Abstract
Background
Natural products are considered effective sources for new therapeutic research and development. The numerous therapeutic properties of natural substances in traditional medicine compel us to investigate the anti-cancer properties of Nimbin (N1) and its semi-natural analog Nimbic acid (N3) from Azadirachta indica against MG-63 Osteosarcoma cells.
Materials and methods
The therapeutic efficacy of N1 and N3 were screened for their toxicity and cytotoxic activity using L6 myotubes, zebrafish larvae and MG-63 osteosarcoma cells. The mitochondrial membrane potential was evaluated using the Rhodamine 123 stain. Further, the nuclear and cellular damage was distinguished using Hoechst and Acridine orange/EtBr stain. The mechanism of cell cycle progression, cellular proliferation and caspase cascade activation was screened using scratch assay, flow cytometry, and mRNA expression analysis.
Results
The Nimbin and analogue N3 were found to be non-toxic to normal L6 cells (Rat skeletal muscles), exhibited cytotoxicity in MG-63 cells, and were exposed to be an active inhibitor of cell proliferation and migration. Analogs N1 and N3 induced negative mitochondrial membrane potential when stained with Rhodamine 123, leading to nuclear damage and apoptosis stimulation using AO/EtBr and Hoechst. Further, N1 and N3 induced cell cycle arrest in G0/G1 phase in flow cytometry using PI staining and induced apoptosis by activating the caspase cascade and upregulated Caspase 3 and caspase 9.
Conclusion
The study demonstrated cytotoxic activity against MG-63 osteosarcoma cells while being non-toxic to normal L6 cells. These compounds inhibited cell proliferation and migration, induced mitochondrial dysfunction, nuclear damage, and apoptosis stimulation. Furthermore, N1 and N3 caused cell cycle arrest and activated the caspase cascade, ultimately leading to apoptosis. These findings indicate that N1 and N3 hold promise as potential candidates used alone or combined with existing drugs for further investigation and development as anti-cancer agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer has recently escalated into a serious epidemic, necessitating a committed and coordinated response to counteract this menacing public health challenge [1] The resistance of cancer cells towards apoptosis poses a great challenge in treating different malignancies, and novel targeted therapeutics are in high demand. Osteosarcoma is the most frequent primary, non-hematopoietic malignant tumour of the skeletal system, which accounts for about 20% of the primary malignant bone tumours. In children and adults, Osteosarcoma is one of the most prevalent malignant-cancer of the bones and is reported to be an aggressive bone tumour that occurs more frequently in men than in women. With an annual incidence of 5.6 cases per million children under 15, Osteosarcoma ranks third among cancers that affect adolescents, behind only brain tumours and lymphomas. In the second decade of life, incidence peaks [2]. In children and adults, Osteosarcoma is one of the most prevalent malignant-cancer of the bones and is reported to be an aggressive bone tumour that occurs more frequently in men than in women. The tumour most commonly affects the growth plate in a metaphyseal area of the long bones, with most cases occurring in the distal femur and proximal febia [3]. Osteosarcoma patients are diagnosed with metastatic stage in the lungs as the common region where the tumour migrates. Surgery and cytotoxic chemotherapy, or a combination of both, are used to treat Osteosarcoma. Currently, cytotoxic chemotherapy is important in treating Osteosarcoma, with 20–70% curing rates.
Conversely, chemotherapy is associated with a plethora of side effects. Each drug, within every class, has its own set of adverse reactions, which may cause patients in compliance and deterioration of their quality of life [4, 5]. This paves the way for developing alternative chemotherapeutic medications, particularly those made from natural ingredients that are non-toxic to normal cells and inexpensive. Natural products can be effective anti-cancer drugs since many cytotoxic medications currently used in clinical practices are derived from plants [1, 6].
In recent years, few reports have highlighted the usefulness of small molecules from plants as therapeutic-chemical reservoirs for various disorders, including cancer [7]. A.Indica (neem) is a medicinal plant of Indian origin, which contains over 140 isolated small molecules and more than 35 physiological active principles that have been demonstrated to operate as tumour suppressors by interfering with carcinogenesis [8]. The small molecules present in Neem are known to have chemo-preventive, immune-modulatory, apoptotic, and induction of p53-independent apoptotic capabilities [7, 9]. In our earlier study, we isolated Nimbin (N1) from neem kernels and semi-synthetically modified it to derivatives N2 (De-acetylated Nimbin) and N3 (Nimbic acid). And further explored its biological activities in discovering patterns [10]. However, the efficacy of N1 and N3 is still unknown. The study aimed to evaluate the therapeutic efficacy and potential anti-cancer properties of compounds N1 and N3. By assessing their toxicity, cytotoxic activity, mitochondrial membrane potential, cellular damage, and effects on cell cycle progression and apoptosis, the study aimed to provide insights into the potential use of N1 and N3 as anti-cancer agents.
Materials and methods
Synthesis of N1 and N3
Nimbin (N1) was isolated from neem seed kernels and was semi-naturally modified to analog (N3). The characterization of N1 and N3 has been published elsewhere [10].
