Abstract
Purpose
Foramen magnum meningiomas (FMMs) are a major surgical challenge, due to relevant surgical morbidity and mortality. The paper aims to review the clinical (symptomatic improvement, complication rate, length of hospital stay) and radiological outcome (completeness of resection) of microsurgical resection of FMMs, and to identify predictors of complications.
Methods
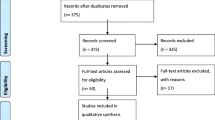
A multi-institutional retrospective review of prospectively maintained database of FMMs included 51 patients (74.5% females) with a median tumor volume of 8.18 cm3 (range, 1.77–57.9 cm3) and median follow-up of 36 months (range, 0.30–180.0 months). Tumors were resected though suboccipital approach (58.8%) or posterior-lateral approaches (39.3%), including far-lateral, extreme lateral and transcondylar approaches.
Results
Gross-total resection (GTR) was achieved in 80.4% and 98% of cases did not present tumor regrowth or recurrence. Clinical symptoms improved in 34 patients (66.7%) and worsened in 5 (9.8%). The median length of hospital stay was 5 days. Mortality was null. Postoperative complications developed in 15 patients (29.4%), with cerebrospinal fluid leak (7.8%) and lower cranial nerves deficits (7.8%) as the most frequent. Craniospinal location (p = 0.03), location anterior to the dentate ligament (DL) (p = 0.02), involvement of vertebral artery (VA) (p = 0.03) were significantly associated with complication rate. These three elements allow calculating the Foramen Magnum Meningioma Risk Score (FRMMRS), to estimate the risk of post-operative complications.
Conclusion
Microsurgical resection allows for high GTR rate and low rate of tumor regrowth or recurrence, despite complications in one third of the patients. The FMMRS allows classifying FMMs and estimating the risk of post-operative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Foramen magnum meningiomas (FMMs) are benign slow-growing tumors located at the craniocervical junction [1]. These lesions represent 0.3 to 3.2% of all meningiomas, 4.2 to 20% of all posterior fossa meningiomas, and 60 to 77% of all benign extramedullary tumors at the craniocervical junction [2, 3]. The optimal management of FMMs is still controversial due to the significant risk for surgical morbidity and mortality related to the presence of several critical neurovascular structures in a narrow space [4,5,6]. Several surgical approaches have been adopted for effective and safe resection of FMMs including, but not limited to: anterior transoral approach [5], endoscopic endonasal approach [6], lateral transcervical approach [7], suboccipital craniotomy [8], far-lateral approach [9,10,11], and extreme lateral approach [9]. The plethora of surgical approaches and variations accounts for the complexity of FMMs and for the difficulty in comparing different studies. The aim of the present study is to review the clinical and radiological outcome of FMMs treated surgically as well as to explore the prognostic value of pre- and peri-operative variables on the clinical and radiological outcome, including patient and tumor characteristics, and surgical approaches. Understanding these factors is of paramount importance in choosing the best course of treatment for these patients and for estimating the surgical risk.
Patients and methods
Patient population
Retrospective chart review of a prospectively maintained electronic database identified consecutive patients with FMMs treated surgically between 2000 and 2020. This multicentric study has been conducted at two academic tertiary care hospitals and was approved by hospitals’ Institutional Review Boards. Patient consent was not required because of the retrospective methodology without identifiable patient data. All the neurosurgeons (5) that operated the included cases are board-certified in neurosurgery, received advanced training in skull-base surgery and/or neuro-oncology in the USA and have an active practice in skull-base surgery at Stanford Hospital or Massachusetts General Hospital.
The study included all meningiomas arising from the foramen magnum treated surgically. The study excluded FMMs treated with radiation therapy alone, multiple meningiomas, radiation-induced tumors as well as patients with incomplete data on clinical outcome assessment.
Definitions
FMMs are tumors arising in a region limited by: anteriorly, the lower third of clivus to upper margin of the axis; laterally, the jugular tubercles and upper margin of C2-lamina; and posteriorly, the anterior edge of the squamous occipital bone to the C2-spinous process [10]. FMMs can be classified according to 3 radiological parameters: first, on the basis of craniocaudal extension, craniospinal (CS) FMMs are mainly intracranial tumors with a caudal extension through foramen magnum into the spinal canal, whereas, spinocranial (SC) FMMs are mainly intraspinal tumors with significant rostral extension into the cranial cavity [11]. Second, on the basis of their position relative to the dentate ligament (DL): anterior FMMs are ventral to the DL, while posterior FMMs as dorsal to the DL Third, on the basis of their involvement of the vertebral artery (VA), [10], FMMs can be classified as: not involving VA, or involving the VA (compressing or encasing the VA). The tumor volume was assessed on MRI (contrast-enhanced T1-sequence) by diameter-based measurement. This calculation was computed by measuring the largest tumor diameter in each orthogonal measurement plane. The craniocaudal diameter (dcc) along the long axis of the tumor was measured on the sagittal images; the anteroposterior diameter (dap) was measured on the sagittal images; and the largest lateral diameter (d1) was measured on the axial images. Diameter-based measurements were computed as ellipsoid (V = dcc*dap*d1*Π/6) to calculate the diameter-based volume (V).
