Abstract
Purpose
Upfront dual checkpoint blockade with immune checkpoint inhibitors (ICI) has demonstrated efficacy for treating melanoma brain metastases (MBM) in asymptomatic patients. Whether the combination of stereotactic radiosurgery (SRS) with dual checkpoint blockade improves outcomes over dual-checkpoint blockade alone is unknown. We evaluated clinical outcomes of patients with MBM receiving ICI with nivolumab and ipilimumab, with and without SRS.
Methods
49 patients with 158 MBM receiving nivolumab and ipilimumab for untreated MBM between 2015 and 2022 were identified at our institution. Patient and tumor characteristics including age, Karnofsky Performance Status (KPS), presence of symptoms, cancer history, MBM burden, and therapy course were recorded. Outcomes measured from initiation of MBM-directed therapy included overall survival (OS), local control (LC), and distant intracranial control (DIC). Time-to-event analysis was conducted with the Kaplan–Meier method.
Results
25 patients with 74 MBM received ICI alone, and 24 patients with 84 MBM received concurrent SRS. Median follow-up was 24 months. No differences in age (p = 0.96), KPS (p = 0.85), presence of symptoms (p = 0.79), prior MBM (p = 0.68), prior MBM-directed surgery (p = 0.96) or SRS (p = 0.68), MBM size (p = 0.67), or MBM number (p = 0.94) were seen. There was a higher rate of nivolumab and ipilimumab course completion in the SRS group (54% vs. 24%; p = 0.029). The SRS group received prior immunotherapy more often than the ICI alone group (54% vs. 8.0%; p < 0.001). There was no significant difference in 1-year OS (72% vs. 71%, p = 0.20) and DIC (63% v 51%, p = 0.26) between groups. The SRS group had higher 1-year LC (92% vs. 64%; p = 0.002). On multivariate analysis, LC was improved with combination therapy (AHR 0.38, p = 0.01).
Conclusion
In our analysis, patients who received SRS with nivolumab and ipilimumab had superior LC without increased risk of toxicity or compromised immunotherapy treatment completion despite the SRS cohort having higher rates of prior immunotherapy. Further prospective study of combination nivolumab and ipilimumab with SRS is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Melanoma is the fifth most common cancer diagnosis in the United States excluding nonmelanoma skin cancers [1]. An estimated 97,610 Americans will be newly diagnosed with melanoma and 7990 will pass due to melanoma in 2023 [2]. Up to 40–50% of patients with advanced disease will develop melanoma brain metastases (MBMs) which are highly associated with increased morbidity and mortality [3]. Historically, stereotactic radiosurgery (SRS) and neurosurgical resection were the cornerstone of MBM management, offering local control, symptom relief, and survival benefit, though their effectiveness was mostly limited to oligometastatic disease [4]. Whole brain radiotherapy (WBRT) and traditional chemotherapy drugs remained options but were ultimately less therapeutic due to high toxicity and poor CNS penetrance [5,6,7]. Therefore, strategies to prevent the development of new MBM were few and prognosis remained grim, ranging on average from 4 to 13 months with very few patients surviving over 5 years [3, 8,9,10].
Improvements in imaging techniques, neurosurgical, and radiotherapeutic techniques have steadily increased survival for patients with MBM over the years. Concurrently, development of contemporary systemic therapies has revolutionized MBM treatment. Single agent immune checkpoint inhibitors (ICI), such as ipilimumab (anti CTLA-4) or pembrolizumab (anti PD-1), and BRAF/MEK inhibitors have demonstrated durable intracranial activity in clinical trials [11,12,13]. Double agent immunotherapies have been shown to yield even greater response, extending progression-free survival and overall survival more than single agent or targeted therapies [14]. Recently, Checkmate-204, a phase II clinical trial, has suggested viability of first-line ipilimumab and nivolumab for active asymptomatic MBM, deferring local therapies until event of progression [15].
