Abstract
Purpose
Approximately 70–80% of breast cancers are hormone receptor-positive (HR+). OET, including tamoxifen and aromatase inhibitors, is considered standard adjuvant therapy for HR+ breast cancer. Despite demonstrated benefits, nearly half of patients are non-adherent and over two-thirds discontinue therapy before the recommended 5 years. Our objective was to identify and summarize literature-reported barriers associated with non-adherence/non-persistence to OET among breast cancer survivors.
Methods
A PUBMED literature search was conducted using the following terms: ‘breast cancer,’ ‘oral endocrine therapy’ or ‘Tamoxifen’ or ‘Aromatase Inhibitors,’ ‘adherence,’ or ‘barriers.’ The search was restricted to past six years. The abstracts of each result were reviewed and categorized as either patient-reported or physician-reported. All patient- and physician-reported factors that affected adherence and persistence were listed and grouped together into the three main categories: Socio-demographic and medical parameters, general psychosocial parameters, and psychosocial parameters related to OET.
Results
A total of 320 articles were identified, of which 19 met inclusion criteria. Adverse drug reactions were the most commonly reported barrier but were generally underreported among physicians. Among patient-reported barriers, common social-demographic and medical parameters were age, comorbidity, and financial status. General psychosocial variables were lack of patient–provider communication, depressive symptoms, and lack of perceived self-efficacy. Treatment toxicity was the most commonly reported psychosocial parameter related to OET.
Conclusion
The determinants of non-adherence and non-persistence are multi-dimensional and influenced by several factors. The three categories of adherence barriers should be evaluated and considered when designing future interventions to enhance OET adherence for a tailored approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nearly 80% of breast cancers are hormone receptor-positive (HR+). Since these tumors are driven by estrogen, oral endocrine therapy (OET) that targets estrogen receptors or estrogen synthesis is a standard of care in all survivors with HR+ breast cancer [1]. Adjuvant treatment options with OET in early-stage breast cancer survivors include either a selective estrogen receptor modulator or an aromatase inhibitor, which may be combined with intramuscular injections of GnRH agonists in premenopausal women [2]. Studies have reported improved disease-free survival and improved overall breast cancer mortality for survivors on OET [1]. Clinical guidelines recommend at least 5 years of treatment to prevent recurrence and improved survival [3]. Several recent studies also suggest that 7–10 years of therapy may be superior to 5 years [4, 5]. While longer OET is clinically beneficial in survivors with early-stage HR+ breast cancer, non-adherence and non-persistence are the biggest clinical challenge in management of these survivors.
Non-adherence is defined as the failure to take medications as prescribed, while non-persistence is defined as the discontinuation of medication prior to the prescribed duration [6]. Further non-adherence can be distinguished as intentional and unintentional non-adherence [7]. While unintentional non-adherence occurs due to difficulty in remembering or lack of self-manage capacity, intentional adherence is associated with various perceptual factors like beliefs and side effects. Studies have reported non-adherence rates among breast cancer for tamoxifen ranging from 12 to 59% and 9 to 50% for aromatase inhibitors, and non-persistence beyond 5 years is reported to be between 31 and 73% [7]. Low adherence and low persistence to OET are associated with an increased risk of mortality, enhanced medical costs, and lower quality of life years [8, 9]. Studies in the UK have reported that adequate adherence to OET could save 400–500 lives annually while saving nearly 30 million dollars per year [9,10,11]. The remarkable survival benefits of improved adherence to OET demands a thorough investigation to identify the barriers associated with sub-optimal adherence. Understanding these barriers will facilitate the design of effective interventions to enhance adherence and ultimately improve associated patient outcomes.
The most commonly reported reason for non-adherence and non-persistence to OET is the side effects [12]. Other common barriers include lack of physician–patient communication, lack of information, and negative emotions associated with therapy [3, 7, 13]. However, the determinants of non-adherence and non-persistence are multi-dimensional and are influenced by several factors [12]. The decision to continue or not continue is a complicated process, occurring over a span of time, as a result of daily decisions and not a single factor [14]. It is, therefore, essential to identify all the determinants of non-adherence and non-persistence. Interventions to improve adherence to OET have been scarce in literature and have not resulted in significant improvement in adherence [12, 15]. A potential reason could be that these interventions were generally generic and were not tailored to the individual needs of each patient [12]. Determining factors associated with non-adherence and differences in these factors among various sub-groups of patients can provide a much-needed basis for a more tailed approach.