Gross-total resection (GTR) was defined as resection without radiological evidence of residual enhancing tumor on contrast-enhanced T1-MRI [12].
Surgical approaches
All patients were operated by experienced neurosurgeons, under endotracheal general anesthesia, microscopic dissection, mild hypothermia and intraoperative neurophysiological neuromonitoring.
The suboccipital approach (SOA) [13] was used to resect tumors posterior to the DL as well as tumors anterior to the DL positioned laterally to the medulla. Tumors anterior to the DL and in anterior or anterolateral position with respect to the medulla were treated with transcondylar approach, far-lateral approach or extreme lateral approach, For statistical analysis, these three approaches are collectively named as “posterior-lateral approaches” (PLAs) to the posterior fossa.. Occasionally, both approaches were combined with cervical laminectomy (C1–C3), depending upon the entity of spinal tumor extension.
Clinical outcome and follow-up
Radiological follow-up with brain MRI was performed every 6-months for 1 year and then yearly, in order to determine the completeness of surgical resection, occurrence of complications or progression of the tumor. Furthermore, regular outpatient follow-up and telephone calls were made.
Statistical analysis
Demographic and clinical characteristics are summarized as counts and percentages for categorical characteristics and as median with interquartile range for continuous characteristics. Continuous variables (age, tumor volume) were tested as dichotomous variables based on their median and upper quartile values. Factors with p-value < 0.05 on univariate testing were placed into a Cox proportional hazards model. This multivariable regression analysis was performed to determine the effect of various pre- and peri-operative parameters on post-operative clinical outcome measures. Confidence intervals were calculated using the modified Wald Method. In FMM scoring system, the co-efficient of the significant variable were proportionally converted to the nearest integer. Moreover, the Hosmer–Lemeshow goodness-of-fit test was used to determine the calibration ability of our scoring system. The area under the receiver operating characteristic curve (AUC) was estimated for scoring system as well as the logistic regression model. All internal validations were performed using 1000 bootstrap samples to estimate the bias-corrected concordance index for describing the predictive accuracy of the model.
The outcomes were further categorized as clinical improvement rate, complications rate, length of hospital stay (< 8 days vs. ≥ 8 days), extent of tumor resection [GTR vs. subtotal resection (STR)], tumor regrowth or recurrence rate. IBM® SPSS® Statistics software v23.0 (Armonk, NY: IBM Corp.) was used to perform all analyses.
External validation
To validate the generalizability of our FMM scoring system, an additional 15 patients with FMMs who qualified for the study under inclusion and exclusion criteria were analyzed using the FMM scoring system. These patients underwent surgical management at another tertiary care hospital by authors J.H.S and W.T.C.
Results
Cohort’s clinical characteristics
The median age of 38 females (74.5%) and 13 males (25.5%) was 59.0 years (range, 20–77 years). All patients were affected with a single meningioma in the foramen magnum. The most frequent symptom at presentation was neck pain (n = 41, 80.4%), followed by headache (n = 39, 76.5%), hemiparesis (n = 30, 58.8%), ataxia (n = 25, 49.0%), imbalance (n = 24, 47.1%), nausea and vomiting (n = 22, 43.1%), paresthesia (n = 21, 41.2%), cranial nerve (CN) deficits (n = 14, 27.5%).
The median Karnofsky Performance Scale score (KPS) preoperatively was 70 (range, 50–80). Three patients (5.9%) were affected by a genetic syndrome, namely Neurofibromatosis type 2 (Table 1). The median follow-up of the study was 36 months (range, 0.30–180.0 months).
