Abstract
Purpose
The involvement of the intestinally expressed xenobiotic transporters P-glycoprotein (P-gp) and Breast Cancer Resistance Protein (BCRP) have been implicated in rivaroxaban disposition based on in vitro studies, similar to what had previously been proposed for apixaban. We recently showed that these efflux transporters were not clinically relevant for apixaban disposition and examine here their relevance for this second Factor Xa inhibitor.
Methods
Using recently published methodologies to discern metabolic- from transporter- mediated drug interactions, a critical evaluation was undertaken of 9 rivaroxaban studies reporting 12 DDIs, one study of food effects and one study of hepatic function.
Results
Rationale examination of these clinical studies using basic pharmacokinetic theory finds little support for the clinical significance of intestinal efflux transporters in rivaroxaban disposition. Drug-drug interactions are most likely adequately predicted based on the level of CYP 3A metabolism.
Conclusion
These analyses indicate that inhibition of efflux transporters appears to have negligible, clinically insignificant effects on the rivaroxaban absorption process, which is consistent with the concern that predictions based on in vitro measures may not translate to a clinically relevant interaction in vivo. We emphasize the need to evaluate gastric emptying, dissolution and other processes related to absorption when using MAT changes to indicate efflux transporter inhibition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
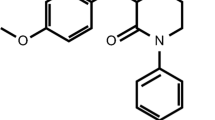
Rivaroxaban is a highly selective and direct Factor Xa inhibitor used to prevent thrombin generation that is increasingly used clinically for the prevention and treatment of thromboembolism due to its ease of use and improved patient compliance as compared to warfarin (1,2,3,4). Rivaroxaban has also been approved for reduction of stroke risk in patients with non-valvular atrial fibrillation, and for prevention and treatment of deep vein thrombosis (5). The most severe adverse effect of rivaroxaban is bleeding and evidence suggests that renal or hepatic dysfunction or drug-drug interactions (DDIs) that increase exposure to rivaroxaban have the potential to increase the risk of bleeding complications (6).
Recently we reported that the intestinal efflux transporters P-gp and BCRP were not clinically relevant for apixaban (7), another approved Factor Xa inhibitor. Here we evaluated the relevance of those intestinal efflux transporters on the disposition of rivaroxaban, suspecting that our analysis may not be as clear-cut since rivaroxaban is a Biopharmaceutics Drug Disposition Classification System (BDDCS) Class 2 drug versus apixaban being a BDDCS Class 1 drug. The BDDCS system suggests that transporter effects would generally be clinically irrelevant for highly soluble, extensively metabolized Class 1 drugs (8), but that intestinal efflux transporters may exhibit clinically relevant interactions for poorly soluble highly metabolized BDDCS Class 2 drugs (9).
Rivaroxaban is eliminated mainly by hepatic metabolism and renal excretion (10, 11). Approximately 51% of an orally administered [14C]-rivaroxaban dose was recovered as inactive metabolites in urine (30%) and feces (21%). Oxidative degradation catalyzed by CYP3A4/5 and CYP2J2 and hydrolysis are the major routes of biotransformation (12).
Based on in vitro studies, rivaroxaban is also a substrate of the efflux transporters P-gp and BCRP (13,14,15). According to the BDDCS classification system, rivaroxaban belongs to Class 2 due to its low solubility and high permeability and thus intestinal apical efflux transporters might be expected to exert an effect on absorption (9). A 2013 clinical study conducted by Mueck et al. (16) investigated rivaroxaban and P-gp/CYP3A4 inhibitors in healthy volunteers, concluding that rivaroxaban can be co-administered with P-gp and/or CYP3A4 substrates/moderate inhibitors, such as clarithromycin, erythromycin and fluconazole, but not with strong P-gp/CYP3A4 inhibitors such as ritonavir and ketoconazole due to the substantially increased rivaroxaban exposure. The FDA approved label for rivaroxaban states that concomitant use with known combined P-gp and strong CYP3A inhibitors or inducers should be avoided (12). However, no analysis related to differentiating the contribution of efflux transporter and enzymes on disposition of rivaroxaban in vivo has been conducted. Due to the in vitro evidence that rivaroxaban is a substrate of efflux transporters, it was of interest to examine the potential of rivaroxaban to interact with perpetrator drugs that can inhibit efflux transporters. Inhibition of intestinal transporters has the potential to alter the absorption rate of a drug in addition to the amount absorbed (17), whereas enzyme inhibition can only influence the amount of drug absorbed, but not the rate of absorption.