Although prior reviews have identified several barriers associated with OET, none of them have further classified them as patient-reported and physician-reported [16, 17]. The primary objective of this review was to summarize and identify all patient- and physician-reported barriers associated with non-adherence and non-persistence of OET among breast cancer survivors overall and as well as by three sub-groups: Socio-demographic and medical factors, general psychosocial factors, and factors specific to OET. These barriers can thus provide a unique and valuable insight to guide the development of future interventions to enhance adherence among breast cancer survivors.
Methods
The review was performed according to the guidelines specified in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement. A PUBMED literature search was conducted in June, 2018 using the following terms: ‘breast cancer,’ ‘oral endocrine therapy’ or ‘oral hormone therapy’ or ‘Tamoxifen’ or ‘Aromatase Inhibitors,’ ‘adherence,’ or ‘barriers.’ The search was restricted to past six years. Relevant articles were obtained from references of selected articles. Inclusion criteria were full texts published in English assessing the barriers associated with non-adherence or non-persistence of OET. Patient-reported or physician-reported survey-based studies were included. Both qualitative and quantitative survey-based studies were included. Studies were excluded if they were more than 6 years, were data-based or gene study-based, were systemic reviews, included barriers to oral chemotherapy medications, or were studies with metastatic breast cancer patients or were published as abstracts only.
Each study was reviewed, and the barriers were categorized as either patient-reported or physician-reported. All patient- and physician-reported factors that affected non-adherence and non-persistence were listed and grouped together into the three main categories: Socio-demographic factors, general psychosocial factors, and factors specific to endocrine therapy.
Results
Literature search
Our literature search identified a total of 320 articles, of which 301 were excluded based on the inclusion and exclusion criteria. A total of 19 patient-reported or physician-reported articles were evaluated in our systematic review (Fig. 1). The articles are summarized in Table 1.
Patient-reported barriers
Patient-reported barriers were categorized into three main categories (as defined by Bright et al. [7]) which are elucidated below:
Socio-demographic factors
These variables included age, marital status, insurance, income, education, transportation, working status, and employment.
Women aged 50 or less were at a higher risk of being non-adherent to OET [12, 18]. Adherence seemed to increase with age (51–69 years) and then decrease for women above 70 years of age [9, 19]. Unmarried women had a higher rate of non-adherence as compared to married women [19]. Survivors on Medicare/without insurance were less adherent than those on Medicaid/more than one source of insurance [3, 19, 20]. For women with lower income, cost of therapy acted as a barrier for adherence [6, 19]. Unintentional non-adherence was associated with higher education and in-paid employment [9]. Another study reported that non-retired survivors were at a greater risk of non-adherence compared to retired survivors [12]. Further, transportation issues were identified as a barrier to non-adherence [21].
The effect of comorbidities on patient adherence was found to be mixed. While one study reported that women with no comorbidity were less adherent than women with at least one comorbidity [3], another study reported that adherence rates varied according to the number of comorbidities. Its findings revealed that women with only one comorbidity had the highest adherence followed by women with two comorbidities further followed by women with no comorbidities. Finally, women with more than three comorbidities had the highest non-adherence [19]. Non-adherence was also associated with switch from one endocrine therapy to another [6]. Interestingly, survivors who switched from tamoxifen to aromatase inhibitors had a higher risk of non-adherence [12].
General psychosocial factors
These variables included patient–provider communication, perceived self-efficacy, social support, depressive symptoms, and lack of fear of recurrence.
A poorer patient–oncologist relationship was significantly associated with non-adherence and non-persistence [6, 20, 22]. Among younger women on tamoxifen, poorer patient–provider relationship at the time of diagnosis and the lack of opportunity to ask questions was significantly associated with its interruption. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey reflects patient–provider communication and is used to measure experiences of care (showing respect to patients, spending enough time, listening carefully, proving necessary information). A study in low-income women with breast cancer revealed that low CAHPS score were associated with lower rates of adherence as compared to higher CAHPS scores [3]. The same study measured the effect of patient-perceived self-efficacy in patient–physician interactions (PEPPI) on adherence. PEPPI scores reflect patient’s perceived capability to gather necessary medical information as well as discuss their concerns with the physician. Low PEPPI scores were associated with lower levels of adherence. Additionally another study showed a strong positive correlation between self-efficacy and medication adherence [19].
