Abstract
Background
Idiopathic pulmonary fibrosis is characterized by progressive lung tissue remodeling and disproportionate deposition of collagenous proteins with limited therapeutic interventions. The purpose of this study was to determine whether curcumin inhibits bleomycin (BLM)-induced increases in synthesis, degradation and cross-linking of lung collagen in rats.
Methods and results
Following a single intratracheal instillation of BLM to rats (0.75 U/100 g, sacrificed 3, 5, 7, 14 and 28 days post-BLM), lung collagen synthesis (determined by incorporation of 3H-proline) and deposition (determined by lung hydroxyproline content) progressively increased at days 7, 14 and 28 post-BLM injection. Lung lavage fluid hydroxyproline and collagenase levels (a measure of collagen turnover) were increased in BLM rats compared with control groups. In addition, BLM instillation resulted in increased concentrations of collagenase and collagenolytic cathepsin in the lungs. Furthermore, increased cross-linking (as determined by aldehyde content of acid soluble collagen), and decreased susceptibility of fibrotic lung insoluble collagen to denaturing agents occurred in BLM-injured lungs. Significant increases in alveolar macrophage (AM) release of transforming growth factor-β1 (TGF-β1) were noted at various time points (days 3, 5, 7, 14 and 28 post-BLM) during the development and progression of lung fibrosis in rats. Curcumin treatment to BLM rats (300 mg/kg 10 days before and daily thereafter throughout the experimental time period) was associated with marked reductions in lung collagen synthesis and deposition, BALF and lung collagenase activity, BALF hydroxyproline content and lung collagenolytic levels. Additionally, reduced levels of collagen cross-linking and enhanced susceptibility of insoluble lung collagen to denaturing agents were observed in curcumin-treated BLM rats. Finally, curcumin inhibited BLM-induced increases in AM production of TGF-β1.
Conclusions
Our data demonstrate for the first time that curcumin prevents fibrotic deposits by modulating collagen turnover, assembly and deposition in BLM-instilled rat lungs, and that curcumin treatment protects against BLM activation of macrophages by suppressing the release of TGF-β1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the normal lung, a delicate balance exists between synthesis and degradation of the extracellular matrix (ECM) proteins. However, this dynamic equilibrium is jeopardized during the pathogenesis of idiopathic pulmonary fibrosis (IPF), resulting in an excessive synthesis and abnormal deposition of ECM proteins, particularly collagens, in the lung parenchyma that leads to severe loss of lung function, respiratory failure and death [1,2,3].
Bleomycin (BLM), a highly efficient antitumor antibiotic used in the treatment of various cancers, causes dose-dependent pulmonary injury, which leads to a progressive destruction of lung parenchyma followed by proliferation of fibroblasts, and abnormal synthesis and accumulation of extracellular matrix (ECM) components in the alveolar interstitium [4, 5]. Activation of interstitial and subepithelial fibroblasts and myofibroblasts to proliferate and to synthesize collagen apparently follows injury to the alveolar epithelium and endothelium [1, 6]. Biochemical studies demonstrate that there is more collagen in BLM-induced fibrotic lung, and in human interstitial pulmonary fibrosis, than in the normal lung [7,8,9,10,11]. Early increase in type III collagen followed by type I collagen at later stages of fibrosis results in an increased ratio of type I to type III collagen [12]. Mediators of fibroproliferative processes include fibrogenic cytokines such as transforming growth factor-β1 (TGF-β1) that serve to enhance the synthesis and deposition of collagen and other matrix constituents [13]. TGF-β1 exerts its profibrotic effects by inducing the synthesis of ECM, decreasing its degradation, and stimulating the synthesis of integrin matrix receptors [14]. Additionally, connective tissue growth factor (CTGF), platelet derived growth factor (PDGF), and fibroblast growth factor 2 (FGF-2), play major roles in the process of lung fibrogenesis [13,14,15].
Untreated IPF patients typically have poor quality-of-life linked to progressively disabling dyspnea, with a median survival of around 3–5 years. Current therapies that inhibit abnormal ECM synthesis and deposition and thus progression to end-stage interstitial lung disease are often limited and have proven unsatisfactory. Although clinical interventions with nintedanib and pirfenidone have been appreciated in IPF, these drugs have shown only a modest efficacy on matrix expansion, remodeling and progression of lung destruction [16,17,18]. Therefore, it is not surprising that modulation of excess collagen deposition has become the center of intense research efforts in pulmonary fibrosis. Continuous efforts are therefore made to find potential novel therapeutic agents for IPF.
Curcumin, diferuloylmethane, a main phenolic compound extracted from turmeric (Curcuma longa), has numerous therapeutic properties and its effects in various lung diseases have been reported [19,20,21,22]. Our laboratory has previously demonstrated the first protective function of curcumin against BLM-induced lung injury and inflammation collagen content [23]. Studies from other laboratories have also confirmed the protective effect of curcumin on lung collagen deposition in animal models of lung fibrosis [24,25,26,27]. However, earlier studies, including our own investigations, on the antifibrotic effect of curcumin were limited to either localization of lung collagen components at the immunohistochemical level or collagen assay; results of detailed collagen metabolism studies were scanty. A detailed understanding of the protective effects of curcumin on BLM-induced changes in collagen metabolism (collagen biosynthesis, extracellular collagen crosslinking and proteinases involved in collagen turnover) during initiation and development of lung fibrosis is largely unexplored. Therefore, we set to determine the new biochemical insights into the protective function of curcumin on dysregulated lung collagen remodeling in a rat model of BLM-induced pulmonary fibrosis.
Methods
Experimental design
Healthy male Wistar rats weighing 325–350 g were obtained from the animal house facilities of Central Leather Research Institute, and allowed to acclimatize for one week before experiments with water and laboratory rat chow ad libitum. A 12-h/12-h light/dark cycle was maintained. All experiments were carried out according to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 86–23, revised 1996).The animal ethical committee of CLRI approved the project proposal and experiments were conducted following the rules of the ethical committee.