Tumor characteristics
The median tumor volume was 8.18 cm3 (range: 1.77–57.9 cm3). In terms of craniocaudal extension of the FMM, 34 tumors (66.7%) were CS, while 17 tumors (33.3%) were SC. Tumors were anterior to the DL in 37 patients (72.5%) or posterior to DL in 14 patients (27.5%). Meningiomas completely encased the VA in 7 cases (13.7%), contacted and/or displaced the VA in 20 patients (39.2%), while in 24 cases (47.1%) there was no contact with VA. Spinal cord and/or brainstem were compressed and displaced in 47 cases (92.2%). Histopathological diagnosis was consistent with WHO Grade 1 in 47 cases (92.2%), and WHO Grade 2 in 4 patients (7.8%). (Table 1).
Surgical aspects
Thirty patients (58.8%) underwent SOA, while 20 patients (39.3%) received a PLAs and 1 patient (1.9%) underwent cervical laminectomy (C1-3) alone. Specifically, 25 patients (49.0%) received SOA and laminectomy, while 13 patients (25.5%) received PLAs and laminectomy. GTR was achieved in 41 patients (80.4%) and STR in 10 patients (19.6%). Out of 10 patients with STR, 3 patients (5.8%) underwent postoperative stereotactic radiosurgery in 3–5 sessions, with a median dose of 14 Gy (range 11–18 Gy). Among the other patients with residual tumors, 6 patients (11.7%) received observation while 1 (1.9%) had additional surgery. In one case (1.9%), a gross-totally resected tumor (WHO grade 2) recurred after 18 months and was treated with surgery.
Clinical and radiological outcome
In 50 patients (98.0%) there was no tumor regrowth or recurrence. The median postoperative KPS was 90 (range: 30–100). The KPS improved in 42 patients (82.4%), remained stable in 5 patients (9.8%), and worsened in 4 patients (7.8%), postoperatively. Overall, the clinical symptoms improved in 34 patients (66.7%), remained stable in 12 patients (23.5%) and worsened in 5 patients (9.8%) (Table 2). Neck pain and headache improved in more than half of the patients (62.7% and 56.8%, respectively), while hemiparesis, ataxia and imbalance improved in more than one third of the patients (39.2%, 39.2%, 37.3%, respectively). The median length of stay in the hospital was 5 days (range: 3–70 days).
Overall, complications developed in 15 patients (29.4%), which included: cerebrospinal fluid (CSF) leak in 4 patients (7.8%), swallowing dysfunction due CN IX and X injury in 3 patients (5.9%), hydrocephalus in 3 patients (5.9%), imbalance and ataxia in 2 patients (3.9%), meningitis secondary to CSF leak in 2 patients (3.9%), aspiration pneumonia secondary to swallowing dysfunction in 1 patient (1.9%), quadriparesis due to post-surgical acute subdural hematoma in 1 patient (1.9%), CN VI palsy in 1 patient (1.9%), CN VII palsy in 1 patient (1.9%), CN VIII palsy in 1 patient (1.9%), and CN XI palsy in 1 patient (1.9%). Among these patients, only 5 patients (9.8%) developed permanent deficits including: 3 patients (5.9%) with swallowing dysfunction, 1 patient (1.9%) with quadriparesis, and 1 patient with CN VI palsy (1.9%). Among patients with dysphagia (5.9%) caused by CN IX and X deficits, 2 patients required feeding tube placement. One patient (1.9%) with quadriparesis underwent tracheostomy and PEG placement due to respiratory failure as a result of bulbar dysfunction.
Univariable and multivariable analysis
The results of univariable and of the multivariable testing of factors associated with clinical improvement, surgery-related complication, length of hospital stay, and completeness of resection are shown in Table 3.
Univariable analysis revealed that clinical improvement is statistically significantly negatively associated with older patient age (≥ 60 years) (p = 0.05), location anterior to DL (p = 0.05), SOA (p = 0.008), addition of laminectomy (p = 0.05). Conversely, clinical improvement is statistically significantly associated with lower histological grade (WHO 1) (p = 0.05), Multivariable analysis confirmed the statistically significant negative association for patient age ≥ 60-years (HR: 0.38, 95% CI 0.15–0.88, p = 0.04), location anterior to DL (HR: 0.11, 95% CI 0.02–0.65, p = 0.04), addition of laminectomy (HR: 0.27, 95% CI 0.10–0.68, p = 0.05). Clinical improvement is statistically significantly associated with lower histological grade (WHO 1) (HR: 2.80, 95% CI 1.21–20.7, p = 0.05).
