Abstract
In this article, novel thiazol-indolin-2-one derivatives 4a–f have been synthesized via treatment of thiosemicarbazide (1) with some isatin derivative 2a–f and N-(4-(2-bromoacetyl)phenyl)-4-tolyl-sulfonamide (3) under reflux in ethanol in the presence of triethyl amine (TEA). The structures of new products were elucidated by elemental and spectral analyses. Moreover, all compounds were investigated for their in vivo anti-inflammatory activity using celecoxib as a reference drug. The target compound 4b was the most active anti-inflammatory candidate and exhibited higher edema inhibition (EI = 38.50%) than that recorded by celecoxib (EI = 34.58%) after 3 h. Furthermore, the most active compounds 4b and 4f were subjected to a molecular docking study inside COX-2 enzyme to show their binding interactions. Both compounds 4b and 4f showed good fitting into COX-2 binding site with docking energy scores − 11.45 kcal/mol and − 10.48 kcal/mol, respectively which indicated that compound 4b revealed the most promising and effective anti-inflammatory potential.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Inflammation is a biological reaction to a disturbance in tissue homeostasis and body defense chemicals in which cells penetrate the affected tissue causing increasing blood flow, vascular permeability, and vasodilatation [1, 2]. Non-steroidal anti-inflammatory drugs (NSAIDs) are the most commonly used medications for relieving pain and inflammation by inhibiting Cyclooxygenase (COX) enzymes [3, 4]. The constitutive COX-1 performs numerous physiological activities as protecting gastric mucosa, vascular homeostasis and platelet aggregation, while the other isoform, the inducible COX-2 is concerned with prostaglandins that promote inflammation and modulate pain [5,6,7].
The use of traditional NSAIDs as aspirin, indomethacin and phenazone causes gastrointestinal side effects due to the inhibition of both COX isoforms [8,9,10]. Selective COX-2 inhibitor medications as celecoxib, valdecoxib, and rofecoxib have been prepared to avoid the side effects produced by traditional NSAIDs [11, 12]. Unfortunately, rofecoxib and valdecoxib were taken off the market due to their cardiovascular side effects including myocardial infarction and the occurrence of high blood pressure [13,14,15]. So, there is a great demand for selective COX-2 inhibitors with diminished side effects. Indole is one of the most widely used scaffolds in a broad range of anti-inflammatory agents [16,17,18]. Many research investigations have focused on indole-based NSAIDs such as indomethacin (I) to enhance their COX-2 selectivity and decrease the ulcerogenic adverse effects that linked to their strong COX-1 selectivity and drugs acidic properties [19,20,21]. Knaus and co-workers synthesized a new set of indole derivatives substituted at N-1 and C-3 [22]. From the prepared indole derivatives, compound II was the most selective (SI > 312) and potent (COX-2 IC50 = 0.32 µM) COX-2 inhibitor. In 2021, new indole derivatives having thiosemicarbazone moiety were prepared and screened for their anti-inflammatory effect using carrageenan-induced paw edema assay [23]. Compound III recorded superior COX-2 selectivity (SI = 23.06) than displayed by celecoxib (SI = 11.88).
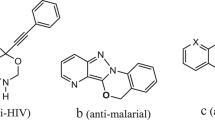
Thiazole is a five-membered heterocyclic ring [24,25,26,27,28] with many pharmacological utilities as anticancer [29, 30], antioxidant [31, 32], antimicrobial [33, 34], antidiabetic [35], anthelmintic [36] and anti-inflammatory [37, 38]. For example, the thiazole derivative IV significantly inhibited edema (60.82%) in carrageenan-induced edema compared with indomethacin (53.21%) [39]. Also, thiazole derivative V recorded comparable edema inhibition (EI = 87%) to that registered by indomethacin (EI = 91%) after 4 h [40].
Considering the aforesaid data and as an extension and development of our previous studies [41,42,43,44,45,46,47,48,49,50], we present the design and construction of novel indole-thiazole hybrids and biologically screened for their anti-inflammatory effect. This work aims to get new compounds with selective COX-2 inhibition, favorable anti-inflammatory potential and minimized gastric side effects. This aim has been achieved by hybridization of the privileged indole ring with the thiazole nucleus in one chemical entity (Fig. 1).
Result and discussion
Chemistry
In this work, treatment of thiosemicarbazide (1) with isatin derivatives 2a–f and 4-(bromoacetyl)-N-(4-methylphenyl)benzenesulfonamide (3) via three-component reaction under reflux in ethanol/tiethylamine (TEA). Firstly, compound 1 was allowed to react with some isatin derivatives 2a–f namely; isatin (2a), 5-chloro-isatin (2b), 5-nitro-isatin (2c), N-methyl-isatin (2d), 5-chloro-N-methyl-isatin (2e), 5-nitro-N-methyl-isatin (2f), then compound 3 was added until the reaction completed (TLC), to obtain thiazol-indolin-2-one derivatives 4a–f (Scheme 1).
The chemical structure of compounds 4a–f was determined using different elemental and spectroscopic analyses such as 1H-NMR, 13CNMR, as well as infrared spectroscopy.