The present study evaluates changes in rivaroxaban absorption time when rivaroxaban is co-administered with other drugs or differing conditions to understand if the efflux transporter inhibition potential observed in vitro has any clinical significance.
Materials and Methods
A systematic literature search was conducted to identify published pharmacokinetic drug interaction studies performed in humans of rivaroxaban in combination with perpetrator drug. PubMed, Medline and Google Scholar were searched from inception through December 2020. The search was restricted to studies with published pharmacokinetic curves with at least 2 time points (except for those only depicting time zero and time to maximal concentration (tmax)) in the absorption phase. Pharmacokinetic profiles were then digitized to generate parameters including area under the curve (AUC), area under the moment time curve (AUMC), maximum concentration (Cmax), tmax, terminal half-life (t1/2) and apparent clearance (CL/F) via non-compartmental analysis with WinNonlin® Professional Edition Version 2.1 (Pharsight, Mountain View, CA). The values of AUC from the digitized curves were compared to published values, and only included in this analysis if these values were within 20% of one another, indicating that the published average pharmacokinetic profiles adequately represented the data. As previously described (17), the concentration-time data were then fit to a two-compartment model with first order absorption using WinNonlin®, and mean absorption time (MAT) was calculated as reciprocal of the first order absorption rate constant. Mean residence time (MRT) was calculated as the ratio of AUMC0-∞ divided by AUC0-∞ minus MAT. The ratios of these pharmacokinetic parameters, treated group to control group, were also calculated. Ratios calculated from published parameters were reported in priority, with digitized results supplementing values that were not specifically reported in the investigated studies. The results are shown in Table I for drug-drug interactions and Table II for food effects and hepatic dysfunction, with values derived from publications specifically noted with the superscript “R”. Pharmacokinetic parameters that displayed a decrease more than 30% and an increase more than 43% (i.e. ratios outside of the range of 0.70 and 1.43) were considered as potential evidence of a clinically significant interaction. These limits are equivalent on a logarithmic scale, similar to ranges utilized to compare bioequivalence.
According to the FDA draft guidance on predicting drug-drug interactions (49), an orally dosed drug has the potential to inhibit intestinal enzymes and transporters in vivo if the total concentration in gut (Igut) is larger than ten-fold of IC50, where Igut = dose of inhibitor/250 mL. Therefore, IC50 values of perpetrator drugs against BCRP/P-gp were identified from the literature and used to calculate Igut/IC50 for P-gp and BCRP for each perpetrator drug. These values are reported in Table I as an indication of potential to inhibit intestinal efflux transporters.
Results
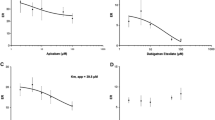
The literature search identified 9 studies with published rivaroxaban concentration-time profiles that included a total of 12 perpetrator drugs, one food-rivaroxaban interaction and one study investigating rivaroxaban disposition with respect to hepatic dysfunction. Among the 12 perpetrator drugs, 7 had the potential to inhibit intestinal P-gp and/or BCRP (clarithromycin (16), erythromycin (16), ketoconazole (16), ritonavir (16), omeprazole (41), cyclosporine (22) and verapamil (44)), one was a P-gp inducer (St John’s Wort (36) (SJW)), but it was co-administered with macitentan (not a BCRP but potentially a P-gp inhibitor), and the remaining 3 perpetrators are neither inhibitors or inducers of intestinal efflux transporters (aspirin (18), fluconazole (16), and naproxen (39)). Table I shows the ratios of rivaroxaban pharmacokinetic parameters with and without addition of different perpetrator drugs. Table II shows the influence of food or hepatic function on rivaroxaban pharmacokinetic parameters (47, 48). Of the 8 P-gp/BCRP inhibitors, 4 exhibited changes in AUC greater than 43% (clarithromycin, cyclosporine, ketoconazole and ritonavir), with 2 others quite close (fluconazole, 42%; verapamil 39% in healthy volunteers and 42% in mild renal failure patients). However, only one of these perpetrators (ritonavir) showed a decrease in MAT greater than 30%, (accompanied by a tmax change in the opposite direction, an increase of 33%). Although cyclosporine caused a greater than 43% increase in rivaroxaban AUC, slower absorption could be implied by the 50% increase in tmax, although only a 10% increase in MAT was observed. Fluconazole (a clinically recommended index inhibitor of CYP3A4) (50) exhibited a 42% increase in AUC and no changes in MAT nor tmax, consistent with its lack of inhibitory effects on P-gp/BCRP. Aspirin showed significant increases in MAT by 2.42-fold and macitentan plus SJW resulted in a 33% decrease in MAT. As for tmax, aspirin and naproxen exhibited a marked increase (2-fold for each) but macitentan (without SJW) decreased tmax by 31%. Food also increased MAT and tmax, with modest, clinically insignificant effects on AUC and CL/F (Table II). In hepatic dysfunctional patients, only moderate hepatic dysfunction subjects exhibited decreased CL/F (ratio of 0.43), but MAT showed no significant change in these patients. In patients with mild hepatic dysfunction, MAT decreased by 40% but CL/F showed no change (Table II).
