Abstract
Purpose
There remains no standard of care for patients with recurrent and chemorefractory glioblastoma. Re-irradiation (reRT) provides an additional management option. However, published series predominantly focus on small reRT volumes utilizing stereotactic hypofractionated regimens. Concerns regarding toxicity have limited utilisation of reRT for larger recurrences, however this may be mitigated with use of bevacizumab (BEV).
Methods and materials
A prospective database of patients managed with the EORTC-NCIC (Stupp) protocol 60 Gy chemoradiotherapy protocol for glioblastoma between 2007 and 2021 was reviewed for those patients receiving reRT for chemorefractory relapse. Serial MRI and PET were used to establish true progression and exclude patients with pseudoprogression or radionecrosis from reRT. The primary endpoint was overall survival (OS) from date of reRT. Prognostic factors were also assessed.
Results
447 patients managed for glioblastoma under the Stupp protocol were identified, of which 372 had relapsed and were thus eligible for reRT. 71 patients underwent reRT. Median relapse-free survival from diagnosis for the reRT and overall cohorts were similar at 11.6 months (95%CI:9.4–14.2) and 11.8 months (95%CI:9.4–14.2) respectively. 60/71 (85%) reRT patients had received BEV prior to reRT and continued concurrent BEV during reRT. Of the 11 patients not managed with BEV during reRT, 10 required subsequent salvage BEV. ReRT patients were younger (median 53 vs. 59 years, p < 0.001), had better performance status (86% vs. 69% ECOG 0–1, p = 0.002) and more commonly had MGMT promoter-methylated tumours (54% vs. 40%, p = 0.083) compared to non-reRT patients. Median reRT PTV volume was 135cm3 (IQR: 69-207cm3). Median OS from reRT to death was 7.1 months (95%CI:6.3–7.9). Patients aged < 50, 50–70 and > 70 years had post-reRT median OS of 7.7, 6.4 and 6.0 months respectively (p = 0.021). Median post-reRT survival was longer for patients with ECOG performance status 0–1 compared to 2–3 (8.1 vs. 6.3 months, p = 0.039). PTV volume, site of relapse, MGMT promoter-methylation status and extent of initial surgical resection were not associated with post-reRT survival. ReRT was well-tolerated. Out of the 6 patients (8%) admitted to hospital after reRT, only one was for reRT toxicity. This was a CTCAE grade 3 radiation necrosis event in a patient managed without prior BEV.
Conclusion
Patients with recurrent glioblastoma who have been previously treated with 60 Gy radiotherapy have a meaningful survival benefit from large volume re-irradiation which is well tolerated. ReRT should not be ignored as a salvage treatment option in patients with chemorefractory progressive disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) is the most common malignant primary brain tumour in adults. However, there remains no standard of care for patients with a chemorefractory relapse of this disease following definitive treatment and multiple salvage systemic therapy regimens [1].
Glioblastoma typically has a poor outcome at relapse, with a median overall survival of 18 months and post-relapse median survival of 6 months [2]. The limited treatment options at relapse include surgical resection, second or third line systemic therapy, and best supportive care. More recently, Bevacizumab (BEV) has become a standard choice of therapy for recurrent GBM, especially following its approval by the United States Food and Drug Administration in 2009 [3]. BEV in combination with reRT has also been effective in minimizing concerns regarding the risk of CNS radionecrosis [4].
Reirradiation (reRT) is also an accepted treatment option at relapse of GBM, but current evidence is predominantly for small volume reRT (PTV 5-50cm3/median of 20-40cm3) delivered with stereotactic techniques. However, a frequent clinical presentation is of large volume relapses (PTV > 75cm3), of which there is little data to support reirradiation to this volume [5].
Studies have demonstrated the feasibility and safety of delivering large volume reRT concurrently with Bevacizumab in high grade gliomas [5]. There are legitimate concerns regarding the risk of radiation necrosis with escalated volume and doses of reRT [6]. Our earlier data for all high grade gliomas has shown that it is both feasible and safe with an improvement in clinical outcome when delivered in conjunction with Bevacizumab [5].
