Abstract
Brain tumor patients undergoing craniotomy generally receive prophylaxis against venous thromboembolism (VTE), but modalities in use differ widely and have been debated in the literature. A systematic review and meta-analysis was conducted to assess the efficacy and safety of VTE prophylaxis among brain tumor patients undergoing craniotomy. Ten randomized controlled trials were included in the final efficacy analysis. The various prophylactic measures employed in these studies reduced the risk for thrombosis compared to controls with an overall risk ratio of 0.61 (95 % CI: 0.47–0.79) in the fixed effect model. Although Cochrane Q-test showed unimportant heterogeneity across studies (p = 0.19) and the I2, a measure of heterogeneity between studies, was reasonably low at 28 %, subgroup analysis indicated that intervention type was a potential effect modifier for efficacy (p = 0.04). Unfractionated heparin alone showed a stronger reduction in VTE risk compared to placebo (RR = 0.27; 95 % CI: 0.10–0.73), and LMWH combined with mechanical prophylaxis showed a lower VTE risk as compared to mechanical prophylaxis alone (0.61; 95 % CI: 0.46–0.82). This meta-analysis demonstrates a statistically significant VTE risk reduction among brain tumor patients receiving prophylaxis, with chemical prophylaxis showing the strongest risk reduction. Five studies were included in the safety analysis, which showed an overall increased risk of bleeding comparing different prophylactic measures to different controls (RR = 2.02; 95 % CI: 1.14–3.58; I2 = 0 %; p = 0.86). Interventions in these studies were associated with an increased risk of post-operative, minor hemorrhage (RR = 2.20; 95 % CI = 1.00; 4.85), while the risk of major hemorrhage was not increased by chemoprophylaxis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with brain tumors undergoing craniotomy are at a significantly increased risk of developing venous thromboembolism (VTE). Previously reported risks for developing deep vein thrombosis (DVT) and pulmonary embolism (PE) are 31 and 5 %, respectively, for patients undergoing craniotomy [1–3]. The etiology of these events is multifactorial and includes relative stasis after surgery, direct activation of the coagulation cascade due to tissue damage, as well as tumor-specific pro-coagulant effects. Other risk factors include older age, large tumor size, and peri-operative steroid use. Injury to the vessel wall due to chemotherapy and/or radiation therapy can further increase the risk of VTE among brain tumor patients [4–7].
Interventions used to prevent VTE in brain tumor patients undergoing craniotomy include mechanical prophylaxis and/or pharmacological prophylaxis. Current modalities for mechanical prophylaxis include the application of sequential compression devices (SCD), graduated compression stockings, or a combination of both [8]. Pharmacological prophylaxis is typically achieved with unfractionated heparin (UFH) or low molecular weight heparin (LMWH), which reduce the incidence of VTE through direct anticoagulation effects but also carry the risk of postoperative bleeding [9, 10].
The American College of Chest Physicians’ (ACCP) guidelines consider patients with central nervous system neoplasms undergoing surgery a high-risk population for VTE and recommend both pharmacologic prophylaxis and mechanical prophylaxis. The exact methods and timing for commencing pharmacological prophylaxis were not specified, however [11]. The National Institute for Health and Care Excellence (NICE) guidelines recommend mechanical prophylaxis among all neurosurgical patients, but recommend pharmacological prophylaxis only among patients who are considered low risk for hemorrhage [12].
In this systematic review and meta-analysis, randomized controlled trials (RCTs) that evaluated the efficacy and safety of different methods of prophylaxis in brain tumor patients undergoing craniotomy were pooled for analysis. We aim to help guide clinical practice for these patients by identifying the most efficacious and safest modality for VTE prophylaxis.
Methods
Literature search
The PubMed, EMBASE, and Cochrane Library databases were searched from their establishment date through October 2014 for studies evaluating the efficacy and safety of pharmacological prophylaxis and/or mechanical prophylaxis in brain tumor patients undergoing craniotomy. An additional supplementary search was performed at the time of manuscript review, through June 30, 2016. Appropriate medical subject heading (MeSH) terms, text words (tw), and Emtree terms were used (Appendix 1). Additional articles were identified from the reference lists of relevant studies and reviews.