Their infrared spectra revealed the existence of new bands in the range 3363–3124 cm−1 corresponding to NH. groups. 1H NMR spectra showed, as well as the aromatic signals, new singlet signals in the region δ 13.30–9.03 ppm for NH groups. The N-CH3 proton in compounds 4d–f appeared as a singlet signal in the range δ 3.73–3.84 ppm, respectively. Moreover, their 13C NMR spectra matched the accurate chemical structure which showed the carbonyl groups in the range 190.6–161.2 ppm and the N-CH3 groups in compounds 4d–f appeared in the region δ 34.5–30.6 ppm, and the CH3 groups at range δ 22.4–21.3 ppm, respectively. Furthermore, elemental analyses of thiazoles 4a–f provided the correct structure of the new products (cf. experimental).
Biological screening
Anti-inflammatory activity
The anti-inflammaory potential of indol-3-ylidenehydrazino-1,3-thiazole derivatives 4a–f was estimated applying the carrageenan-induced rat paw edema method using celecoxib as a standard. Each target compound was taken immediately before inflammation induction by carrageenan injection. The anti-inflammatory potential was recorded according to paw volume changes after 1, 3 and 5 h as displayed in Table 1. The obtained outcomes disclosed that 4-{2-[2-(5-chloro-2-oxo-1,2-dihydro-3H-indol-3-ylidene)hydrazino]-1,3-thiazol-4-yl}-N-phenyl-4-tolylsulfonamide (4b) was the most active candidate with edema inhibition percent equal to 12.72–45.63%. Furthermore, this compound 4b showed higher edema inhibition (EI = 38.50%) than that exhibited by celecoxib (EI = 34.58%) after 3 h. Moreover, compound 4f revealed comparable edema inhibition (3 h; EI = 31.94%, 5 h; EI = 41.84%) to that recorded by celecoxib (3 h; EI = 34.58%, 5 h; EI = 49.30%). In addition, within 1H-indole derivatives 4a–c, the 5-chloroindole derivative (4b) was the most active anti-inflammatory candidate (3 h; EI = 38.50%, 5 h; EI = 45.63%) followed by 5-nitro analogue (4c) (3 h; EI = 23.33%, 5 h; EI = 39.19%) while compound 4a with no substitution at positions 1 and 5 of indole moiety exhibited the least anti-inflammatory activity (3 h; EI = 18.05%, 5 h; EI = 12.76%). In case of N-methylindole derivatives (4d–f), the 5-nitroindole candidate (4f) showed the highest edema inhibition percent (3 h; EI = 31.94%, 5 h; EI = 41.84%) followed by compound 4d (3 h; EI = 15.41%, 5 h; EI = 23.76%) then the 5-chloro analogue (4e) (3 h; EI = 5.69%, 5 h; EI = 8.72%). From the recorded data in (Table 1 and Fig. 2), it is clear that compound 4b has the most promising anti-inflammatory potential in comparison with celecoxib.
Histological investigation
The impact of compound 4b on paw tissue after carrageenan injection, comparing the results to those observed with indomethacin. It has been found that compound 4b is the most effective of the tested products. As shown in Fig. 3, the paw tissues of control rats (2, A) are not inflamed. The carrageenan model demonstrated neutrophil migration in addition to acute inflammation (black arrow) and hemorrhagic edema (black star) (Fig. 2B). Nevertheless, the rats given Celecoxib showed a notable decrease in inflammation Fig. 2C. Figure 2D demonstrated the impact of test chemical 4b on paw tissue inflammation, demonstrating a notable reduction in inflammatory cells and edema.
Microscopic examination of the impact of 4b on paw tissues following carrageenan injection. A control group with normal paw tissue, B carrageenan group disclosed an acute inflammation (black arrow) with edema (black star), C Celecoxib group with remarkable attenuation of edema and neutrophils migration, D compound 4b treated group with significant attenuation of inflammation and edema. Sections stained with H&E, (× 200)
In vitro COX inhibition screening
Using a colorimetric enzyme immunoassay (EIA), the most active candidates 4b and 4f inhibitory efficacy against COX-1/COX-2 enzymes was ascertained. For each hybrid, the effectiveness was measured using serial dilutions to determine the concentration that inhibited 50% of the enzyme (IC50) (100, 10, 1, and 0.1 M). Additionally, for COX-1/COX-2, selectivity indexes (SI values) against COX-2 were computed and compared with reference drugs celecoxib and indomethacin.
The results obtained from the 4b and 4f hybrids are displayed in (Table 2), which indicates that both compounds 4b and 4f exhibited higher COX-2 inhibitory effect than COX-1 enzyme.
Compound 4b was the most potent COX-2 inhibitor (IC50 = 8.26 µM), while 4f was the most COX-2 selective (SI = 4.32) compared with indomethacin (COX-2 IC50 = 0.77 µM, SI = 0.67) and celecoxib (COX-2 IC50 = 1.60 µM, SI = 4.44). Furthermore, both 4b (SI = 2.65) and 4f (SI = 4.32) were more COX-2 selective than indomethacin (SI = 0.67). In addition, the 5-nitroindole candidate (4f) exhibited comparable selectivity index (SI = 4.32) to that recorded by celecoxib (SI = 4.44).