ReRT for relapsed GBM in particular is therefore emerging as a safe management option, but outcome data for this approach remains limited for patients with chemorefractory recurrent GBM following previous EORTC-NCIC (Stupp) protocol chemoradiotherapy to 60 Gy, who have had disease progression following multiple salvage systemic therapy regimens. These patients tend to have tumours of a larger volume, as reflected by the median PTV of 135cm3 in our study.
The aim of this retrospective study was to demonstrate the outcome of reRT in conjunction with BEV, and whether that treatment option can be of benefit to patients with large volume recurrent GBM that cannot be managed with further systemic therapy regimens, surgical resection, stereotactic radiosurgery or brief hypofractionation regimens.
Method
A retrospective analysis was performed from an established prospective patient database approved by the Institutional Ethics Review Board. 447 patients with glioblastoma who had previously received EORTC-NCIC 60 Gy radiotherapy between 2007 and 2021 were identified.
Patient selection
Patients included in the analysis included those with a diagnosis of GBM initially managed with EORTC-NCIC 60 Gy radiotherapy with concurrent temozolomide (TMZ). These patients had radiological or histopathological evidence of intracranial recurrence/disease progression. Stringent efforts were made to distinguish progressive disease from pseudoprogression and radionecrosis via use of sequential MRI, 18F-Fluoro-ethyl-tyrosine (FET) and 18F-Fluoro-deoxyglucose (FDG) PET scans and multidisciplinary review. Relapse was defined as local, marginal or distant based upon relationship to initial defined gross tumour volume (GTV or the surgical cavity and residual tumour). If more than 50% of the recurrent tumour was within the GTV it was defined aslocal relapse; if 50% of tumour was outside the GTV but within 20 mm of the GTV it was then defined as marginal; and 50% of tumour outside a 20 mm margin from the GTV was recorded as distant failure. Patients were chemorefractory with an Eastern Cooperative Oncology Group (ECOG) performance status of 0–3.
Chemorefractory disease
Chemorefractory disease was defined as radiological or symptomatic progression after a minimum of one course of salvage systemic cytotoxic chemotherapy (after having completed EORTC-NCIC definitive chemoradiotherapy with concurrent and adjuvant Temozolomide to 60 Gy at the time of initial diagnosis), thus correlating to the second or third episode of tumour progression. Most patients in this analysis also had disease progression on BEV.
67 (94%) patients were managed after progression on salvage chemotherapy, which was usually two sequential agents by time of referral for ReRT. Salvage regimens were re-introduction of temozolomide either as single agent or in combination with procarbazine; lomustine and BEV. No cytotoxic chemotherapy other than BEV was delivered concurrently with ReRT.
Concurrent BEV was delivered at doses between 5 and 10 mg/m2 every 2 weeks, then subsequently maintained at 2–4 weekly intervals until cessation at clinical deterioration.
Reirradiation
Eligible patients required a history of previous EORTC-NCIC 60 Gy radiotherapy with concurrent temozolomide. ReRT was defined as the subsequent course of radiotherapy with overlap of the regions to at least a dose of 30 Gy in 2 Gy equivalent fractions. Post-Bevacizumab target volumes were defined by T2FLAIR + DWI MRI sequences and clarified by FET PET if target volume delineation was uncertain.
Non isotropic margins were used to delineate the CTV (GTV + 5 mm and + 20 mm along neural tracts).
IMRT or VMAT technique was used, and 35-40 Gy was delivered over 10–15 fractions. Cumulative dose tolerances included chiasm sum of less than 75 Gy, and brainstem sum of less than 85 Gy. Brain dose hotspots above 100 Gy were accepted. The summative plans werecalculated in the Varian ECLIPSE software using total doses.
Study endpoints
The primary endpoints for analysis included the median survival, and the 6-month overall survival (OS) rates following reRT. The relapse-free survival (RFS) post reRT and the median OS from date of diagnosis were also analysed.