Current treatment strategies for MBM management often involve surgery, radiation, and systemic therapy either sequentially or concurrently at the discretion of multidisciplinary review or tumor boards. However, clinical practice guidelines regarding radiation are inconsistent and based on low-level evidence or consensus opinion [16]. Furthermore, no prospective clinical trials combining ICI with SRS/surgery for MBM have been completed [17]. Questions remain unanswered regarding outcomes, optimal timing, sequencing of therapy, and potential toxicities of combined approaches. Thus, we conducted a single-institution retrospective study comparing clinical outcomes of active MBM treated with ipilimumab and nivolumab only, versus ipilimumab and nivolumab with SRS.
Materials and methods
We identified 49 patients with untreated-MBM who received nivolumab and ipilimumab from August 2015 to October 2022, from a prospectively maintained database of patients receiving nivolumab and ipilimumab. Of those patients, 24 received additional SRS as part of their original treatment plan within 6 weeks of ICI, including single-fraction SRS and fractionated stereotactic radiation (FSRT), delivered to intact brain metastases. Decision on whether to treat with SRS or nivolumab and ipilimumab alone was left up to the multi-disciplinary team. Patients were stratified into 2 groups by intended therapy: ICI alone, or ICI with SRS. The study was approved by the Moffitt Cancer Center Institutional Review Board (Protocol No: 21960).
Systemic therapy
Patients received nivolumab 1 mg/kg and ipilimumab 3 mg/kg intravenously once every 3 weeks over 12 weeks (total 4 doses), followed by nivolumab 3 mg/kg intravenously every 2 weeks over 24 months or until progression or unacceptable toxicity.
Stereotactic radiation technique
Magnetic resonance imaging (MRI, Siemens Sonata, Siemens Medical Systems, Erlangen, Germany) with 1 mm slices was completed prior to the delivery of radiation for treatment planning purposes. The MRI was co-registered and fused with computed tomography (CT) simulation imaging (General Electric Medical System, Milwaukee, WI). Patient immobilization was achieved by using a head mask fixation system (BrainlabAG, Feldkirchen, Germany).
The gross tumor volume (GTV) was expanded uniformly by 1–2 mm to create the planning target volume (PTV). Doses were prescribed to ensure that the prescription dose covered at least 95% of the PTV. Treatments were delivered using multiple dynamic conformal arcs or intensity modulated radiotherapy (IMRT). Image guidance was provided with the BrainLab ExacTrac positioning system.
Follow-Up
Each patient was followed with physical examination with full neurologic assessment and MRI of the brain at 2–3 month intervals with the treating radiation oncologist, neurosurgeon, and/or medical oncologist. Local brain metastasis failure was defined by RANO-BM criteria in which there was a ≥ 20% increase that remained consistent or demonstrated continued progression on subsequent imaging, while local brain metastasis control (LC) included all treated lesions not meeting these criteria [18]. Distant intracranial failure was defined as the development of new brain metastasis or leptomeningeal disease (LMD) outside the previously treated field. Cases were deemed radionecrosis (RN) either after pathological confirmation or following a multidisciplinary review including neuroradiology, radiation oncology, and neurosurgery. Patient and tumor characteristics and outcomes including age, gender, Karnofsky Performance Status (KPS), presence of symptoms, cancer history, MBM burden, toleration of therapy, and salvage therapy were recorded via retrospective chart review.
Statistical analysis
Patient, tumor, and treatment characteristics were compared between the 2 groups via the Wilcoxon signed rank test and Chi-square test as appropriate. The Kaplan–Meier (KM) method was used to calculate overall survival (OS), local control (LC), and distant intracranial control (DIC) from start date of therapy, with log-rank testing used to assess differences between groups. The Cox proportional hazards model was used for univariable analysis (UVA) and multivariable analysis (MVA). Only variables found to be statistically significant (p < 0.05) upon UVA were included for multivariable analysis (MVA). Statistical analyses were performed using JMP 13 (SAS Institute Inc, Cary, NC, USA).