Lack of social support, which composed of the total number of family members and friends, were associated with non-persistence [20]. Depressive symptoms were associated with higher concern beliefs and non-persistence [2, 6]. Reduced fear of recurrence was associated with increased interruptions of tamoxifen among younger women and non-persistence to OET [20, 22].
Factors specific to OET
These variables were side effects, medication beliefs, negative emotions, behavioral regulation, memory, and environment stressors, as described below.
The most commonly cited barrier to OET is a significant side effect profile [3, 8, 9, 20, 21, 23,24,25]. Common side effects reported include hot flushes, muscle and joint pain, weight gain, fatigue, depression, difficulty concentrating, numbness or tingling in the extremities, vaginal dryness, and hair loss [9, 24]. Other side effects included low esteem and low libido [9]. Intentional non-adherence was greater for women who perceived that their side effects had a moderate to high impact in their daily lives [9].
Lower perceived needs and higher concerns regarding OET were significantly associated with intentional non-adherence [6, 9, 21, 22, 25]. Concerns included worries about addiction, tolerance, and long-term adverse effects, while necessity included beliefs about protection from recurrence, future health, and positivity. Another study reported the predictors of greater concern beliefs demonstrating that higher depression scores in women were associated with higher concern beliefs [2]. Negative emotions towards OET have been associated with increased non-adherence as well as non-persistence and were reported as a risk factor [6, 22].
Behavioral regulation included behavioral constructs related to organization skills and effective planning strategies for taking of OET. Non-adherent women displayed difficulty establishing a routine for taking OET and struggled to refill and self-monitor their prescriptions. They also reported memory problems and presence of environment stressors [22].
Studies that examined perceived barriers, perceived facilitators, and perceived benefits have reported that the presence of perceived barriers is significantly associated with non-adherence [7, 26]. Further, the presence of perceived barriers with no corresponding facilitator (such as cognitive self-talk, positive emotions, and self-management strategies) was the greatest risk factor of non-adherence [7].
Physician-reported barriers
While physicians reported that OET non-initiation was rare, OET non-adherence was a major concern. A significant side effect profile was reported as the main barrier [13, 27]. Lack of effective strategies for management of side effects as well as patient heterogeneity in experiencing side effects was reported as a challenge by physicians [27]. Another study revealed that physicians underreported the side effects, giving more information on joint pain, muscle pain, hot flushes, as well as sleep disturbances. However, less information was given on other quality of life areas such as hair loss, painful intercourse, and fatigue [13]. Other barriers included age, adjuvant chemotherapy, and sequential endocrine therapy [18]. Further, a study which compared physician-reported adherence with patient-reported observed that physicians estimated adherence higher than other alternative measures [18].
Lastly a study employing a multi-level framework from the provider’s perspective on barriers and facilitators to OET-related symptom management among survivors was reported. In this study, patient, provider, and system level barriers were described by providers [28]. The study reported limited time, resource constraints, and difficulty in distinguishing OET-related side effects from other condition side effects, as key barriers at both patient and provider levels. Lack of available knowledge of alternate clinical services and a general discomfort among primary care providers in management of OET-related side effects were additional barriers at the provider level. Among system level barriers, lack of cancer care coordination and complexity of the maneuvering through the system created confusion among survivors in seeking symptom management services.
Discussion
Our review summarizes patient- as well as physician-reported factors that are associated with non-adherence to OET. Patient-reported surveys, in a real-world clinic setting, are essential in understanding patient experience and perception as well as determining treatment-related side effects. Studies have demonstrated the validity of self-reported adherence surveys and one such study has shown the correlation between medication adherence measures and actual medication taking behavior [19, 29].
Our findings indicate that there is no single determinant of non-adherence; it is influenced by several factors. Our findings are validated through a recently published review article on patient-reported factors associated with non-adherence of OET [30]. However, in contrast to Lambert et al. we have summarized both physician- and patient-reported factors. Also, we have categorized related factors in three sub-groups as defined by Bright et al.: socio-demographic factors, general psychosocial factors, and factors specific to OET.