Culture and maintenance of zebrafish
Adult zebrafish (Danio rerio) were procured from a commercial dealer, NSK Aquarium, in Kolathur, Tamil Nadu, India. The fish were housed in a 3 L glass tank, maintained at a controlled water temperature of 28.5 °C, and subjected to a 14/10 h light/dark cycle. The Zebrafish were fed a diet of live Artemia salina (brine shrimp) thrice daily. Following a one-month acclimatization period, the fish were selectively bred to obtain viable embryos. In a designated spawning tank, a male-to-female ratio of 2:1 was maintained, and a mesh partition was utilized at the tank’s bottom to prevent adult fish from consuming the laid eggs. The spawning process was initiated at the beginning of the light cycle, and the resulting eggs were collected after a 30-minute interval. Subsequently, the collected embryos were incubated at 26 ± 1 °C within a 12-well plate. Microscopic examination was performed to identify and select fertilized embryos displaying normal morphology for subsequent experimental procedures.
Culture and maintenance of L6 myotubes and MG-63 cells
The Rat skeletal muscles (L6 myotubes) and human osteosarcoma cells (MG-63) (Passage number: 14) were obtained from National Centre for Cell Science (NCCS), Pune. The cells are grown in a DMEM medium with high glucose (4.5 g/L), 10% FBS, and an antibiotic-antimycotic solution (10,000 U/L penicillin/streptomycin). The cells were maintained at 37 °C in an incubator with 5% CO2 [11, 12].
Evaluation of cytotoxicity in L6 myotubes using (4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)
The MTT assay was carried out using a method described earlier (Issac et al., 2020). The L6 and MG-63 cells (1 × 104) were cultured in a 96-well plate at 37 °C in a CO2 incubator with a 5% CO2 supply. N1 and N3 were treated with varying concentrations (25, 50 and 100 µM) after achieving the desired confluence (n = 3 well/group). Following treatment, 20 µL of MTT solution (5 mg/mL in sterile PBS) was added and incubated (4 h). 200 µL of DMSO (0.01%) was added to disolve the formazan crystals, and the absorbance was measured at 570 nm using a microplate reader. Using GraphPad Prism software, the anti-cancer activity was calculated by computing the IC50 value (the concentration that induced 50% cell death) from the data acquired from the inhibition rate [13, 14].
Developmental toxicity study using the zebrafish embryo
The toxicity of N1 and N3 were tested on a developing zebrafish embryo 4 h post-fertilization (hpf). The zebrafish embryos were randomly segregated on a 6-well plate and treated with N1 and N3 at varying concentrations (25 µM, 50 µM, and 100 µM). The untreated embryos were a control group, and the results were compared to the control group. The heart rate was calculated by counting the beats per minute (bpm) through the microscope. The larvae without the treatment were used as a control. The embryos were inspected between 4 hpf and 72 hpf for morphological abnormalities. Zebrafish used for the experiments were approved by the Institutional Animal Care and Use Committee of SRMIST (No. SAF/IAEC/211,215/004).
Cytomorphological evaluation
The cytomorphological alterations of MG-63 cells treated with N1 and N3 were assessed using the microscopic examination according to a previously described method (Pan et al. 2016). The MG-63 cells were seeded in a 6-well plate to achieve the necessary concentration. The cells were then treated with N1 and N3 at the following concentrations for 24 h: 25 µM, 50 µM, and 100 µM. The Photomicrographs were taken using an inverted microscope post-treatment.
Mitochondrial membrane potential stained using rhodamine,123
The mitochondrial membrane potential of N1 and N3 were determined using a method published earlier with minor modifications [15, 16]. In brief, the MG-63 cells were exposed to N1 and N3 at various concentrations for 12 h. After treatment, the cells were stained for 30 min in the dark with rhodamine 123 dye at a concentration of 10 µg/mL. The excess stain was washed away with PBS, and the results were observed under a fluorescence microscope (CoolSNAP Pro, Olympus, Tokyo, Japan) for quantitative estimation using ImageJ software (Ver 1.49, NIH, USA).
Mitochondrial membrane potential induced Apoptosis by N1 and N3 using Hoechst staining/ Acridine Orange (AO)/ Ethidium Bromide (EtBr)
The potency of N1 and N3 in inducing apoptotic cell death was investigated through Hoechst 33,342 staining assay. In brief, 1 × 106 MG-63 cells were seeded in a six-well plate, and the cells were then treated with N1 and N3 at various concentrations. The cells were washed with PBS, stained with Hoechst 33,342 (10 mg/mL) for 10 min, and incubated in the dark. The apoptotic bodies were observed under a fluorescence microscope [17].
The morphological figures of Apoptosis in MG-63 cells were further studied using the AO/EtBr dye. A concentration of 1 × 106 MG-63 cells was initially grown in T25 culture flasks and then treated with N1 and N3 at different concentrations. The untreated cells served as a negative control, while the positive control was cells treated with 100 µM Doxorubicin. After 12 h of incubation at 37 °C in 5% CO2, treated and untreated cells were centrifuged at 1800 rpm for 5 min. After removing the supernatant, the pellet cells were washed with phosphate-buffered saline (PBS). The pellet cells were then suspended in a 1:1 AO/EtBr mixture at 10 µg/mL concentration. Cell morphological changes were evaluated using a fluorescent microscope [4].
Cell cycle analysis
The cell cycle analysis was carried out at a concentration of 100 µM, which was shown to be optimal. In a 6-well plate, cells were cultivated overnight at a density of 1 × 106 cells/well and treated with 100 µM of N1 and N3 for 12 h. The cells were washed twice in PBS after being fixed in 100% ice-cold ethanol overnight at 4 °C. The cells were resuspended in a cold PI solution for 10 min in the dark, and then flow cytometry was performed at 617 nm in a BD-Facs caliber using Max quest pro software [18].
