Abstract
Introduction
The treatment of brain metastases with stereotactic radiosurgery (SRS) in combination with immune checkpoint inhibitors (ICI) has become more common in recent years, but there is a lack of prospective data on cancer control outcomes when these therapies are administered concurrently.
Methods
Data were retrospectively reviewed for patients with non-small cell lung cancer (NSCLC) and melanoma brain metastases treated with SRS at a single institution from May 2008 to January 2017. A parametric proportional hazard model is used to detect the effect of concurrent ICI within 30, 60, or 90 days of ICI administration on local control and distant in-brain control. Other patient and lesion characteristics are treated as covariates and adjusted in the regression. A frailty term is added in the baseline hazard to capture the within-patient correlation.
Results
We identified 144 patients with 477 total lesions, including 95 NSCLC patients (66.0%), and 49 (34.0%) melanoma patients. On multivariate analysis, concurrent SRS and ICI (SRS within 30 days of ICI administration) was not associated with local control but was associated with distant brain control. When controlling for prior treatment to lesion, number of lesions, and presence of extracranial metastases, patients receiving this combination had a statistically significant decrease in distant brain failure compared to patients that received non-concurrent ICI or no ICI (HR 0.15; 95% CI 0.05–0.47, p = 0.0011).
Conclusion
Concurrent ICI can enhance the efficacy of SRS. Prospective studies would allow for stronger evidence to support the impact of concurrent SRS and ICI on disease outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of brain metastases with stereotactic radiosurgery (SRS) in combination with immune checkpoint inhibitors (ICI) has become more common in recent years with the emerging role of PD-1 inhibitors including pembrolizumab and nivolumab and the anti-CTLA-4 blocking antibody ipilimumab. Preclinical evidence and retrospective studies have suggested that combination of nonredundant mechanisms through concurrent administration may optimize the immune response against the tumor [1,2,3,4,5,6,7]. There is a lack of prospective data on cancer control outcomes when these therapies are administered concurrently. To investigate the outcome of combined SRS and ICI treatment, a retrospective analysis was performed comparing outcomes between radiated lesions of lung cancer and melanoma patients that received this therapy combination to those that received SRS alone or non-concurrent ICI during the same time period.
Methods and materials
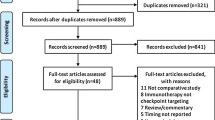
We retrospectively reviewed the data from patients with non-small cell lung cancer (NSCLC) and melanoma brain metastases treated at our institution from May 2008 to January 2017 with SRS delivered in 1 fraction with or without ICI. Local failure was defined as increase in size of the treated lesion. Local control was determined from the date of SRS to the date of local failure for lesions that failed locally, with lesions that did not fail locally censored at the patient’s date of last disease evaluation. Distant in-brain failure was defined as the appearance of new brain metastases. Distant brain control was calculated similarly using the date of distant in-brain failure for lesions that failed distantly. Local control and distant in-brain control were calculated for each treated lesion. Overall survival (OS) was calculated from date of initial SRS to date of death from any cause. Patients remaining alive were censored at their last known alive date. The Kaplan–Meier method was used to estimate median OS.
A parametric proportional hazard model was used to evaluate the association between treatments and local control and distant in-brain control, with the baseline hazard modeled by the Weibull distribution. A frailty term was added to take intrapatient correlations into account when modeling multiple lesions per patient. Other covariates considered for the model included primary tumor histology, lesion location, number of lesions, lesion diameter, presence of extracranial metastases, ICI receipt relative to SRS, prior treatment to lesion, time between whole brain radiation (WBRT) and SRS, type of SRS, and prescription dose. ICI receipt was categorized according to the relative timing of the therapies: SRS within 30 days of ICI administration, SRS between 31 and 60 days of ICI, and SRS between 61 and 90 days of ICI, due to variation in definitions of concurrent therapy in the literature from 30 days to 5 biological half-lives [2, 8]. Variables that were significant at p < 0.10 in the univariate analysis were included in the final multivariate model. Lesions without imaging follow-up were excluded from modeling. Analyses were repeated excluding patients who received prior whole-brain radiation therapy. P-value < 0.05 was considered statistically significant. SAS version 9.4 (SAS Institute, Cary, NC) was used for all analyses.