Univariable analysis revealed that surgical complication rate is associated with CS location (p = 0.02), location anterior to DL (p = 0.01), VA involvement (p = 0.01) and GTR (p = 0.05). Multivariable analysis confirmed the statistically significant association of CS extension (HR: 3.83, 95% CI 1.54–38.6, p = 0.03), and location anterior to DL (HR: 5.74, 95% CI 1.97–31.1, p = 0.02), VA involvement (HR: 1.12, 95% CI 1.01–13.8, p = 0.03).
Univariable analysis revealed that length of hospital stay is statistically significantly associated with SOA (p = 0.01), as confirmed by multivariable analysis (HR: 1.26, 95% CI 1.09–7.89, p = 0.02).
Univariable analysis revealed that GTR is negatively associated with CS location (p = 0.02), location anterior to DL (p = 0.03), VA involvement (p = 0.03) and SOA (p = 0.02). Multivariable analysis confirmed the statistically significant negative association with CS location (HR: 0.71, 95% CI 0.23–0.95, p = 0.03), location anterior to DL (HR: 0.63, 95% CI 0.25–0.98, p = 0.03), involvement of VA (HR: 0.44, 95% CI 0.20–0.97, p = 0.04), and SOA (HR: 0.29, 95% CI 0.13–0.67, p = 0.004).
Classification scheme for foramen magnum meningioma
A novel classification scheme, Foramen Magnum Meningioma Risk Score (FMMRS), ranging from 2 to 9 points, was developed to estimate the risk of post-operative complications, on the basis of craniocaudal location, anteroposterior location, and VA involvement. (Table 4) Patients harboring FMM located in SC position, located posteriorly to the DL, without VA involvement (FMMRS = 2 point), have the lowest predicted risk of complications after surgery (0–4.76%) (Fig. 1). In our series, 3 patients (5.9%) belonged to this category and none of them had complications. Conversely, patients harboring FMM located in CS position, located anteriorly to the DL, with VA involvement (FMMRS = 9 points) have the highest predicted risk of complications after surgery (96.1–100%) (Fig. 1). In our series, 4 patients (7.8%) belonged to this category and all of them had complications.
Low-risk (FMMRS 1) (a–d) FMM. A 43-year old women with no previous family history of meningioma, presented with history of headaches and progressive gait difficulties. MRI revealed heterogenous contrast enhancing lesion measuring 2.1 cm × 1.5 cm × 1.1 cm at the foramen magnum with severe cervicomedullary contact, and no left VA encasement, as illustrated on the axial (a) and sagittal plane (b). The FMMRS score is 2, due to: spinocranial location (1 point), location posterior to the DL (1 point), no VA involvement (0 point). A sub-occipital approach with removal of posterior arch of C1 was adopted. Her postoperative course was regular. A 1-year follow-up MRI confirmed GTR with craniocervical decontact, as visualized on the axial (c) and sagittal plane (d). High-Risk (FMMRS 5) FMM (e–h). A 67-year old women with no previous family history of meningioma, presented with history of headaches, progressive unsteadiness, double vision to the leftward gaze, swallowing difficulty including choking on solids and left-sided drooling. MRI revealed contrast enhancing lesion centered at the lower third of the clivus measuring 3.1 cm × 2.9 cm × 3.1 cm, extending to the foramen magnum with severe cervicomedullary contact and partial left VA encasement (arrowhead), as illustrated on the axial (e) and sagittal plane (f). The FMMRS score is 9: craniospinal location (3 points), location anterior to the DL (5 point), VA involvement (1 point). A transcondylar approach with removal of posterior arch of C1 was adopted. Her postoperative course was complicated by a posterior fossa subdural and subarachnoid hematoma with left hemiparesis and hydrocephalus (requiring permanent shunting). A 2-year follow-up MRI revealed GTR with complete left VA (arrowhead) and craniocervical decompression, as visualized on axial (g) and sagittal plane (h)
The risk of surgical complications was estimated to be low (≤ 28.6%) when the total score was 2–4, intermediate (29.3–76.2%) when the total score was 5–7, and high (≥ 77.4%) when the total score was 8–9. The estimated risk and the observed values for each score were similar (R2 = 0.363, Homer–Lemeshow goodness-of-fit test, p = 0.898). The area under the receiving operating characteristic curve was 0.81 (95% CI 0.61–0.98). (Supplemental Fig. 1a).
To determine the generalizability of our FMMRS, external validation was performed using an additional data set of 15 patients. The observed values of complications at each score were comparable to the values estimated by the scoring system. The AUC of the scoring system was 0.86 (95% CI 0.65–0.97). (Supplemental Fig. 1b).