Study selection
Studies were included if they met the following criteria: (1) RCTs conducted on patients diagnosed with brain tumor and undergoing craniotomy, (2) patients were older than 18 years old, recently diagnosed with a brain tumor of any grade, not at risk of VTE and without a history of VTE events, and who were randomly assigned to prophylaxis (chemical prophylaxis, mechanical prophylaxis, or a combination of both), (3) sample size of greater than or equal to 20 patients with reported data on efficacy outcomes (e.g., symptomatic and objectively verified VTE) or safety outcomes (e.g., major or minor hemorrhage). Articles were excluded if they were not in English. Titles and abstracts were screened and potentially relevant articles were selected for full-text evaluation, which was performed independently by five investigators. Discrepancies were resolved by consultation with the senior authors (R.A.M., T.R.S.). The quality of the RCTs was evaluated using the Jadad score, which assesses randomization, double blinding, and withdrawals/dropouts on a scale from zero (very poor) to five (rigorous) [12].
Data extraction
For each identified article, the following information was extracted: study characteristics (authors, publication year, country of origin, sample size, number included for intent-to-treat analysis, center type, number of surgeons, follow-up duration, journal impact factor); participant characteristics (gender, age, ethnicity, inclusion/exclusion criteria, types of tumor, comorbidities), perioperative details, VTE intervention details (dose, duration, frequency, administration time), study control type, efficacy outcomes (number of VTE events in each group), and safety outcomes (occurrence of bleeding, hemorrhage, or any other adverse event). Data extraction was conducted independently by two investigators.
Data analysis
Data analysis was performed using Comprehensive Meta-Analysis (CMA) Version 3 (Biostat, Inc., Englewood, NJ, USA). The fixed-effects model using the inverse variance method was used to obtain the overall relative risk (RR) estimates and the 95 % confidence intervals for both the efficacy and safety analyses. A random-effects model according to the method of DerSimonian and Laird [13] that accounted for variation between studies in addition to within-study variance was evaluated for comparison. Forest plots were used to visualize the individual and summary estimates. Heterogeneity was evaluated among studies by using the Cochran’s Q-test (p < 0.10) and the I2 to measure the proportion of total variation due to that heterogeneity. An I2 value >50 % was considered to be high [14]. Potential sources of heterogeneity were explored using sub-group analyses by categorical covariates [intervention type (chemical vs. chemical; chemical vs. mechanical; chemical vs. placebo; and mechanical vs. placebo), follow-up duration (≤30 days; >30 days; N/A), intervention time (preoperative; postoperative), study quality (≤3; >3), center type (multicenter; single), and region of study origin (US; non-US)]. Studies that classified prophylaxis as preoperative and/or perioperative were grouped in one category. A univariate meta-regression was conducted on each categorical covariate separately as well as on age (continuous) and a multivariate meta-regression was also used to explore sources of heterogeneity. A sensitivity analysis was conducted to examine the influence of individual studies on the overall risk estimate by recalculating the pooled estimates for the remainder of the studies after removing one study at a time. A cumulative meta-analysis was conducting by publication year. Potential publication bias was assessed by funnel plots, Egger’s linear regression test, and Begg’s correlation test. If publication bias was indicated, the number of missing studies was evaluated by the trim and fill method. A p-value <0.05 was considered significant unless otherwise indicated. Because Peto’s method [15] using the hypergeometric variance performs well with low-rate events (≤1 %), all of the above models using were recalculated using Peto odds ratio (OR) estimates.
Results
Study characteristics
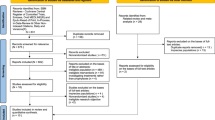
After the systematic search, 826 articles from PubMed, 226 articles from Embase, and eight articles from the Cochrane Library were identified (Fig. 1). After the removal of duplicates and papers that did not meet the inclusion criteria based on title and abstract, 33 articles remained for full text review. After the final review, ten RCTs reporting 212 VTE events among 1263 participants were included in this meta-analysis [1–6, 9, 16–18]. No RCTs meeting the inclusion criteria were identified in the supplementary search performed at the time of review, through June 30, 2016.
Characteristics of the ten RCTs included in this meta-analysis are found in Table 1. In the intervention arm, the total number of participants ranged from 11 to 193 and the number of VTE cases from 1 to 33. In the control arm, the total number of participants ranged from 20 to 207 and the number of VTE cases from 0 to 51. All studies included both men and women but only seven of ten studies gave the exact percentage of men and women per study. For those studies, the male percentage ranged from 45 to 52 % in the intervention arm and from 44 to 58 % in the control arm.