Discussion
The results of this analysis indicate that the intestinal efflux transporters are not strongly involved in the absorption phase of rivaroxaban contrary to what had been previously hypothesized by the field and suggested in the package insert (12). To verify this, MAT and tmax changes were examined in DDIs studies involving rivaroxaban with P-gp/BCRP inhibitors versus non-inhibitors. Rivaroxaban is suggested to be a substrate of P-gp and BCRP, therefore inhibition of P-gp or BCRP is expected to result in decreases in MAT and tmax as the efflux transporters suggested to be involved in rivaroxaban disposition can no longer cycle rivaroxaban between the enterocytes and intestinal lumen, thereby decreasing absorption rate. When rivaroxaban was co-administered with inhibitors of P-gp or BCRP, the MAT and tmax values for rivaroxaban do not increase by more than 43% or decrease by more than 30% except for ritonavir, where MAT decreased but tmax did not. Generally, changes in tmax can be used to reflect changes absorption rate only if terminal half-life remains unchanged, as we have recently discussed in detail (17). The tmax value can be obtained by directly examining the concentration-time curve with understanding that it depends strongly on the sampling frequency (51) and can also be affected by the elimination half-life (t½) as previously discussed (17). MAT is a relatively more sensitive value that is only a function of the absorption rate, which directly reflects changes in absorption caused by inhibition, activation or induction of intestinal transporters. Our laboratory has previously recognized that the action of P-gp and BCRP inhibitors and inducers result in altered absorption rate because these transporters are highly expressed apically in the intestine and serve as an effective barrier to the intestinal absorption of numerous substrates (17). The absence of a corresponding change in tmax can be explained by the concomitant change in substrate elimination from the systemic circulation (52). However, none of the DDI studies included in this investigation reported changes in absorption rate in individual patients as the focus of those studies was on how drug exposure changed.
From our results, we report that among the 12 perpetrator drugs, including significant in vitro inhibitors of P-gp/BCRP, most of them did not markedly change MAT except for ritonavir and aspirin. Of the 8 P-gp and/or BCRP inhibitors only ritonavir resulted in more than a 30% MAT change (decreased by 52%), while the even more potent inhibitors such as ketoconazole (with Igut/IC50 values of approximately 200 for BCRP and 500–2000 for P-gp) did not change MAT. Ritonavir is potentially a strong inhibitor of P-gp (Igut/IC50 = 118–876) and BCRP (Igut/IC50 = 504). Although our calculated MAT change for this interaction indicated increased absorption rate, the authors reported a 33% increase in tmax with a 21% increase in terminal half-life suggesting either a slight decrease in absorption rate or no change.
Concomitant dosing of aspirin exhibited the greatest increase in MAT (2.42-fold) with a comparable 2.0-fold increase in reported tmax (18), but no significant change in exposure (AUC). There are no reports of aspirin either inducing or inhibiting xenobiotic transporters. However, absorption time may change due to additional factors beyond transporter inhibition or induction, such as changes in gastric emptying rate, drug dissolution rate and permeability, as these processes can also be the rate-limiting steps during drug absorption (52). Aspirin can also prolong gastric emptying, which may have contributed to the observed 2.42-fold increase in MAT, as there is evidence of delayed time to peak blood-ethanol levels after treatment with low dose aspirin (53). The mechanism is attributed to the inhibition by aspirin of endogenous prostaglandins to produce macroscopic changes of the gastric mucosa (54, 55).
