The effect of mexidol (M) and nitroxymexidol (NM) on the activity of phosphodiesterase of cyclic guanosine monophosphate (PDEcGMP), regulation of lipid peroxidation (LPO), and antiradical and antihypoxic activity was investigated under normoxia and normobaric hypercapnic hypoxia conditions. Reversible and noncompetitive inhibition of the hydrolytic function of PDEcGMP by M and NM was revealed. The Ki value for M was 1 ×10–4 M; for NM, 1 ×10–5 M, i.e., NM was 10 times more active than M. It was shown that the lifetime of experimental animals in a closed space increased by 36% under the action of M as compared with that of the control group while it increased by 53% for NM. The ventricular contraction time increased by 137% for NM. The atrial contraction time increased from 31 min in the control to 52 and 57 min for M and NM, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Syntheses of new highly effective and non-toxic drugs capable of generating NO during biotransformation have recently been developed at the IPCP, RAS [1, 2].
A new non-toxic mexidol derivative, nitroxymexidol (NM), was synthesized at the IPCP, RAS [5].
The goal of the present work was to study the roles of M and NM in the regulation of LPO, antiradical protection, modulation of cyclic guanosine monophosphate (cGMP) phosphodiesterase (PDE) activity, and antihypoxic activity with normoxia and hypercapnic normobaric hypoxia.
Experimental Part
We used cGMP nucleotidase (as cobra venom), histidine, and Tris-HCl (Sigma) without additional purification. Trichloroacetic acid and ammonium molybdate (Reakhim, Russia) were purified before use. Mexidol (M) was synthesized as before [6]. Nitroxymexidol (NM) was synthesized by the literature method [5] with its nitro group bonded to succinic acid. It was 98% pure according to GC.
PDE of cGMP (PDEcGMP) was isolated from the brain cortex of male Wistar rats [7]. Brain tissue was homogenized in a Potter homogenizer in ten times the weight of cold Tris-HCl buffer (0.2 M) at pH 7.5. The homogenate was centrifuged for 1 h at 40,000 g in a K-32M centrifuge. The supernatant containing the enzyme was frozen in liquid nitrogen.

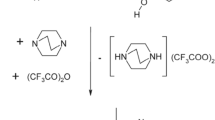
The protein concentration was determined by a modified Lowry method [8]. The activity of PDEcGMP in the presence and absence of M and NM was derived from the amount of GMP formed during the enzymatic reaction, which was equal to the amount of inorganic phosphate formed from GMP upon adding the nucleotidase [6]. The overall reaction scheme was:
Tris buffer (1 mL, 0.2 M, pH 7.6) was treated with PDEcGMP solution containing 1 mg of protein. The studied compounds (100, 10, and 1 μM) were added to the enzyme, pre-incubated for 30 min at room temperature, and treated with substrate (0.1 mM cGMP).
The samples were stored in a thermostat at 30°C for 20 min. Samples were also incubated on a boiling-water bath for 3 – 5 min and cooled to room temperature. Then, cobra venom (50 μg) was added. The samples were stored at 30°C for 10 min. The reaction was stopped by adding trichloroacetic acid (0.2 mL, 55%) to each sample. The mixture was centrifuged at 4,500 rpm for 15 min. The PDEcGMP activity in the presence (test) and absence (control) of the compounds was determined from the amount of inorganic phosphate accumulated during the enzymatic reaction using spectroscopy at 735 nm on a Specord M-40 spectrophotometer (Carl Zeiss).
The relative activity of the enzyme was calculated using the formula
where I is the relative activity; A 0, the specific content of inorganic phosphate in the control (without compounds); A, the specific content of inorganic phosphate in the test sample (with compounds).
The reversibility of the compound action was determined using dialysis of samples containing enzyme with (100 μM) and without the compounds in the samples. The dialysis was performed against a 100-fold excess of the incubation medium without the compounds for 24 h at 4 – 5°C.
The nature of PDEcGMP inhibition was determined by the literature method [9]. The rate of the enzymatic reaction as a function of the substrate (cGMP) concentration with (100 μM) and without the compounds was investigated. The PDEcGMP enzymatic reaction as a function of substrate concentration was plotted in Lineweaver—Burke coordinates.