Results
Patient and treatment characteristics
A total of 49 patients with 158 untreated MBM received nivolumab and ipilimumab (Table 1). 25 patients with 74 MBM received ICI only, while 24 patients with 84 MBM received ICI and SRS. The median interval between SRS/FSRT and ICI was 8 days (range: 1–41 days). Eighteen patients received SRS or FSRT prior to ICI, while 6 patients received ICI prior to SRS or FSRT. The two groups were balanced in terms of gender (p = 0.40), age (p = 0.96), KPS (p = 0.85), active extracranial disease (p = 0.48), presence of symptoms (p = 0.79), current MBM size (p = 0.67), and number of active MBM (p = 0.94). Both groups also had similar rates of prior MBM (p = 0.68), prior MBM-directed surgery (p = 0.96), and prior MBM-directed SRS (p = 0.68). The SRS group more often received prior immunotherapy compared to the nivolumab and ipilimumab only group (54% vs. 8%, p < 0.001).
Toxicity
In the entire cohort, 43% of patients experienced grade 3 acute toxicity, and 4% experienced grade 4 acute toxicity (Supplemental Table 1). The most common toxicities experienced included rash, fatigue, headache, hypothyroidism, colitis, and elevated transaminases. The SRS group completed the current course of nivolumab and ipilimumab more often (54% vs. 24%, p = 0.029, Table 1) and less commonly experienced toxicity requiring discontinuation of the ipilimumab and nivolumab (12.0% vs. 48.0%, p = 0.022). The majority of patients who discontinued ipilimumab and nivolumab completed either 1 cycle (39%) or 2 cycles (42%). The SRS group had a lower rate of grade 3 + acute toxicity, though this did not reach statistical significance (33.3% vs. 52.0%, p = 0.185). The SRS group experienced more intracranial acute grade 1–2 (37.5% vs. 4.0%, p = 0.002) and grade 3 (12.5% vs. 0%, p = 0.034) toxicities, though there were no cases of acute grade 4 intracranial toxicity (Table 2).
Of the 84 MBM treated with SRS/FSRT, there were 5 cases (6.0%) of symptomatic radiation necrosis (RN). The 1- and 2-year rates of symptomatic RN were 1.6 and 1.6%, respectively.
Clinical outcomes
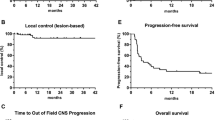
The median follow-up by reverse KM was 24.0 months (range 0.7–96.2 months). For the entire cohort, the 1-year OS (Fig. 1a), DIC (Fig. 1b), and LC (Fig. 1c) were 71.2, 57.1, and 77.8%, respectively. There was no significant difference in OS (1-year OS 71.8% vs. 70.8%, p = 0.2, Fig. 2a) or DIC (1-year DIC 63.0% vs. 50.7%, p = 0.26, Fig. 2b) between groups. The SRS group had superior LC (1-year LC 92.1% vs. 63.9%, p = 0.002, Fig. 2c).
On UVA, only KPS (p = 0.027) and the receipt of ICI with SRS significantly predicted improved LC compared to ICI only (p = 0.004; HR 0.34, Table 3). Upon MVA, only receipt of ICI with SRS remained significant ((adjusted hazard ratio (AHR) 0.38, 95% CI 0.18–0.79, p = 0.01)). There were no significant predictors for OS or DIC upon UVA.
Discussion
To our knowledge, this retrospective, single-institution study is the first series to date comparing outcomes in active and untreated MBM managed with upfront nivolumab and ipilimumab alone or with SRS. Our analysis suggests the following: (i) combination therapy with SRS and nivolumab with ipilimumab was well tolerated with no increased toxicity over nivolumab and ipilimumab alone to compromise systemic therapy course completion, and (ii) inclusion of SRS was associated with improved LC.
