Abstract
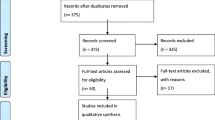
Foramen magnum meningiomas (FMMs) are challenging lesions and controversy still exists regarding their optimal management. In the present paper, we propose some principles of surgical treatment of FMMs. We analyzed our series of 39 patients: the average maximum diameter was 31.1 mm (sd, 10.7). In two cases, there was extradural extension. We operated all anterior lesions through dorsolateral approach to craniovertebral junction and all posterior lesions through midline suboccipital approach and C1 laminectomy, following the prevalence of side of the tumor. There were no complications except for one case of post-operative hypoglossus paresis. We translated our experience with surgery of foramen magnum meningiomas into a classification system and a complexity score, in order to assign a score to each individual case and plan the surgical strategy. When the complexity score is 5 or more, we propose subtotal removal, in consideration of the benign nature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Foramen magnum meningioma (FMM) has first been describes in 1872 [22]. Meningiomas located in this area represent challenging lesions because of their close proximity with the brainstem and lower cranial nerves as well as with the adjacent vertebral artery and its branches. The majority of these lesions (90%) are ventral and ventrolateral, but they can be located anywhere in the foramen magnum ring [11, 12, 39,40,41]; thus, surgical approaches need to be tailored to the location of the mass. However, controversy still exists regarding the optimal management of anterior or anterolateral lesions. In the current analysis, we review our experience over the last 15 years in the surgery of FMMs. In view of the favorable results we have seen in this series, we have translated the decisions made with respect to guidance and treatment of the patients into a classification system and complexity score.
Materials and methods
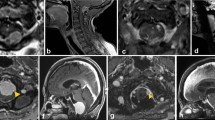
The 39 patients included in this study were operated by the senior author (H.B.) for FMMs. We summarized clinical presentation in long tract symptoms, cranial nerve symptoms, and other symptoms (Table 1). For the pre-operative and post-operative disability evaluation, we used the modified Rankin Scale. Imaging work-up included contrast-enhanced magnetic resonance imaging (MRI), computed tomography (CT) with bone algorithm, and vertebral angiography.
Surgical approaches were evaluated for complications and mortality. Based on these evaluations, we classified the lesion feature: maximum tumor diameter, compartment of development (intradural, extradural, and intra-extradural), vertebral artery (VA) involvement (partial and total encasement), brainstem (BS) adhesion, and grade of removal.
In addition, we defined parameters for axial and sagittal localization and attachment of the tumor as follows:
Axial localization and axial dural attachment: the lesions located in front of the dentate ligament were classified as “anterior” and the lesions behind the dentate ligament were considered as “posterior.” We further divided the anterior dura into left and right sides along the midline and every side into three thirds to systematically analyze the characteristics of dural attachment. This way, we classified lesions with symmetrical dural attachment along the midline as “purely anterior” and lesions with asymmetrical dural attachment with prevalence to one side as “anterolateral.” Within the anterolateral lesions, meningiomas with a complete prevalence towards one side and no extension of dural attachment beyond the midline were classified as “type A” and the meningiomas with the dural attachment on both sides along the midline with differing degrees of extension as “type B” (Fig. 1A, B).
Sagittal localization: the FM region was divided into two regions. Tumors located between the horizontal line passing through the junction middle-inferior third of the clivus and the horizontal line passing through the basion were classified as “high FM” and tumors located between this last line and the horizontal line passing through the superior edge of the C2 vertebral body were considered as “low FM” (Fig. 2).
Sagittal dural attachment: we evaluated the extension of the sagittal dural attachment and the ratio with maximum craniocaudal diameter of the tumor. Within the anterior lesions, we described as “type 1” the tumor with ratio < 1, and “type 2” with ratio ≥ 1 (Fig. 3)
Graphical illustration of the two regions considered for foramen magnum (FM). High FM (H): between the horizontal line passing through the junction middle-inferior third of the clivus and the horizontal line passing through the basion. Low FM (L): between this last line and the horizontal line passing through the superior edge of C2 vertebral body
We then retrospectively analyzed our set of 39 patients according to these features and developed a complexity score (CS) for anterior and anterolateral lesions in order to define the best surgical approach and to predict the prognosis. The score can have from a minimum value of 1 to a maximum of 8 (Table 2). We correlated the value of CS with the grade of removal and clinical follow-up.