Rats were divided into four groups. The first group (SAL) consisted of saline-instilled rats, which received a single intratracheal (i.t.) dose of 0.4 ml of sterile physiological saline. The second group (CUR) received 300 mg/kg of curcumin. The third group (BLM) received a single i.t. dose of bleomycin (0.75 U/100 g body weight in sterile physiological saline). The final group (CUR + BLM) received 300 mg/kg of curcumin 10 days before BLM and daily thereafter throughout the experimental period (28-d period). Saline and BLM were instilled to rats through the endotracheal catheter (a non-toxic polyethylene tubing, inner diameter: 1.67 mm; outer diameter: 2.42 mm, length: 70 mm) using a sterile 1-ml syringe under sodium pentobarbital anaesthesia (35 mg/kg) followed by 3 ml of air to distribute the drugs equally. Curcumin, prepared fresh everyday, was suspended in 1% gum acacia and administered by gastric intubation.
Bronchoalveolar lavage fluid (BALF)
Bronchoalveolar lavage was performed at days 3, 5, 7, 14 and 28 post-BLM administration as described previously. Briefly, the animals were anaesthetized with an intraperitoneal dose of sodium pentobarbital. A polyethylene catheter was placed in the trachea and secured in place. Rats were exsanguinated via the abdominal aorta, and an incision was made in the diaphragm (to allow the lungs to expand during lavage procedures). The lungs were lavaged 5 times with 5 ml/wash of calcium and magnesium-free phosphate-buffered saline, pH 7.4, prewarmed at 37 °C. The BALF was centrifuged at 300×g for 10 min at 4 °C, and the cell-free supernatant was aliquoted and stored at − 70 °C.
Collagen biosynthesis
Lung collagen synthesis was determined following the method of Clark et al. [7] as outlined by [28]. Lung slices were incubated in 5 ml of Dulbecco’s modified Eagle’s medium containing 10% foetal bovine serum, 50 μg/ml ascorbic acid, 75 μg/ml ferrous sulphate, 200 U/ml penicillin, 200 μg/ml streptomycin and 30 μCi of 3H-Proline. Lung slices were equilibrated with 95% O2/5% CO2 and incubated for 4 h at 37 °C in a Controlled Environment Incubator Shaker (New Brunswick Scientific Co. Inc., Edison, New Jersey, USA). At the end of incubation period, lung samples were homogenized with a Polytron homogenizer in 10% trichloroacetic acid (TCA) and washed 4 times with 5% TCA. The TCA soluble fraction was hydrolyzed with 6 N hydrochloric acid (final concentration) and the hydroxyproline content and radioactivity of hydroxyproline were determined [29]. The results were expressed as cpm of 3H-hydroxyproline/hour/lung.
Determination of total hydroxyproline content and the radioactivity of 3H-hydroxyproline
The total hydroxyproline content and the radioactivity of 3H-hydroxyproline were determined following the procedure of [30]. The samples after acid hydrolysis with 6 N hydrochloric acid were neutralized with potassium hydroxide and made up to known volume. About 2 ml of sample containing 1–10 μg of hydroxyproline was mixed with 1 ml of chloramine-T (0.141 g of chloramine-T mixed with 2 ml of distilled water), 3 ml of peroxide free methyl cellosolve and 5 ml of sodium acetate-citrate buffer, pH 6.0, and allowed to stand for 20 min at room temperature. The oxidation process was stopped by the addition of 0.5 ml of 2 M sodium thiosulphate. After thorough shaking, the reaction mixture was saturated with approximately 2 g sodium chloride. The oxidation product of proline and other interfering substances were removed by extraction with toluene. To convert the oxidation product of hydroxyproline to pyrrole, the aqueous solution was heated in a boiling water bath for 30 min, cooled at room temperature and pyrrole obtained from hydroxyproline was extracted with 6 ml of toluene. One ml of toluene layer containing pyrrole was mixed with 4 ml of Ehrlich’s reagent (0.5 g p-dimethylaminobenzaldehyde in 9 ml of absolute ethanol and 1 ml of 12 N hydrochloric acid). The contents were shaken, kept for 30 min at room temperature and the colour developed was read at 557 nm. Aliquots containing 4 ml of the toluene layer were transferred to scintillation vials containing ready gel liquid scintillation cocktail and the radioactivity of 3H-hydroxyproline were measured in an automated liquid scintillation system (Beckman LS-1701).
Estimation of total collagen in lungs
The total collagen content of the lung tissue was determined by the estimation of hydroxyproline, a characteristic imino acid of collagen. Lung tissues were washed with physiological saline, cut into small pieces and defatted with chloroform: methanol (2% v/v). Lung tissue (either dry or wet weight) was hydrolyzed with 6 N HCl at 110 °C for 20 h in sealed tubes. After hydrolysis, the sample was evaporated to dryness; the residue was dissolved in water and made up to a known volume. The hydroxyproline was then estimated by the method of Woessner [30]. The collagen content of lung tissues was then calculated by multiplying the hydroxyproline content by the factor 7.46 [31].
2 ml portions containing 2–10 μg hydroxyproline were placed in test tubes. A series of standards were prepared containing 0–10 μg hydroxyproline in a total volume of 2 ml. Hydroxyproline oxidation was initiated by adding 1 ml of chloramine-T (0.141 g of chloramine-T mixed with 2 ml of distilled water, 3 ml of peroxide free methyl cellosolve and 5 ml of sodium acetate-citrate buffer, pH 6.0) to each tube. The tube contents were vortexed for few minutes and allowed to stand for 20 min at room temperature. The chloramine-T was then destroyed by adding 1 ml of perchloric acid (27 ml of perchloric acid to 100 ml water) to each tube. The contents were mixed and allowed to stand for 5 min. Finally 1 ml of p-dimethylaminobenzaldehyde (PDAB; 20% solution was prepared shortly before use by adding methyl cellosolve to 20 g of PDAB to give a final volume of 100 ml and warmed to 60 °C to facilitate solubilization) solution was added and the mixture was shaken. The tubes were placed in a 60 °C water bath for 20 min, and then cooled in tap water for 5 min. The colour developed was read at 557 nm. Results are expressed as μg/mg dry tissue or mg/g wet tissue.
Extraction, purification and fractionation of collagen
Extraction, purification and fractionation of collagen were carried out at 4 °C, according to the procedure described by Miller and Rhodes [32].