Current joint ASCO-SNO-ASTRO guidelines recommend upfront ipilimumab and nivolumab for asymptomatic MBM, reserving local therapy for progression [19]. Data supporting this guideline primarily stems from several clinical trials. Margolin et al. investigated asymptomatic and symptomatic MBM treated with ipilimumab (NCT00623766) in an open label trial, and found disease control rates of 24 and 10%, respectively [12]. Long et al. conducted the only randomized phase 2 clinical trial (NCT02374242), comparing efficacy and safety of nivolumab versus ipilimumab and nivolumab for MBM showed 46% response rate in MBM treated with dual-agent versus 20% in single-agent therapy [20]. Checkmate204 (NCT02320058), also an open-label trial studying nivolumab and ipilimumab in asymptomatic MBM reported an intracranial response rate of 55% with a 6-month progression free survival of 64% [21]. No clinical trial has been conducted comparing ipilimumab and nivolumab versus ipilimumab and nivolumab with SRS in active, untreated MBM head-to-head.
Notably, our study found no decreased course completion or increased toxicity with combination SRS and immunotherapy. This was noted in the context of the SRS group having been exposed to more lines of prior immunotherapy. Moreover, there was an increased rate of early systemic therapy discontinuation in the ipilimumab and nivolumab alone arm; however, this was related to increased systemic toxicity. Commonly reported neurotoxicities in SRS include fatigue, headache, and radiation necrosis [22]. Our 6% symptomatic RN rate is comparable to the reported rates in SRS (0–20%) and FSRT (1–8%) administered alone [23]. Patel et al. investigated outcomes of MBM treated with SRS and ipilimumab and versus SRS alone reported no difference in RN [24]. Ultimately, our results are consistent with the literature and indicate combination treatment of brain metastases with SRS and immunotherapy is well-tolerated, and the addition of SRS does not jeopardize completion of immunotherapy.
SRS was associated with LC in MBMs compared to those that only received nivolumab and ipilimumab, with 12-month LCs of 89.5 and 63.9%, respectively (Table 2, Fig. 2). Our results are consistent with those reported in literature, as SRS has been shown to provide 1-year LC rates to brain metastases of varying primary histologies ranging from 73 to 92% [25]. The previously referenced retrospective review published by Patel et al. comparing SRS with ipilimumab vs SRS alone reported similar 1-year LC rates of 92.3 and 71.4%, respectively with no significant difference between the two cohorts [24]. Kotecha et al. found a 1-year LC rate of 93% for patients with MBM treated with SRS and PD-1/CTLA-4 agents [26]. These rates also compare with our institutional results assessing LC in 1048 MBM across multiple different systemic therapies where LC ranged between 83 and 96% at 1 year between groups [27].
Limitations of this study include its retrospective nature without predefined endpoints, relatively small sample size, follow-up intervals, relatively small metastasis treated, and criteria for dosing of stereotactic radiation. Additionally, though our cohorts were balanced in terms of patient characteristics, symptoms, tumor burden, prior surgery, and prior radiation, our combination therapy cohort was more advanced in terms of systemic therapy, more often having prior immunotherapy. Despite its limitations, this study is one of the few investigating MBM treated with nivolumab and ipilimumab and SRS. These results require prospective validation, which may come from the currently enrolling phase II ABC-X Study, which randomizes patients with asymptomatic, untreated MBM to ipilimumab and nivolumab alone versus ipilimumab and nivolumab with stereotactic radiotherapy (NCT03340129).
In conclusion, patients with active and untreated MBM receiving nivolumab and ipilimumab may receive SRS without added toxicity or increased risk of treatment discontinuation. No differences in OS or DIC were noted; however, lesions treated with SRS had superior LC. Further prospective study of combination nivolumab and ipilimumab with SRS in MBM management is warranted to assess the potential synergy between combination therapies.
Data availability
Summary data supporting the results reported in this article can be requested by emailing the corresponding author.