Results
The baseline characteristics for 144 patients with 477 total lesions treated are summarized in Tables 1 and 2, respectively. There were 95 NSCLC patients (66.0%), and 49 (34.0%) of patients had melanoma. Median age at brain metastases diagnosis was 60.1 years with a range of 30.1–84.9 years. Seventy-five (52.1%) of patients were male, and 69 (47.9%) were female. A median of 2 brain metastases were treated per patient with a range of 1–16 brain metastases. Thirty-eight patients received ICI (26.4%). Twenty-six patients received prior brain surgery (18.1%), while 42 patients received WBRT before SRS (29.2%). Median tumor diameter was 0.7 cm (range 0.1–3.5 cm). A majority of lesions were treated with Gamma Knife (GK) (364 lesions, 76.3%) compared to linear accelerator (LINAC) (113 lesions, 23.7%). Median prescription dose was 22 Gy (range 11–30 Gy). The median imaging follow-up from the initial SRS was 9.9 months (range 0–116 months). The majority of the lesions were not associated with any toxicity after treatment (450/477 lesions, 94.3%), but 18 lesions (3.8%) had radiation necrosis, and 9 lesions (1.9%) had hemorrhage.
Fifteen patients had at least one lesion with concurrent ICI (within 30 days of SRS). No patients with concurrent ICI had local failure. Univariate and multivariate analyses for local failure are shown in Table 3. On multivariate analysis for local failure, concurrent ICI was not associated with improved control when concurrent was defined as SRS within 30 days of ICI. The multivariate model for local failure included SRS concurrent with ICI (within 90 days of ICI) vs. non-concurrent or no ICI received (HR 0.55; 95% CI 0.10–2.94, primary tumor histology of NSCLC vs. melanoma (HR 3.06; 95% CI 0.78–11.92), prior treatment to lesion (HR 0.82 for WBRT vs. none and HR 0.63 for surgery vs. none), number of lesions (HR 0.90; 95% CI 0.68–1.19), SRS with LINAC vs. GK (HR 4.40; 95% CI 1.43–13.59), prescription dose (HR 0.77; 95% CI 0.61–0.98), and lesion diameter (HR 1.66; 95% CI 0.89–3.09) with only type of SRS and prescription dose being significantly associated with local failure.
Univariate and multivariate analyses for distant brain failure are shown in Table 4. On multivariate analysis for distant brain failure, concurrent ICI was associated with improved control when concurrent was defined as SRS within 30 days of ICI. The multivariate model for distant brain failure included SRS concurrent with ICI (within 30 days of ICI) vs. non-concurrent or no ICI received (HR 0.15; 95% CI 0.05–0.47), prior treatment to lesion (WBRT vs. none HR 1.72, 95% CI 0.75–3.92; Surgery vs. none HR 0.64, 95% CI 0.21–1.91; Surgery and/or WBRT vs. none HR 6.81, 95% CI 2.37–19.54), number of lesions (HR 1.28; 95% CI 1.13–1.45) and presence of extracranial metastases (HR 11.33; 95% CI 4.90–26.21).
Six patients (19 brain lesions) with concurrent ICI (administered within 30 days of SRS) experienced distant in-brain failure. Among the 19 lesions, 11 were treated with ICI prior to SRS, while eight of the lesions were treated with ICI after SRS. Among the 19 lesions, 10 had systemic failure at the time of distant brain failure, while nine did not have systemic failure at the time of distant brain failure. For those that did not experience distant in-brain failure, nine lesions were treated within 30 days prior to ICI administration and 25 lesions were treated with ICI within 30 days after SRS. Of the lesions that were treated with non-concurrent or no ICI, 82 lesions (36.6%) had systemic failure at the time of brain failure, and 142 lesions (63.4%) did not have systemic failure at the time of brain failure.
Kaplan–Meier curve for OS is shown in Fig. 1. Curves for distant in-brain failure are shown in Figs. 2 and 3 (by concurrent ICI vs. non-concurrent or no ICI). The curves are relative to each patient’s first treated brain metastasis and patients who had WBRT were excluded. These results suggest that patients that received concurrent ICI had increased time to distant brain failure compared to patients that received non-concurrent ICI or no ICI.