There is an urgent need to first distinguish and then identify modifiable and non-modifiable influences of OET. Although recent literature has started examining modifiable factors, they have only identified single factors that influence OET [6, 16, 26]. Thus, it is critical to identify and target a range of modifiable factors to develop innovative behavioral interventions. Our study categorized all patient-reported factors in three sub-groups among which socio-demographic factors might help in identifying target non-adherent populations but cannot be used to determine factors that modify behavior. However, the remaining two sub-groups, general psychosocial factors and factors specific to OET, potentially reflect modifiable influences that could be specifically targeted for developing interventions. Improving patient–provider communication, perceived self-efficacy, social support, depressive symptoms, medication beliefs, negative emotions, behavioral regulation, memory, and environment stressors could fall under potentially modifiable predictors of non-adherence to OET. Designing innovative interventions specific to each sub-group could provide a much-needed tailored approach.
Side effects are the major barrier in both patient-reported and physician-reported surveys. Effective management of side effects including both pharmacological and non-pharmacological strategies is essential to improve long-term adherence to OET. Various pharmacological and non-pharmacological strategies to overcome side effects of OET are available [9, 16, 31, 32]. Adequate and patient-tailored education of the potential side effects may better prepare the survivors in understanding the risks, severity, and prevention or treatment strategies [13]. Similarly, communication about the benefits of oral endocrine therapy in reducing the risk of recurrence and mortality to improve adherence by providers may be critical in improving the adherence. Studies have revealed that improved provider skills in communication, such as expressing empathy, providing all necessary information clearly, and checking if the patient understood, were associated with increased adherence to OET.
Increased utilization of health care services such as use of pharmacists, nurses, and GPs can help improve adherence to OET. Nurses and Pharmacists can validate the information provided by physicians and provide an additional opportunity for discussing patient issues or concerns. Further, they can monitor side effects and help change beliefs about the medication [9, 13]. Studies have revealed that the presence of perceived barriers and negative beliefs regarding medication was associated with non-adherence. Interventions that include motivational-interviewing (MI) by pharmacists or nurses can overcome this ambivalence, promote self-management behavior, and strengthen the internal motivation to change [33,34,35]. MI is a patient-centered style of communication that can strengthen motivation and commitment for behavioral change in a supportive, collaborative, and empathetic manner. It has been used to improve adherence in several chronic illnesses such as HIV, diabetes, and hypertension [36,37,38]. Future interventions should consider the patient characteristics summarized in this review in combination with effective strategies shown to improve adherence in other chronic illnesses like MI for designing more customized interventions.
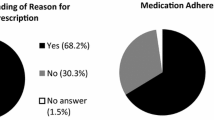
In conclusion, determinants of non-adherence are multi-dimensional and are influenced by several factors. In this review, we have categorized patient-reported barriers into socio-demographic factors, general psychosocial factors, and factors specific to OET. We have also highlighted physician-reported barriers (Fig. 2). Further, it distinguishes and identifies modifiable and non-modifiable factors of non-adherence. Future studies should design several interventions tailored for sub-groups of patient population, thereby enhancing OET adherence and further reducing breast cancer recurrence and mortality.
References
Bowles EJ, Buist DS, Chubak J, Yu O, Johnson J, Chestnut J, Boudreau DM (2012) Endocrine therapy initiation from 2001 to 2008 varies by age at breast cancer diagnosis and tumor size. J Oncol Pract 8(2):113–120