References
Saginala K, Barsouk A, Aluru JS, Rawla P, Barsouk A (2021) Epidemiology of melanoma. Med Sci (Basel). https://doi.org/10.3390/medsci9040063
National Cancer Institute (2023) SEER Cancer Stat Facts: Melanoma of the Skin. Accessed July 24. https://seer.cancer.gov/statfacts/html/melan.html
Davies MA, Liu P, McIntyre S et al (2011) Prognostic factors for survival in melanoma patients with brain metastases. Cancer 117(8):1687–1696. https://doi.org/10.1002/cncr.25634
Sloan AE, Nock CJ, Einstein DB (2009) Diagnosis and treatment of melanoma brain metastasis: a literature review. Cancer Control 16(3):248–255. https://doi.org/10.1177/107327480901600307
Bates JE, Youn P, Usuki KY et al (2015) Brain metastasis from melanoma: the prognostic value of varying sites of extracranial disease. J Neurooncol 125(2):411–418. https://doi.org/10.1007/s11060-015-1932-9
Agarwala SS, Kirkwood JM, Gore M et al (2004) Temozolomide for the treatment of brain metastases associated with metastatic melanoma: a phase II study. J Clin Oncol 22(11):2101–2107. https://doi.org/10.1200/jco.2004.11.044
Tallet AV, Azria D, Barlesi F et al (2012) Neurocognitive function impairment after whole brain radiotherapy for brain metastases: actual assessment. Radiat Oncol 7(1):77. https://doi.org/10.1186/1748-717X-7-77
Lotze M, Dallal R, Kirkwood J, Flickinger J (2000) Cutaneous Melanoma En: Devita VT, Hellman S, Rosenberg SA, editors. Cancer Principles and Practice of Oncology. Philadelphia: Lippincott-Raven
Bander ED, Yuan M, Carnevale JA et al (2021) Melanoma brain metastasis presentation, treatment, and outcomes in the age of targeted and immunotherapies. Cancer 127(12):2062–2073. https://doi.org/10.1002/cncr.33459
Sampson JH, Carter JH Jr, Friedman AH, Seigler HF (1998) Demographics, prognosis, and therapy in 702 patients with brain metastases from malignant melanoma. J Neurosurg 88(1):11–20. https://doi.org/10.3171/jns.1998.88.1.0011
Davies MA, Saiag P, Robert C et al (2017) Dabrafenib plus trametinib in patients with BRAF(V600)-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol 18(7):863–873. https://doi.org/10.1016/s1470-2045(17)30429-1
Margolin K, Ernstoff MS, Hamid O et al (2012) Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol 13(5):459–465. https://doi.org/10.1016/s1470-2045(12)70090-6
Kluger HM, Chiang V, Mahajan A et al (2019) Long-term survival of patients with melanoma with active brain metastases treated with pembrolizumab on a phase II trial. J Clin Oncol 37(1):52–60. https://doi.org/10.1200/jco.18.00204
Rulli E, Legramandi L, Salvati L, Mandala M (2019) The impact of targeted therapies and immunotherapy in melanoma brain metastases: a systematic review and meta-analysis. Cancer 125(21):3776–3789. https://doi.org/10.1002/cncr.32375
Tawbi HA, Forsyth PA, Hodi FS et al (2021) Long-term outcomes of patients with active melanoma brain metastases treated with combination nivolumab plus ipilimumab (CheckMate 204): final results of an open-label, multicentre, phase 2 study. Lancet Oncol 22(12):1692–1704. https://doi.org/10.1016/s1470-2045(21)00545-3
Thompson JF, Williams GJ, Hong AM (2022) Radiation therapy for melanoma brain metastases: a systematic review. Radiol Oncol 56(3):267–284. https://doi.org/10.2478/raon-2022-0032
Galli G, Cavalieri S, Di Guardo L et al (2019) Combination of immunotherapy and brain radiotherapy in metastatic melanoma: a retrospective analysis. Oncol Res Treat 42(4):186–194. https://doi.org/10.1159/000497211
Lin NU, Lee EQ, Aoyama H et al (2015) Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol 16(6):e270–e278. https://doi.org/10.1016/s1470-2045(15)70057-4
Vogelbaum MA, Brown PD, Messersmith H et al (2021) Treatment for brain metastases: ASCO-SNO-ASTRO guideline. J Clin Oncol 40(5):492–516. https://doi.org/10.1200/JCO.21.02314