Spontaneous LPO of C57BL male mouse (22 – 24 g) brain homogenate was carried out in Tris-HCl buffer (0.1 M) at pH 7.4, protein concentration 1 mg/mL, and 36°C for 30 min with (test) or without (control) the compounds [10]. The extent of LPO was determined from the formation of diene conjugates (DC) [11]; antiradical activity, by chemiluminescence [12].
Hypoxia with hypercapnia was studied in 30 male mice (18 – 20 g). Animals were placed in 250-mL glass jars with hermetic lids that were immersed in water to avoid an influx of air. M and NM were injected i.p. at a dose of 5 mg/kg 30 min before hypoxia. The time for onset of agonal responses was recorded.
Cardiac hypoxia was studied using an “open heart” model. The chest cavity was opened after animals were sacrificed by cervical dislocation. The duration of ventricular and atrial contractile activity in the control and after injection of M and NM was noted. The myocardium was wetted periodically with normal saline from a pipette in order to avoid desiccation. The compounds were injected i.p. 30 min before decapitation at a dose of 5 mg/kg.
Results and Discussion
The effects of M and NM on PDEcGMP activity were compared. Accumulation of cGMP, a secondary messenger involved in the regulation of vessel tone and leukocyte aggregation, is known to occur upon PDEcGMP inhibition [13–15].
Table 1 shows that M and NM inhibited PDEcGMP functioning.
NM was the most pronounced enzyme inhibitor. It at a concentration of 10 μM inhibited cGMP cleavage by 85 ±9%; at 1.0 μM, by 53 ±6%. This was significantly greater than inhibition by M, 42 ±8% and 30 ±5%, respectively. The effects of the different M and NM concentrations on cGMP hydrolysis indicated that they reacted differently with the enzyme.
The cGMP hydrolysis rate with and without the compounds was studied as a function of substrate concentration (from 0.1 to 0.01 mM) in order to determine the mechanism of action of M and NM on cGMP hydrolysis.
The results were plotted in Lineweaver—Burke coordinates (Fig. 1). It was shown that Km of cGMP for PDEcGMP was 8 ×10–5 M. Inhibition of the PDEcGMP hydrolytic function by M and NM was found to be non-competitive. The Ki of M was 1 ×10–4 M; of NM, 1 ×10–5 M. Therefore, NM was an order of magnitude more active than M.
The results indicated that M and NM did not interact directly with the enzyme active site.
Table 2 shows that M and NM were reversible PDEcGMP inhibitors. The enzyme activity was fully restored after dialysis of the enzyme solution containing M and NM (0.1 mM) against Tris-HCl buffer (200 mL) without the compounds for 24 h at 4 – 5°C. This indicated that M and NM were non-covalently bound to the enzyme.
Thus, the results indicated that inhibition of PDEcGMP substrate hydrolysis by newly synthesized NM was preferred over that by M.
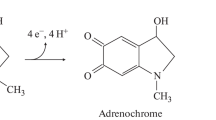
Figures 2 and 3 compare the antihypoxic activities of NM and M in two experimental models.
The results (Fig. 2) indicated that the lifetime of the animals in the closed space increased by 36% relative to the control through the action of M whereas this parameter for NM was 53%.
The duration of contractile activity of the various heart sections (Fig. 3) indicated that ventricular contraction time increased by 122% after administration of M and by 137% for NM. The atrial contraction time increased from 31 min for the control to 52 and 57 min for M and NM, respectively.
Thus, the comparison of M and NM indicated that NM had more pronounced antihypoxic effects than M. It was shown that NM caused hemodynamic effects that were similar to those of other NO(donors, i.e., reduced the demand of myocardium for oxygen by reducing the ventricle wall strain; by lowering arterial pressure and ventricle volume; by improving the oxygen supply to myocardium as a result of decreased blood flow, coronary resistance, and coronary artery spasm; and by decreasing coronary blood flow. These effects suggested that NM was an NO donor.
The genesis and progression of various pathologies are related to disruption of equilibrium in LPO systems, i.e., antioxidant protection, which requires the appropriate adjustment using exogenous antioxidants [16, 17].