Other endpoints included hospitalisation rates (during the reRT period), functional status pre-reRT, and site of subsequent relapse (local within the reRT PTV versus distant to reRT PTV).
Statistical analysis
The data were summarized/presented as mean, standard deviation (symmetric normal data), median, range (skewed data or ordinal data), proportions, and hazard ratios with a 95% confidence interval (CI). Kaplan-Meier survival analysis was used to summarize (median with 95% CI) and present (Kaplan-Meier survival curve) the overall and progression-free survival time distribution. Log-rank test was used to compare the survival time distribution across patient sub-groups to assess the factors associated with improved survival post-reRT.
The Cox-proportional hazards regression was used to estimate the hazard ratio (risk of death or progression) for patient sub-groups. The proportionality assumption in Cox regression was tested using the Schoenfeld residuals test.
Test of median age at diagnosis between ReRT and non-ReRT patients was performed using Mood’s median test. The proportion of patients with ECOG score 0 or 1, the extent of resection equal to sub-total (50 − 90%), and patients with MGMT between ReRT and non-ReRT patients were performed using Chi-square test or Fisher’s exact test for small samples or expected frequencies.
All the statistical tests were performed at a 0.05 level of significance. All statistical analyses were performed in STATA V16.0.
Results
447 patients treated for glioblastoma between 2007 and 2021 were identified. The median follow-up time for all surviving patients was 37.7 months (95% CI: 24.1–53.4). The median overall survival time from diagnosis for the entire cohort was 18.0 months (95% CI: 17.0–19.2). There were 396 progression events: 237 local, 28 marginal, 95 distant, and 36 combined local and distant. The median progression-free survival time was 11.8 months (95% CI: 11.0–12.5).
A total of seventy-one patients with a chemo refractory, recurrent glioblastoma were managed with reRT, all of whom were previously treated with EORTC-NCIC (Stupp Protocol) 60 Gy radiotherapy. 301 patients with a GBM were eligible for but did not have reRT (non-reRT patients). The median overall survival from initial diagnosis for the reRT patient subgroup was 23.6 months (95% CI: 21.0-33.1). The median progression-free survival from initial diagnosis was 11.66 months (95% CI: 9.36 − 14.19).
Patient characteristics
The demographics of the full cohort and ReRT administration can be seen in Table 1. Patients were aged between 17 and 80 years with a median age of 58 years, 95% CI: 57–60. Median age at diagnosis was lower in the subgroup of patients who received reRT, compared with non-reRT patients (53 years compared with 59 years respectively, p < 0.001). At time of initial diagnosis, 71% (n = 317) of the whole cohort had an ECOG performance status of 0 or 1, while 86% (n = 61) of the reRT subgroup had an ECOG status of 0 or 1 (p = 0.002). The median Ki67 was 30%. With respect to MGMT status, 32% (n = 142) had no methylation and 28% (n = 124) had promoter methylation. The percentage of patients with wildtype IDH1 was 95% (n = 424). More than 50% of patients had a local recurrence (n = 237).
The PTV volume, MGMT promoter methylation status, site of initial relapse and extent of initial surgical resection were not significant predictors of whether a patient received reRT.
The reRT schedule was 40 Gy in 15 fractions and 35 Gy in 10 fractions in 32 (45%) and 28 (39%) patients respectively. Eight (11%) patients received other schedules (36, 30 or 25 Gy). The median PTV volume was 135 cc (range 1-360 cc). 60 of 71(85%) reRT patients had previously progressed on BEV and continued concurrent BEV during reRT. An additional 10/71(14%) had salvage BEV after reRT.
Outcomes
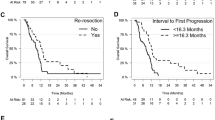
Post-ReRT survival
Figure 1 represents the Kaplan-Meier curve for post-ReRT survival time. The median overall survival time post-ReRT was 7.1 months (95% CI: 6.3–7.9) and the 6-month post-reRT overall survival rate was 63.4% (45 of 71 patients).