The mean age of participants ranged from 49 to 57.5 years. Seven studies were conducted in the United States (US), one in Israel, one in Germany, and one in Canada. Study follow-up varied across studies (5–348 days). VTE prophylaxis was started either pre/perioperatively (six studies) [2, 5, 17–20] or postoperatively (four studies) [3, 9, 16, 21]. The types of prophylaxis used in each study were diverse and were compared to different controls.
Assessment of study quality using the Jadad score yielded an average score of 2.8. The diagnosis and reporting of VTE varied across the RCTs. In all studies except for one [5], asymptomatic VTE was diagnosed by using an ultrasound or a venography during the post-operative period prior to discharge. The study publication year started as early as 1977 and the most recent study was in 2003. Trials that did not report details about the type of control were considered compared to placebo. The analyses conducted on the ten RCTs as well as in our meta-analysis were done on the intent-to-treat population.
Efficacy analysis
Of the ten studies included in the meta-analysis, only two demonstrated a significant reduction in VTE risk [1, 4]; one study was borderline significant [9]; while the remaining seven trials reported non-statistically significant results. Pooling results from all ten studies demonstrated a protective effect between the different prophylaxis regimens and VTE risk (Fig. 2). The pooled RR of VTE was 0.61 (95 % CI: 0.47; 0.79; fixed-effects model). Results from the random-effects model were similar (0.60; 95 % CI: 0.40; 0.89) and no significant heterogeneity was observed (I2 = 28 %; P-heterogeneity = 0.19).
Forest plot represents the relative risk for developing venous thromboembolism (VTE) (95 % CI) with different prophylactic regimens as compared to different control regimens from ten randomized controlled studies in adult brain tumor patients undergoing craniotomy. Horizontal lines denote 95 % CIs, solid squares represent the point estimate of each study and the diamond represents the pooled estimate of the intervention effect. The size of the solid squares is proportional to the weight of the study. Weights are from the fixed-effects analysis using the using the inverse variance method. The I2 and p values for heterogeneity are shown
Subgroup analyses revealed that intervention type was a potential effect modifier (p = 0.04). Specifically, UFH alone showed a stronger reduction in VTE risk as compared to placebo (RR = 0.27; 95 % CI: 0.10–0.73), while LMWH combined with mechanical prophylaxis showed a lower VTE risk as compared to mechanical prophylaxis alone (RR = 0.61; 95 % CI: 0.46–0.82). The remaining comparisons (combination of LMWH and mechanical prophylaxis vs. combination of UFH and mechanical prophylaxis; mechanical prophylaxis vs. placebo) showed non-significant results (Fig. 3). Using the Peto OR for the comparison of mechanical prophylaxis vs. placebo revealed a significant reduction in VTE events (Peto OR = 0.30; 95 % CI = 0.11; 0.87). Subgroup analysis and meta-regression analyses based on other trial-level covariates such as age (p = 0.24), intervention time (p = 0.74), follow-up duration (p = 0.15), study quality (p = 0.67), center type (p = 0.98), and country (p = 0.98) showed no significant evidence that effects varied by group. Dose was not tested for effect modification because of the diversity of the interventions used in these trials.
Forest plot represents the relative risk for developing venous thromboembolism (VTE) (95 % CI) with different prophylactic regimens as compared to different control regimens from ten randomized controlled studies in adult brain tumor patients undergoing craniotomy. Horizontal lines denote 95 % CIs, solid squares represent the point estimate of each study and the diamonds represent the pooled estimate of the intervention effects for each subgroup. The size of the solid squares is proportional to the weight of the study. Weights are from the fixed-effects analysis using the using the inverse variance method. The first group represents the anticoagulant UFH alone as compared to placebo (I2 = 48.61 %; p = 0.16); the second group represents the combination of LMWH with mechanical prophylaxis vs. combination of UFH with mechanical prophylaxis (I2 = 0 %; p = 0.84); the third group represents the combination of LMWH with mechanical prophylaxis vs. mechanical prophylaxis alone (I2 = 0 %; p = 0.57); the fourth group represents mechanical prophylaxis vs. placebo (I2 = 0 %; p = 0.54)
A multi-covariate meta-regression model adjusting for all the previous variables did not explain significant between-study variance (overall p = 0.38). A symmetrical inverted funnel plot suggested the absence of publication bias along the efficacy analysis (Fig. 4). Both Begg’s rank correlation test (p = 0.93) and Egger’s linear regression test (p = 0.94) indicated no publication bias. The one-study removal sensitivity analysis did not change the summary estimate. The cumulative meta-analysis showed that the efficacy of the intervention was shown as early as 1978 and remained consistent until the latest study in 2003 (Fig. 5).