Total collagen (TC)
Lung tissues of different experimental groups were washed, weighed and minced in 0.05 M Tris–HCl, pH 7.5. The minced tissues were homogenized in 0.05 M Tris–HCl and a portion of the homogenate was used for the estimation of hydroxyproline content and radioactivity.
Neutral salt soluble collagen (NSSC)
The remaining portion was extracted twice with 1 M sodium chloride in 0.05 M Tris–HCl pH 7.5 containing 20 mM EDTA and 1 mM phenylmethylsulfonylfluoride at 4 °C in a refrigerated centrifuge. An aliquot of the supernatant was hydrolyzed with an equal volume of 12 N hydrochloric acid, and the collagen content was determined.
Acid soluble collagen (ASC)
The residue left after sodium chloride extraction was again extracted with 0.5 M acetic acid, pH 3.0, under similar conditions as described above for a total period of 72 h, with daily changes of fresh acid. The supernatants obtained were pooled together and centrifuged at 20,000 rpm for 1 h at 4 °C. An aliquot of the supernatant was subjected to the determination of collagen content.
Pepsin soluble collagen (PSC)
The residue left after acetic acid extraction was again extracted with 0.5 M acetic acid containing pepsin (1:100 ratio between the weight of the enzyme and dry weight of the tissue to be extracted) under similar conditions as described above for a total period of 72 h, with daily changes of fresh acid. The supernatants obtained were pooled together and centrifuged at 20,000 rpm for 1 h at 4 °C. An aliquot of the supernatant was subjected to the determination of collagen content.
Insoluble collagen (ISC)
Neutral salt soluble, acid soluble and pepsin soluble collagen were expressed as percentage of total collagen. Insoluble collagen content was calculated by substracting the sum of soluble collagen contents (NSSC + ASC + PSC) from 100.
Assay of BALF collagenase
Collagenase activity in lung lavage fluid was measured following the method of Christner et al. [33], with modification. Assays were carried out as follows: (1) an aliquot of acetic acid solution of rat skin type 1 collagen was incubated with 0.1 M Tris–HCl (pH 7.5) containing 0.15 M sodium chloride, and 0.1 M EDTA for 60 min at 37 °C. (The amount of lavage fluid added to the assay mixture was 50 μl). The tube was capped and the contents were mixed gently and incubated at 37 °C for 24 h. The reaction tube was placed on ice for 10 min just after incubation, and then centrifuged at 15,000 rpm for 15 min. 50 μl of supernatant including the cleaved collagen was separately hydrolyzed with 6 N hydrochloric acid and assayed for hydroxyproline by the method of Woessner [30]. Total collagenolytic activity was expressed as μg collagen degraded/hour/ml of lavage fluid.
Assay of lung collagenase activity
The lung collagenolytic activity was determined according to the method of Woessner [34].
Preparation of lung samples
Minced lungs from each animal were weighed and frozen. When ready for assay they were thawed, suspended in 5 ml of 0.05 M Tris–HCl buffer (pH7.6) containing 0.25% Triton x-100 and 0.01 M calcium chloride. Each sample was then homogenized in a Polytron homogenizer. After centrifugation at 10,000×g for 15 min, the pellet was resuspended in 5 ml of 0.05 M Tris–HCl (pH 7.6) containing 200 units/ml penicillin and 250 μg/ml streptomycin and 0.15 M sodium chloride. This suspension was used for the assay of lung collagenolytic activity.
Procedure
The samples to be assayed were divided into two equal portions. The first one served as the blank and contained 0.01 M EDTA and the volume was made up to 10 ml with Tris buffer. The second portion, which served as test contained 0.01 M calcium chloride and made up to 10 ml with the same buffer. To both tubes, 100 μg trypsin was added, incubated at 37 °C for 5 min (to activate latent collagenase) and stopped with 400 μg of soyabean trypsin inhibitor. They were then incubated in a Controlled Environment Incubator Shaker (New Brunswick Scientific Co., Inc. Edison, New Jersey, USA) for 24 h at 37 °C. Soluble hydroxyproline containing peptides were released by collagenase from lung collagen present in the pellets. These products were separated from undigested insoluble collagen by centrifugation of the digests at 4 °C for 30 min at 30,000×g. The resulting supernatants and the pellets were separately hydrolyzed with 6 N hydrochloric acid and assayed for hydroxyproline by the method of Woessner [30]. Total collagenolytic activity was expressed as μg of collagen degraded/mg of collagen.
Assay of lung collagenolytic cathepsin
The activity of lung collagenolytic cathepsin was assayed by the modified method of Anderson [35] using bovine tendon collagen as the substrate. The bovine tendon collagen was suspended at a concentration of 10 mg/ml in a solution of 0.25% acetic acid in 25% of glycerol (v/v). The collagen was dispersed with the Polytron homogenizer and the resulting homogenate was adjusted to pH 3.5 with acetic acid. Aliquots (0.5 ml) of enzyme were added to 0.5 ml of collagen suspension in a series of centrifuge tubes. One ml of 0.2 M sodium formate buffer, pH 3.5, containing 10 mM cysteine was added to each tube and mixed thoroughly. The reaction mixture was incubated at 37 °C for 3 h and centrifuged at 3,000×g for 15 min to remove residual collagen. The blank readings were obtained from assay mixture that had been prepared on ice and then centrifuged without prior incubation. Hydroxyproline content in the supernatant was determined by the method of Woessner [30] as described above. The amount of collagen degraded was calculated and enzyme activity was expressed as μM of hydroxyproline liberated/mg protein.
Estimation of aldehydes in acid soluble collagen
Aldehydes in collagen were measured according to the method of Paz et al. [36]. One ml of 0.2% solution of purified acid soluble collagen in 0.5 M acetic acid was used for the estimation of aldehydes. The solution was heated for 3 min at 100 °C in a screw-capped tube with 0.2 ml of 1% solution of N-methylbenzothiazolone hydrazone (MBTH). To the cooled reaction mixture, 2.5 ml of 0.2% ferric chloride solution was added, reacted for 5 min and then 6.5 ml of acetone was added. The colour developed was read at 670 nm. A reagent blank and a series of standards (2 nmol to 1 micromole/ml of aldehyde) were run simultaneously to give a standard curve.