Histological evaluation of ulcers
Most NSAIDs have been found to induce stomach ulcers. Finding innovative anti-inflammatory medicines that helps to avoid this problem is crucial because the unfavorable gastrointestinal adverse reactions of current anti-inflammatory therapies is a major disadvantage Thus, to find any gastroprotective effects of the most potent anti-inflammatory compounds 4b and 4f, we investigated how hybrids affected rat stomach ulcers. Figure 4 clearly depicts the changes in the histology of the stomachs of rats. While the indomethacin-treated group (Fig. 4B) showed an interfered with glandular mucosal layer with numerous focal ulcerative zones, marked by the bringing of the epithelial lining and an accumulation of necrotic tissue, the control group (Fig. 4A) showed a normal gastric mucosa without any indication of erosion or inflammation. Furthermore, after administration of both compounds 4b and 4f (Fig. 4C, D) the glandular mucosa and submucosa in the several regions investigated in the stomach mucosa exhibited largely intact histological structure without any defects. More information from a new study with long term treatment is required to clarify the gastric effects of these compounds at long term of usage.
Inflammation induced by LPS in the RAW 264.7 cell line
The efficacy of synthesized compounds and their cytotoxicity on LPS-induced RAW 264.7 cells were evaluated at different concentrations by using the MTT assay. As seen in Fig. 5, as compared to LPS-induced macrophages, none of the two compounds were able to stop the growth of macrophages at 5 µM.
Structure–activity relationship
From the anti-inflammatory activity of the newly prepared compounds, some relations between their structure and activity could be concluded as outlined in Fig. 6.
In case of 1H-indole derivatives 4a-c, the presence of electron-withdrawing groups (Cl, NO2) at C-5 of indole moiety markedly improved the in vivo anti-inflammatory potential. This is obvious upon comparing the anti-inflammatory activity of compound 4b (3 h; EI = 38.50%, 5 h; EI = 45.63%) and 4c (3 h; EI = 23.33%, 5 h; EI = 39.19%) with unsubstituted analog 4a (3 h; EI = 18.05%, 5 h; EI = 12.76%). In addition, methylation of N-1 of indole derivatives attenuated the anti-inflammatory potential (except 4c) as observed in methylation of 4b (3 h; EI = 38.50%, 5 h; EI = 45.63%) to 4e (3 h; EI = 5.69%, 5 h; EI = 8.72%). While, methylation of 5-nitroindole derivative (4c) (3 h; EI = 23.33%, 5 h; EI = 39.19%) to 5-nitro-N-methylindole derivative 4f (3 h; EI = 31.94%, 5 h; EI = 41.84%) enhanced the anti-inflammatory potential.
Molecular docking study
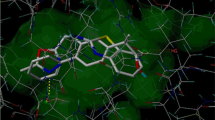
To gain insights into the fundamental mechanism of action of newly prepared indol-3-ylidenehydrazino-1,3-thiazole derivatives, molecular docking of the most active candidates (4b and 4f) was conducted inside COX-2 active region. The results of docking including docking score (Kcal/mol), types of interactions and the binded amino acids are listed in Table 3 and Figs. 7 and 8.
Compound 4b revealed good binding within COX-2 with binding energy score = -11.45 kcal/mol. Conventional hydrogen bonds with ARG376, TRP139, ASP229 and GLY235 amino acids were detected (Fig. 7). In addition, this compound 4b displayed other Pi-Cation interactions with LYS333, Pi-Alkyl binding with LEU145, PRO538; Amide-Pi Stacked with LEU224 and Van der Waals interactions with SER143 and ASN375 (Fig. 7).
Furthermore, compound 4f exhibited three hydrogen bonding interactions with ARG44, CYS41 and GLY135 amino acids with a binding energy score equal to − 10.48 kcal/mol. also, other binding interactions were registered as Pi-Alkyl binding with LYS468, PRO153 and ALA156; Amide-Pi binding with VAL155 and Van der Waals interaction with ASN34, ALA156 and ARG469 (Fig. 8).
Experimental
Chemistry
All melting points were recorded on Melt-Temp II melting point apparatus. IR spectra were measured as KBr pellets on a Shimadzu DR-8001 spectrometer. 1H NMR and 13C NMR spectra were recorded on a Bruker at 400 MHz and 100 MHz using TMS as an internal reference, DMSO-d6 as solvent. The elemental analyses were carried out on a Perkin-Elmer 240C Micro analyzer. All reactions were monitored by thin layer chromatography (TLC) using precoated plates of silica gel G/UV-254 of 0.25 mm thickness (Merck 60F254), with Rf value 0.58–64 (eluent solvent, Hexane/EtOH, 5:1).
General Procedure for the Synthesis of thiazole derivatives 4a–f
An equimolar mixture of thiosemicarbazide (1) (0.01 mol, 0.91 g) with the appropriate isatin derivative (2a–f) (0.01 mol) was allowed to reflux in ethanol (20 ml., 5 drops TEA). Then 4-(bromoacetyl)-N-(4-methylphenyl)benzenesulfonamide (3) (0.01 mol, 0.35 g) was added to the reaction mixture, and refluxing was continued for 20–30 min until the reaction was complete (TLC) to afford the corresponding thiazole derivatives (4a–f). The reaction mixture was allowed to cool to room temperature and the solid precipitate was filtrated, and recrystallized from ethanol.