Efficacy funnel plot of log risk ratio according to their standard errors using the fixed-effect model. The vertical solid line is drawn at the pooled log risk ratio, and the other two lines represent the expected 95 % confidence interval for a given standard error. The plot shows no significant publication bias
Cumulative efficacy of controlled trials of different prophylactic regimens among brain tumor patients undergoing craniotomy, fixed-effect model. The data corresponds to Fig. 2. A statistically significant beneficial effect on venous thromboembolism risk became evident in 1978
Safety analysis
Only five studies were included in the safety analysis as data pertaining to the occurrence of hemorrhage or bleeding was lacking from the remaining five studies [3–6, 9], of which only four discerned major [3, 4] from minor [4–6] bleeding. None of the five studies showed a significant increased risk of combined major/minor hemorrhagic events in the intervention group; however, pooling these study results demonstrated a significant effect between the different prophylaxis regimens and combined major/minor hemorrhagic events risk (Fig. 6). This increased risk seemed to be mostly driven by minor hemmorhages (RR = 2.20; 95 % CI = 1.00; 4.85) as the pooled OR for major hemmorhages was not significant (RR = 1.20; 95 % CI = 0.36; 3.95). The pooled RR of adverse events was 2.02 (95 % CI: 1.14; 3.58; fixed-effect model). Results from the random-effects model were similar (RR = 2.02; 95 % CI: 1.14; 3.58) and no significant heterogeneity was observed (I2 = 0 %; P-heterogeneity = 0.86).
Forest plot represents the relative risk for developing complications (95 % CI) with different prophylactic regimens as compared to different control regimens from five randomized controlled studies in adult brain tumor patients undergoing craniotomy. Horizontal lines denote 95 % CIs, solid squares represent the point estimate of each study and the diamond represents the pooled estimate of the intervention effect. The size of the solid squares is proportional to the weight of the study. Weights are from the fixed-effect analysis using the using the inverse variance method. The I2 and p values for heterogeneity are shown
Subgroup analyses provided no evidence that the pooled effects varied by group for either intervention type (p = 0.96), intervention time (p = 0.90), follow-up duration (p = 0.96), study quality (p = 0.35), center (p = 0.90), or country (p = 0.40). Both the univariate meta-regression analyses on age and on each of these covariates separately (all p values >0.05) and the multi-variate meta-regression (simultaneously adjusting for study quality and center; overall p = 0.58) did not explain significant between-study variance. Although the funnel plot did not give clear results owing to the limited number of safety studies (n = 5) (not shown), both Begg’s rank correlation test (p = 0.46) and Egger’s linear regression test (p = 0.42) indicated no publication bias. The one-study removal sensitivity analysis did not change the summary estimate. The cumulative meta-analysis showed that the efficacy of the intervention was shown as early as 1998 and remained consistent until the latest study in 2003. All of the above-mentioned results did not materially change with the random-effects model (not shown) or when using Peto odds ratio (not shown), except when otherwise indicated.
Discussion
Upon meta-analysis, a statistically significant decrease in VTE events with prophylaxis was found. Subgroup analysis suggested that intervention type is an effect modifier of this risk reduction. Among the studies included, UFH alone showed a stronger reduction in VTE events than placebo, followed by LMWH and mechanical prophylaxis combined, which showed a lower VTE risk than mechanical prophylaxis alone. These findings suggest that chemoprophylaxis for VTE is effective and can successfully reduce the incidence of VTE in patients undergoing craniotomy for brain tumor.