Sensitivity analysis performed excluding patients that received prior whole-brain radiation therapy revealed similar results (see supplementary data).
Conclusions
In our retrospective analysis, concurrent SRS and ICI (defined as SRS within 30 days of ICI administration) in NSCLC and melanoma patients was not associated with local control but was associated with distant brain control. When controlling for prior treatment to lesion, number of lesions, and presence of extracranial metastases, patients receiving this therapy combination had decreased risk of distant brain failure compared to patients that received non-concurrent ICI or no ICI (HR 0.15; 95% CI 0.05–0.47, p = 0.0011). Results are consistent with evidence that concurrent ICI may enhance the efficacy of radiation treatment.
A potential benefit to the combination of ICI with SRS is the possibility for enhanced antigen presentation and immunological priming. Nivolumab can penetrate the cerebrospinal fluid allowing for potential intracranial antigen response and ICI may otherwise affect the central nervous system through peripherally activated T cells crossing the blood–brain barrier [9, 10]. These mechanisms may explain the effect on distant brain control.
Although combination radiosurgery and ICI have increasingly been used, no prospective studies have reported data on efficacy of this therapy combination. Prior retrospective studies have mixed conclusions about the efficacy of this therapy combination. A retrospective matched cohort study of patients who had undergone SRS for one or more NSCLC-derived brain metastases comparing patients that received ICI before or after SRS within a 3 month period (concurrent ICI, 17 patients with 45 brain metastases) to those that did not (ICI naïve, 34 patients with 92 metastases) showed no significant difference in local control, OS, or progression free survival. Additionally, concurrent ICI did not prevent the development of out-of-field brain metastases, defined as new brain metastases or leptomeningeal disease, with 12 month CNS distant control rate of 47.5% for the concurrent-ICI group versus 66.5% for the ICI-naive cohort (p = 0.061) [5]. A retrospective analysis of metastatic non-small cell lung cancer, melanoma, and renal cell carcinoma patients who had brain metastases treated with SRS without WBRT with concurrent ICI defined as ICI given within 2 weeks of SRS showed that concurrent ICI (79/260 patients) predicted for decreased likelihood of the development of ≥ 3 new brain metastases compared to those that received SRS alone (181/260 patients) (p = 0.045; odds ratio 0.337) [4]. A retrospective analysis of consecutive patients with lung cancer or melanoma treated with SRS for brain metastases found that ICI (administered in 101/271 patients) was associated with improved OS compared to no ICI (OS 15.9 months vs. 6.1 months, p < 0.01) and decreased likelihood of neurologic death [11].
Interpretation of results of single institution studies is limited by variation in definitions of concurrent ICI and variation in patient populations. A systematic review and meta-analysis that evaluated the effect of concurrent ICI and SRS (within 1 month) vs. nonconcurrent ICI identified 8 retrospective studies and demonstrated that concurrent ICI with SRS was associated with a 12 month overall survival benefit (OR 1.74; p = 0.011), while local and distant progression free survival were both comparable between the groups [12]. A meta-analysis of 17 retrospective studies that included 534 patients with 1570 brain metastases (most frequently from melanoma and NSCLC) that received ICI concurrent (within 1 month) vs. noncurrent with SRS found that 1 year OS, 1 year local control, and 1 year regional brain control were significantly better for concurrent SRS and ICI [8].