Susceptibility of insoluble collagen to denaturing agents
The susceptibility of insoluble collagen to denaturing agents such as urea and potassium cyanide was studied according to the method of Adam et al. [37]. Homogenized insoluble collagen samples of wet weight 900 mg were suspended in 15 ml of 6 M urea and 2 M potassium cyanide separately at room temperature for 24 h with constant stirring. The samples were then centrifuged and the amount of solubilized collagen was calculated by estimating the hydroxyproline content of the supernatant by the method of Woessner [30] as described above.
Preparation of alveolar macrophage (AM)-conditioned media and determination of rat TGF-β1
AM culture was performed as described before [23] and the concentration of TGF-β1 in AM-conditioned media was determined using a human TGF-β1 ELISA kit (R&D Systems, MN, USA) that detects rat TGF-β1 protein with a sensitivity of 5 pg/ml. The assay detects only the active form of TGF-β1, and samples were activated before measurement according to the manufacturer’s protocol. All assays were done in triplicate wells.
Statistical analysis
Results are expressed as mean ± standard deviation of six independent experiments. Statistical analysis was performed by one-way analysis of variance (ANOVA) for multiple comparisons followed by post-hoc Bonferroni test (Graphpad Prism, version 3.01).
Results
Figure 1 illustrates the time course studies on BLM-induced changes in collagen synthesis (as measured by the incorporation of 3H-proline). Compared to control lungs, a dramatic increase in lung collagen synthesis was observed at 7 days post-BLM injection. Collagen synthesis was also elevated at 14 and 28 days after BLM administration. Administration of curcumin markedly reduced BLM-induced increases in lung collagen biosynthesis.
Protective effects of curcumin on bleomycin-induced increases in lung collagen synthesis. Results are mean ± SD of six independent observations in each group. Statistical analysis was done using one way analysis of variance with post-hoc Bonferroni test. *Significantly (p < 0.001) higher than all groups; §significantly (p < 0.001) lower than bleomycin rats
Since a maximal increase in lung collagen was observed at 28 days post-BLM administration, various collagen fractions were isolated and characterized at this time point. Figure 2a demonstrates the concentration of neutral salt soluble and acid soluble collagen in the lungs of BLM-treated rats. Compared with controls, BLM lungs had a decrease in NSSC. In contrast, increased levels of ASC were noted in BLM lungs. BLM-induced changes in collagen fractions were significantly inhibited by curcumin treatment. Concentrations of PSC and TC were increased in BLM-injured lungs (Fig. 2b) as compared with control lungs. However, curcumin inhibited BLM-induced increases in lung PSC and TC.
Protective effects of curcumin on bleomycin-induced changes in lung collagen fractions: NSSC & ASC (a); PSC & TC (b). Results are mean ± SD of six rats in each group. Statistical analysis was done using one way analysis of variance with post-hoc Bonferroni test. ¶Significantly (p < 0.001) lower than all groups; #significantly (p < 0.001) higher than bleomycin rats; *significantly (p < 0.001) higher than all groups; §significantly (p < 0.001) lower than bleomycin rats. NSSC neutral salt soluble collagen; ASC acid soluble collagen; PSC pepsin soluble collagen; TC total collagen
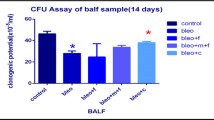
Analysis of BAL fluid revealed a progressive increase in collagenase activity (Fig. 3a) in BLM rats, while collagenase activity was virtually absent in BAL fluid of control rats. BALF collagenase activity was elevated 3 days after BLM and reached its peak at day 7. Thereafter, collagenase level decreased but it was still significantly higher than control values. Similarly, BALF hydroxyproline content was elevated in BLM rats, compared to controls, reaching its peak 7 days after BLM injection (Fig. 3b). Statistically significant (p < 0.001) inhibition of BLM-stimulated BALF collagenase and hydroxyproline was found with curcumin treatment.
Protective effects of curcumin on bleomycin-induced changes in collagenase (a) and hydroxyproline (b) content in lung lavage fluid. Results are mean ± SD of six rats in each group. Statistical analysis was done using one way analysis of variance with post-hoc Bonferroni test. *Significantly (p < 0.001) higher than all groups; ‡significantly (p < 0.001) lower than bleomycin rats
Levels of lung collagenase (Fig. 4a) and collagenolytic cathepsin (Fig. 4b) increased between 1.5- and 2.5-fold in BLM rats compared with control rats (p < 0.001). Both collagenase and collagenolytic cathepsin activities were up-regulated as early as 3 days post-BLM, reached its peak 7 days after BLM, and remained higher until the end of experimental time period. In the fibrotic rats treated with curcumin, levels of lung collagenase and collagenolytic cathepsin were dramatically reduced to near control values.
Protective effects of curcumin on bleomycin-induced changes in lung collagenase (a) and collagenolytic cathepsin (b). Results are mean ± SD of six rats in each group. Statistical analysis was done using one way analysis of variance with post-hoc Bonferroni test. *Significantly (p < 0.001) higher than all groups; #significantly (p < 0.001) lower than bleomycin rats
Levels of aldehyde from acid soluble collagen of BLM-injured lungs increased 3-fold compared with control lungs (Fig. 5a), whereas treatment with curcumin dramatically reduced BLM-induced increases in aldehyde content of acid soluble collagen. The susceptibility of lung insoluble collagen to denaturing agents such as 6 M urea and 2 M KCN were significantly (p < 0.001) lower in BLM rats compared with control animals (Fig. 5b), but curcumin treatment significantly increased the susceptibility of fibrotic lung insoluble collagen to denaturing agents.
Protective effects of curcumin on bleomycin-induced changes in aldehyde content (a) and susceptibility of lung collagen to denaturing agents (b). Results are mean SD of six rats in each group. Statistical analysis was done using one way analysis of variance with post-hoc Bonferroni test. *significantly (p < 0.001) higher than all groups; §Significantly (p < 0.001) lower than bleomycin rats; †significantly (p < 0.001) lower than all groups; ‡significantly (p < 0.001) higher than bleomycin rats
Transforming growth factor-β1 release was measured as an indicator for BLM-induced macrophage activation. AM production of TGF-β1 was significantly (p < 0.001) higher in BLM rats: the levels of TGF-β1 increased on days 3 and 5, peaked at day 7, and remained elevated until the end of the observation time (Fig. 6). It is also interesting to note that AM from BLM rats elaborated greater amounts of TGF-β1 in culture medium without any exogenous stimulus suggesting that BLM has activated (“primed”) AM in vivo to release this fibrotic cytokine. Interestingly, curcumin treatment significantly (p < 0.001) suppressed BLM-induced AM release of TGF-β1.