Verapamil has the potential to inhibit P-gp according to its Igut/IC50 ratio, which would result in a decreased MAT ratio. However, co-administration of verapamil resulted in the counterintuitive 1.33-fold increase in MATin healthy volunteers, but no change in patients with mild renal function. With respect to transporters, increase in MAT may be caused by 1) induction or activation of efflux transporters or 2) inhibition of intestinal uptake transporters. Our laboratory has previously demonstrated the potential for P-gp to be activated (56), although we did not find any literature supporting P-gp activation by verapamil. Further, no literature evidence exists for involvement of uptake transporters in rivaroxaban disposition. However, it has been demonstrated that in addition to inhibitory effects on CYP3A4 and P-gp, verapamil can also induce CYP3A4 (57). Considering that the expression of CYP3A4 and P-gp are regulated by the same transcription factor PXR, P-gp may also be induced by verapamil (58). In the healthy volunteer study, verapamil was dosed for 10 days (120 mg, day 1; 240 mg, day 2; 360 mg, days 3–10), therefore the potential for P-gp induction may be a possibility. Verapamil is a calcium-channel blocker, in a class of drugs that exert their effect by inhibiting calcium entry into cells, which can potentially decrease gastric smooth muscle contraction and delay gastric emptying. Studies in preclinical species have demonstrated delayed gastric emptying caused by verapamil (59), and the results in humans reported a slight decrease in gastric emptying rate (60).
Another confounding study is the DDI interaction with macitentan in the presence and absence of additional SJW co-administration (36). Of the 11 drug DDI studies with rivaroxaban in Table I, macitentan is the only perpetrator to cause both MAT and tmax to decrease close to 30%, but there is no effect on AUC and CL/F. Dhillon (61), summarizing macitentan published DDI studies, reports that although macitentan is a CYP3A4 substrate, showing changes in macitentan kinetics with strong inhibitors and inducers of CYP3A, in vitro studies of macitentan “did not have clinically relevant inhibitory or inducing effects on CYP enzymes” nor inhibit hepatic or renal transporters including P-gp. However, “in vitro macitentan inhibits the breast cancer resistance protein at clinically relevant intestinal concentrations”. These findings are in concordance with the DDI results listed in Table I (36). Further addition of SJW, yields no change in the MAT decrease, but increases the observed ratio of tmax change to 0.95, with an observed 35% increase in CL/F and a 26% decrease in t½. Chronic use of SJW (12 days in the present study) can markedly induce CYP3A4 metabolism and can also induce the expression of P-gp (36, 37, 62). Although the decrease in AUC of rivaroxaban in the presence of chronic SJW and macitentan was only on average 26% and no clinically relevant change in endothelin antagonism was observed, the authors recommend (36) that “the combination of SJW with rivaroxaban should be avoided.” In the present analysis, it is possible that an intestinal transporter interaction is occurring, but it is difficult to confirm its relevance considering the other studies analyzed here.
Our study has limitations. First, estimation of MAT from computer fitting of mean concentration time curves rather than from individual pharmacokinetic profiles of the study population may be confounding as we have previously noted (17). Second, some drugs are absorbed relatively quickly after oral administration; therefore, depending on the design of the clinical study, if the pharmacokinetic curve does not have enough points in absorption phase, this will affect the integrity of the calculated absorption rate constants.
Conclusions
The analyses here indicate that inhibition of intestinal efflux transporters have minimal, clinically insignificant effects on rivaroxaban absorption, which is consistent with the concern that in vitro measures may not always translate to clinically significant in vivo relevance. However, the data here for rivaroxaban are not as consistent as our previous analysis of apixaban data (7). We emphasize, particularly for BDDCS Class 2 poorly soluble drugs, the need to consider gastric emptying, drug dissolution and other factors related to absorption rate when utilizing MAT changes to evaluate the involvement of intestinal transporters in drug disposition.