Salgado TM, Davis EJ, Farris KB, Fawaz S, Batra P, Henry NL (2017) Identifying socio-demographic and clinical characteristics associated with medication beliefs about aromatase inhibitors among postmenopausal women with breast cancer. Breast Cancer Res Treat 163(2):311–319
Liu Y, Malin JL, Diamant AL, Thind A, Maly RC (2013) Adherence to adjuvant hormone therapy in low-income women with breast cancer: the role of provider-patient communication. Breast Cancer Res Treat 137(3):829–836
Milata JL, Otte JL, Carpenter JS (2018) Oral endocrine therapy nonadherence, adverse effects, decisional support, and decisional needs in women with breast cancer. Cancer Nurs 41(1):E9–E18
Jinih M, Relihan N, Corrigan MA, O’Reilly S, Redmond HP (2017) Extended adjuvant endocrine therapy in breast cancer: evidence and update—a review. Breast J 23(6):694–705
Stanton AL, Petrie KJ, Partridge AH (2014) Contributors to nonadherence and nonpersistence with endocrine therapy in breast cancer survivors recruited from an online research registry. Breast Cancer Res Treat 145(2):525–534
Bright EE, Petrie KJ, Partridge AH, Stanton AL (2016) Barriers to and facilitative processes of endocrine therapy adherence among women with breast cancer. Breast Cancer Res Treat 158(2):243–251
Harrow A, Dryden R, McCowan C, Radley A, Parsons M, Thompson AM, Wells M (2014) A hard pill to swallow: a qualitative study of women’s experiences of adjuvant endocrine therapy for breast cancer. BMJ Open 4(6):e005285
Brett J, Fenlon D, Boulton M, Hulbert-Williams NJ, Walter FM, Donnelly P, Lavery B, Morgan A, Morris C, Watson E (2018) Factors associated with intentional and unintentional non-adherence to adjuvant endocrine therapy following breast cancer. Eur J Cancer Care 27(1):e12601
Hershman DL, Shao T, Kushi LH, Buono D, Tsai WY, Fehrenbacher L, Kwan M, Gomez SL, Neugut AI (2011) Early discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer. Breast Cancer Res Treat 126(2):529–537
Makubate B, Donnan PT, Dewar JA, Thompson AM, McCowan C (2013) Cohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortality. Br J Cancer 108(7):1515–1524
Tinari N, Fanizza C, Romero M, Gambale E, Moscetti L, Vaccaro A, Seminara P, Longo F, Gori S, Vici P et al (2015) Identification of subgroups of early breast cancer patients at high risk of nonadherence to adjuvant hormone therapy: results of an Italian survey. Clin Breast Cancer 15(2):e131–e137
Luschin G, Habersack M (2014) Oral information about side effects of endocrine therapy for early breast cancer patients at initial consultation and first follow-up visit: an online survey. Health Commun 29(4):421–426
Milata JL, Otte JL, Carpenter JS (2016) Oral endocrine therapy nonadherence, adverse effects, decisional support, and decisional needs in women with breast cancer. Cancer Nurs 41:E9–E18
Ekinci E, Nathoo S, Korattyil T, Vadhariya A, Zaghloul HA, Niravath PA, Abughosh SM, Trivedi MV (2018) Interventions to improve endocrine therapy adherence in breast cancer survivors: what is the evidence? J Cancer Surviv 12:348–356
Murphy CC, Bartholomew LK, Carpentier MY, Bluethmann SM, Vernon SW (2012) Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat 134(2):459–478
Moon Z, Moss-Morris R, Hunter MS, Carlisle S, Hughes LD (2017) Barriers and facilitators of adjuvant hormone therapy adherence and persistence in women with breast cancer: a systematic review. Patient Prefer Adherence 11:305–322
Font R, Espinas JA, Gil-Gil M, Barnadas A, Ojeda B, Tusquets I, Segui MA, Margeli M, Arcusa A, Prat A et al (2012) Prescription refill, patient self-report and physician report in assessing adherence to oral endocrine therapy in early breast cancer patients: a retrospective cohort study in Catalonia, Spain. Br J Cancer 107(8):1249–1256
Karmakar M, Pinto SL, Jordan TR, Mohamed I, Holiday-Goodman M (2017) Predicting adherence to aromatase inhibitor therapy among breast cancer survivors: an application of the protection motivation theory. Breast Cancer (Auckl) 11:1178223417694520
Cluze C, Rey D, Huiart L, BenDiane MK, Bouhnik AD, Berenger C, Carrieri MP, Giorgi R (2012) Adjuvant endocrine therapy with tamoxifen in young women with breast cancer: determinants of interruptions vary over time. Ann Oncol 23(4):882–890
Freedman RA, Revette AC, Hershman DL, Silva K, Sporn NJ, Gagne JJ, Kouri EM, Keating NL (2017) Understanding breast cancer knowledge and barriers to treatment adherence: a qualitative study among breast cancer survivors. Biores Open Access 6(1):159–168