All the data were analyzed using commercially available software (IBM SPSS Statistics for Mac, Version 22.0, Armonk, NY: IBM Corp) for descriptive statistics and ANOVA test. Significance was ascribed for p < 0.05. Logistic regression analysis was used to assess the predictive value of CS.
Results
Our set included 39 patients, 23 women and 16 men. The average age was 53 ± 14 years, ranging from 15 to 78 years of age. Female patients had an average age of 49.2 years and male patients had an average age of 60.3 years. None of the lesions showed signs of atypia during histological exam.
Thirty-three patients (84.6%) showed long tract symptoms and 14 patients (35.8%) showed cranial nerve deficits. Other symptoms were headache and neck pain (6 and 5 cases respectively) (Table 1). The average pre-operative modified Rankin Scale was 1.46 ± 0.9.
Surgery and follow-up
We operated all anterior lesions in a dorsolateral approach to the craniovertebral junction and all posterior lesions in a midline suboccipital approach and C1 laminectomy, according to the side prevalence of the tumor. There were no complications except for one case of post-operative hypoglossus paresis. We did not report any deaths. The average modified Rankin Scale at the discharge is 1.48 (± 0.99). In two cases, the clinical condition deteriorated at discharge and the CS was 5 and 6. Minimum follow-up was 6 months. During the follow-up period, no remissions or deaths were reported. Total removal was possible in 29 patients (Table 3).
Tumor features and complexity score
Considering the relationship between the axial dural attachment of the tumor and the dentate ligament, 33 patients showed anterior lesions (84.6%) and six patients showed posterior lesions (15.3%). We further differentiated the dural attachment within the anterior lesions into eight purely anterior and 25 anterolateral lesions. The anterolateral tumors were divided into 12 “type A” tumors and 13 “type B” tumors (Table 3).
Of the meningiomas, 10 were located in the “low FM,” 23 in the “high FM,” and six cases showed a symmetrical growth in both regions of the FM. Studying the features of the sagittal dural attachment for the anterior and anterolateral tumors, the “type 1” meningiomas were 22 and the “type 2” were 11 (Table 3).
The average maximum diameter was 31.1 mm (± 10.7 mm). In two cases (5.1%), there was an extradural extension of the tumor.
We also considered the involvement of neurovascular structures. Brainstem adhesions were present in six cases (18.0%) and a VA encasement was present in 17 cases (51.5%) (Table 3), 12 of the latter being cases of total encasement (30.7% of patients) and five of partial encasement (12.8% of patients).
We decided to add two additional points to the CS for total VA encasement and BS adhesion as these key conditions influence surgical treatment and prognosis. In fact, the frequency of both these parameters was significantly higher (p < 0.05) in the group of patients who underwent partial removal than in the total removal group.
We calculated the CS for each patient with anterior meningioma obtaining the following results: five cases with CS 1, eight cases with CS 2, nine cases with CS 3, five cases with CS 4, three cases with CS 5, two cases with CS 6, and one case with CS 7 (Table 3).
Correlating CS and grade of removal, we obtained that the cases in which a total removal was possible had significantly (p < 0.05) lower CS mean value (2.5) than patients who underwent only partial removal (CS 4.9).
A logistic regression was performed to ascertain the value of CS on the likelihood to have partial removal of the lesion. The logistic regression model was statistically significant (p = 0.001). The model explained 37% (Nagelkerke R2) of the variance and correctly classified 85.0% of cases.
Discussion
Meninigiomas are the most frequent FM tumors. FMMs account for 2.5% of all intracranial meningiomas and 4.0% of those are found in the posterior fossa [11, 12, 39,40,41].