Overall survival
The median overall survival from initial diagnosis for the ReRT patients (n = 71) was 23.1 months (95% CI: 20.8–32.1). The median overall survival time for patients who were eligible for but did not receive ReRT (n = 301) was 16.2 months (95% CI: 15.3–17.8, p = < 0.001).
Prognostic factors
Table 2 presents the results of univariate analysis for predictors of overall survival time following reRT.
Predictors of improved overall survival following radiotherapy were younger age (p = 0.021), a period greater than 24 months from diagnosis to reRT (p = 0.045) and ECOG performance status of 0–1 (p = 0.039).
Patients aged < 50, 50–70 and > 70 years had post-reRT median overall survival of 7.7, 6.4 and 6.0 months respectively (p = 0.021). Patients older than 70 years who underwent reRT had poorer survival compared to patients aged 70 years or less (p < 0.001). Each additional year in age was associated with an average increase of 4% in the risk of death (HR = 1.04, 95% CI: 1.02–1.06).
The median survival time for patients with ECOG score 0 or 1 (median survival = 8.1 months, 95% CI: 7.0–9.5) was significantly higher (p = 0.039) than those with ECOG score 2 or 3 (median survival = 6.3 months, 95% CI: 5.0–7.1). Patients with ECOG score 2 or 3 had a higher risk of death post-reRT, compared to patients with ECOG 1 or 2 (HR = 1.66, 95% CI: 1.0–2.7, p = 0.046).
The median survival time was significantly greater when reRT was undertaken 24 months or more following initial diagnosis (median survival = 8.5 months, 95% CI: 7.0–10.5, p = 0.045) as compared with reRT performed less than 2 years from diagnosis (less than 12 months: median survival = 6.5 months, 95% CI: 2.6–9.0, and 12–24 months: median survival = 6.4, 95% CI: 4.8–7.7).
Factors not associated with post-reRT survival included PTV volume (p = 0.91), ReRT regimen (p = 0.63), anatomical location (p = 0.65), pattern of local or distant recurrence (p = 0.87) and MGMT promoter methylation status (p = 0.77).
Safety
Of 6(8%) admissions to hospital within 30 days of reRT, only 1 was for reRT-related toxicity. This was a CTCAE grade 3 radiation necrosis event in a patient managed without prior BEV.
Discussion
In a cohort of patients with chemorefractory and predominantly bevacizumab-refractory recurrent large volume glioblastoma, our study achieved a median OS from time of reRT of 7.1 months. Historical data presented by Magnuson et al. in their analysis of 16 phase II trials in the setting of recurrent glioblastoma demonstrated a median overall survival of 3.8 months from time of bevacizumab failure, with no further treatments [7]. A more recent appraisal of historical studies utilising conventional or hypo-fractionated reirradiation (24 to 36 Gy, with daily fractional size of 1.8 to 6 Gy) for recurrent glioblastoma with large tumour volume demonstrated a progression free survival of 5.4 months from time of reirradiation [8]. Previous data has also shown that chemorefractory and bevacizumab-refractory disease progression in recurrent GBM is associated with decline over 4–6 weeks [9]. Thus, the survival time of 7 months in this current study following addition of reRT in this broad subgroup of selected patients appears favourable, and this is the largest study to date on the role of reirradiation in this cohort of patients with large volume recurrent GBM with very limited treatment options.
The recent RTOG 1205 study comparing Bevacizumab delivered with re-irradiation (35 Gy in 10 fractions covering contrast enhancing disease) in a large cohort of 170 patients with relapsed GBM with Bevacizumab alone has demonstrated a significant benefit in median and 6-month progression free survival rates [10]. The median PTV in the RTOG 1205 study was 54cm3, which is again much smaller than this current study median of 135cm3, but was well tolerated. The overall survival rate following re-RT was similar in this current study, despite larger target volumes, which included coverage of non-enhancing disease.