4-{2-[2-(2-Oxo-1,2-dihydro-1H-indol-3-ylidene)hydrazino]-1,3-thiazol-4-yl}-N-phenyl-4-tolyl sulfonamide (4a)
Yield, 85%; Mp 335–337 °C; Rf value = 0.59; IR cm−1: 3363, 3178, 3120 (3NH), 3064 (C–Harom.), 1682 (C=O), 1H NMR δ 13.30 (br,1H, NH), 11.20 (s, 1H, NH), 10.29 (s, 1H, NH), 7.76–6.85 (m, 13H, CHarom.), 2.33 (s, 3H, -CH3); 13C NMR; 166.5 (C=O), 150.9, 143.8, 141.7, 137.9, 137.0, 132.5, 130.9, 130.3, 130.2, 130.1, 127.1, 125.0, 122.9, 120.4, 120.2, 120.1, 111.5, 106.4, 21.3; Anal. Calcd. For C24H19N5O3S2 (489.56) C (58.88%), H (3.91%), N (14.31%), S (13.10%); Found C (58.95%), H (3.98%), N (14.26%), S (13.16%).
4-{2-[2-(5-Chloro-2-oxo-1,2-dihydro-3H-indol-3-ylidene)hydrazino]-1,3-thiazol-4-yl}-N-phenyltolylsulfonamide (4b)
Yield, 88%; Mp 341–343 °C; Rf value = 0.58; IR cm−1: 3308, 3124 (3NH), 3061 (CH- arom.), 1671 (C=O), 1H NMR δ: 13.24 (s,1H, NH), 11.26 (s, 1H, NH), 10.29 (s, 1H, NH), 8.39–6.81 (m, 12H, CHarom.), 2.33 (s, 3H, -CH3); 13C NMR δ: 163.3 (C=O), 150.9, 143.9, 143.8, 141.0, 140.2, 138.7, 137.9, 137.0, 131.3, 130.2, 129.9, 127.1, 127.0, 127.0, 125.8, 121.8, 120.4, 120.1, 119.4, 21.3; Anal. Calcd. For C24H18ClN5O3S2 (524.01) C (55.01%), H (3.46%), N (13.36%), S (12.24%); Found; C (54.98%), H (3.39%), N (13.29%), S (12.18%); MS: m/z: 524 [M]+.
4-{2-[2-(5-Nitro-2-oxo-1,2-dihydro-3H-indol-3-ylidene)hydrazino]-1,3-thiazol-4-yl}-N-phenyl- tolysulfonamide (4c)
Yield, 78%; Mp 312–314 °C; Rf value = 0.60; IR cm−1: 3247- 3154 (3NH), 3085 (C–Harom.), 1654 (C=O), 1H NMR δ: 10.28 (s,1H, NH), 9.14 (s, 1H, NH), 8.64–7.11 (m, 13H, CHarom + NH.), 2.32 (s, 3H, CH3), 13C NMR δ: 163.5 (C=O), 146.6, 146.2, 144.9, 134.1, 133.5, 133.0, 131.5, 130.0, 130.7, 130.3, 128.9, 128.7, 128.6, 127.2, 123.8, 123.6, 123.4, 22.4; Anal. Calcd. For C24H18N6O5S2 (534.56); C (53.92%), H (3.39%), N (15.72%), S (12.00%) Found: C (53.86%), H (3.46%), N (15.65%), S (12.06%); MS: m/z: 534 [M]+.
(4-(2-(2-(1-methyl-2-oxoindolin-3-ylidene)hydrazinyl)thiazol-4-yl)-N-(p-tolyl) benzene sulfonamide (4d)
Yield, 82%; Mp 328–330 °C; Rf value = 0.64; IR cm−1: 3217, 3161 (2NH), 3078 (C–Harom.), 1658 (C=O), 1H NMR δ 13.16 (br,1H, NH), 10.45 (s, 1H, NH), 7.75–7.02 (m, 13H, CHarom.), 3.73 (s, 3H, N-CH3), 2.30 (s, 3H, CH3); 13C NMR δ: 161.2 (C=O), 152..4, 143.8, 142.1, 138.7, 137.1, 133.0, 131.2, 130.2, 129.8,128.9, 127.2, 123.3, 122.2, 120.5, 119.5, 119.3, 115.4, 34.5, 21.3; Anal. Calcd. For C25H21N5O3S2 (503.36); C (59.62%), H (4.20%), N (13.91%), S (12.73%) Found; C (59.69%), H (4.16%), N (13.84%), S (12.85%); MS: m/z: 503 [M]+.