Discussion
Surgical approaches and radiological outcome
The goal of surgery for FMM is to achieve the maximal resection, while minimizing the morbidity (“maximal safe resection”), due to injury of critical neurovascular structures nearby. Over the past years, several approaches were advocated for the resection of these tumors [5,6,7,8,9, 14, 15], depending on their location on the axial plane, with respect to the medulla. Two main approaches can be identified. First, the SOA is ideal for the resection of FMM posterior to the DL and of small FMMs anterior to the DL and lateral to the medulla [10]. Posterior FMMs accounts only for 27.5% in our series, and for 2.5–28.5% in other series.[16, 17]. The posterior-lateral approaches (PLAs) to the posterior fossa include the far-lateral approach[14, 15, 18], the extreme-lateral approach,[9], and the transcondylar approach [19]This approach is ideal for tumors located anteriorly to the DL, in anterior or anterolateral position with respect to the medulla. Tumors anterior to the DL are the majority in our series (72.5%) as well as in previous series (12.5–100%). [1, 16, 17, 20] Various degrees of partial condylar drilling (less than 40%) allows for maximizing the visualization of the pre-medullary space, while minimizing the manipulation of the brainstem and the risk for atlantoaxial instability [21]. In our series, no cases of atlantoaxial instability were reported. Multivariable analysis shows that SOA carries lower chances of complete tumor resection (GTR) with respect to PLAs (HR: 0.29; 95% CI 0.15–0.67; p = 0.004), while the risk for complications and for clinical improvement were not significantly different. These data confirm that PLAs plays a pivotal role in complete excision of FMM, especially with a pre-medullary component, as it provides excellent exposure of the lateral aspect and anterior aspect of the brainstem and upper cervical spinal cord. [22] The addition of cervical laminectomy to the surgical approach is associated with a lower chance of clinical improvement (HR: 0.27; 95% CI 0.1–0.68; p = 0.05) and a higher, yet not statistically significant, risk of complications. Arguably, FMMs requiring cervical laminectomy could expose brainstem, lower CN and VA to a higher risk of injury during manipulation of the upper cervical spinal cord [23].
In selected cases of small FMMs anterior to the medulla without VA involvement, the transoral approach [5] and, more recently, the endoscopic endonasal approach [6] were found to be valuable alternatives to the PLAs. However, anterior approaches to FMMs are rarely performed because of the relevant risk for incomplete dural repair, CSF leak and meningitis. [5, 24,25,26] In our series, GTR was achieved in 80.4% of the cases, while STR in 19.6%. Multivariable analysis shows that the most technically challenging tumors to resect, namely CS tumors, tumors anterior to DL and tumors involving VA are statistically significantly negatively associated with GTR. Importantly, the VA involvement negatively correlates with the completeness of resection in multivariate analysis (HR: 0.44, 95% CI 0.2–0.97, p = 0.04). In these cases, a conservative approach was adopted to prevent VA injuries. When STR is achieved, the residual tumor was further treated with SRS in 5.8%, surgery in 1.9%, while in the remaining 11.7% no further treatment was required. At the end of follow-up, the absence of tumor regrowth or recurrence was 98%. In one case (1.9%), a gross-totally resected tumor (WHO grade 2) recurred after 18 months. Although our study has a short median follow-up, our data about tumor regrowth or recurrence are consistent with previous studies. [10, 27]Although GTR is certainly the most desirable goal, surgical aggressiveness should be tempered in cases with significant risk for surgical morbidity, considering the extremely low risk of recurrence of FMMs, and that, if needed, any residual can be safely treated with SRS. [28] Accordingly, GTR carries a borderline higher risk of complications (HR: 2.13; 95% CI 1.43–15.9; p = 0.06) and a non-statistically significant longer hospital stay than STR.
Clinical outcome and risk of complications
After surgery, symptoms improved or remained stable in 90.2%, while worsened in 9.8%. Complications occurred in 29.4% of the patients, mainly due to: first, incomplete dural repair, which include CSF leak, pseudomeningocele and meningitis and, second, CN deficits including CN VI, VII, VIII, IX, X, XI and associated complications like aspiration pneumonia due to swallowing dysfunction. Our results are consistent with previous series, reporting clinical improvement in 70–100%, stability in 2.5–20% and worsening in 7.5–10% [1, 13, 17]. Surgical morbidity was reported around 40%, with incomplete dural repair and lower CN deficits as the most frequent complications [27, 29,30,31]. Although in our series the mortality rate is null, that has been estimated to range between 0 and 25% [10].