In 1938, Cushing and Eisenhardt have first proposed a classification system for foramen magnum tumors, by differentiating them into craniospinal and spinocranial lesions [16]. In 1953, Castellano and Ruggiero [15] have then proposed a classification of meningiomas of the posterior cranial fossa according to the site of dural attachment posterior surface of the petrous bone, tentorium, cerebellar convexity, clivus, and foramen magnum. In the following years, different aspects of these kinds of tumors have been further analyzed in more detail. George et al., in 1997 [18], have classified FMMs into anterior, lateral, or posterior lesions and inradural, extradural, or intra-extradural, and above, below, or both sides of the VA according to the insertion zone along the midline and denticulate ligament, the compartment of growth, and extent along the VA, respectively.
Here, we add an additional, more detailed classification system based on an analysis of the results of our surgical series. We further translate the applied guidance and treatment into a classification system. The key features analyzed by our classification system, in particular those regarding the characteristics of dural attachment, allow to define the surgical approach. By providing a tailored approach, we minimize the surgical trauma and, consequently, the number of potential complications for our patients.
Many surgical strategies have been proposed for the treatment of anterior and anterolateral FMMs including the more recent endoscopic transclival approach that has been preferred by some authors in purely ventral lesions [25]. In our experience, the dorsolateral trans-condylar approach represents a valid and safe surgical route; however, a standardized surgical approach may also include unnecessary surgical steps [6, 7]. Meningiomas located anterior to the brainstem and cervical cord cannot be removed safely without a sufficiently tailored exposure. There is continuing controversy in the literature concerning the necessity of resecting the occipital condyle [2, 4, 9, 10, 19, 21, 24, 27, 32, 33, 35, 36] but it is our conviction that a wide exposure of the tumor dural attachment is essential. In fact, an early devascularization of meningioma, proved to be the best strategy, is possible only at the site of tumor insertion to the dura, requiring a so-called extreme lateral exposure. To visualize the tumor from a lateral direction requires resection not only of the medial rim of the FM (medial portion of the condyle) but also of the jugular tubercle and, depending on the caudal extension of the tumor, of the medial portion of the C1 lateral mass. Based on these concepts, we developed a classification system directly relating to the required surgical exposure. Like with a “compass,” the angle of the surgical approach must be “open” laterally as much as the dural attachment of the tumor is anterior and extended (Fig. 4).
In consequence, meningioma types A.5-2, A.6-2, and B.2 (Figs. 3 and 5), as proposed by our CS, with anterior, extended axial, and sagittal dural attachment, require maximum extreme lateral exposure. Following the same principles, for type A.1-1, A.2-1, and A.3-1 meningiomas, with a lower axial and sagittal extension of the dural attachment, lateral exposure can be reduced and some surgical steps such as mastoidectomy, exposure of the transverse process of the atlas, extensive resection of the occipital condyle including its articular facet, and complete exposure of the jugular bulb can be avoided.
The location of the tumor on the sagittal plane is an important feature to decide the craniocaudal extension of surgical approach. Using the anatomical limits defined by George and Lot in 1995 [17], we divided the FM region into two parts, high and low FM, by an imaginary line passing through the basion. The larger extension of the meningioma in the superior or inferior part of the FM region determines the superior extent of the craniotomy or the levels of laminotomy [5, 8]. In our series, we did not observe significant differences in relation to the sagittal localization, in terms of surgical resection and outcome, presumably because adherence to neurovascular structures, in particular the encasement of VA, shows almost the same frequency between the two types of localization (high and low FM). We observed VA encasement in 50% of tumors located in low FM and in 43% of tumors located in the high FM.
The complexity score based on our classification system and three additional important tumor features (VA encasement, BS adhesion, and extradural extension), proposed here, could help the intraoperative decision-making. In our hands, in patients with a high complexity score (i.e., CS ≥ 5), the risk of surgical injury of neurovascular structures is very high and the subtotal removal of the tumor is advised. For the calculation of our score, we decided to assign the highest values to total VA encasement and BS adhesion, as, in our experience, these appear to be two key features contraindicating a safe tumor removal.