Protective effects of curcumin against bleomycin-induced changes in alveolar macrophage release of transforming growth factor-1. Results are mean ± SD of six independent observations in each group. Statistical analysis was done using one way analysis of variance with post-hoc Bonferroni test. *Significantly (p < 0.001) higher than all groups; $significantly (p < 0.001) lower than bleomycin rats
Discussion
Remodeling of the alveolar interstitial matrix is a final common pathway towards lung destruction in pulmonary fibrosis. Increase in lung cellularity and ECM, specifically, collagens, are important histological abnormalities that occur both in animal models and in human pulmonary fibrosis [1, 38, 39]. Increased deposition and remodeling of lung collagen could lead to changes in biochemical, biomechanical and functional properties of the lung tissue in pulmonary fibrosis. Our earlier studies on curcumin inhibition of BLM-induced lung injury led us to postulate whether this protective activity of curcumin extends to modulation of collagen turnover. The present study demonstrates a protective role for curcumin in BLM-induced fibrotic remodeling by regulating lung tissue collagen metabolism, assembly and deposition. In BLM-injured lungs, an increase in collagen synthesis and deposition and a decrease in neutral salt soluble collagen (NSSC) were observed. The NSSC fraction represents the youngest form of collagen that serves as precursor to insoluble collagen [40], and a decrease in NSSC could indicate the involvement of NSSC in the formation of insoluble collagen in pulmonary fibrosis. The data also indicate significant increases in acid soluble collagen (being the more mature fiber-forming protein), and enhanced turnover of insoluble collagen (in this case pepsin soluble collagen), suggesting increased conversion of soluble collagen to insoluble collagen in fibrotic lungs. Interestingly, studies on specific and total activities of soluble and insoluble collagen of sponge-implanted rats in vivo revealed that acid soluble collagen contributes to the formation of insoluble collagen [41].
The observations of the present study reveal increased levels of BALF collagenase and hydroxyproline that ran parallel with the increases in lung collagenase and collagenolytic cathepsin activities in BLM rats. The peak levels of BALF hydroxyproline coincided with the peak increases in myeloperoxidase and collagenase activities in the BALF and lung tissue of BLM rats, indicating that collagen degradation was maximal at the time of intense inflammation. Collagenase, a secretory enzyme, extracellularly cleaves collagens near neutral pH at specific loci in the polypeptide chain across the triple helix. Collagenolytic cathepsins degrade collagens in acidic media at the N-terminal nonhelical region containing the intramolecular cross-link. In addition, lysosomal proteinases are able to degrade collagen at acid pH (4–7); therefore, the lysosomes may also play a role in the degradation of collagen or of collagen fragments. Newly secreted collagen is also degraded extracellularly before deposition in mature collagen fibers, and this pathway is important in regulating collagen deposition. These enzymes, together with the intracellular degradation of newly synthesized collagen, control the overall rate of collagen degradation in the lung.
The present results are in agreement with the findings of Blaisdell and Giri [42], and that of Bakowska and Adamson [43], who reported increased levels of collagenase in the lungs and BALF, respectively. An increased level of BALF hydroxyproline observed in this study agrees with the findings of Bakowska and Adamson [43]. Increased levels of collagenase have been reported in idiopathic pulmonary fibrosis [44], and in experimental models of lung fibrosis [28] and in patients with adult respiratory distress syndrome [33].
Our observations together with reports from other laboratories indicate that although normal lung contains a small amount of collagenase activity, this activity increases during earlier stages of lung fibrosis. However, this raises a pertinent question as to why an increase in collagen deposition in fibrotic lungs should occur in presence of increased collagenase activity. Increased collagenase activity could be recognized as an essential intervention to reduce excess collagen accumulation; however, this might also make worse the situation further by supplying collagen degradation products that would augment more collagen synthesis and deposition in the fibrotic lung. This is especially the case in idiopathic pulmonary fibrosis [44].
The extent of cross-linking was increased in fibrotic lung collagen, as measured biochemically by the increase in aldehyde content. Increased aldehyde content shows a greater potential for crosslink formation [45, 46]. This crosslink formation is necessary for the stabilization of collagen fibrils and fibers, and for the integrity and elasticity of mature elastin. The degree of cross-linking in collagen is inversely proportional to its solubility [47]. The lower the amount of cross-linking, greater the susceptibility of collagen to denaturing agents. Accordingly, the present study used hydroxyproline release from insoluble collagen as an index of collagen solubility. The data demonstrated a consistent decrease in the release of hydroxyproline from fibrotic lung collagen compared with normal lung collagen, indicating an increase in intermolecular cross-linking of collagen in the fibrotic lung. In this regard, Vater et al. [48] have demonstrated that collagen crosslinks mediated by lysyl oxidase was ten times more resistant to digestion by mammalian collagenase.
Importantly, curcumin administration reduced BLM-induced increases in BALF hydroxyproline and collagenase levels, and lung collagenolytic activities, and also enhanced the susceptibility of insoluble collagen to denaturing agents in BLM-damaged lungs. This may be due to the anti-inflammatory and membrane stabilizing properties of curcumin [19, 49,50,51,52], thus preventing leakage and accumulation of collagenolytic activities, which may contribute to protective effects. Importantly, curcumin was reported to lower the secretion of collagenase, elastase and hyaluronidase from rat peritoneal macrophages [53].
Collagen fibers mostly determine the structural stability of lung tissue. Results of the analysis of collagenolytic enzymes on lung structure and function have enabled to characterize the mechanical properties of these fibrous proteins in the lung. Collagens provide structural support and regulate a variety of cellular processes such as cell attachment, migration, proliferation and differentiation. It is well appreciated that fibrotic lung diseases exhibit changes in collagen composition and mechanical properties during disease progression. Abnormal collagen deposition followed by increased collagen crosslinking and ECM remodeling result in an increase in ECM stiffness and scar tissue, traction bronchiectasis, thickened interlobular septae and subpleural honeycombing, compared to normal tissue [54]. Interestingly, curcumin treatment inhibited BLM-induced increases in lung collagen deposition and collagen cross-link formation. The mechanism (s) by which curcumin inhibits BLM-induced increases in lung collagen deposition is not clear. Whether curcumin induces changes in collagen fibril size and morphology in BLM-injured lungs is not known. Furthermore, whether curcumin influences post-translational control of collagen molecules, in addition to transcriptional control of constituent proteins remains to be studied. These are the subjects of our future investigations.