Abbreviations
- AUC:
-
Area under the curve
- AUMC:
-
Area under the moment time curve
- BCRP:
-
Breast cancer resistance protein
- CL/F:
-
Apparent clearance
- Cmax :
-
Maximum concentration
- CYP:
-
Cytochrome P450
- DDIs:
-
Drug-drug interactions
- Igut :
-
Maximum perpetrator concentration in gut
- MAT:
-
Mean absorption time
- MRT:
-
Mean residence time
- P-gp:
-
P-glycoprotein
- SJW:
-
St. John’s Wort
- tmax :
-
Time of maximum concentration
- t1/2 :
-
Terminal half-life
References
Hellwig T, Gulseth M. Pharmacokinetic and pharmacodynamic drug interactions with new oral anticoagulants: what do they mean for patients with atrial fibrillation? Ann Pharmacother. 2013;47(11):1478–87.
Mega JL, Simon T. Pharmacology of antithrombotic drugs: an assessment of oral antiplatelet and anticoagulant treatments. Lancet. 2015;386(9990):281–91.
Plitt A, Ruff CT, Giugliano RP. Non-vitamin K antagonist oral anticoagulants in atrial fibrillation. Hematol Oncol Clin North Am. 2016;30(5):1019–34.
Nutescu EA, Burnett A, Fanikos J, Spinler S, Wittkowsky A. Pharmacology of anticoagulants used in the treatment of venous thromboembolism. J Thromb Thrombolysis. 2016;41(1):15–31.
Buller HR, Lensing AW, Prins MH, Agnelli G, Cohen A, Gallus AS, et al. A dose-ranging study evaluating once-daily oral administration of the factor Xa inhibitor rivaroxaban in the treatment of patients with acute symptomatic deep vein thrombosis: the Einstein-DVT dose-ranging study. Clin Trials Observ. 2008;112(6):2242–7.
Goodman SG, Wojdyla DM, Piccini JP, White HD, Paolini JF, Nessel CC, et al. Factors associated with major bleeding events: insights from the ROCKET AF trial (rivaroxaban once-daily oral direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation). J Am Coll Cardiol. 2014;63(9):891–900.
Sodhi JK, Liu S, Benet LZ. Intestinal efflux transporters P-gp and BCRP are not clinically relevant in apixaban disposition. Pharm Res. 2020;37(10):208.
Wu CY, Benet LZ. Predicting drug disposition via application of BCS: transport/absorption/ elimination interplay and development of a biopharmaceutics drug disposition classification system. Pharm Res. 2005;22(1):11–23.
Shugarts S, Benet LZ. The role of transporters in the pharmacokinetics of orally administered drugs. Pharm Res. 2009;26(9):2039–54.
Mueck W, Stampfuss J, Kubitza D, Becka M. Clinical pharmacokinetic and pharmacodynamic profile of rivaroxaban. Clin Pharmacokinet. 2014;53(1):1–16.
Weinz C, Schwarz T, Kubitza D, Mueck W, Lang D. Metabolism and excretion of rivaroxaban, an oral, direct factor Xa inhibitor, in rats, dogs, and humans. Drug Metab Dispos. 2009;37(5):1056–64.
Rivaroxaban package insert. Full prescribing information.2020. Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/202439s031,022406s035lbl.pdf. Accessed Dec 2020.
Gong IY, Kim RB. Importance of pharmacokinetic profile and variability as determinants of dose and response to dabigatran, rivaroxaban, and apixaban. Can J Cardiol. 2013;29(7):S24–33.
Schinkel AH, Wagenaar E, Mol CA, Deemter LV. P-glycoprotein in the blood-brain barrier of mice influences the brain penetration and pharmacological activity of many drugs. J Clin Invest. 1996;97(11):2517–24.
Gnoth MJ, Buetehorn U, Muenster U, Schwarz T, Sandmann S. In vitro and in vivo P-glycoprotein transport characteristics of rivaroxaban. J Pharmacol Exp Ther. 2011;338(1):372–80.
Mueck W, Kubitza D, Becka M. Co-administration of rivaroxaban with drugs that share its elimination pathways: pharmacokinetic effects in healthy subjects. Br J Clin Pharmacol. 2013;76(3):455–66.
Sodhi JK, Benet LZ. The necessity of using changes in absorption time to implicate intestinal transporter involvement in oral drug-drug interactions. AAPS J. 2020;22(5):111.