Pooled analysis also demonstrated a statistically significant increase in hemorrhagic events among patients receiving prophylaxis, although only five studies were included in this analysis. While there was a statistically significant increase in hemorrhagic events, this was driven by minor, and not major, bleeding, although only two studies reported major bleeding [3, 4]. These findings correlate with the efficacy analysis and characterize the dilemma inherent in prophylaxis for patients undergoing tumor resection: the more effective the intervention (due to its mechanism of action), the higher the chance of adverse events such as minor hemorrhage. Nevertheless, only five studies published data regarding safety of intervention, and only four of these discerned major from minor bleeding; thus, this topic would benefit from further studies.
Patients undergoing surgery of any type have repeatedly been shown to be at an increased risk of VTE, which is classically explained by Virchow’s triad of hemodynamic changes, endothelial injury, and hypercoaguability [22–27]. Relative stasis post-operatively can result in procoagulative hemodynamic changes in the venous circulation, while direct tissue violation intraoperatively increases the risk of coagulation in general [28, 29]. Some tumors, such as glioblastoma multiforme, have also been shown to exert direct hypercoagulative effects through the secretion of circulating tissue factor [30, 31].
Similarly, patients undergoing craniotomy for brain tumor are considered to be at high risk for VTE, due to both the above-mentioned factors and particularly prolonged stasis as a result of long durations of general anesthesia and longer hospital stays [11, 28, 32–34]. In clinical decision making, however, these risks must be weighed against the risks of adverse events from anticoagulation, including postoperative hemorrhage. In the case of patients undergoing resection of brain tumor, the complications of hemorrhage into the tumor bed can be particularly severe, and can include permanent neurological deficit, stroke, or death [35–38]. In all cases, regardless of the findings of RCTs or meta-analyses, post-operative anticoagulation must be individualized to the patient. Nevertheless, high quality data in the form of meta-analyses regarding the relative efficacy and safety of a treatment modality across entire populations, such as post-operative anticoagulation, can help drive effective clinical practice.
To evaluate the safety and efficacy of various anticoagulation methods typically used for patients undergoing craniotomy, numerous investigators have undertaken randomized clinical trials [3, 5, 9, 16, 17, 21, 39–42]. These clinical trials have variably compared different forms of mechanical prophylaxis (e.g., stockings, SCD) and chemical prophylaxis (e.g., LMWH, UFH) against different controls.
Our specific aim was to advance the understanding of VTE prophylaxis after craniotomy for brain tumor, in terms of both efficacy and safety, by pooling together the results of these studies in a meta-analysis. Although some studies have demonstrated the efficacy of prophylaxis, others have shown no statistical difference between the tested prophylaxis modalities and controls [2, 3, 5, 9, 21, 43]. Additionally, none of the studies included in this analysis reported an increased risk of adverse events with prophylaxis. By pooling these studies together, we hoped to increase the power of the analysis, potentially discovering new findings that could inform clinical decision making surrounding the complex and nuanced issue of VTE prophylaxis in patients undergoing craniotomy for brain tumors. Interestingly, the most recent study included in this analysis was published in 2003, demonstrating a need for more up-to-date recommendations on VTE prophylaxis that we believed could be generated by detailed meta-analysis of the highest quality studies available.
Previous meta-analyses in the neurosurgical literature on VTE development and prophylaxis are relatively limited. In 2008, Collen et al. reported the results of a comprehensive meta-analysis analyzing VTE prophylaxis in all neurosurgical patients [43]. The results of their study suggested that patients undergoing craniotomy for intracranial neoplasms may be at higher risk for VTE development, and would therefore benefit from combined therapy, a finding corroborated by the data presented here. The RR of VTE development in patients receiving prophylaxis reported in their study was similar to that reported here (0.60, 95 % CI: 0.44–0.81 vs. 0.61, 95 % CI: 0.47–0.79). This prior study was limited in that it reported higher rates of heterogeneity than those reported here, likely due to the inclusion of both RCTs and cohort studies, and did not stratify into detailed subgroup analyses by other covariates. Third, the high heterogeneity in the previous meta-analysis could be attributed to the inclusion of both RCTs and cohort studies as well as the inclusion of all neurosurgery patients; both of these issues were amended in our meta-analysis in which only RCTs including brain tumor patients undergoing craniotomy were included.