Cell migration assay
A cell migration assay was performed to investigate further the effects of N1 and N3 on directional cell migration on MG-63 cells. In a 6-well plate, 1 × 106 cells were cultivated for 24 h at 37 °C. A straight scratch was formed in each well on the confluent cell monolayer with a 10 µl pipette tip. To eliminate the floating cells, fresh medium was added, and the remaining cells were imaged instantly (at 0 h). Except for the control, the media was removed and replaced with new media containing N1 and N3. Images were taken after a 12-hour incubation at 37 °C, and migratory cell ability was detected [4, 19].
mRNA expression
The MG-63 cells were cultured on a 6-well plate and treated with 100 µM N1 and N3 for 24 h, with untreated cells as a control. The obtained total RNA was transformed into cDNA and employed as a template for the gene expression investigation using the standard TRIZOL procedure. For RT-PCR analysis and additional reaction buffer, the KAPA SYBR Quick qPCR Master Mix was utilized. A standardized thermal profile was used to run the cycle. The internal control (β-actin) was used to standardize the experimental results. The relative fold change was then calculated using the 2 − ΔΔct method, yielding the ct value [20,21,22].
Statistical significance
The data included in this investigation is the ± standard deviation of the average spanning three replicates. Graph Pad Prism’s (Ver.5.0) one-way ANOVA followed by Dunnet’s multiple comparison Test were used to assess the statistical significance of each experiment carried out for this study.
Results
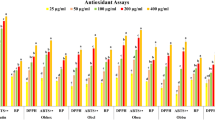
Nimbin is thought to be responsible for the biological activities of Neem oil. In discovering patterns, we semi-synthetically modified Nimbin (N1) to derivatives N2 and N3. N1, N2 and N3 exhibited higher antioxidant and anti-inflammatory properties. In this study, we intend to explore the anti-cancer potential of N1 and N3 towards MG-63 Osteosarcoma cells.
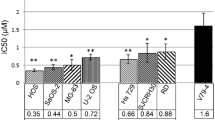
Cell viability and cytotoxicity in MG-63 cells
The formazan produced in Culture is proportional to the number of live cells present, while MTT assesses cell respiration. The amount of formazan produced changes in tandem with changes in cell number, showing the level of cytotoxicity induced by the drug. Initially, the toxicity of N1 and N3 was screened using L6 cells. The results revealed that N1 and N3 were not toxic up to 100 µM, whereas, at a concentration of 150 µM, mild toxicity was observed (Fig. 1A). From the MTT results, a significant property of N1 and N3 was observed; its specificity to target the cancer cells and not the normal cells. Further, the cytotoxic effects of N1 and N3 were screened using MG-63 cells. A dose-dependent decrease in the viability of the cells was observed. At a concentration of 25 µM, 65% of the cells remained viable. Similarly, at a concentration of 50 µM, 44% of the cells were viable at 100 µM, and 32% were viable. Interestingly, these viability rates were comparable to the positive control, where cells treated with 100 µM Doxorubicin showed 22% viability. (Fig. 1B). The IC50 values were calculated to be 48.8 µM for N1 and 52 µM for N3 for 24 h exposure.
A Cell viability of N1 and N3 by MTT assay in L6 myotubes cells in exposure to various concentrations for 24 h. Values are mean ± SD of three independent experiments. * indicates the significance level at p < 0.05 compared to the respective positive control. B Cell viability of N1 and N3 by MTT assay in MG-63 Osteosarcoma cells in exposure to various concentrations for 24 h. Values are mean ± SD of three independent experiments. * indicates the significance level at p < 0.05 compared to the respective positive control. C Effect of N1 on development toxicity and heart rate in zebrafish larvae. The treatment showed no significant effect on the developing larvae. Experiments were performed in triplicate, and the data were expressed as mean ± SD.D Effect of N3 on development toxicity and heart rate in zebrafish larvae. The treatment showed no significant effect on the developing larvae. Experiments were performed in triplicate, and the data were expressed as mean ± SD.
N1 and N3 induced no developmental toxicity in zebrafish
The zebrafish embryos exposed to N1 and N3 in varying concentrations resulted in no significant changes in the development of the zebrafish larvae. No structural deformities were observed during (0 hpf- 72 hpf). The N1 and N3 intervention groups observed no significant heart rate reduction. Therefore, N1 and N3 are non-toxic to the zebrafish embryos (Fig. 1C, D).
N1 and N3 induce cytomorphological changes
Exposure to N1 and N3 resulted in significant alterations in the cell morphology of MG-63 cells. Under the phase-contrast inverted microscope, the cells depicted in (Fig. 2A) showed that N1 and N3 reduced cell viability in a dose-dependent manner that was apparent from MTT data. Apoptosis-related alterations in cell morphology, such as granulation and cell rounding, were observed.
A Cytomorphological analysis of cell viability of N1 and N3 in MG-63 Osteosarcoma cells in exposure to various concentrations for 24 h. The treatment indicated a dose-dependent inhibition of cell proliferation and migration compared to the control. B Effect of N1 and N3 in migration of MG-63 Osteosarcoma cells in exposure to N1 and N3 for 12 h. The treatment indicated a dose-dependent inhibition of cell proliferation and migration compared to the control
Effect of N1 and N3 on MG-63 cell migration
A wound-healing assay was performed to evaluate the effect of N1 and N3 on MG-63 cells for cell migration. After incubating the physically wounded cells for 24 h, a high number of cells in migration was observed in the control group. In contrast, N1 and N3 inhibited the migration of cells in a dose-dependent manner significant to the control group (Fig. 2B).