4-{2-[2-(5-Chloro-2-oxo-1,2-dihydro-N-methyl-3H-indol-3-ylidene)hydrazino]-1,3-thiazol-4-yl}-N-phenyl-4 tolylsulfonamide (4e)
Yield, 92%; Mp 330–335 °C; Rf value = 0.62; IR cm−1: 3190, 3167 (2NH), 3047 (C–Harom.), 1661 (C=O), 1H NMR δ 12.27 (s,1H, NH), 10.33 (s, 1H, NH), 7.79–6.99 (m, 12H, CHarom.), 3.75 (s, 3H, N-CH3), 2.33 (s, 3H, CH3), 13C NMR δ (ppm): 190.6 (C=O), 146.6, 146.5, 140.5, 137.3, 134.2, 132.8, 131.8, 131.1, 130.8, 129.0, 128.6, 128.5, 127.5, 126.0, 123.3, 122.7, 122.3,121.8, 118.7, 31.6, 21.6; Anal. Calcd. For C25H20ClN5O3S2(538.04) C (55.81%), H (3.75%), N (13.02%), S (11.92%) Found C (55.86%), H (3.83%), N (12.97%), S (11.86%); MS: m/z: 538 [M]+.
4-{2-[2-(5-Nitro-2-oxo-N-methyl-3H-indol-3-ylidene)hydrazino]-1,3-thiazol-4-yl}-N-phenyl-4-tolylsulfonamide (4f)
Yield, 86%; Mp 305–307 °C; Rf value = 0.60; IR cm−1: 3251, 3126 (2NH), 3085 (C–Harom.), 1654 (C=O), 1H NMR δ 9.18 (s,1H, NH), 9.03 (s, 1H, NH), 8.64–7.11 (m, 12H, CHarom.), 3.84 (s, 3H, N-CH3), 2.34 (s, 3H, CH3), 13C NMR δ: 162.3 (C=O), 154.2, 153.0, 151.0, 150.3, 146.3, 133.2, 132.7, 132.6, 132.3, 131.7, 130.7, 129.8, 129.7, 129.3, 128.6, 124.4, 123.0, 30.6, 22.0; Anal. Calcd. For C25H20N6O5S2 (548.59); C (54.73%), H (3.67%), N (15.32%), S (11.69%) Found: C (54.69%), H (3.73%), N (15.26%), S (11.78%). MS: m/z: 548 [M]+.
Biological evaluation
In vivo anti-inflammatory activity
For the in vivo assessment of the test compounds' anti-inflammatory activity, male Wister rats weighing 180 ± 10 g each were employed, with celecoxib serving as the reference drug. All animals had to acclimate to the criteria set by the Institutional Animals Ethics Committee (IAEC) of the Faculty of Science at Sohag University for at least one week prior to the investigations (permit No;). For this in vivo evaluation, 40 adult male Westar rats (n = 4) were randomly assigned. The selected agents were suspended in 1% newly prepared carboxy methyl cellulose (CMC) prior to being administered orally by gavage. Following a sub plantar injection of 100 µL of freshly prepared carrageenan gel (1% distilled water) into each rat's left hind paw, changes in paw thickness were observed [46]. Rats were administered test compounds orally via gavage one hour before the injection of carrageenan. Paw thickness was measured one, three, and five hours after the development of inflammation. The tested compound's effects were quantified as a percentage of edema inhibition. The anti-inflammatory potential is expressed as a percentage suppression of paw edema and quantified [52].
Histopathological analysis of the tissues in the paws
Prior to being embedded in paraffin, the tissues from the paws were stored in a 10% formalin-neutral buffer. Hematoxylin and eosin (H&E) were used to stain the slides after thin sections of 5–6 µm were cut using a microtome. The slides that were made with a light microscope exhibit pathological changes in them.
In vitro COX inhibition Screening
By utilizing the appropriate Human enzyme immune assay (ELIA) kits (Cayman Chemical, USA) and adhering to the manufacturer's instructions, the inhibitory activities of the test hybrids 4b and 4f versus COX-1, and COX-2 enzymes were assessed. The results were expressed as an IC50 value (µM). The data for studies conducted in triplicate are shown as IC50 ± SD. As positive controls, we employed the well-known COX-1, and COX-2 inhibitors indomethacin and celecoxib [53].
Histological evaluation of ulcers
To assess the ulcerogenic potential of different hybrids, twenty-four adult male Albino Wistar rats weighing 180 ± 20 g were divided into four groups. Water was supplied to the animals as needed throughout their overnight fast before treatment. The chosen hybrids were given orally at a dose of 50 mg/kg, whereas the positive control was indomethacin (30 mg/kg suspension in 1% CMC orally). Four hours later, the rats were slaughtered, and to assess the extent of gastrointestinal injury, their stomachs were promptly removed, cleaned with ice-cold saline, and preserved in 10% formalin saline [54]. The stomach tissues from each group were thinly sliced and prepared into slides, which were then stained with hematoxylin and eosin (H&E) for microscopic examination [55].
Assessment of the cytotoxicity of selected hybrids on RAW cells
RAW 264.7 cells were seeded at 5000 cells per well in a 96-well plate and incubated for 24 h. Following this, the cells were exposed to the investigated hybrids (4b and 4f) at five concentrations (5, 10, 20, 40, and 80 µM) for two hours before being stimulated with 1 µg/mL lipopolysaccharide (LPS) for 48 h. The cytotoxic activity of the produced hybrids was determined using the MTT assay. The hybrids were used at subtoxic concentrations to the cells in all subsequent tests to prevent any cytotoxic influence [56,57].