Several predictors of complications were identified in the literature, such as: anterior tumor location [32, 33], tumor size [10], tumor invasiveness [10], extradural extension [32], VA encasement [8], absence of arachnoidal sheath [17], and adherence to the surrounding structures in recurrent lesions. [17] Our analysis revealed that 3 factors are strongly associated with the risk of complications both in univariate and multivariate analysis, namely CS location, anterior location and VA involvement. Arguably, CS location and anterior location could require longer and more complex surgical exposure with higher risk of injury to the anterior surface of the brainstem, to the CN and to the VA. In a similar fashion, VA involvement with displacement and/or encasement requires careful microsurgical dissection with potential morbidity. In the present series there were not any VA injuries. Although the size of the present cohort does not allow any further dichotomization on the basis of the complication type, 3/5 of the lower CN complications occurred in tumors encasing the VA and therefore requiring extensive microsurgical dissection. Moreover, the VA was involved in 3/4 cases of CSF leak. This is typically due to the complex dural reconstruction after dissection to mobilize the VA at the level of its dural entry and intradural course.
In the present series, CSF complications (leak/hydrocephalus) were the most frequent and were included in our risk analysis and predictive score. When the radiological characteristics of FMMs with CSF complications are compared with the characteristics of the entire cohort, the tumors were more frequently in CS position (85.7% vs. 66.7%), were bigger (median size 10.3 cm3 vs. 8.1 cm3) and more frequently involved the VA (71.4% vs. 52.9%), but were in anterior location with similar frequency (71.4% vs. 72.5%) Although the characteristics of our cohort (size and number of complications) limits further analysis of the predictors of each complication type, the abovementioned tumor features taken together suggest that large, CS, VA-involving FMMs could indirectly lead to increased risk of CSF complications as they require more extensive myofascial dissection, bone drilling, dural exposure and repair, especially when VA exposure and transposition is needed at the level of its dural entry and intracranial course. Posterior fossa surgery requiring more extensive myofascial dissection and bone disruption is associated with higher risk of CSF leak and pseudomeningocele [34, 35]. When indicated and feasible, minimally-invasive techniques of myofascial dissection and bone drilling in posterior fossa approaches allows dramatically reducing the risk of CSF leakage and pseudomeningocele [35,36,37].
The FMMRS is a new classification based on craniocaudal extension, anteroposterior location and VA involvement. That system simplifies previous classifications, such as the classification proposed by Bruneau and George [10] based on anteroposterior location (tumor anterior, lateral, posterior), VA involvement (tumor below, above, on both sides) and intra-extradural extension of the FMM. [10, 17] At the best of our knowledge, the FMMRS is the first scoring system to estimate the surgical risk of post-operative complications of FMM. Although the scoring system underwent successful internal and external validation, further larger studies are required for validation. Our study is limited by its retrospective nature, the sample size, lack of standardization of the surgical procedure. The different experience of the surgeons could affect the outcome of patients and the generalizability of our results. Objective evaluation, comparison and standardization of the surgical experience remains an unresolved challenge in neurosurgical training and research. Moreover, the present series includes patients operated across two decades, with evolving concepts and techniques, such as stereotactic radiosurgery that was successfully used to treat 3 sub totally-resected tumors [28]. Our multivariate analysis revealed a statistically significant negative correlation between completeness of resection with CS location, anterior location and VA involvement. The correlation suggests that the three anatomical features prompt neurosurgeons with different experience across different institutions to embrace a more conservative approach. In our analysis the VA encasement and VA contact with tumor were grouped in a single category as VA involvement. Although any degree of VA involvement mandates additional tumor dissection and manipulation, VA encasement can be more technically challenging with respect to VA contact, in order to preserve the VA, lower CN and brainstem. Further larger studies are required to investigate the impact of different degrees of VA involvement on the surgical morbidity. In the present series cervical laminectomy is not associated with a statistically significant difference in complication rate. Moreover, there is no obvious association with a specific complication subtype such as spinal fluid leakage or cranial neuropathy. Larger studies could ascertain the impact of laminectomy on the morbidity.