Kubitza D, Becka M, Mueck W, Zuehlsdorf M. Safety, tolerability, pharmacodynamics, and pharmacokinetics of rivaroxaban-an oral, direct factor Xa inhibitor-are not affected by aspirin. J Clin Pharmacol. 2006;46(9):981–90.
Cook JA, Feng B, Fenner KS, Kempshall S, Liu R, Rotter C, et al. Refining the in vitro and in vivo critical parameters for P-glycoprotein, [I]/IC50 and [I2]/IC50, that allow for the exclusion of drug candidates from clinical digoxin interaction studies. Mol Pharm. 2010;7(2):398–411.
Eberl S, Renner B, Neubert A, Reisig M, Bachmakov I, König J, et al. Role of P-glycoprotein inhibition for drug interactions: evidence from in vitro and pharmaco epidemiological studies. Clin Pharmacokinet. 2007;46(12):1039–49.
Kellick KA, Bottorff M, Toth PP. The National Lipid Association's safety task force. A clinician's guide to statin drug-drug interactions. J Clin Lipidol. 2014;8:S30–46.
Brings A, Lehmann ML, Foerster KI, Burhenne J, Weiss J, Haefeli WE, et al. Perpetrator effects of ciclosporin (P-glycoprotein inhibitor) and its combination with fluconazole (CYP3A inhibitor) on the pharmacokinetics of rivaroxaban in healthy volunteers. Br J Clin Pharmacol. 2019;85(7):1528–37.
Sugimoto H, Matsumoto S, Tachibana M, Niwa S, Hirabayashi H, Amano N, et al. Establishment of in vitro P-glycoprotein inhibition assay and its exclusion criteria to assess the risk of drug-drug interaction at the drug discovery stage. J Pharm Sci. 2011;100(9):4013–23.
Rautio J, Humphreys JE, Webster LO, Balakrishnan A, Keogh JP, Kunta JR, et al. In vitro P-glycoprotein inhibition assays for assessment of clinical drug interaction potential of new drug candidates: a recommendation for probe substrates. Drug Metab Dispos. 2006;34(5):786–92.
Ozvegy C, Litman T, Szakács G, Nagy Z, Bates S, Váradi A, et al. Functional characterization of the human multidrug transporter, ABCG2, expressed in insect cells. Biochem Biophys Res Commun. 2001;285(1):111–7.
Xia CQ, Liu N, Miwa GT, Gan LS. Interactions of cyclosporin A with breast cancer resistance protein. Drug Metab Dispos. 2007;35(4):576–82.
Ekins S, Kim RB, Leake BF, Dantzig AH, Schuetz EG, Lan LB, et al. Three-dimensional quantitative structure-activity relationships of inhibitors of P-glycoprotein. Mol Pharmacol. 2002;61(5):964–73.
Eriksson UG, Dorani H, Karlsson J, Fritsch H, Hoffmann KJ, Olsson L, et al. Influence of erythromycin on the pharmacokinetics of ximelagatran may involve inhibition of P-glycoprotein-mediated excretion. Drug Metab Dispos. 2006;34(5):775–82.
Franke RM, Lancaster CS, Peer CJ, Gibson AA, Kosloske AM, Orwick SJ, et al. Effect of ABCC2 (MRP2) transport function on erythromycin metabolism. Clin Pharmacol Ther. 2011;89(5):693–701.
Wang EJ, Lew K, Casciano CN, Clement RP, Johnson WW. Interaction of common azole antifungals with P glycoprotein. Antimicrob Agents Chemother. 2002;46(1):160–5.
Lempers VJC, van den Heuvel JJMW, Russel FGM, Aarnoutse RE, Burger DM, Brüggemann RJ, et al. Inhibitory potential of antifungal drugs on ATP-binding cassette transporters P-gp, MRP1-5, BCRP and BSEP. Antimicrob Agents Chemother. 2016;60(6):3372–9.
Keogh JP, Kunta JR. Development, validation and utility of an in vitro technique for assessment of potential clinical drug-drug interactions involving P-glycoprotein. Eur J Pharm Sci. 2006;27(5):543–54.
Wang E, Casciano CN, Clement RP, Johnson WW. The farnesyl protein transferase inhibitor SCH66336 is a potent inhibitor of MDR1 product P-glycoprotein. Cancer Res. 2001;61(20):7525–9.