Magnuson et al. have also demonstrated in a small group of 23 patients that large volume reirradiation (median PTV 424cm3) initiated for recurrent GBM that progressed on bevacizumab was well tolerated with minimal grade 3–4 toxicities, and demonstrated a median OS and 6 month OS of 6.9 months and 65% respectively, using a pulsed-reduced dose rate technique [7]. While the technique is different and the cohort is smaller, these results undoubtedly support the use of large volume reirradiation in this clinical setting of recurrent GBM refractory to bevacizumab alone. Our study has also demonstrated that the reRT regimen and PTV volume were not associated with a detriment to survival in the patients receiving reRT.
The novel nature of this current study is that all patients were previously managed with high dose (60 Gy) RT, and had chemorefractory disease with large volume relapse. There has been limited data available regarding reirradiation of large volumes after prior high dose RT, as previous studies have primarily focused on treating patients with a smaller volume of disease (PTV < 40cm3) and often at initial relapse. The results of a current literature review of “large volume re-irradiation” of relapsed glioblastoma is outlined in Table 3 [5, 7, 10,11,12,13,14,15], and we note that studies with other high grade glioma pathologies have been included in this review. The authors have previously been able to demonstrate the safety of large volume reRT in patients who are unsuitable for surgical resection and/or stereotactic radiosurgery with varying glioma pathologies when delivered in conjunction with bevacizumab [5].
Current prognostic scores that have been developed are largely directed at patients for consideration of small volume reirradiation for all recurrent gliomas, such as the Combs score, which utilises factors including the patient age (above or below 50), and time interval from initial radiotherapy (more or less than 12 months) [16]. This current study has provided further insight into factors that may have more specific application to large volume irradiation in recurrent GBM. Perhaps unsurprisingly, younger age, better performance status and longer time since commencement of initial therapy were all associated with more favourable outcomes in this group of patients.
This is a retrospective study with non-randomised data. Our toxicity data is limited. Notably patients selected for reRT tended to be younger and with better functional status. The study cohort was relatively small (71 patients) but is much larger than any other study that has investigated large-volume reirradiation in this context.
The authors continue to consider the use of FET PET with MRI imaging in assisting with delineation of reRT target volumes. This is a significant consideration for future studies to allow improved tumour coverage in infiltrating non-enhancing disease. Future studies may collect further information regarding treatment toxicity, radiological response, performance status, quality of life, steroid use, and the role of Bevacizumab following re-irradiation. The impact of timing of reRT delivery (either earlier at the commencement of BEV or later at the time of BEV-refractory disease) on the median survival benefit of reRT is also for further investigation.
Conclusion
There is a meaningful median overall survival following large volume reirradiation for chemorefractory recurrent GBMs who have previously received radical chemoradiotherapy to 60 Gy and multiple salvage systemic therapy regimens, particularly in patients who are younger and of better performance status. In combination with bevacizumab, large volume reirradiation in this group of patients is feasible and well tolerated. This data supports large volume reRT as a viable approach when faced with a large volume, chemorefractory GBM recurrence with limited alternative treatment options.