Over the years, several authors have analyzed the difficulties encountered during the surgical treatment of FMMs. Tumor recurrence, extradural growth, vascular encasement, and arachnoid scarring are important and widely accepted factors in the decision against radical excision of meningiomas of the foramen magnum [1, 18, 33, 34]. We report 51.5% global percentage of VA encasement with total VA encasement in 30.7%. In the literature, this percentage varies considerably, with the mean value of 42.9% of all published surgical series [3, 13, 14, 18,19,20, 23, 28, 30,31,32,33, 38, 39]. During pre-operative planning, it is very important to analyze the course of VA and the presence of VA encasement trough MRI imaging, as this artery can be damaged during different steps of surgery: muscular dissection, bone opening, tumor removal [3, 29, 38, 39].
The presence or absence of an arachnoidal plane between the tumor and the BS is another crucial point that determines the extent of removal [1, 38] and post-operative morbidity [19, 33]. In our series, we report six cases of BS adhesion (18%).
The last feature determining our score is the extradural extension of the tumor. In meningiomas, this is a rare condition [13]. The VA sheath and even the arterial adventitia can also be infiltrated. This situation can explain the higher incidence of incomplete removal and higher morbidity as compared to intradural meningiomas [26, 29, 37]. In case of extradural extension of the meningioma, maximum extreme lateral exposure is often required. In our series, we report extradural extension in 5% of cases.
With these considerations in mind, a detailed pre-operative planning is required and, during surgery, an accurate devascularization of the tumor is mandatory for working in a clean surgical field for the proper identification of neurovascular structures. However, for patients with a particularly high CS (CS 4.9), partial removal was the preferred surgical approach. In fact, total removal was usually performed in patients with a significantly lower mean CS value (2.5). For CS ≥ 5, partial tumor removal may provide the best surgical result considering outcome and prognosis.
Conclusions
Based on our experience with surgery of foramen magnum meningiomas, we developed a classification system and associated complexity score in order to make the right decisions at every turn of the patient’s course. Our score includes the following: type of dural attachment, vertebral artery encasement, brainstem adhesion, and extradural extension. In consideration of the benign behavior of the tumor, we propose subtotal removal for a complexity score of 5 or higher.
References
Arnautovic KI, Al-Mefty O, Husain M (2000) Ventral foramen magnum meninigiomas. J Neurosurg 92:71–80
Babu RP, Sekhar LN, Wright DC (1994) Extreme lateral transcondylar approach: technical improvements and lessons learned. J Neurosurg 81:49–59. https://doi.org/10.3171/jns.1994.81.1.0049
Bassiouni H, Ntoukas V, Asgari S, Sandalcioglu EI, Stolke D, Seifert V (2006) Foramen magnum meningiomas: clinical outcome after microsurgical resection via a posterolateral suboccipital retrocondylar approach. Neurosurgery 59:1177–1185; discussion 1185–1177. https://doi.org/10.1227/01.neu.0000245629.77968.37
Bejjani G, Sekhar LN, Riedel C (2000) Occipitocervical fusion following the extreme lateral transcondylar approach. Surg Neurol 54:109–116
Bertalanffy H, Benes L, Becker R, Aboul-Enein H, Sure U (2002) Surgery of intradural tumors at the foramen magnum level. Oper Tech Neurosurg 5:11–24