N1 and N3 induce mitochondrial membrane potential damage
The effect of the mitochondrial membrane potential of N1 and N3 was evaluated on MG-63 cells. The mitochondrial membrane potential is crucial for energy storage in oxidative phosphorylation in healthy cells. The mitochondrial membrane potential was evaluated using Rhodamine123, which stained the negative membrane potential across the inner mitochondrial membrane. Changes in the mitochondrial membrane and release of cellular components into the cytoplasm were observed depending on the concentration of N1 and N3. Depolarisation of the mitochondrial membrane, with a swollen membrane and transcalent matrix, was observed in the treatment group. The control group had a clear mitochondrial matrix, whereas the mitochondrial cristae were significantly reduced in the treatment group. N1 and N3 exhibited a dose-dependent increase of high potential indicated by high fluorescent intensity similar to the 100 µM Doxorubicin group compared to the control group (Fig. 3A and B).
A. Effect of N1 and N3 (B) on mitochondrial membrane potential in MG-63 Osteosarcoma cells stained using Rhodamine 123 in exposure to various concentrations for a time period of 12 h. Changes in the mitochondrial membrane potential depending upon the concentration of N1 and N3 were observed. The treatment indicated a dose-dependent increase in activity compared to the control. C. The fluorescent intensity of the cells stained with Rhodamine 123 was quantified using ImageJ software. Experiments were performed in triplicate, and the data were expressed as mean ± SD. * represents the statistical significance at p < 0.05 compared to the control
Mitochondrial membrane potential induced apoptosis by AO/EtBr and Hoechst staining
The cytomorphological effects of N1 and N3 were examined using Hoechst staining. The control (untreated) cells were normal. In contrast, higher doses of N1 and N3 treatment (50 µM and 100 µM) caused apoptosis in a dose-dependent manner. The higher the concentration, the more apoptotic signs were detected, such as cytoplasmic haemorrhage, cytoplasmic vacuolation, nuclear swelling, chromatin fragmentation, multinucleation, and late apoptosis chromatin condensation were detected (Fig. 4A).
A Effect of N3 on apoptosis and nuclear damage stained using Hoechst staining in MG-63 Osteosarcoma cells in exposure to various concentrations for a time period of 12 h. The treatment indicated a dose-dependent increase in activity compared to the control. B Effect of N1 on cellular damage and apoptosis stained using Acridine Orange /Ethidium Bromide staining in MG-63 Osteosarcoma cells in exposure to various concentrations for a time period of 12 h. The treatment indicated a dose-dependent increase in activity compared to the control. C Effect of N3 on cellular damage and apoptosis stained using Acridine Orange /Ethidium Bromide staining in MG-63 Osteosarcoma cells in exposure to various concentrations for a time period of 12 h. The treatment indicated a dose-dependent increase in activity compared to the control. D Effect of N1 and N3 on Cell cycle analysis using PI staining in MG-63 Osteosarcoma cells in the exposure of 100µM N1 and N3 for a time period of 12 h
The mitochondrial membrane damage-induced apoptosis was investigated through AO/EtBr staining. The viable cells have taken the AO stain through cell penetration, and EtBr has stained dead cells. The control group has shown very few apoptotic cells (reddish yellow) compared to the Doxorubicin group, with high fluorescent intensity representing cell death. The N1 (Fig. 4B) and N3 (Fig. 4C) treatment groups showed a significant dose-dependent increase in cell death. The fluorescent intensity of the cells is directly proportional to the percentage of cell death.
Detection of cellular apoptosis and cell cycle arrest in MG-63 cells using flow cytometry
The cellular apoptosis was detected using PI staining in MG-63 cells evaluating the effect of N1 and N3 on inhibiting the cellular events for 24 h. From the results, it has been observed that the G1 phase was affected. The G1-phase arrest of cell cycle progression allows cells to undergo the apoptotic pathway. Compared to the control, a significant shift was observed in the sub-G1 phase (M1 in the histogram). Compared to 100 µM Doxorubicin, N1 and N3 at a concentration of 100 µM exhibited a shift difference at the sub G1 phase almost similar to 100 µM Doxorubicin. Therefore, the results show that N1 and N3 affect the Sub-G1 phase of the cell cycle in MG-63 cells, stimulating the induction of Apoptosis (Fig. 4D).
N1 and N3 activates Caspase3 and Caspase9 induced apoptosis
The apoptotic gene expression of N1 and N3 was evaluated using RT-PCR on apoptotic genes caspase3 and caspase9. The analogs N1 and N3 at a concentration of 100 µM significantly upregulated the apoptotic gene expression, indicating that N1 and N3 stimulate apoptosis, which supported the cellular apoptosis data evaluated using flow cytometry (Fig. 5).
Discussion
Osteosarcoma is one of the most prevalent bone malignancies in paediatric children. The death rate of metastatic Osteosarcoma remains unacceptably high despite surgery, chemotherapy, and radiotherapy improvements. For the past 20 years, the same treatment regimen has been used to treat this bone cancer and has several harmful side effects. A key tactic to enhance cancer treatment is the identification of novel natural substances that are efficient against cancers with resistance. Nature has been a great source of chemical diversity used to treat human sickness throughout history, from ancient to the present. Numerous compounds with anti-cancer capabilities have been found by studying natural products using modern scientific technologies [21, 23].