Conclusions
Microsurgical resection of FMMs through SOA and PLAs allows for symptomatic improvement or stability as well as for GTR in the vast majority of patients, despite complications in one third of the patients. Risk of tumor recurrence or regrowth after surgery is minimal. CS and anterior tumor locations, VA involvement are significant independent predictors of complications and can be successfully used as part of a classification and scoring system (FMMRS) to estimate the risk of post-operative complications.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- CS:
-
Craniospinal
- DL:
-
Dentate ligament
- FMM:
-
Foramen magnum meningioma
- FMMRS:
-
Foramen Magnum Meningioma Risk Score
- HR:
-
Hazards ratio
- KPS:
-
Karnofsky Performance Scale
- GTR:
-
Gross total resection
- SC:
-
Spinocranial
- SOA:
-
Sub-occipital approach
- STR:
-
Subtotal resection
- PLAS:
-
Posterior-lateral approaches
- VA:
-
Vertebral artery
References
Arnautović KI, Al-Mefty O, Husain M (2000) Ventral foramen magnum meningiomas. J Neurosurg. https://doi.org/10.3171/spi.2000.92.1.0071
Castellano F, Ruggiero G (1953) Meningiomas of the posterior fossa. Acta Radiol Suppl 104:1–57
Arnautović KI, Al-Mefty O, Pait TG et al (1997) The suboccipital cavernous sinus. J Neurosurg. https://doi.org/10.3171/jns.1997.86.2.0252
David CA, Spetzler RF (1997) Foramen magnum meningiomas. Clin Neurosurg 44:467–89
Miller E, Crockard HA (1987) Transoral transclival removal of anteriorly placed meningiomas at the foramen magnum. Neurosurgery. https://doi.org/10.1227/00006123-198706000-00026
Khattar N, Koutourousiou M, Chabot JD et al (2018) endoscopic endonasal and transcranial surgery for microsurgical resection of ventral foramen magnum meningiomas: a preliminary experience. Oper Neurosurg (Hagerstown, Md). https://doi.org/10.1093/ons/opx160
Stevenson GC, Stoney RJ, Perkins RK, Adams JE (1966) A transcervical transclival approach to the ventral surface of the brain stem for removal of a clivus chordoma. J Neurosurg. https://doi.org/10.3171/jns.1966.24.2.0544
Guidetti B, Spallone A (1980) Benign extramedullary tumors of the foramen magnum. Surg Neurol. https://doi.org/10.1007/978-3-7091-6954-4_3
Salas E, Sekhar LN, Ziyal IM et al (1999) Variations of the extreme-lateral craniocervical approach: anatomical study and clinical analysis of 69 patients. J Neurosurg. https://doi.org/10.3171/spi.1999.90.2.0206
Bruneau M, George B (2008) Foramen magnum meningiomas: Detailed surgical approaches and technical aspects at Lariboisière Hospital and review of the literature. Neurosurg Rev. https://doi.org/10.1007/s10143-007-0097-1
Bydon M, Martin Ma T, Xu R et al (2014) Surgical outcomes of craniocervial junction meningiomas: a series of 22 consecutive patients. Clin Neurol Neurosurg. https://doi.org/10.1016/j.clineuro.2013.11.023
Koc K, Anik I, Cabuk B, Ceylan S (2008) Fluorescein sodium-guided surgery in glioblastoma multiforme: a prospective evaluation. Br J Neurosurg. https://doi.org/10.1080/02688690701765524
Boulton MR, Cusimano MD (2003) Foramen magnum meningiomas: concepts, classifications, and nuances. Neurosurg Focus 14(6):1–8
Lanzino G, Paolini S, Spetzler RF (2005) Far-lateral approach to the craniocervical junction. Neurosurgery. https://doi.org/10.1227/01.NEU.0000176848.05925.80
Heros RC (1986) Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg. https://doi.org/10.3171/jns.1986.64.4.0559
Marin Sanabria EA, Ehara K, Tamaki N et al (2002) Surgical experience with skull base approaches for foramen magnum meningioma. Neurol Med Chir (Tokyo). https://doi.org/10.2176/nmc.42.472
George B, Lot G, Sen C (1995) Anterolateral and posterolateral approaches to the foramen magnum: Technical description and experience from 97 cases. Skull Base Surg 5:9–19
Couldwell WT (2015) Far lateral transcervical approach to the lower clivus and upper cervical spine. In: Snyderman C, Gardner P (eds) Master techniques in otolaryngology head and neck surgery skull base surgery. Wolters Kluwer, Philadelphia, pp 591–604
Barut N, Kale A, Suslu HT et al (2009) Evaluation of the bony landmarks in transcondylar approach. Br J Neurosurg. https://doi.org/10.1080/02688690902814725
Akalan N, Seçkin H, Kiliç C, Özgen T (1994) Benign extramedullary tumors in the foramen magnum region. Clin Neurol Neurosurg. https://doi.org/10.1016/0303-8467(94)90115-5