Bertalanffy H, Bozinov O, Sürücü O, Benes L, Sure U, Kappus CH (2011) Intraaxial lesions of the foramen magnum. In: Bruneau M, George B, Spetzler R (eds) The vertebral artery. Springer-Verlag, Berlin, pp 455–469
Bertalanffy H, Bozinov O, Sürücü O, Sure U, Benes L, Kappus CH, Krayenbühl N (2010) Dorsolateral approach to the craniocervical junction. In: Cappabianca P (ed) Cranial, cranio-facial and skull base surgery. Springer-Verlag, Italia, pp 175–196
Bertalanffy H, Gilsbach JM, Mayfrank L, Klein HM, Kawase T, Seeger W (1996) Microsurgical management of ventral and ventrolateral foramen magnum meningiomas. Acta Neurochir Suppl 65:82–85
Bertalanffy H, Seeger W (1991) The dorsolateral, suboccipital, transcondylar approach to the lower clivus and anterior portion of the craniocervical junction. Neurosurgery 29:815–821
Bertalanffy H, Sure U (2000) Surgical approaches to the jugular foramen. Cranial base surgery London pp 237–258
Borba LA, de Oliveira JG, Giudicissi-Filho M, Colli BO (2009) Surgical management of foramen magnum meningiomas. Neurosurg Rev 32:49–58; discussion 59–60. https://doi.org/10.1007/s10143-008-0161-5
Bruneau M, George B (2008) Foramen magnum meningiomas: detailed surgical approaches and technical aspects at Lariboisiere Hospital and review of the literature. Neurosurg Rev 31:19–32; discussion 32–33. https://doi.org/10.1007/s10143-007-0097-1
Bruneau M, George B (2010) Classification system of foramen magnum meningiomas. J Craniovertebr Junction Spine 1:10–17. https://doi.org/10.4103/0974-8237.65476
Bydon M, Ma TM, Xu R, Weingart J, Olivi A, Gokaslan ZL, Tamargo RJ, Brem H, Bydon A (2014) Surgical outcomes of craniocervial junction meningiomas: a series of 22 consecutive patients. Clin Neurol Neurosurg 117:71–79. https://doi.org/10.1016/j.clineuro.2013.11.023
Castellano F, Ruggiero G (1953) Meningiomas of the posterior fossa. Acta Radiol Suppl 104:1–177
Cushing H, Eisenhardt L (1938) Meningiomas: their classification, regional behaviour, life history, and surgical end results. Charles C Thomas, Springfield. https://doi.org/10.1016/S0002-9610(38)91219-X
George B, Lot G (1995) Foramen magnum meningiomas. A review from personal experience of 37 cases and from cooperative study of 106 cases. Neurosurg Q 5:149–167
George B, Lot G, Boissonnet H (1997) Meningioma of the foramen magnum: a series of 40 cases. Surg Neurol 47:371–379
Goel A, Desai K, Muzumdar D (2001) Surgery on anterior foramen magnum meningiomas using a conventional posterior suboccipital approach: a report on an experience with 17 cases. Neurosurgery 49:102–106; discussion 106–107
Guidetti B, Spallone A (1988) Benign extramedullary tumors of the foramen magnum. Adv Tech Stand Neurosurg 16:83–120
Hakuba A, Tsujimoto T (1993) Transcondylar approach for foramen magnum meningiomas. Surgery of cranial base tumors New York
Hallopeau H (1874) Note sur deux faits de tumeur de mesocephale. Gaz Med (Paris) 3
Kandenwein JA, Richter HP, Antoniadis G (2009) Foramen magnum meningiomas--experience with the posterior suboccipital approach. Br J Neurosurg 23:33–39. https://doi.org/10.1080/02688690802545932
Katsuta T, Matsushima T, Wen HT (2000) Trajectory of the hypoglossal nerve in the hypoglossal canal: significance for the transcondylar approach. Neurol Med Chir (Tokyo) 40:206–209
Khattar N, Koutourousiou M, Chabot JD, Wang EW, Cohen-Gadol AA, Snyderman CH, Fernandez-Miranda JC, Gardner PA (2018) Endoscopic endonasal and transcranial surgery for microsurgical resection of ventral foramen magnum meningiomas: a preliminary experience. Oper Neurosurg (Hagerstown) 14:503–514. https://doi.org/10.1093/ons/opx160
Levy WJ Jr, Bay J, Dohn D (1982) Spinal cord meningioma. J Neurosurg 57:804–812. https://doi.org/10.3171/jns.1982.57.6.0804