Cahir C, Dombrowski SU, Kelly CM, Kennedy MJ, Bennett K, Sharp L (2015) Women’s experiences of hormonal therapy for breast cancer: exploring influences on medication-taking behaviour. Support Care Cancer 23(11):3115–3130
Aiello Bowles EJ, Boudreau DM, Chubak J, Yu O, Fujii M, Chestnut J, Buist DS (2012) Patient-reported discontinuation of endocrine therapy and related adverse effects among women with early-stage breast cancer. J Oncol Pract 8(6):e149–e157
Gallicchio L, Calhoun C, Helzlsouer K (2017) A prospective study of aromatase inhibitor therapy initiation and self-reported side effects. Support Care Cancer 25(9):2697–2705
Bluethmann SM, Murphy CC, Tiro JA, Mollica MA, Vernon SW, Bartholomew LK (2017) Deconstructing decisions to initiate, maintain, or discontinue adjuvant endocrine therapy in breast cancer survivors: a mixed-methods study. Oncol Nurs Forum 44(3):E101–E110
Brier MJ, Chambless DL, Gross R, Chen J, Mao JJ (2017) Perceived barriers to treatment predict adherence to aromatase inhibitors among breast cancer survivors. Cancer 123(1):169–176
Wheeler SB, Roberts MC, Bloom D, Reeder-Hayes KE, Espada M, Peppercorn J, Golin CE, Earp JA (2016) Oncology providers’ perspectives on endocrine therapy prescribing and management. Patient Prefer Adher 10:2007–2019
Samuel CA, Turner K, Donovan HAS, Beckjord E, Cardy A, Dew MA, van Londen GJ (2017) Provider perspectives on barriers and facilitators to adjuvant endocrine therapy-related symptom management. Support Care Cancer 25(12):3723–3731
Brier MJ, Chambless D, Gross R, Su HI, DeMichele A, Mao JJ (2015) Association between self-report adherence measures and oestrogen suppression among breast cancer survivors on aromatase inhibitors. Eur J Cancer 51(14):1890–1896
Lambert LK, Balneaves LG, Howard AF, Gotay CC (2018) Patient-reported factors associated with adherence to adjuvant endocrine therapy after breast cancer: an integrative review. Breast Cancer Res Treat 167(3):615–633
Archer DF, Dupont CM, Constantine GD, Pickar JH, Olivier S, Study I (2009) Desvenlafaxine for the treatment of vasomotor symptoms associated with menopause: a double-blind, randomized, placebo-controlled trial of efficacy and safety. Am J Obstet Gynecol 200(3):238–e238
Bertelli G, Venturini M, Del Mastro L, Bergaglio M, Sismondi P, Biglia N, Venturini S, Porcile G, Pronzato P, Costantini M et al (2002) Intramuscular depot medroxyprogesterone versus oral megestrol for the control of postmenopausal hot flashes in breast cancer patients: a randomized study. Ann Oncol 13(6):883–888
Miller WR, Rollnick S (2009) Ten things that motivational interviewing is not. Behav Cogn Psychother 37(2):129–140
Velasquez MSK, Dodrill C, Kan L (2005) The transtheoretical model as a framework for developing substance abuse interventions. J Addict Nurs 16:31–40
Christie D, Channon S (2014) The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: a clinical review. Diabetes Obes Metab 16(5):381–387
Abughosh S, Wang X, Serna O, Esse T, Mann A, Masilamani S, Holstad MM, Essien EJ, Fleming M (2017) A motivational interviewing intervention by pharmacy students to improve medication adherence. J Manag Care Spec Pharm 23(5):549–560
DiIorio C, McCarty F, Resnicow K, McDonnell Holstad M, Soet J, Yeager K, Sharma SM, Morisky DE, Lundberg B (2008) Using motivational interviewing to promote adherence to antiretroviral medications: a randomized controlled study. AIDS Care 20(3):273–283
Ogedegbe G, Chaplin W, Schoenthaler A, Statman D, Berger D, Richardson T, Phillips E, Spencer J, Allegrante JP (2008) A practice-based trial of motivational interviewing and adherence in hypertensive African Americans. Am J Hypertens 21(10):1137–1143
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rutugandha Paranjpe declares that she has no conflict of interest. Grace John declares that she has no conflict of interest. Meghana Trivedi declares that she has no conflict of interest. Susan Abughosh declares that she has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. Hence, it does not need any human consent.
Rights and permissions
About this article
Cite this article
Paranjpe, R., John, G., Trivedi, M. et al. Identifying adherence barriers to oral endocrine therapy among breast cancer survivors. Breast Cancer Res Treat 174, 297–305 (2019). https://doi.org/10.1007/s10549-018-05073-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-05073-z