Fibroblast differentiation into myofibroblasts and epithelial-mesenchymal transition (EMT) are key cellular events initiating the development of fibrosis. These cells appear to participate actively in tissue repair, but the production of excess ECM eventually reduces the respiratory function in the lung. We suggest the possibility that curcumin may inhibit the fibrogenic process in bleomycin lungs by affecting cellular processes such as cell proliferation, cell differentiation, production of inflammatory and fibrotic cell mediators [55,56,57,58,59]. Saidi et al. [56] have shown that curcumin inhibited TGF-β1-dependent lung fibroblast differentiation of human lung CCD-19Lu fibroblasts. Furthermore, these authors have reported that the expression of alpha smooth muscle actin (α-SMA), a profibrotic marker, was reduced, and the levels of both soluble and insoluble collagen were reduced to values comparable to those found in undifferentiated fibroblasts. Liu et al. [58] have reported that curcumin displayed anti-fibrosis property by inhibiting TGF-β induced differentiation of mouse lung fibroblasts to myofibroblasts, possibly mediated by the regulation of the expression of peroxisome proliferator activated receptor γ (PPAR-γ) and platelet derived growth factor R β (PDGFR-β). Thus, curcumin inhibition of cellular processes and fibrogenic mediator/cytokine (in our case TGF-β1) expression opens up the possibility that this would have negative impact on inflammation and development of fibrosis. TGF-β1, a profibrotic cytokine, is involved in the fibrotic response because of its ability to stimulate synthesis of ECM macromolecules, while inhibiting their degradation [13, 60]. Bronchiolar epithelial cells and interstitial fibroblasts express TGF-β1 under normal conditions. Cellular sources of TGF-β1 during tissue injury and inflammation include macrophages and mesenchymal, endothelial and mesothelial cells of the lung [61]. Lung biopsies from fibrotic subjects display increased expression of TGF-β1 [60,61,62]. Hoyt and Lazo [63] have shown enhanced TGF-β1 mRNA and protein content that occur before the increased expression of collagens in BLM-induced pulmonary fibrosis [63]. Giri et al. [64] have reported the importance of TGF-β1 on bleomycin induced accumulation of lung collagen using a neutralizing antibody to TGF-β1. In the present study, curcumin treatment significantly suppressed AM release of TGF-β1 in BLM rats.
The precise mechanism of suppression of macrophage TGF-β1 secretion in curcumin-treated BLM rats is not known at present, however, it is possible that curcumin may suppress activator protein-1 (AP-1), a transcription factor involved in TGF-β signaling pathway [65, 66], and results in the suppression of TGF-β1 expression. Interestingly, curcumin has been reported to be an inhibitor of AP-1 [67]. Thus, inhibition of TGF-β1 secretion might decrease inflammation and development of fibrosis because of its ability to influence ECM synthesis and deposition. This is supported by the decreased collagen synthesis and deposition in curcumin-treated BLM lungs as described above. We have recently demonstrated that curcumin treatment is associated with a profound inhibition of excess glycoproteins deposition in BLM-induced lung fibrosis [68]. Taken together, the present study demonstrates the significance of curcumin as an important therapeutic compound in not only inhibiting the amount of collagen being synthesized, but also regulating the amount of collagen available for crosslinking in lung fibrosis. Thus, curcumin may be a promising antifibrotic agent to prevent lung ECM remodeling in pulmonary fibrosis.
Data availability
All relevant data are within the manuscript.
References
Crouch E (1990) Pathobiology of pulmonary fibrosis. Am J Physiol 259:L159-184
Snijder J, Peraza J, Padilla M, Capaccione K, Salvatore MM (2019) Pulmonary fibrosis: a disease of alveolar collapse and collagen deposition. Expert Rev Respir Med 13:615–619
Jones MG, Andriotis OG, Roberts JJ et al (2018) Nanoscale dysregulation of collagen structure-function disrupts mechano-homeostasis and mediates pulmonary fibrosis. Elife 7:e36354
Cooper JAD Jr (1997) Drug-induced lung disease. Adv Intern Med 42:231–268
Giri SN, Wang Q (1989) Mechanisms of bleomycin-induced lung injury. Comments Toxicol 3:145–176
Goldstein RH, Fine A (1986) Fibrotic reactions in the lung: the activation of the lung fibroblast. Exp Lung Res 11:245–261
Clark JG, Overton JE, Marino BA, Uitto J, Starcher BC (1980) Collagen biosynthesis in bleomycin-induced pulmonary fibrosis in hamster. J Lab Clin Med 96:943–953
Kelly J, Newman RA, Evans JN (1980) Bleomycin-induced pulmonary fibrosis in the rat: prevention with an inhibitor of collagen synthesis. J Lab Clin Med 96:954–964
Fulmer JD, Bienkowski RS, Cowan MJ (1980) Collagen concentration and rates of synthesis in idiopathic pulmonary fibrosis. Am Rev Respir Dis 122:289–301
Kirk JM, Da Costa PE, Turner-Warwick M, Littleton RJ, Laurent GJ (1986) Biochemical evidence for an increased and progressive deposition of collagen in lungs of patients with pulmonary fibrosis. Clin Sci 70:39–45
Selman M, Montano M, Ramos C, Chapela R (1986) Concentration, biosynthesis and degradation of collagen in idiopathic pulmonary fibrosis. Thorax 41:355–359
Kuhn C 3rd, Boldt J, King TE Jr, Crouch E, Vartio T, McDonald JA (1989) An immunohistochemical study of architectural remodeling and connective tissue synthesis in pulmonary fibrosis. Am Rev Respir Dis 140:1693–1703