Vermeer LMM, Isringhausen CD, Ogilvie BW, Buckley DB. Evaluation of ketoconazole and its alternative clinical CYP3A4/5 inhibitors as inhibitors of drug transporters: the in vitro effects of ketoconazole, ritonavir, clarithromycin, and itraconazole on 13 clinically-relevant drug transporters. Drug Metab Dispos. 2016;44(3):453–9.
Gupta A, Unadkat JD, Mao QC. Interactions of azole antifungal agents with the human breast cancer resistance protein (BCRP). J Pharm Sci. 2007;96(12):3226–35.
Huppertz A, Werntz L, Meid AD, Foerster KI, Burhenne J, Czock D, et al. Rivaroxaban and macitentan can be co administered without dose adjustment but the combination of rivaroxaban and St John’s Wort should be avoided. Br J Clin Pharmacol. 2018;84(12):2903–13.
Weiss J, Theile D, Ruppell MA, Speck T, Spalwisz A, Haefeli WE. Interaction profile of macitentan, a new non-selective endothelin-1 receptor antagonist, in vitro. Eur J Pharmacol. 2013;701(1–3):168–75.
Lepist EI, Gillies H, Smith W, Hao J, Hubert C, St Claire RL, et al. Evaluation of the endothelin receptor antagonists ambrisentan, bosentan, macitentan, and sitaxsentan as hepatobiliary transporter inhibitors and substrates in sandwich-cultured human hepatocytes. PLoS One. 2014;9(1):e87548.
Kubitza D, Becka M, Mueck W, Zuehlsdorf M. Rivaroxaban (BAY 59-7939) - an oral, direct factor Xa inhibitor - has no clinically relevant interaction with naproxen. Br J Clin Pharmacol. 2006;63(4):469–76.
Saito H, Hirano H, Nakagawa H, Fukami T, Oosumi K, Murakami KA. New strategy of high-speed screening and quantitative structure-activity relationship analysis to evaluate human ATP-binding cassette transporter ABCG2-drug interactions. J Pharmacol Exp Ther. 2006;317(3):1114–24.
Moore KT, Plotnikov AN, Thyssen A, Vaccaro N, Ariyawansa J, Burton PB. Effect of multiple doses of omeprazole on the pharmacokinetics, pharmacodynamics, and safety of a single dose of rivaroxaban. J Cardiovasc Pharmacol. 2011;58(6):581–8.
Neuhoff S, Langguth P, Dressler C, Andersson TB, Regårdh CG, Spahn-Langguth H. Affinities at the verapamil binding site of MDR1-encoded P-glycoprotein: drugs and analogs, stereoisomers and metabolites. Int J Clin Pharmacol Ther. 2000;38(4):168–79.
Breedveld P, Zelcer N, Pluim D, Sönmezer O, Tibben MM, Beijnen JH, et al. Mechanism of the pharmacokinetic interaction between methotrexate and benzimidazoles: potential role for breast cancer resistance protein in clinical drug-drug interactions. Cancer Res. 2004;64(16):5804–11.
Greenblatt DJ, Patel M, Harmatz JS, Nicholson WT, Rubino CM, Chow CR. Impaired rivaroxaban clearance in mild renal insufficiency with verapamil co-administration: potential implications for bleeding risk and dose selection. J Clin Pharmacol. 2018;58(4):533–40.
Römermann K, Wanek T, Bankstahl M, Bankstahl JP, Fedrowitz M, Müller M. (R)-[(11)C] verapamil is selectively transported by murine and human P-glycoprotein at the blood-brain barrier, and not by MRP1 and BCRP. Nucl Med Biol. 2013;40(7):873–8.
Zhang Y, Gupta A, Wang HG, Zhou L, Vethanayagam RR, Unadkat JD, et al. BCRP transports dipyridamole and is inhibited by calcium channel blockers. Pharm Res. 2005;22(12):2023–34.
Kubitza D, Becka M, Zuehlsdorf M, Mueck W. Effect of food, an antacid, and the H2 antagonist ranitidine on the absorption of BAY 59-7939 (rivaroxaban), an oral, direct factor Xa inhibitor, in healthy subjects. J Clin Pharmacol. 2006;46(5):549–58.