Yang SY, Boniello AJ, Poorman CE et al (2014) A review of the diagnosis and treatment of atlantoaxial dislocations. Glob Spine J. https://doi.org/10.1055/s-0034-1376371
Rhoton J (2000) The far-lateral approach and its transcondylar, supracondylar, and paracondylar extensions. Neurosurgery. https://doi.org/10.1097/00006123-200009001-00020
Wright NM, Lauryssen C (1998) Vertebral artery injury in C1–2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. J Neurosurg. https://doi.org/10.3171/jns.1998.88.4.0634
Choi D, Crockard HA (2013) Evolution of transoral surgery: three decades of change in patients, pathologies, and indications. Neurosurgery. https://doi.org/10.1227/01.neu.0000430324.24623.10
Crockard HA (1985) The transoral approach to the base of the brain and upper cervical cord. Ann R Coll Surg Engl 67(5):321
Tuite GF, Veres R, Crockard HA, Sell D (1996) Pediatric transoral surgery: indications, complications, and long-term outcome. J Neurosurg. https://doi.org/10.3171/jns.1996.84.4.0573
Magill ST, Shahin MN, Lucas CHG et al (2018) Surgical Outcomes, Complications, and management strategies for foramen magnum meningiomas. J Neurol Surg Part B Skull Base. https://doi.org/10.1055/s-0038-1654702
Mehta GU, Zenonos G, Patibandla MR et al (2018) Outcomes of stereotactic radiosurgery for foramen magnum meningiomas: an international multicenter study. J Neurosurg. https://doi.org/10.3171/2017.3.JNS163008
Margalit NS, Lesser JB, Singer M, Sen C (2005) Lateral approach to anterolateral tumors at the foramen magnum: factors determining surgical procedure. Neurosurgery. https://doi.org/10.1227/01.NEU.0000156796.28536.6D
Talacchi A, Biroli A, Soda C et al (2012) Surgical management of ventral and ventrolateral foramen magnum meningiomas: report on a 64-case series and review of the literature. Neurosurg Rev 35(3):359–68
Li D, Wu Z, Ren C et al (2017) Foramen magnum meningiomas: surgical results and risks predicting poor outcomes based on a modified classification. J Neurosurg. https://doi.org/10.3171/2016.2.JNS152873
George B, Lot G, Boissonnet H (1997) Meningioma of the foramen magnum: a series of 40 cases. Surg Neurol. https://doi.org/10.1016/S0090-3019(96)00204-2
Samii M, Klekamp J, Carvalho G (1996) Surgical results for meningiomas of the craniocervical junction. Neurosurgery. https://doi.org/10.1097/00006123-199612000-00003
Legnani FG, Saladino A, Casali C et al (2013) Craniotomy vs. craniectomy for posterior fossa tumors: a prospective study to evaluate complications after surgery. Acta Neurochir (Wien) 155:2281–2286. https://doi.org/10.1007/s00701-013-1882-y
Legninda Sop FY, D’Ercole M, Izzo A et al (2021) The impact of neuronavigation on the surgical outcome of microvascular decompression for trigeminal neuralgia. World Neurosurg 149:80–85. https://doi.org/10.1016/j.wneu.2021.02.063
Lau T, Reintjes S, Olivera R et al (2015) C-shaped incision for far-lateral suboccipital approach: anatomical study and clinical correlation. J Neurol Surg Part B Skull Base 76:117–121. https://doi.org/10.1055/s-0034-1390396
Felbaum DR, Mueller K, Anaizi A et al (2016) Preservation of the myofascial cuff during posterior fossa surgery to reduce the rate of pseudomeningocele formation and cerebrospinal fluid leak: a technical note. Cureus. https://doi.org/10.7759/cureus.946
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
IRB Approved Stanford Health Care and Massachusetts General Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11060_2021_3773_MOESM1_ESM.jpg
Supplementary file1 Predicted probability of tumor resection with complications on the basis of Foramen Magnum Meningioma Risk Score (FMMRS) class. (a) The AUC curve was 0.81 (95% CI 0.61–0.98) in the internal validation cohort. (b) The AUC of the scoring system was 0.86 (95% CI 0.65–0.97) in the external validation cohort. (JPG 52 kb)
Rights and permissions
About this article
Cite this article
Fatima, N., Shin, J.H., Curry, W.T. et al. Microsurgical resection of foramen magnum meningioma: multi-institutional retrospective case series and proposed surgical risk scoring system. J Neurooncol 153, 331–342 (2021). https://doi.org/10.1007/s11060-021-03773-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03773-z