Nimbin from the neem family has been known to pose various biological activities [24]. In our previous report, we isolated Nimbin (N1) from neem seeds and semi-naturally modified them to analogs Deacetyl Nimbin (N2) and Nimbic acid (N3) and explored their antioxidant and anti-inflammatory properties [10]. Therefore, although there are multiple commercially accessible anti-cancer medications, specific studies demonstrating plant substances’ efficacy against cancer cells with inherent resistance have been difficult. In our present study, the therapeutic potential of N1 and N3 against skeletal malignancies was screened using MG-63 Osteosarcoma cells. Initially, the toxicity of N1 and N3 was screened using L6 cells. The results indicated that these compounds were not toxic at concentrations up to 100 µM. However, mild toxicity was observed at a higher concentration of 150 µM. This result also correlated with our previous report on N1 and N3 in MDCK cells [25]. This suggests that L6 cells are relatively resistant to the compounds, as they only exhibit toxicity at higher concentrations.
Further investigation is required to understand the mechanisms underlying this differential sensitivity. To investigate the cytotoxic effects on cancer cells, MG-63 cells were utilized. The viability of these cells decreased dose-dependent when exposed to N1 and N3. At 25 µM, 65% of the cells remained viable, indicating a moderate cytotoxic effect. Similarly, at 50 µM, viability decreased to 44%, and at 100 µM, viability further reduced to 32%. These viability rates were comparable to the positive control, where cells treated with 100 µM Doxorubicin, a known anti-cancer drug, showed 22% viability. These findings suggest that N1 and N3 have significant cytotoxic effects on MG-63 cancer cells. The calculated IC50 values were 48.8 µM for N1 and 52 µM for N3 after a 24-hour exposure period. These values represent the concentrations at which 50% of cell viability is inhibited. The relatively similar IC50 values indicate comparable potency between the two compounds, suggesting that they are similarly effective in inhibiting cell growth and survival in MG-63 cells.
Interestingly, the discussion mentions a unique property of N1 and N3: their specificity to target cancer cells rather than normal cells. This observation suggests a potential selectivity of the compounds towards cancer cells, which is a desirable characteristic for anti-cancer therapeutics. However, further investigations are needed to understand this specificity’s underlying mechanisms and determine if it holds across different cancer cell lines. The exposure of zebrafish embryos to varying concentrations of N1 and N3 did not result in significant changes in the development of the zebrafish larvae. No structural deformities were observed during the entire observation period from 0 h post-fertilization (hpf) to 72 hpf. This suggests that N1 and N3 did not cause major developmental abnormalities or overt toxicity in the zebrafish embryos. These findings indicate a relative safety profile of N1 and N3 regarding embryonic development in zebrafish.
Additionally, the intervention groups exposed to N1 and N3 showed no significant reduction in heart rate. This further supports the non-toxic nature of N1 and N3 in zebrafish embryos, as a decrease in heart rate often indicates cardiac toxicity. The absence of heart rate reduction suggests that N1 and N3 did not adversely affect the cardiovascular function of the zebrafish embryos. In contrast to the zebrafish embryo findings, exposure to N1 and N3 resulted in significant alterations in the cell morphology of MG-63 cells. Cellular morphology is impacted by damage to the cell membrane. Apoptosis is indicated by abnormal morphology, which includes granulation cell shrinkage. The N1 and N3 intervention groups showed signs of cell structural degradation, granulation, and shrinking. A dose-dependent increase in cell death was observed throughout 24 h.
Under the phase-contrast inverted microscope, the cells depicted in (Fig. 2A) showed that N1 and N3 reduced cell viability in a dose-dependent manner, as evident from the MTT assay data. This indicates that N1 and N3 have cytotoxic effects on MG-63 cells.
An intricate web of signalling pathways, including cytoskeleton-modifying proteins, motor proteins, small GTPases, and kinases, controls how quickly cells migrate. Targeting cancer cell migration has emerged as a therapeutically demanding strategy in recent years. In the control group, where no treatment was applied, many cells migrated into the wound area after 24 h of incubation. This is indicative of the normal migratory capacity of the MG-63 cells in the absence of any external factors. The observed migration in the control group serves as a baseline for comparison with the effects of N1 and N3 treatments.
In contrast to the control group, the application of N1 and N3 inhibited cell migration in a dose-dependent manner. As the concentration of N1 and N3 increased, the number of cells migrating into the wound area decreased significantly compared to the control group. The dose-dependent inhibition of cell migration suggests that N1 and N3 have an inhibitory effect on the migratory capacity of MG-63 cells. The significant inhibition of cell migration by N1 and N3 implies that these compounds may interfere with the cellular processes involved in migration, such as cytoskeletal rearrangements and cell signalling pathways. Cell migration involves coordinating various molecular mechanisms, including cell adhesion, cell polarization, and actin cytoskeleton dynamics. Disruption of any of these processes can impede cell migration. The observed inhibitory effect of N1 and N3 on cell migration aligns with the previous findings of cytotoxicity and apoptosis induction in MG-63 cells. It suggests that these compounds not only affect cell viability but also impact the functional behaviour of the cells, such as their ability to migrate and participate in wound healing processes. Impaired cell migration can be beneficial in certain contexts, such as inhibiting cancer cell metastasis or preventing excessive tissue scarring. The molecular mechanism of N1 and N3 on Apoptosis and cellular damage was further evaluated.