Limitations of our study include the inherent limitations of a meta-analysis, most importantly a dependence on the quality of studies pooled for analysis. In an effort to combine only the highest quality evidence, we elected to include only RCTs in this meta-analysis, excluding all cohort studies. The relatively low heterogeneity of the included studies and the lack of evidence of publication bias both support the findings of this meta-analysis. No meta-analytic conclusion could be drawn regarding the best administration time or type of the prophylaxis with respect to major bleeding, however, owing to the lack of information included in the studies analyzed. Missing data that would have been relevant in this analysis included the histologic type of tumors being treated, whether patients were undergoing index or repeat craniotomy, and the location and type of hemorrhage post-operatively. The first two of these may affect the risk of VTE post-operatively, while the latter would affect the relative safety of chemoprophylaxis in the post-operative period.
Conclusion
This meta-analysis demonstrates a statistically significant VTE risk reduction among brain tumor patients receiving prophylaxis, with chemical prophylaxis showing the strongest risk reduction. Interventions in these studies were associated with an increased risk of post-operative minor hemorrhage.
References
Cerrato D, Ariano C, Fiacchino F (1978) Deep vein thrombosis and low-dose heparin prophylaxis in neurosurgical patients. J Neurosurg 49:378–381. doi:10.3171/jns.1978.49.3.0378
Dickinson LD, Miller LD, Patel CP, Gupta SK (1998) Enoxaparin increases the incidence of postoperative intracranial hemorrhage when initiated preoperatively for deep venous thrombosis prophylaxis in patients with brain tumors. Neurosurgery 43:1074–1081
Goldhaber SZ, Dunn K, Gerhard-Herman M, Park JK, Black PM (2002) Low rate of venous thromboembolism after craniotomy for brain tumor using multimodality prophylaxis. Chest 122:1933–1937
Agnelli G, Piovella F, Buoncristiani P, Severi P, Pini M, D’Angelo A, Beltrametti C, Damiani M, Andrioli GC, Pugliese R, Iorio A, Brambilla G (1998) Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med 339:80–85. doi:10.1056/NEJM199807093390204
Constantini S, Kanner A, Friedman A, Shoshan Y, Israel Z, Ashkenazi E, Gertel M, Even A, Shevach Y, Shalit M, Umansky F, Rappaport ZH (2001) Safety of perioperative minidose heparin in patients undergoing brain tumor surgery: a prospective, randomized, double-blind study. J Neurosurg 94:918–921
Macdonald RL, Amidei C, Baron J, Weir B, Brown F, Erickson RK, Hekmatpanah J, Frim D (2003) Randomized, pilot study of intermittent pneumatic compression devices plus dalteparin versus intermittent pneumatic compression devices plus heparin for prevention of venous thromboembolism in patients undergoing craniotomy. Surg Neurol 59:363–372
Perry JR, Julian JA, Laperriere NJ, Geerts W, Agnelli G, Rogers LR, Malkin MG, Sawaya R, Baker R, Falanga A, Parpia S, Finch T, Levine MN (2010) PRODIGE: a randomized placebo-controlled trial of dalteparin low-molecular-weight heparin thromboprophylaxis in patients with newly diagnosed malignant glioma. J Thromb Haemost 8:1959–1965. doi:10.1111/j.1538-7836.2010.03973.x
Auguste KI, Quinones-Hinojosa A, Berger MS (2004) Efficacy of mechanical prophylaxis for venous thromboembolism in patients with brain tumors. Neurosurg Focus 17:E3
Nurmohamed MT, van Riel AM, Henkens CM, Koopman MM, Que GT, d’Azemar P, Buller HR, ten Cate JW, Hoek JA, van der Meer J, van der Heul C, Turpie AG, Haley S, Sicurella A, Gent M (1996) Low molecular weight heparin and compression stockings in the prevention of venous thromboembolism in neurosurgery. Thromb Haemost 75:233–238
Salmaggi A, Simonetti G, Trevisan E, Beecher D, Carapella CM, DiMeco F, Conti L, Pace A, Filippini G (2013) Perioperative thromboprophylaxis in patients with craniotomy for brain tumours: a systematic review. J Neurooncol 113:293–303. doi:10.1007/s11060-013-1115-5