Gauldie J, Jordana M, Cox M (1993) Cytokines and pulmonary fibrosis. Thorax 48:931–935
Border WA, Noble NA (1994) Transforming growth factor-β in tissue fibrosis. N Engl J Med 331:1286–1292
Henderson NC, Rieder F, Wynn TA (2020) Fibrosis: from mechanisms to medicines. Nature 587:555–566
Raghu G, Remy-Jardin M, Myers JL, Richeldi, Ryerson CJ, Lederer DJ, Behr J, Cottin V, Danoff SK, Morell F et al (2018) Diagnosis of idiopathic pulmonary fibrosis. an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med 198:e44–e68
Hutchinson J, Fogarty A, Hubbard R, McKeever T (2015) Global incidence and mortality of idiopathic pulmonary fibrosis: a systematic review. Eur Respir J 46:795–806
Glass DS, Grossfeld D, Renna HA, Agarwala P, Spiegler P, Kasselman LJ, Glass AD, DeLeon J, Reiss AB (2020) Idiopathic pulmonary fibrosis: Molecular mechanisms and potential treatment approaches. Respir Investig 58:320–335
Ammon HP, Wahl MA (1991) Pharmacology of Curcuma longa. Planta Med 57:1–7
Venkatesan N, Punithavathi D, Babu M (2007) Protection from acute and chronic lung diseases by curcumin. Adv Exp Med Biol 595:379–405
Lelli D, Sahebkar A, Johnston TP, Pedone C (2017) Curcumin use in pulmonary diseases: state of the art and future perspectives. Pharmacol Res 115:133–148
Rahman I, Biswas SK, Kirkham PA (2006) Regulation of inflammation and redox signaling by dietary polyphenols. Biochem Pharmacol 72:1439–1452
Punithavathi D, Venkatesan N, Babu M (2000) Curcumin inhibition of bleomycin-induced pulmonary fibrosis in rats. Br J Pharmacol 131:169–172
Smith MR, Gangireddy SR, Narala VR, Hogaboam CM, Standiford TJ, Christensen PJ, Kondapi AK, Reddy RC (2010) Curcumin inhibits fibrosis-related effects in IPF fibroblasts and in mice following bleomycin-induced lung injury. Am J Physiol Lung Cell Mol Physiol 298:L616–L625
Hu Y, Zhang M, Jin Y (2018) Inhalation treatment of idiopathic pulmonary fibrosis with curcumin large porous microparticles. Int J Pharm 551:212–222
Amini P, Saffar H, Nourani MR, Motevaseli E, Najafi M, Ali Taheri R, Qazvini A (2018) Curcumin mitigates radiation-induced lung pneumonitis and fibrosis in rats. Int J Mol Cell Med. 7(4):212–219
Chun-Bin S, Yi Y, Qin-Yi W, Yang L, Jing-Ze Y, Hai-Jing X, Si-Qi Z, Jiong H, Jing W, Fei-Yu L, Jin-Yuan Y, Jia-Li Y, Yang ZS (2020) The main active components of Curcuma zedoaria reduces collagen deposition in human lung fibroblast via autophagy. Mol Immunol 124:109–116
Ramos C, Montano M, Gonzalez G, Vadillo F, Selman M (1988). Collagen metabolism in experimental lung silicosis. A trimodal behaviour of collagenolysis. Lung 166:347-353
Rojkind M, Gonzalez E (1974) An improved method for determining specific radioactivities of proline-14C and hydroxyproline-14C in collagen and in noncollagenous proteins. Anal Biochem 57:1–7
Woessner JF Jr (1961) The determination of hydroxyproline in tissue and protein samples containing small proportions of this imino acid. Arch Biochem Biophys 93:440–447
Neuman RE, Logan MA (1950) Determination of collagen and elastin in tissues. J Biol Chem 186:549–556
Miller EJ, Rhodes RK (1982). Preparation and characterization of the different types of collagen. Methods Enzymol. 82 Pt A, 33–64
Christner P, Fein A, Goldberg S, Lipmann M, Abrams W, Weinbaum G (1985) Collagenase in the lower respiratory tract of patients with adult respiratory distress syndrome. Am Rev Respir Dis 131:690–695
Woessner JF Jr (1979) Total, latent and active collagenase during the course of post-partum involution of the rat uterus. Effect Oestradiol Biochem J 180:95–102
Anderson AJ (1969) Effects of lysosomal collagenolytic enzymes, anti-inflammatory drugs and other substances on some properties of insoluble collagen. Biochem J 113:457–463
Paz MA, Blumenfeld OO, Rojkind M, Henson E, Furfine C, Gallop PM (1965) Determination of carbonyl compounds with N-methyl benzathiozolone hydrazone. Arch Biochem Biophys 109:548–559
Adam M, Fietzek P, Kuhn K (1968) The reaction of metals with collagen in vivo II. The formation of cross-links in the collagen of lathyritic rats after gold treatment in vivo. Eur J Biochem 3:411–421
Pickrell JA, Mauderly JL (1981). Lung connective tissue: Location, metabolism and response to injury. In: Pickrell JA (ed). CRC Press, Boca Raton, Florida
Witschi HP, Haschek WM, Meyer KR, Ulrich RL, Dalbey WE (1980) A pathogenetic mechanism in lung fibres. Chest 78(Suppl):395–399
Jackson DS, Bentley JP (1960) Significance of the extractable collagen. J Biophys Biochem Cytol 7:37–42
Tsurufugi S, Ogata Y (1965) Biosynthesis of collagen in skin minces in relation to the mechanism of the formation of insoluble collagen. Biochim Biophys Acta 104:193–199
Blaisdell RJ, Giri SN (1995) Mechanism of antifibrotic effect of taurine and niacin in the multidose bleomycin-hamster model of fibrosis: inhibition of lysyl oxidase and collagenase. J Biochem Toxicol 10:203–210
Bakowska J, Adamson IYR (1998) Collagenase and gelatinase activities in bronchoalveolar lavage fluids during bleomycin-induced lung injury. J Pathol 185:319–323
Gadek JE, Kelman JA, Fells G, Weinberger SE, Horwitz AL, Reynolds HY, Fulmer JD, Crystal RG (1979) Collagenase in the lower respiratory tract of patients with idiopathic pulmonary fibrosis. N Engl J Med 301:737–742
Siegel RC (1976) Collagen cross-linking. Synthesis of collagen cross-links in vitro with highly purified lysyl oxidase. J Biol Chem 251:5786–5792