In the treatment group exposed to N1 and N3, changes in the mitochondrial membrane and release of cellular components into the cytoplasm were observed, depending on the concentration of the compounds. This suggests that N1 and N3 impact mitochondrial function and integrity. Specifically, depolarization of the mitochondrial membrane was observed in the treatment group. The depolarization was accompanied by a swollen membrane and a transcalent matrix, indicating disruption and dysfunction of the mitochondria. In contrast, the control group exhibited a clear mitochondrial matrix, indicating normal mitochondrial morphology.
Furthermore, the treatment group showed a significant reduction in mitochondrial cristae compared to the control group. Mitochondrial cristae are important for the efficient functioning of oxidative phosphorylation and ATP production. The reduced cristae suggest impairment of mitochondrial function in response to N1 and N3 treatment. Regarding the fluorescent intensity of Rhodamine123 staining, N1 and N3 exhibited a dose-dependent increase in high potential, as indicated by high fluorescent intensity. This suggests that N1 and N3 can cause a hyperpolarization of the mitochondrial membrane potential.
Interestingly, this effect was similar to that observed in the group treated with 100 µM Doxorubicin, a known mitochondrial disruptor and anti-cancer drug. The disruption of mitochondrial function can significantly affect cell viability and survival. An increase in mitochondrial membrane potential inhibits ATP synthase [26]. Mitochondria play a central role in energy production, and their dysfunction can lead to various cellular consequences, including impaired cellular metabolism and induction of cell death pathways.
The cytomorphological effects of N1 and N3 compounds were investigated using Hoechst staining, which allowed for the visualization of cellular changes at the nuclear level. The control cells, which were not treated, exhibited normal morphology. In contrast, when higher doses of N1 and N3 (50 µM and 100 µM) were administered, a dose-dependent induction of apoptosis was observed. Apoptosis, or programmed cell death, is a tightly regulated process essential for maintaining cellular homeostasis. In this study, the higher the concentration of N1 and N3, the greater the extent of apoptotic cell death, as indicated by several characteristic cytomorphological features. These features included cytoplasmic haemorrhage and cellular contents’ leakage into the cytoplasm due to compromised membrane integrity. Cytoplasmic vacuolation was also observed, forming fluid-filled vacuoles in the cytoplasm.
Nuclear swelling, which signifies cellular damage and disruption of nuclear architecture, was evident. Also, chromatin fragmentation was detected, characterized by the breakdown of DNA into smaller fragments. Multinucleation, multiple nuclei within a single cell, and late apoptosis chromatin condensation were also observed, indicating advanced stages of apoptosis [27]. To further investigate the mechanism of apoptosis induced by N1 and N3 compounds, mitochondrial membrane damage was assessed using AO/EtBr staining. This staining method distinguishes viable cells, which take up the AO stain through cell penetration and emit green fluorescence, from dead cells stained by EtBr and emitting reddish-yellow fluorescence. The control group exhibited minimal apoptotic cell death, as indicated by low fluorescent intensity.
In contrast, the Doxorubicin group, used as a positive control to induce apoptosis, showed a high fluorescent intensity, representing a significant amount of cell death. The N1 and N3 treatment groups demonstrated a notable dose-dependent increase in cell death, as evidenced by the increasing fluorescent intensity. This suggests that N1 and N3 compounds induce apoptosis, at least in part, through mitochondrial membrane damage. Mitochondria regulate apoptosis, releasing pro-apoptotic factors when their integrity is compromised. The observed increase in cell death suggests that N1 and N3 compounds may disrupt the mitochondrial membrane, activating apoptotic pathways. The effect of N1 and N3 compounds on cellular apoptosis was investigated in MG-63 cells by using PI staining and evaluating their impact on cell cycle progression over 24 h. The results indicated that the G1 phase of the cell cycle was affected by the treatment with N1 and N3 compounds. The G1 phase is a crucial stage in the cell cycle where cells prepare for DNA synthesis and subsequent cell division. Disruption of the G1 phase can lead to cell cycle arrest and trigger the apoptotic pathway. This study observed that the treatment with N1 and N3 compounds caused a significant shift in the sub-G1 phase, represented as M1 in the histogram analysis. The sub-G1 phase typically corresponds to cells with fragmented DNA, a characteristic feature of apoptotic cells. The increase in the sub-G1 population indicates that a higher percentage of cells treated with N1 and N3 underwent apoptotic cell death than the control group. This suggests that N1 and N3 compounds can induce apoptosis in MG-63 cells. Furthermore, comparing N1 and N3 at a concentration of 100 µM with 100 µM Doxorubicin, a known apoptosis-inducing agent, revealed a similar shift in the sub-G1 phase. This implies that N1 and N3 compounds exhibit comparable efficacy to Doxorubicin in inducing apoptosis in MG-63 cells.