Docking study
The crystal structure of COX-2 was downloaded from Protein Data Bank (PDB:1CX2) and the molecular docking was performed following our previously reported work [52].
Statistical analysis
The obtained data were statistically analyzed using GraphPad Prism version 9, and the mean values and standard deviations (mean ± SD) were presented as a result. The significance of mean differences was evaluated using the Tukey–Kramer test and one-way analysis of variance (ANOVA), with p-values of less than 0.05 being considered statistically significant.
Conclusion
New series of novel indole-thiazole hybrids derivatives 4a–f were synthesized via multi-components of thiosemicarbazide with some isatine derivatives a–f and N-(4-(2-bromoacetyl)phenyl)-4-methylbenzenesulfonamide (3) under reflux in ethanol. The chemical structures of novel compounds were elucidated by elemental and spectral analyses. All new compounds have been screened for their anti-inflammatory activity using celecoxib as a reference drug. It has been found that compound 4b (3 h; EI = 38.50%, 5 h; EI = 45.63%) has the most promising and effective anti-inflammatory potential. Furthermore, molecular docking study of compounds 4b and 4f displayed that these compounds fitted into the COX-2 binding site with good docking energy scores.
Data availability
No datasets were generated or analysed during the current study.
.References
Silva LA (2015) literature review of inflammation and its relationship with the oral cavity. Glob J Infect Dis Clin Res 1:21–27
Abdellatif KRA, Abdelall EKE, Bakr RB (2017) Nitric oxide-NASIDS donor prodrugs as hybrid safe anti-inflammatory agents. Curr Top Med Chem 17:941–955
Jahnavi K, Reddy PP, Vasudha B, Narender B (2019) Non-steroidal anti-inflammatory drugs: an overview. J Drug Deliv Ther 9:442–448
Hilário, MOE, Terreri, MT, and Len, CuA. (2006) Nonsteroidal anti-inflammatory drugs: cyclooxygenase 2 inhibitors. J Pediatr 82:S206–S212
Gudis K, Sakamoto C (2005) The role of cyclooxygenase in gastric mucosal protection. Dig Dis Sci 50:S16–S23
Martinez-Gonzalez J, Badimon L (2007) Mechanisms underlying the cardiovascular effects of COX-inhibition: benefits and risks. Curr Pharm Des 13:2215–2227
Perrone G, Scilimati M (2010) Selective COX-1 inhibition: a therapeutic target to be reconsidered. Curr Med Chem 17:3769–3805
Vitale P, Panella A, Scilimati A, and Perrone MG (2016) COX-1 Inhibitors: beyond structure toward therapy. Med Res Rev 36:641–671
Abdelgawad MA, Bakr RB, Azouz AA (2018) Novel pyrimidine-pyridine hybrids: synthesis, cyclooxygenase inhibition, anti-inflammatory activity and ulcerogenic liability. Bioorg Chem 77:339–348
Bakr RB, Azouz AA, Abdellatif KR (2016) Synthesis, cyclooxygenase inhibition, anti-inflammatory evaluation and ulcerogenic liability of new 1-phenylpyrazolo [3, 4-d] pyrimidine derivatives. J Enzyme Inhib Med Chem 31:6–12
McMurray RW, Hardy KJ (2002) Cox-2 inhibitors: today and tomorrow. Am J Med Sci 323:181–189
Bakr RB, Ghoneim AA, Azouz AA (2019) Selective cyclooxygenase inhibition and ulcerogenic liability of some newly prepared anti-inflammatory agents having thiazolo [4, 5-d] pyrimidine scaffold. Bioorg Chem 88:102964
Dogn J-M, Supuran CT, Pratico D (2005) Adverse cardiovascular effects of the coxibs. J Med Chem 48:2251–2257
Burnier M (2005) The safety of rofecoxib. Expert Opin Drug Saf 4:491–499
PraticoÌ D, DogneÌ J-M (2005) Selective cyclooxygenase-2 inhibitors development in cardiovascular medicine. Circulation 112:1073–1079
Hemalatha K, Madhumitha G, Roopan SM (2013) Indole as a core anti-inflammatory agent: a mini review. Chem Sci Rev Lett 2:287–292
Singh S, Sharma N, Chandra R (2022) The indole nucleus as a selective COX-2 inhibitor and anti-inflammatory agent (2011–2022). Org Chem Front 9:3624–3639
Kumar D, Kumar RR, Pathania S, Singh PK, Kalra S, Kumar B (2021) Investigation of indole functionalized pyrazoles and oxadiazoles as anti-inflammatory agents: synthesis, in-vivo, in-vitro and in-silico analysis. Bioorg Chem 114:105068
Amin NH, El-Saadi MT, Hefny AA, Abdelazeem AH, Elshemy HA, Abdellatif KR (2018) Anti-inflammatory indomethacin analogs endowed with preferential COX-2 inhibitory activity. Future Med Chem 10:2521–2535
