oncology clinical practice guideline focused update. J Clin Oncol. 2014;32:2255–69.
Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805–16.
Howell A, Cuzick J, Baum M, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365:60–2.
Hershman DL, Kushi LH, Shao T, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients. J Clin Oncol. 2010;28:4120–8.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
Paranjpe R, John G, Trivedi M, et al. Identifying adherence barriers to oral endocrine therapy among breast cancer survivors. Breast Cancer Res Treat. 2019;174:297–305.
Wassermann J, Gelber SI, Rosenberg SM, et al. Nonadherent behaviors among young women on adjuvant endocrine therapy for breast cancer. Cancer. 2019;125:3266–74.
Hershman DL, Shao T, Kushi LH, et al. Early discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer. Breast Cancer Res Treat. 2011;126:529–37.
Makubate B, Donnan PT, Dewar JA, et al. Cohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortality. Br J Cancer. 2013;108:1515–24.
Winn AN, Dusetzina SB. The association between trajectories of endocrine therapy adherence and mortality among women with breast cancer. Pharmacoepidemiol Drug Saf. 2016;25:953–9.
Hsieh KP, Chen LC, Cheung KL, et al. Interruption and non-adherence to long-term adjuvant hormone therapy is associated with adverse survival outcome of breast cancer women–an Asian population-based study. PLoS ONE. 2014;9:e87027.
McCowan C, Wang S, Thompson AM, et al. The value of high adherence to tamoxifen in women with breast cancer: a community-based cohort study. Br J Cancer. 2013;109:1172–80.
Xu H, Jin F, Zhang XJ, et al. Adherence status to Adjuvant Endocrine Therapy in Chinese Women with Early Breast Cancer and its influencing factors: A cross-sectional survey. Cancer Med. 2020;9:3703–13.
Gao P, You L, Wu D, et al. Adherence to endocrine therapy among Chinese patients with breast cancer: current status and recommendations for improvement. Patient Prefer Adherence. 2018;12:887–97.
Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73:691–705.
Lundgren C, Lindman H, Rolander B, et al. Good adherence to adjuvant endocrine therapy in early breast cancer - a population-based study based on the Swedish Prescribed Drug Register. Acta Oncol. 2018;57:935–40.
Murphy CC, Bartholomew LK, Carpentier MY, et al. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat. 2012;134:459–78.
Hagen KB, Aas T, Kvaløy JT, et al. Adherence to adjuvant endocrine therapy in postmenopausal breast cancer patients: A 5-year prospective study. Breast Cancer Res Treat. 2019;44:52–8.
Yu KD, Zhou Y, Liu GY, et al. A prospective, multicenter, controlled, observational study to evaluate the efficacy of a patient support program in improving patients’ persistence to adjuvant aromatase inhibitor medication for postmenopausal, early stage breast cancer. Breast Cancer Res Treat. 2012;134:307–13.
Bright EE, Stanton AL. Correspondence Between Objective and Self-reported Endocrine Therapy Adherence Among Women With Breast Cancer. Ann Behav Med. 2019;53:849–57.
Ekinci E, Nathoo S, Korattyil T, et al. Interventions to improve endocrine therapy adherence in breast cancer survivors: what is the evidence? J Cancer Surviv. 2018;12:348–56.
Cathcart-Rake EJ, Ruddy KJ. Smart Technology and Endocrine Therapy Adherence. J Clin Oncol. 2020;38:2117–8.
Acknowledgements
The authors sincerely thank the physicians, nurses, and administrators in the treatment team.
Funding
This work was supported by the Clinical Research Innovation and Cultivation Fund of Ren Ji hospital (RJPY-LX-008), Research Project of Drug Clinical Comprehensive Evaluation and Drug Treatment Pathway (SHYXH-ZP-2021–001), Ren Ji Boost Project of National Natural Science Foundation of China (RJTJ-JX-001), and Shanghai “Rising Stars of Medical Talent” Youth Development Program – Youth Medical Talents – Clinical Pharmacist Program (SHWJRS (2019)_072).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, YD., Fu, J., Gu, ZC. et al. Adherence to endocrine therapy in patients with hormone receptor-positive early-stage breast cancer: a retrospective study. Int J Clin Pharm 45, 184–190 (2023). https://doi.org/10.1007/s11096-022-01450-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-022-01450-3