N1 and N3 could have increased ROS production and diminished the mitochondrial membrane potential, which releases cytochrome c to the cytoplasm. The negative mitochondrial cytochrome c is a key signal for the induction of the intrinsic pathway of apoptosis. A class of cysteine proteases known as caspases play crucial roles in apoptosis. Caspase 9 participates in the intrinsic, in contrast. Caspase 8 participates in the extrinsic apoptotic pathway. Interacting with caspases 8 and 9, caspase 3 is essential for the execution phase of cell death. The gene expression results revealed N1 and N3 upregulated the Caspase activity [28]. Caspases are activated during the final stage of apoptosis, and understanding the mechanism by which cytotoxic drugs do this could be crucial for developing improved therapeutic interventions [29]. N1 and N3 were able to trigger the caspase activity of caspase 3 and caspase 9. Therefore, the activation of caspase activity revealed that N1 and N3 played a significant role in the signal transduction pathway. N1 and N3 could be potential small molecules among various bioactive molecules to induce apoptosis in Osteosarcoma (Fig. 6).
Effect of N1 and N3 in the pathophysiology of cell migration and proliferation of Osteosarcoma MG-63 cells. N1 and N3 induced negative mitochondrial membrane potential and triggered apoptosis via activation of caspase 3 and caspase 9 and cell cycle progression arrest in the G1 and sub-G1 phase of the cell cycle
Conclusion
When exposed to different concentrations, N1 and N3 exhibited anti-cancer activities in MG-63 Osteosarcoma cells; simultaneously, they were non-toxic to L6 myotubes. N1 and N3 inhibited Cell proliferation and migration in a dose-dependent manner and induced negative mitochondrial membrane potential-mediated apoptosis. The underlying mechanism was via the stimulation of apoptosis and cell cycle arrest in the G0/G1 phase. Further analysis revealed N1 and N3 induced apoptosis by stimulating the caspase cascade suggesting a potential chemotherapeutic molecule paving the way for further research towards in-vivo anti-cancer model and therapy.
Limitations
The findings revealed that N1 and N3 have anti-cancer properties. However, the study’s animal model is boundaries. The efficacy of N1 and N3 should be further evaluated in a higher mammalian model to be clinically relevant to humans.
Data Availability
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
References
Yi C, Li G, Wang W et al (2021) Disruption of yy1-ezh2 interaction using synthetic peptides inhibits breast cancer development. Cancers (Basel) 13:1–23. https://doi.org/10.3390/cancers13102402
Cooper G (1951) Bone cancer. Va Med Mon (1918) 78:654. https://doi.org/10.6004/jnccn.2013.0088
Mantyh P (2013) Bone cancer pain: causes, consequences, and therapeutic opportunities. Pain 154:S54–S62. https://doi.org/10.1016/j.pain.2013.07.044
Song X, Zhang Y, feng Wang X et al (2017) Casticin induces apoptosis and G0/G1 cell cycle arrest in gallbladder cancer cells. Cancer Cell Int 17:1–10. https://doi.org/10.1186/s12935-016-0377-3
Siddiqui MA, Alhadlaq HA, Ahmad J et al (2013) Copper Oxide Nanoparticles Induced Mitochondria mediated apoptosis in human Hepatocarcinoma cells. PLoS ONE 8:e69534. https://doi.org/10.1371/journal.pone.0069534
Chen Y, McAndrews KM, Kalluri R (2021) Clinical and therapeutic relevance of cancer-associated fibroblasts. Nat Rev Clin Oncol 18:792–804. https://doi.org/10.1038/s41571-021-00546-5
Alzohairy MA (2016) Therapeutics role of azadirachta indica (neem) and their active constituents in diseases prevention and treatment. Evidence-based Complement Altern Med. https://doi.org/10.1155/2016/7382506. 2016:
Moga MA, Bălan A, Anastasiu CV et al (2018) An overview on the anticancer activity of azadirachta indica (neem) in gynecological cancers. Int J Mol Sci 19. https://doi.org/10.3390/ijms19123898
Mogana R, Teng-Jin K, Wiart C (2013) The Medicinal timber Canarium patentinervium Miq. (Burseraceae Kunth.) Is an anti-inflammatory bioresource of dual inhibitors of cyclooxygenase (COX) and 5-Lipoxygenase (5-LOX). ISRN Biotechnol 2013:1–8. https://doi.org/10.5402/2013/986361
Sudhakaran G, Prathap P, Guru A et al (2022) Anti-inflammatory role demonstrated both in vitro and in vivo models using non‐steroidal tetranortriterpenoid, Nimbin (N1) and its analogues (N2 and N3) that alleviate the domestication of alternative medicine. Cell Biol Int 24:327–332. https://doi.org/10.1002/cbin.11769
Sharma V, Vijay J, Ganesh MR, Sundaramurthy A (2020) Multilayer capsules encapsulating nimbin and doxorubicin for cancer chemo-photothermal therapy. Int J Pharm 582:119350. https://doi.org/10.1016/j.ijpharm.2020.119350
Issac PK, Karan R, Guru A et al (2021) Insulin signaling pathway assessment by enhancing antioxidant activity due to morin using in vitro rat skeletal muscle L6 myotubes cells. Mol Biol Rep 48:5857–5872. https://doi.org/10.1007/s11033-021-06580-x
Zarandi PK, Mirakabadi AZ, Sotoodehnejadnematalahi F (2019) Cytotoxic and anticancer effects of ICD-85 (venom derived peptides) in human breast adenocarcinoma and normal human dermal fibroblasts. Iran J Pharm Res 18:232–240. https://doi.org/10.22037/ijpr.2019.2341