Nagesh KM, Prashanth T, Khamees HA, Khanum SA (2022) Synthesis, analgesic, anti-inflammatory, COX/5-LOX inhibition, ulcerogenic evaluation, and docking study of benzimidazole bearing indole and benzophenone analogs. J Mol Struct 1259:132741
Sravanthi T, Manju S (2015) Indoles: a promising scaffold for drug development. Eur J Pharm Sci 91:1–10
Kaur J, Bhardwaj A, Huang Z, Knaus EE (2012) N-1 and C-3 substituted indole Schiff bases as selective COX-2 inhibitors: synthesis and biological evaluation. Bioorg Med Chem Lett 22:2154–2159
ÃrT J, Gomes FO, de Miranda MD, de Almeida SM, da Cruz-Filho IJ, Peixoto CA, da Silva TG, Moreira DR, de Melo CM, de Oliveira JF (2023) Anti-inflammatory activity of novel thiosemicarbazone compounds indole-based as COX inhibitors. Pharmacol Rep 73:907–925
Hassan M, Ghaffari R, Sardari S, Farahani YF, Mohebbi S (2020) Discovery of novel isatin-based thiosemicarbazones: synthesis, antibacterial, antifungal, and antimycobacterial screening. Res Pharm Sci 15(3):281–290
Rahim F, Taha M, Iqbal N, Hayat S, Qureshi F, Uddin I, Zaman K, Rab A, Wadood A, Uddin N, Nawaz M (2020) Isatin based thiosemicarbazide derivatives as potential inhibitor of α-glucosidase, synthesis and their molecular docking study. J Mol Struct 1222:128922
Cheng R, Shi W, Yuan Q, Tang R, Wang Y, Yang D, Xiao X, Zeng J, Chen J, Wang Y (2021) 5-Substituted isatin thiosemicarbazones as inhibitors of tyrosinase: Insights of substituent effects. Spectrochim Acta Part A 255:119669
Freitas LAB, Santos AC, Silva GC, Albuquerque FN, Silva ED, Simone CA, Pereira VR, Alves LC, Brayner FA, Leite AC, Gomes PA (2021) Structural improvement of new thiazolyl-isatin derivatives produces potent and selective trypanocidal and leishmanicidal compounds. Chem Biol Interact 345:109561
Hasan Y, Mohammed A, Sevgi K, Halit M, Mustafa E, Parham T, Ümit MK, Muhammet K, Saud A, Kim M (2023) Isatin/thiosemicarbazone hybrids: facile synthesis, and their evaluation as anti-proliferative agents and metabolic enzyme inhibitors. Bull Chem Soc Ethiop 37(5):1221–1236
Patel S, Patle R, Parameswaran P, Jain A, Shard A (2019) Design, computational studies, synthesis and biological evaluation of thiazole-based molecules as anticancer agents. Eur J Pharm Sci 134:20–30
Pawar S, Kumar K, Gupta MK, Rawal RK (2021) Synthetic and medicinal perspective of fused-thiazoles as anticancer agents. Anticancer Agents Med Chem 21:1379–1402
Djukic M, Fesatidou M, Xenikakis I, Geronikaki A, Angelova VT, Savic V, Pasic M, Krilovic B, Djukic D, Gobeljic B (2018) In vitro antioxidant activity of thiazolidinone derivatives of 1, 3-thiazole and 1, 3, 4-thiadiazole. Chem Biol Interact 286:119–131
Muluk M, Patil PS, Kasare SL, Kulkarni RS, Dixit PP, Choudhary P, Haval KP (2020) Synthesis and molecular docking studies of novel pyridine-thiazole-hydrazone conjugates as antimicrobial and antioxidant agents. Eur Chem Bull 9:184–192
Borcea A-M, IonuÈ I, CriÈan O, Oniga O (2021) An overview of the synthesis and antimicrobial, antiprotozoal, and antitumor activity of thiazole and bisthiazole derivatives. Molecules 26:624
Mishra I, Mishra R, Mujwar S, Chandra P, Sachan N (2020) A retrospect on antimicrobial potential of thiazole scaffold. J Heterocycl Chem 57:2304–2329
Khatik GL, Datusalia AK, Ahsan W, Kaur P, Vyas M, Mittal A, Nayak SK (2018) A retrospect study on thiazole derivatives as the potential antidiabetic agents in drug discovery and developments. Curr Drug Discov Technol 15:163–177
Amnerkar ND, Bhusari KP (2011) Synthesis of some thiazolyl aminobenzothiazole derivatives as potential antibacterial, antifungal and anthelmintic agents. J Enzyme Inhib Med Chem 26:22–28
Kamat V, Santosh R, Poojary B, Nayak SP, Kumar BK, Sankaranarayanan M, Faheem Khanapure S, Barretto DA, Vootla SK (2020) Pyridine-and thiazole-based hydrazides with promising anti-inflammatory and antimicrobial activities along with their in silico studies. ACS Omega 5:25228–25239