Kubitza D, Roth A, Becka M, Alatrach A, Halabi A, Hinrichsen H, et al. Effect of hepatic impairment on the pharmacokinetics and pharmacodynamics of a single dose of rivaroxaban, an oral, direct factor Xa inhibitor. Br J Clin Pharmacol. 2013;76(1):89–98.
U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER). In vitro drug interaction studies – cytochrome P450 enzyme- and transporter- mediated drug interactions guidance for industry. 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/vitro-drug-interaction-studies-cytochrome-p450-enzyme-and-transporter-mediated-drug-interactions. Accessed Dec 2020.
Tornio A, Filppula AM, Niemi M, Backman JT. Clinical studies on drug-drug interactions involving metabolism and transport: methodology, pitfalls, and interpretation. Clin Pharmacol Ther. 2019;105(6):1345–61.
Han YR, Lee PI, Pang KS. Finding Tmax and Cmax in multi compartmental models. Drug Metab Dispos. 2018;46(11):1796–804.
Martinez MN, Amidon GL. A mechanistic approach to understanding the factors affecting drug absorption: A review of fundamentals. J Clin Pharmacol. 2002;42(6):620–43.
Kechagias S, Jonsson KA, Norlander B, Carlsson B, Jones AW. Low-dose aspirin decreases blood alcohol concentrations by delaying gastric emptying. Eur J Clin Pharmacol. 1997;53:241–65.
Leivonen M, Sipponen P, Kivilaakso E. Gastric changes in coronary operated patients with low-dose aspirin. Scand J Gastroenterol. 1992;27(11):912–6.
Prichard PJ, Kitchingman GK, Walt RP, Daneshmend TK, Hawkey CJ. Human gastric mucosal bleeding induced by low-dose aspirin, but not warfarin. BMJ. 1989;298(6672):493–6.
Soldner A, Christians U, Susanto M, Wacher VJ, Silverman JA, Benet LZ. Grapefruit juice activates P-glycoprotein-mediated drug transport. Pharm Res. 1999;16(4):478–85.
Fahmi OA, Maurer TS, Kish M, Cardenas E, Boldt S, Nettleton D. A combined model for predicting CYP3A4 clinical net drug-drug interaction based on CYP3A4 inhibition, inactivation, and induction determined in vitro. Drug Metab Dispos. 2008;36(8):1698–708.
Manda VK, Avula B, Dale OR, Ali Z, Khan IA, Walker LA, et al. PXR mediated induction of CYP3A4, CYP1A2, and P-gp by Mitragyna speciose and its alkaloids. Phytother Res. 2017;31(12):1935–45.
Brage R, Cortijo J, Esplugues J, Esplugues JV, MartiBonmati E, Rodriguez C. Effects of calcium channel blockers on gastric emptying and acid secretion of the rat in vivo. Br J Pharmacol. 1986;89(4):627–33.
Krevsky B, Maurer AH, Niewiarowski T, Cohen S. Effect of verapamil on human intestinal transit. Dig Dis Sci. 1992;37(6):919–24.
Dhillon S. Macitentan: A review of its use in patients with pulmonary arterial hypertension. Drugs. 2014;74(13):1495–507.
Perlo MD, Moltke LV, Störmer E, Shader RI, Greenblatt DJ. Saint John's Wort: an in vitro analysis of P-glycoprotein induction due to extended exposure. Br J Clin Pharmacol. 2001;134(8):1601–8.
ACKNOWLEDGEMENTS AND DISCLOSURES
This work was supported in part by a Mary Ann Koda-Kimble Seed Award for Innovation. Ms. Kou’s stay in the UCSF Benet Laboratory was supported by the Educational Foundation Program of Lanzhou University. Dr. Sodhi was supported in part by an American Foundation for Pharmaceutical Education Predoctoral Fellowship, NIGMS grant R25 GM56847 and a Louis Zeh Fellowship. Dr. Benet is a member of the UCSF Liver Center supported by NIH grant P30 DK026743. All authors contributed to the writing and analysis of this manuscript. The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kou, W., Sodhi, J.K., Wu, X. et al. Investigating Intestinal Transporter Involvement in Rivaroxaban Disposition through Examination of Changes in Absorption. Pharm Res 38, 795–801 (2021). https://doi.org/10.1007/s11095-021-03039-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-021-03039-3