References
Minniti G, Niyazi M, Alongi F, Navarria P, Belka C (2021) Current status and recent advances in reirradiation of glioblastoma. Radiation Oncology. 2021;16(1)
Jayamanne D, Wheeler H, Cook R, Teo C, Brazier D, Schembri G et al (2017) Survival improvements with adjuvant therapy in patients with glioblastoma. ANZ J Surg 88(3):196–201. https://doi.org/10.1111/ans.14153
Ghiaseddin A, Peters KB (2015) Use of Bevacizumab in recurrent glioblastoma. CNS Oncol 4(3):157–169. https://doi.org/10.2217/cns.15.8
Levin VA, Bidaut L, Hou P, Kumar AJ, Wefel JS, Bekele BN et al (2011) Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. IJROBP 79(5):1487–1495. https://doi.org/10.1016/j.ijrobp.2009.12.061
Chan J, Jayamanne D, Wheeler H, Khasraw M, Wong M, Kastelan M et al (2020) The role of large volume re-irradiation with Bevacizumab in chemorefractory high grade glioma. Clin Translational Radiation Oncol 22:33–39
Ho ALK, Jena R (2018) Re-irradiation in the brain: primary gliomas. Clin Oncol 30(2):124–136. https://doi.org/10.1016/j.clon.2017.11.006
Magnuson W, Ian Robins H, Mohindra P, Howard S (2014) Large volume reirradiation as salvage therapy for glioblastoma after progression on bevacizumab. J Neurooncol 117(1):133–139. https://doi.org/10.1007/s11060-014-1363-z
Kim I (2019) Appraisal of re-irradiation for the recurrent glioblastoma in the era of MGMT promotor methylation. Radiat Oncol J 37(1):1–12. https://doi.org/10.3857/Froj.2019.00171
Cuncannon M, Wong M, Jayamanne D, Guo L, Cove N, Wheeler H et al (2019) Role of delayed salvage bevacizumab at symptomatic progression of chemorefractory glioblastoma. BMC Cancer 19(1). https://doi.org/10.1186/s12885-019-5678-1
Tsien CI, Pugh SL, Dicker AP, Raizer JJ, Matuszak MM, Lallana EC et al (2023) NRG Oncology/RTOG1205: a randomized phase II trial of concurrent bevacizumab and reirradiation versus bevacizumab alone as treatment for recurrent glioblastoma. J Clin Oncol 41(6):1285–1295. https://doi.org/10.1200/jco.22.00164
Fokas E, Wacker U, Gross MW, Henzel M, Encheva E, Engenhart-Cabillic R (2009) Hypofractionated stereotactic reirradiation of recurrent glioblastomas. Strahlenther Onkol 185(4):235–240. https://doi.org/10.1007/s00066-009-1753-x
Dixit KS, Sachdev S, Amidei C, Kumthekar P, Kruser TJ, Gondi V et al (2021) A multi-center prospective study of re-irradiation with bevacizumab and temozolomide in patients with bevacizumab refractory recurrent high-grade gliomas. J Neurooncol 155(3):297–306. https://doi.org/10.1007/s11060-021-03875-8
Maranzano E, Anselmo P, Casale M, Trippa F, Carletti S, Principi M et al (2011) Treatment of recurrent glioblastoma with stereotactic radiotherapy: long-term results of a mono-institutional trial. Tumori J 97(1):56–61. https://doi.org/10.1177/030089161109700111
Arpa D, Parisi E, Ghigi G, Savini A, Colangione SP, Tontini L et al (2020) Re-irradiation of recurrent glioblastoma using helical tomotherapy with simultaneous integrated boost: preliminary considerations of treatment efficacy. Sci Rep 10(1). https://doi.org/10.1038/s41598-020-75671-9
Adkison JB, Tomé W, Seo S, Richards GM, Robins HI, Rassmussen K et al (2011) Reirradiation of large-volume recurrent glioma with pulsed reduced-dose-rate radiotherapy. IJROBP 79(3):835–841. https://doi.org/10.1016/j.ijrobp.2009.11.058
Combs SE, Edler L, Rausch R, Welzel T, Wick W, Debus J (2012) Generation and validation of a prognostic score to predict outcome after re-irradiation of recurrent glioma. Acta Oncol 52(1):147–152. https://doi.org/10.3109/0284186x.2012.692882
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the manuscript. E.T. and P.H. authored the main manuscript text, and M.B., H.W., M.W., J.C., and M.K. were instrumental in the conception, design, acquisition and clinical interpretation of the data. V.V. drafted the analysis of the data. All authors reviewed and were involved in the revisions of the manuscript, and M.B. approved the version of the manuscript to be published.
Corresponding author
Ethics declarations
Ethical approval
This study was performed utilising an established prospective patient database approved by the Institutional Ethics Review Board.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tong, E., Horsley, P., Wheeler, H. et al. Hypofractionated re-irradiation with bevacizumab for relapsed chemorefractory glioblastoma after prior high dose radiotherapy: a feasible option for patients with large-volume relapse. J Neurooncol 168, 69–76 (2024). https://doi.org/10.1007/s11060-024-04643-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-024-04643-0