Guyatt GH, Norris SL, Schulman S, Hirsh J, Eckman MH, Akl EA, Crowther M, Vandvik PO, Eikelboom JW, McDonagh MS, Lewis SZ, Gutterman DD, Cook DJ, Schunemann HJ (2012) Methodology for the development of antithrombotic therapy and prevention of thrombosis guidelines: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141:53S–70S doi:10.1378/chest.11-2288
Treasure T, Hill J (2010) NICE guidance on reducing the risk of venous thromboembolism in patients admitted to hospital. J R Soc Med 103:210–212. doi:10.1258/jrsm.2010.100086
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188 pii]
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. doi:10.1136/bmj.327.7414.557327/7414/557
Bradburn MJ, Deeks JJ, Berlin JA, Russell Localio A (2007) Much ado about nothing: a comparison of the performance of meta-analytical methods with rare events. Stat Med 26:53–77 doi:10.1002/sim.2528
Turpie AG, Gallus A, Beattie WS, Hirsh J (1977) Prevention of venous thrombosis in patients with intracranial disease by intermittent pneumatic compression of the calf. Neurology 27:435–438
Skillman JJ, Collins RE, Coe NP, Goldstein BS, Shapiro RM, Zervas NT, Bettmann MA, Salzman EW (1978) Prevention of deep vein thrombosis in neurosurgical patients: a controlled, randomized trial of external pneumatic compression boots. Surgery 83:354–358
Bucci MN, Papadopoulos SM, Chen JC, Campbell JA, Hoff JT (1989) Mechanical prophylaxis of venous thrombosis in patients undergoing craniotomy: a randomized trial. Surg Neurol 32:285–288
Cerrato D, Ariano C, Fiacchino F (1978) Deep vein thrombosis and low-dose heparin prophylaxis in neurosurgical patients. J Neurosurg 49:378–381
Macdonald RL, Amidei C, Baron J, Weir B, Brown F, Erickson RK, Hekmatpanah J, Frim D (2003) Randomized, pilot study of intermittent pneumatic compression devices plus dalteparin versus intermittent pneumatic compression devices plus heparin for prevention of venous thromboembolism in patients undergoing craniotomy. Surg Neurol 59:363–372 (discussion 372–364)
Agnelli G, Piovella F, Buoncristiani P, Severi P, Pini M, D’Angelo A, Beltrametti C, Damiani M, Andrioli GC, Pugliese R, Iorio A, Brambilla G (1998) Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med 339:80–85
Brandes AA, Scelzi E, Salmistraro G, Ermani M, Carollo C, Berti F, Zampieri P, Baiocchi C, Fiorentino MV (1997) Incidence of risk of thromboembolism during treatment high-grade gliomas: a prospective study. Eur J Cancer 33:1592–1596
Marras LC, Geerts WH, Perry JR (2000) The risk of venous thromboembolism is increased throughout the course of malignant glioma: an evidence-based review. Cancer 89:640–646. doi:10.1002/1097-0142(20000801)89:3<640::AID-CNCR20>3.0.CO;2-E
Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA (2000) Prognosis of cancers associated with venous thromboembolism. N Engl J Med 343:1846–1850. doi:10.1056/NEJM200012213432504
Knovich MA, Lesser GJ (2004) The management of thromboembolic disease in patients with central nervous system malignancies. Curr Treat Options Oncol 5:511–517
Alcalay A, Wun T, Khatri V, Chew HK, Harvey D, Zhou H, White RH (2006) Venous thromboembolism in patients with colorectal cancer: incidence and effect on survival. J Clin Oncol 24: 1112–1118. doi:10.1200/JCO.2005.04.2150
Spyropoulos AC, Brotman DJ, Amin AN, Deitelzweig SB, Jaffer AK, McKean SC (2008) Prevention of venous thromboembolism in the cancer surgery patient. Cleve Clin J Med 75(Suppl 3):S17–S26
Smith TR, Nanney AD 3rd, Lall RR, Graham RB, McClendon J Jr, Lall RR, Adel JG, Zakarija A, Cote DJ, Chandler JP (2015) Development of venous thromboembolism (VTE) in patients undergoing surgery for brain tumors: results from a single center over a 10 year period. J Clin Neurosci 22:519–525. doi:10.1016/j.jocn.2014.10.003