The extent of LPO was estimated directly by determining the contents of primary oxidation products of diene conjugates [11]. Figure 4 shows the results. It can be seen that M and NM decreased the diene conjugate content by 19 and 22%, respectively (difference statistically insignificant). The antiradical activities of M and NM were measured using chemiluminescence [12] and were statistically significant (Table 3). Thus, chemiluminescence was 50% inhibited for M at a concentration of 4.3 ×10–5 M; for NM, 7.3 ×10–6 M.
The comparison of M and NM indicated that NM had more pronounced antihypoxic and antiradical activity than M. The results enabled NM to be recommended for further study as a potential drug for treating infarcts, strokes, and other vascular diseases.
References
T. N. Roudneva, N. Sanina, D. Mischenko, et al., Nitric Oxide: Biol. Chem., 19, Supplement, 43 (2008).
L. V. Tat’yanenko, O. V. Dobrokhotova, R. A. Kotel’nikov, et al., Pharm. Chem. J., 45(6), 329 – 332 (2011).
L. M. Baider, O. L. Belaya, Z. V. Kuropteva, et al., Vopr. Biol. Med. Farm. Khim., No. 3, 44 – 47 (2009).
R. G. Glushkov, S. D. Yuzhakov, M. V. Alekseev, et al., Khim.-farm. Zh., 45(3), 3 – 8 (2011); Pharm. Chem. J., 45(3), 131 –136 (2011).
B. S. Fedorov, M. A. Fadeev, V. N. Varfolomeev, et al., RU Pat. No. 2,394,815, Jul. 20, 2010, “Nitroxy-succinate 2-ethyl-6-methyl-3-oxypyridine (versions of use) and method for producing said compound.”
V. K. Promonenkov and V. P. Rutkovskij, RU Pat. No. 2,211,833, Sep. 10, 2003, “Method for preparing 2-ethyl-6-methyl-3-hydroxy-pyridine.”
R. E. Liberzon, T. T. Shchekoldina, and O. S. Vatolkina, Vopr. Med. Khim., 4, 526 – 530 (1977).
J. L. Bailey, Techniques in Protein Chemistry, Elsevier Pub. Co., New York (1967) [Russian translation pp. 53 – 60].
I. B. Berezin and A. A. Khlesov, Practical Course in Chemical and Enzyme Kinetics [in Russian], Izd. MGU, Moscow (1976), pp. 77 – 84.
R. A. Kotel’nikova, D. V. Mishchenko, D. A. Zhokhova, et al., High Energy Chem., 43(7), 582 – 586 (2010).
T. F. Slater, Methods Enzymol., 105, 283 – 293 (1984).
R. F. Kotel’nikova and I. I. Faingol’d, Izv. Akad. Nauk, Ser. Khim., 6, 1146 – 1150 (2011).
F. Rind, Mod. Drug Discovery, Nov / Dec, 31 (1998).
V. G. Granik and N. B. Grigor’ev, Izv. Akad. Nauk, Ser. Khim., 8, 1268 – 1272 (2002).
V. G. Granik and N. B. Grigor’ev, Nitric Oxide (NO). New Pathway to Drug Discovery [in Russian], Vuzovskaya Kniga, Moscow (2004), p. 360.
R. A. Kotel’nikova, I. I. Faingold, D. A. Poletaeva, et al., Russ. Chem. Bull., 60(6), 1172 – 1176 (2011).
A. I. Kotel’nikov, G. N. Bogdanov, D. V. Mishchenko, et al., Al’manakh Klin. Med., 1(17), 199 – 200 (2008).
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Khimiko-Farmatsevticheskii Zhurnal, Vol. 48, No. 7, pp. 3 – 6, July, 2014.
Rights and permissions
About this article
Cite this article
Tat’yanenko, L.V., Dobrokhotova, O.V., Varfolomeev, V.N. et al. Effect of Mexidol and Nitroxymexidol on Phosphodiesterase Activity, Some Oxidation Processes, and Hypoxia Resistance. Pharm Chem J 48, 417–420 (2014). https://doi.org/10.1007/s11094-014-1123-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11094-014-1123-6