Stimler NP, Tanzer ML (1976) Crosslinking. In: Ramachandran GN, Reddi AH (eds) Biochemistry of collagen. Plenum Press, New York, pp 137–162
Golub LM, Greenwald RA, Zebrowski EJ, Ramamurthy NS (1978) Effect of experimental diabetes on molecular characteristics of soluble rat tail tendon collagen. Biochim Biophys Acta 534:73–81
Vater CA, Harris ED, Siegel RC (1979) Native cross-links in collagen fibrils induce resistance to human synovial collagenase. Biochern J 181:639–645
Nirmala C, Puvanakrishnan R (1996) Protective role of curcumin against isoproterenol induced myocardial infarction in rats. Mol Cell Biochem 159:85–93
Satoskar RR, Shah SJ, Shenoy SG (1986) Evaluation of anti-inflammatory property of curcumin (diferuloylmethane) in patients with postoperative inflammation. Int J Clin Pharmacol Ther Toxicol 24:651–654
Srimal RC, Dhawan BN (1973) Pharmacology of diferuloylmethane (curcumin), a non-steroidal anti-inflammatory agent. J Pharm Pharmacol 25:447–452
Srivastava V, Srimal KC (1985) Modification of certain inflammation induced biochemical changes by curcumin. Ind J Med Res 81:215–223
Joe B, Lokesh BR (2000) Dietary n-3 fatty acids, curcumin and capsaicin lower the release of lysosomal enzymes and eicosanoids in rat peritoneal macrophages. Mol Cell Biochem 203:153–161
Noble PW, Barkauskas CE, Jiang D (2012) Pulmonary fibrosis: patterns and perpetrators. J Clin Invest 122:2756–2762
Chang WA, Chen CM, Sheu CC, Liao SH, Hsu YL, Tsai MJ, Kuo PL (2020) The potential effects of curcumin on pulmonary fibroblasts of idiopathic pulmonary fibrosis (IPF)-approaching with next-generation sequencing and bioinformatics. Molecules 25:5458
Saidi A, Kasabova M, Vanderlynden L, Wartenberg M, Kara-Ali GH, Marc D, Lecaille F, Lalmanach G (2019) Curcumin inhibits the TGF-beta1-dependent differentiation of lung fibroblasts via PPARgamma-driven upregulation of cathepsins B and L.Sci
Tyagi N, Singh DK, Dash D, Singh R (2019) Curcumin modulates paraquat-induced epithelial to mesenchymal transition by regulating transforming growth factor-beta (TGF-beta) in A549 Cells. Inflammation 42:1441–1455
Liu D, Gong L, Zhu H, Pu S, Wu Y, Zhang W, Huang G (2016) Curcumin Inhibits Transforming Growth Factor beta Induced Differentiation of Mouse Lung Fibroblasts to Myofibroblasts. Front Pharmacol 7:419
Zhang D, Huang C, Yang C, Liu RJ, Wang J, Niu J, Brömme D (2011) Antifibrotic effects of curcumin are associated with overexpression of cathepsins K and L in bleomycin treated mice and human fibroblasts. Respir Res 12:154
Khalil N, O’Connor RN, Unruh HW, Warren PW, Flanders KC, Kemp A, Bereznzy OH, Greenberg AH (1991) Increased production and immunochemical localization of transforming growth factor-beta in idiopathic pulmonary fibrosis. Am J Respir Cell Mol Biol 5:155–162
Santana A, Saxena B, Noble NA, Gold LI, Marshall BC (1995) Increased expression of transforming growth factor beta isoforms (β1, β2, β3) in bleomycin-induced pulmonary fibrosis. Am J Respir Cell Mol Biol 13:34–44
Broekelmann TJ, Limper AH, Colby TV, McDonald JA (1991) Transforming growth factor β1 is present at sites of extracellular matrix gene expression in human pulmonary fibrosis. Proc Natl Acad Sci USA 88:6642–6646
Hoyt DG, Lazo JS (1988) Alterations in pulmonary mRNA encoding procollagens, fibronectin and transforming growth factor-beta precede bleomycin-induced pulmonary fibrosis in mice. J Pharmacol Exp Ther 24:765–771
Giri SN, Hyde DM, Hollinger MA (1993) Effect of antibody to transforming growth factor beta on bleomycin induced accumulation of lung collagen in mice. Thorax 48:959–966
Kim SJ, Angel P, Lafyatis R, Hattori K, Kim KY, Sporn MB, Karin M, Roberts AB (1990) Autoinduction of transforming growth factor β1 is mediated by the AP-1 complex. Mol Cell Biol 10:1492–1497
Zhang Y, Feng XH, Deryneck R (1998) Smad3 and Smad4 cooperate with c-Jun/c-Fos to mediate TGF-beta-induced transcription. Nature 394:909–913
Pendurthi UR, Williams JT, Rao LV (1997) Inhibition of tissue factor gene activation in cultured endothelial cells by curcumin. Suppression of activation of transcription factors Egr-1, AP-1, and NF-kappa B. Arterioscler Thromb Vasc Biol 17:3406–3413
Durairaj P, Venkatesan S, Narayanan V, Babu M (2020) Protective effects of curcumin on bleomycin-induced changes in lung glycoproteins. Mol Cell Biochem 2020(469):159–167
Acknowledgements
The authors would like to thank Dr. V. Arumugam for his help in statistical analysis and Mr V. Elango for his help in animal experiments.
Author information
Authors and Affiliations
Contributions
Conceived and designed the current manuscript study: PD, VN, MB. Developed study protocols: PD, VN, MB. Data collection: PD, VN, MB. Analyzed and interpreted data: PD, VN, SV, MB. Prepared and edited the manuscript: PD, VN, SV, MB. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to declare for all authors that are relevant to the content of this article.
Ethical approval
All animals were treated with humane conditions and institutional guidelines for the care and use of animals were followed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Durairaj, P., Venkatesan, S., Narayanan, V. et al. Curcumin inhibition of bleomycin-induced changes in lung collagen synthesis, deposition and assembly. Mol Biol Rep 48, 7775–7785 (2021). https://doi.org/10.1007/s11033-021-06790-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-021-06790-3