Cote DJ, Smith TR (2016) Venous thromboembolism in brain tumor patients. J Clin Neurosci 25:13–18. doi:10.1016/j.jocn.2015.05.053
Sartori MT, Della Puppa A, Ballin A, Saggiorato G, Bernardi D, Padoan A, Scienza R, d’Avella D, Cella G (2011) Prothrombotic state in glioblastoma multiforme: an evaluation of the procoagulant activity of circulating microparticles. J Neurooncol 104:225–231. doi:10.1007/s11060-010-0462-8
Perry JR (2012) Thromboembolic disease in patients with high-grade glioma. Neuro-oncol 14(Suppl 4):iv73–i80. doi:10.1093/neuonc/nos197
Macdonald RL, Amidei C, Lin G, Munshi I, Baron J, Weir BK, Brown F, Erickson RK, Hekmatpanah J (1999) Safety of perioperative subcutaneous heparin for prophylaxis of venous thromboembolism in patients undergoing craniotomy. Neurosurgery 45:245–251 (discussion 251–242)
Danish SF, Burnett MG, Ong JG, Sonnad SS, Maloney-Wilensky E, Stein SC (2005) Prophylaxis for deep venous thrombosis in craniotomy patients: a decision analysis. Neurosurgery 56:1286–1292 (discussion 1292–1284)
Smith TR, Lall RR, Graham RB, McClendon J Jr, Lall RR, Nanney AD, Adel JG, Zakarija A, Chandler JP (2014) Venous thromboembolism in high grade glioma among surgical patients: results from a single center over a 10 year period. J Neurooncol. doi:10.1007/s11060-014-1557-4
Browd SR, Ragel BT, Davis GE, Scott AM, Skalabrin EJ, Couldwell WT (2004) Prophylaxis for deep venous thrombosis in neurosurgery: a review of the literature. Neurosurg Focus 17:E1
Epstein NE (2005) A review of the risks and benefits of differing prophylaxis regimens for the treatment of deep venous thrombosis and pulmonary embolism in neurosurgery. Surg Neurol 64:295–301 (discussion 302)
Tetri S, Hakala J, Juvela S, Saloheimo P, Pyhtinen J, Rusanen H, Savolainen ER, Hillbom M (2008) Safety of low-dose subcutaneous enoxaparin for the prevention of venous thromboembolism after primary intracerebral haemorrhage. Thromb Res 123:206–212. doi:10.1016/j.thromres.2008.01.018
Jenkins EO, Schiff D, Mackman N, Key NS (2010) Venous thromboembolism in malignant gliomas. J Thromb Haemost 8:221–227. doi:10.1111/j.1538-7836.2009.03690.x
Gruber UF, Rem J, Meisner C, Gratzl O (1984) Prevention of thromboembolic complications with miniheparin-dihydroergotamine in patients undergoing lumbar disc operations. Eur Arch Psychiatry Neurol Sci 234:157–161
Bostrom S, Holmgren E, Jonsson O, Lindberg S, Lindstrom B, Winso I, Zachrisson B (1986) Post-operative thromboembolism in neurosurgery. A study on the prophylactic effect of calf muscle stimulation plus dextran compared to low-dose heparin. Acta Neurochir (Wien) 80:83–89
Voth D, Schwarz M, Hahn K, Dei-Anang K, al Butmeh S, Wolf H (1992) Prevention of deep vein thrombosis in neurosurgical patients: a prospective double-blind comparison of two prophylactic regimen. Neurosurg Rev 15:289–294
Geerts WH, Jay RM, Code KI, Chen E, Szalai JP, Saibil EA, Hamilton PA (1996) A comparison of low-dose heparin with low-molecular-weight heparin as prophylaxis against venous thromboembolism after major trauma. N Engl J Med 335:701–707
Collen JF, Jackson JL, Shorr AF, Moores LK (2008) Prevention of venous thromboembolism in neurosurgery: a metaanalysis. Chest 134:237–249. doi:10.1378/chest.08-0023
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. This work has not been presented or published previously. The authors did not receive any financial support for this work.
Additional information
Nasser Alshehri and David J. Cote have contributed equally as first authors. Timothy R. Smith and Rania A. Mekary have contributed equally as senior authors.
Rights and permissions
About this article
Cite this article
Alshehri, N., Cote, D.J., Hulou, M.M. et al. Venous thromboembolism prophylaxis in brain tumor patients undergoing craniotomy: a meta-analysis. J Neurooncol 130, 561–570 (2016). https://doi.org/10.1007/s11060-016-2259-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-016-2259-x