Yan CH, Li F, Ma YC (2015) Plumbagin shows anticancer activity in human osteosarcoma (MG-63) cells via the inhibition of s-phase checkpoints and down-regulation of c-myc. Int J Clin Exp Med 8:14432–14439
Liu W, Yang Y, Zhang J et al (2014) Effects of dietary microencapsulated sodium butyrate on growth, intestinal mucosal morphology, immune response and adhesive bacteria in juvenile common carp (Cyprinus carpio) pre-fed with or without oxidised oil. Br J Nutr 112:15–29. https://doi.org/10.1017/S0007114514000610
Velayutham M, Guru A, Gatasheh MK et al (2022) Molecular Docking of SA11, RF13 and DI14 peptides from Vacuolar Protein sorting Associated protein 26B against Cancer Proteins and in vitro investigation of its Anticancer Potency in Hep-2 cells. Int J Pept Res Ther 28. https://doi.org/10.1007/s10989-022-10395-0
Al-Dabbagh B, Elhaty IA, Al Hrout A et al (2018) Antioxidant and anticancer activities of Trigonella foenum-graecum, Cassia acutifolia and rhazya stricta. BMC Complement Altern Med 18:1–12. https://doi.org/10.1186/s12906-018-2285-7
Song J, Liu K, Yi J et al (2010) Luteolin inhibits Lysophosphatidylcholine-Induced apoptosis in endothelial cells by a Calcium/Mithocondrion/Caspases-Dependent pathway. Planta Med 76:433–438. https://doi.org/10.1055/s-0029-1186197
Umapathy E, Ndebia EJ, Meeme A et al (2010) An experimental evaluation of Albuca setosa aqueous extract on membrane stabilization, protein denaturation and white blood cell migration during acute inflammation. J Med Plants Res 4:789–795. https://doi.org/10.5897/JMPR10.056
Sarkar P, Stefi RV, Pasupuleti M et al (2020) Antioxidant molecular mechanism of adenosyl homocysteinase from cyanobacteria and its wound healing process in fibroblast cells. Mol Biol Rep 47:1821–1834. https://doi.org/10.1007/s11033-020-05276-y
Kazantseva L, Becerra J, Santos-Ruiz L (2022) Traditional Medicinal plants as a source of inspiration for Osteosarcoma Therapy. Molecules 27:5008. https://doi.org/10.3390/molecules27155008
Velayutham M, Haridevamuthu B, Priya PS et al (2022) Serine O-acetyltransferase derived NV14 peptide reduces cytotoxicity in H2O2 induced MDCK cells and inhibits MCF-7 cell proliferation through caspase gene expression. Mol Biol Rep 49:9205–9215. https://doi.org/10.1007/s11033-022-07746-x
Velayutham M, Sarkar P, Sudhakaran G et al (2022) Anti-cancer and anti-inflammatory activities of a short molecule, PS14 derived from the virulent cellulose binding domain of Aphanomyces invadans, on human laryngeal epithelial cells and an in vivo zebrafish embryo model. Molecules 27:7333. https://doi.org/10.3390/molecules27217333
Koriem KMM (2013) Review on pharmacological and toxicologyical effects of oleum azadirachti oil. Asian Pac J Trop Biomed 3:834–840. https://doi.org/10.1016/S2221-1691(13)60165-3
Sudhakaran G, Prathap P, Guru A et al (2022) Anti-inflammatory role demonstrated both in vitro and in vivo models using nonsteroidal tetranortriterpenoid, Nimbin (N1) and its analogs (N2 and N3) that alleviate the domestication of alternative medicine. Cell Biol Int 46:771–791. https://doi.org/10.1002/cbin.11769
Zorova LD, Popkov VA, Plotnikov EY et al (2018) Mitochondrial membrane potential. Anal Biochem 552:50–59. https://doi.org/10.1016/j.ab.2017.07.009
Velayutham M, Sarkar P, Karuppiah KM et al (2023) PS9, derived from an aquatic Fungus virulent protein, glycosyl hydrolase, arrests MCF-7 proliferation by regulating intracellular reactive oxygen species and apoptotic pathways. ACS Omega 8:18543–18553. https://doi.org/10.1021/acsomega.3c00336
Guru A, Lite C, Freddy AJ et al (2021) Intracellular ROS scavenging and antioxidant regulation of WL15 from cysteine and glycine-rich protein 2 demonstrated in zebrafish in vivo model. Dev Comp Immunol 114:103863. https://doi.org/10.1016/j.dci.2020.103863
Issac PK, Lite C, Guru A et al (2021) Tryptophan-tagged peptide from serine threonine-protein kinase of Channa striatus improves antioxidant defence in L6 myotubes and attenuates caspase 3–dependent apoptotic response in zebrafish larvae. Fish Physiol Biochem 47:293–311. https://doi.org/10.1007/s10695-020-00912-7
Acknowledgements
This work was funded by Princess Nourah bint Abdulrahman University Researchers Supporting Project Number (PNURSP2023R62), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
G.S and M.V performed most of experiments and wrote the manuscript. N.H.A; T.M.A; and S.A reviewed and edited the manuscript. A.G and J.A supervised and validated the work.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have declared that no competing interests exist.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sudhakaran, G., Velayutham, M., Aljarba, N.H. et al. Nimbin (N1) and analog N3 from the neem seeds suppress the migration of osteosarcoma MG-63 cells and arrest the cells in a quiescent state mediated via activation of the caspase-modulated apoptotic pathway. Mol Biol Rep 50, 7357–7369 (2023). https://doi.org/10.1007/s11033-023-08627-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08627-7