This study represents a large single-institution analysis, however there was heterogeneity within the patient population as the study included patients that underwent surgical resection and prior WBRT and patients that received a variety of ICI agents. Additionally, the patients in this analysis were not compared to patients that received ICI alone, thus it is unclear if the improvement in distant brain failure is an additive effect of ICI on SRS or synergistic. Multiple intervals between SRS and ICI were analyzed, with the final multivariate model for distant brain failure including a 30 day interval. Future studies might benefit from considering the interval between SRS and ICI as an important variable. Prospective studies would allow for stronger evidence to support the impact of concurrent SRS and ICI on disease outcomes.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Twyman-Saint Victor C, Rech AJ, Maity A et al (2015) Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 520(7547):373–377. https://doi.org/10.1038/nature14292
Kotecha R, Kim JM, Miller JA et al (2019) The impact of sequencing PD-1/PD-L1 inhibitors and stereotactic radiosurgery for patients with brain metastasis. Neuro Oncol 21(8):1060–1068. https://doi.org/10.1093/neuonc/noz046
Schapira E, Hubbeling H, Yeap BY et al (2018) Improved overall survival and locoregional disease control with concurrent PD-1 pathway inhibitors and stereotactic radiosurgery for lung cancer patients with brain metastases. Int J Radiat Oncol Biol Phys 101(3):624–629. https://doi.org/10.1016/j.ijrobp.2018.02.175
Chen L, Douglass J, Kleinberg L et al (2018) Concurrent immune checkpoint inhibitors and stereotactic radiosurgery for brain metastases in non-small cell lung cancer, melanoma, and renal cell carcinoma. Int J Radiat Oncol Biol Phys 100(4):916–925. https://doi.org/10.1016/j.ijrobp.2017.11.041
Shepard MJ, Xu Z, Donahue J, Eluvathingal Muttikkal TJ, Cordeiro D, Hansen L, Mohammed N, Gentzler RD, Larner J, Fadul CE et al (2019) Stereotactic radiosurgery with and without checkpoint inhibition for patients with metastatic non-small cell lung cancer to the brain: a matched cohort study. J Neurosurg 26:1–8. https://doi.org/10.3171/2019.4.JNS19822
Singh C, Qian JM, Yu JB, Chiang VL (2019) Local tumor response and survival outcomes after combined stereotactic radiosurgery and immunotherapy in non-small cell lung cancer with brain metastases. J Neurosurg 132(2):512–517. https://doi.org/10.3171/2018.10.JNS181371
Kowalski ES, Remick JS, Sun K, Alexander GS, Khairnar R, Morse E, Cherng HR, Berg LJ, Poirier Y, Lamichhane N, Becker S, Chen S, Molitoris JK, Kwok Y, Regine WF, Mishra MV (2020) Immune checkpoint inhibition in patients treated with stereotactic radiation for brain metastases. Radiat Oncol 15(1):245. https://doi.org/10.1186/s13014-020-01644-x
Lehrer EJ, Peterson J, Brown PD, Sheehan JP, Quiñones-Hinojosa A, Zaorsky NG, Trifiletti DM (2019) Treatment of brain metastases with stereotactic radiosurgery and immune checkpoint inhibitors: an international meta-analysis of individual patient data. Radiother Oncol 130:104–112. https://doi.org/10.1016/j.radonc.2018.08.025
van Bussel MTJ, Beijnen JH, Brandsma D (2019) Intracranial antitumor responses of nivolumab and ipilimumab: a pharmacodynamic and pharmacokinetic perspective—a scoping systematic review. BMC Cancer 19(1):519. https://doi.org/10.1186/s12885-019-5741-y
Kamath SD, Kumthekar PU (2018) Immune checkpoint inhibitors for the treatment of central nervous system (CNS) metastatic disease. Front Oncol 8:414. https://doi.org/10.3389/fonc.2018.00414
Lanier CM, Hughes R, Ahmed T, LeCompte M, Masters AH, Petty WJ, Ruiz J, Triozzi P, Su J, O’Neill S, Watabe K, Cramer CK, Laxton AW, Tatter SB, Wang G, Whitlow C, Chan MD (2019) Immunotherapy is associated with improved survival and decreased neurologic death after SRS for brain metastases from lung and melanoma primaries. Neurooncol Pract 6(5):402–409. https://doi.org/10.1093/nop/npz004
Lu VM, Goyal A, Rovin RA, Lee A, McDonald KL (2019) Concurrent versus non-concurrent immune checkpoint inhibition with stereotactic radiosurgery for metastatic brain disease: a systematic review and meta-analysis. J Neurooncol 141(1):1–12. https://doi.org/10.1007/s11060-018-03020-y
Funding
The authors declare that no funds, Grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Data collection was performed by AL and HM.TL and JM were involved in initial study conception and design, but all authors contributed. HB and YZ assisted with statistical analysis and interpretation.The first draft of the manuscript was written by A L and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Le, A., Mohammadi, H., Mohammed, T. et al. Local and distant brain control in melanoma and NSCLC brain metastases with concurrent radiosurgery and immune checkpoint inhibition. J Neurooncol 158, 481–488 (2022). https://doi.org/10.1007/s11060-022-04038-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04038-z