Long GV, Atkinson V, Lo S et al (2018) Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol 19(5):672–681. https://doi.org/10.1016/S1470-2045(18)30139-6
Tawbi HA, Forsyth PA, Algazi A et al (2018) Combined nivolumab and ipilimumab in melanoma metastatic to the brain. N Engl J Med 379(8):722–730. https://doi.org/10.1056/NEJMoa1805453
Clair WHS, Given CA (2003) Stereotactic radiosurgery associated neurotoxicity. Technol Cancer Res Treat 2(2):147–151. https://doi.org/10.1177/153303460300200211
Gondi V, Bauman G, Bradfield L et al (2022) Radiation therapy for brain metastases: an ASTRO clinical practice guideline. Pract Radiat Oncol 12(4):265–282. https://doi.org/10.1016/j.prro.2022.02.003
Patel KR, Shoukat S, Oliver DE et al (2017) Ipilimumab and stereotactic radiosurgery versus stereotactic radiosurgery alone for newly diagnosed melanoma brain metastases. Am J Clin Oncol 40(5):444–450. https://doi.org/10.1097/coc.0000000000000199
Soliman H, Das S, Larson DA, Sahgal A (2016) Stereotactic radiosurgery (SRS) in the modern management of patients with brain metastases. Oncotarget 7(11):12318–12330. https://doi.org/10.18632/oncotarget.7131
Kotecha R, Miller JA, Venur VA et al (2018) Melanoma brain metastasis: the impact of stereotactic radiosurgery, BRAF mutational status, and targeted and/or immune-based therapies on treatment outcome. J Neurosurg 129:50–59. https://doi.org/10.3171/2017.1.Jns162797
Dohm AE, Nakashima JY, Kalagotla H et al (2023) Stereotactic radiosurgery and anti-PD-1 + CTLA-4 therapy, anti-PD-1 therapy, anti-CTLA-4 therapy, BRAF/MEK inhibitors, BRAF inhibitors, or conventional chemotherapy for the management of melanoma brain metastases. Eur J Cancer. https://doi.org/10.1016/j.ejca.2023.113287
Acknowledgements
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by JT, MM, JN, AD, and KA. The first draft of the manuscript was written by JT, MM, and KA. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Joseph D. Tang: no disclosures. Matthew N. Mills: no disclosures.Justyn Nakashima: no disclosures.Ammoren E. Dohm: no disclosures.Nikhil I. Khushalani: personal consulting fees from Astra-Zeneca, Bristol Myers Squibb, Incyte, Iovance, Merck, Novartis, Nektar, Replimune, Regeneron, Jounce, Castle Biosciences, and Instill Bio; receives research funding from Bristol Myers Squibb, Merck, Novartis, Replimune, Celgene, Regeneron, HUYA Biopharmaceuticals, and GlaxoSmithKline; and has common stock holdings in Bellicum Pharmaceuticals, Amarin Corp, and Asensus Surgical. Peter A. Forsyth: has funding from Pfizer and Celgene and is on the advisory boards of Novocure, BTG, Inovio, AbbVie, Ziopharm, Tocagen, and Pfizer. Michael A. Vogelbaum: has indirect equity and royalty interests in Infuseon Therapeutics, Inc. and has received honoraria from Tocagen, Inc. and Celgene. Evan J. Wuthrick: has served on the advisory board and has received honoraria from Bayer, has received research funding from Bristol-Myers Squibb, and has intellectual property: cGMP as protector for chemotherapy and radiation. Hsiang-Hsuan Michael Yu: has received speaker’s honoraria from BrainLab and is on the advisory boards of Novocure and AbbVie. Daniel E. Oliver: no disclosures. James K.C. Liu: no disclosures. Kamran A. Ahmed: has received research funding from Bristol-Myers Squibb, Eli Lilly, and Genentech.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tang, J.D., Mills, M.N., Nakashima, J. et al. Clinical outcomes of melanoma brain metastases treated with nivolumab and ipilimumab alone versus nivolumab and ipilimumab with stereotactic radiosurgery. J Neurooncol 166, 431–440 (2024). https://doi.org/10.1007/s11060-023-04543-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04543-9