Lot G, George B (1999) The extent of drilling in lateral approaches to the cranio-vertebral junction area from a series of 125 cases. Acta Neurochir 141:111–118
Margalit NS, Lesser JB, Singer M, Sen C (2005) Lateral approach to anterolateral tumors at the foramen magnum: factors determining surgical procedure. Neurosurgery 56:324–336; discussion 324–336
Meyer FB, Ebersold MJ, Reese DF (1984) Benign tumors of the foramen magnum. J Neurosurg 61:136–142. https://doi.org/10.3171/jns.1984.61.1.0136
Pamir MN, Kilic T, Ozduman K, Ture U (2004) Experience of a single institution treating foramen magnum meningiomas. J Clin Neurosci 11:863–867. https://doi.org/10.1016/j.jocn.2004.02.007
Pirotte BJ, Brotchi J, DeWitte O (2010) Management of anterolateral foramen magnum meningiomas: surgical vs conservative decision making. Neurosurgery 67:ons58–70; discussion ons70. doi:https://doi.org/10.1227/01.neu.0000382971.63877.dd
Salas E, Sekhar LN, Ziyal IM, Caputy AJ, Wright DC (1999) Variations of the extreme-lateral craniocervical approach: anatomical study and clinical analysis of 69 patients. J Neurosurg 90:206–219
Samii M, Klekamp J, Carvalho G (1996) Surgical results for meningiomas of the craniocervical junction. Neurosurgery 39:1086–1094 discussion 1094–1085
Sekhar LN, Swamy N, Jaiswal V, Rubinstein E, Hirsch WJ, Wright DC (1994) Surgical excision of meningiomas involving the clivus: preoperative and intraoperative features as predictors of postoperative functional deterioration. J Neurosurg 81:860–868
Sen CN, Sekhar LN (1990) An extreme lateral approach to intradural lesions of the cervical spine and foramen magnum. Neurosurgery 27:197–204
Spector S, Anderson G, McMenomey S, Horgan M, Kellogg J, Delashaw J (2000) Quantitative description of the far-lateral transcondylar transtubercular approach to the foramen magnum and clivus. J Neurosurg 92:824–831
Stein BM, Leeds NE, Taveras JM, Pool JL (1963) Meningiomas of the foramen magnum. J Neurosurg 20:740–751. https://doi.org/10.3171/jns.1963.20.9.0740
Talacchi A, Biroli A, Soda C, Masotto B, Bricolo A (2012) Surgical management of ventral and ventrolateral foramen magnum meningiomas: report on a 64-case series and review of the literature. Neurosurg Rev 35:359–367; discussion 367–358. https://doi.org/10.1007/s10143-012-0381-6
Wu Z, Hao S, Zhang J, Zhang L, Jia G, Tang J, Xiao X, Wang L, Wang Z (2009) Foramen magnum meningiomas: experiences in 114 patients at a single institute over 15 years. Surg Neurol 72:376–382; discussion 382. https://doi.org/10.1016/j.surneu.2009.05.006
Yasargil M, Mortara R, Curcic M (1980) Meningiomas of basal posterior fossa. Advances and technical standards in neurosurgery Berlin
Yasuoka S, Okazaki H, Daube JR, MacCarty CS (1978) Foramen magnum tumors. Analysis of 57 cases of benign extramedullary tumors. J Neurosurg 49:828–838. https://doi.org/10.3171/jns.1978.49.6.0828
Acknowledgements
We thank Miriam Polak for the artworks and Claudia Davenport for critically reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The clinical study was approved by the ethical commission of the institute.
Informed consent
All patients (parents in the case of minors) were fully informed about the surgery and the documentation used for this study and signed informed consent.
Rights and permissions
About this article
Cite this article
Giordano, M., Dugoni, D. & Bertalanffy, H. Improving results in patients with foramen magnum meningiomas by translating surgical experience into a classification system and complexity score. Neurosurg Rev 42, 859–866 (2019). https://doi.org/10.1007/s10143-018-01060-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-01060-6