Pattan SR, Hullolikar R, Dighe NS, Ingalagi B, Hole M, Gaware V, Chavan P (2009) Synthesis and evaluation of some new phenyl thiazole derivatives for their anti-inflammatory activities. J Pharm Sci Res 1:96
Tratrat C, Haroun M, Tsolaki E, Petrou A, Gavalas A, Geronikaki A (2021) Thiazole-based chalcone derivatives as potential anti-inflammatory agents: Biological evaluation and molecular modeling. Curr Top Med Chem 21:257–268
Manju S (2020) Identification and development of thiazole leads as COX-2/5-LOX inhibitors through in-vitro and in-vivo biological evaluation for anti-inflammatory activity. Bioorg Chem 100:103882
Helal M, Salem M, El-Gaby M, Aljahdali M (2013) Synthesis and biological evaluation of some novel thiazole compounds as potential anti-inflammatory agents. Eur J Med Chem 65:517–526
Elkanzi NA, Abdelhamid AA, Ali AM (2022) Designing and anti-inflammatory effectiveness of novel phenytoin derivatives via one pot multicomponent reaction. Chem Select 7:e202201293
Abdelgawad MA, Bakr RB, El-Gendy AO, Kamel GM, Azouz AA, Bukhari SNA (2017) Discovery of a COX-2 selective inhibitor hit with anti-inflammatory activity and gastric ulcer protective effect. Future Med Chem 9:1899–1912
Abdelgawad MA, Elkanzi NA, Musa A, Ghoneim MM, Ahmad W, Elmowafy M, Ali AM, Abdelazeem AH, Bukhari SN, El-Sherbiny M (2022) Optimization of pyrazolo [1, 5-a] pyrimidine based compounds with pyridine scaffold: synthesis, biological evaluation and molecular modeling study. Arab J Chem 15:104015
Abdelgawad MA, Al-Sanea MM, Musa A, Elmowafy M, El-Damasy AK, Azouz AA, Ghoneim MM, Bakr RB (2022) Docking study, synthesis, and anti-inflammatory potential of some new pyridopyrimidine-derived compounds. J Inflammat Res 5:451–463
Elkanzi NA, AlHazmi AKG, Bakr RB, Gad MA, Abd ElLateef HM, Ali AM (2023) Design and synthesis of pyridine and thiazole derivatives as ecofriendly insecticidal to control olive pests. Chem Biodivers 20:e202300559
Shaker ME, Goma HA, Alsalahat I, Elkanzi NA, Azouz AA, Abdel-Bakky MS, Ghoneim MM, Hazem SH, El-Mesery ME, Farouk F (2023) Design and construction of novel pyridine-pyrimidine hybrids as selective COX-2 suppressors: anti-inflammatory potential, ulcerogenic profile, molecular modeling and ADME/Tox studies. J Biomol Struct Dyn 9:1–14. https://doi.org/10.1080/07391102.2023.2293257
Khodairy A, Ali AM, ElWassimy M (2018) Synthesis and reactions of new thiazoles and pyrimidines containing sulfonate moiety. J Heterocycl Chem 55:964–970
Elkanzi NA, Kadry AM, Ryad RM, Bakr RB, Ali El-Remaily MAEAA, Ali AM (2022) Efficient and recoverable bio-organic catalyst cysteine for synthesis, docking study, and antifungal activity of new bio-active 3, 4-dihydropyrimidin-2 (1 H)-ones/thiones under microwave irradiation. ACS Omega 7:22839–22849
Winter CA, Risley EA, Nuss GW (1962) Carrageenin-induced edema in hind paw of the rat as an assay for antiinflammatory drugs. Proc Soc Exp Biol Med 111(3):544–547
Arooj B (2023) Anti-inflammatory mechanisms of eucalyptol rich Eucalyptus globulus essential oil alone and in combination with flurbiprofen. Inflammopharmacology 31(4):1849–1862
Rudrapal M, Eltayeb WA, Rakshit G, El-Arabey AA, Khan J, Aldosari SM (2023) Dual synergistic inhibition of COX and LOX by potential chemicals from Indian daily spices investigated through detailed computational studies. Sci Rep 13:8656
Subhawa S, Arpornchayanon W, Jaijoy K, Chansakaow S, Soonthornchareonnon N, Sireeratawong S (2023) Anti-inflammatory, antinociceptive, antipyretic, and gastroprotective effects of Eurycoma longifolia Jack ethanolic extract. Life 13(7):1465
Shaik RA (2024) Parthenolide alleviates indomethacin-induced gastric ulcer in rats via antioxidant, anti-inflammatory, and antiapoptotic activities. Naunyn Schmiedebergs Arch Pharmacol 4:1–13. https://doi.org/10.1007/s00210-024-03110-x
Mohamed MFA, Marzouk AA, Nafady A, El-Gamal DA, Allam RM, Abuo-Rahma GE-DA, El Subbagh HI, Moustafa AH (2020) Design, synthesis and molecular modeling of novel aryl carboximidamides and 3-aryl-1,2,4-oxadiazoles derived from indomethacin as potent anti-inflammatory iNOS/PGE2 inhibitors. Bioorgan Chem 105:104439
Ghoneim MM, Abdelgawad MA, Elkanzi NA, Parambi DGT, Alsalahat I, Farouk A, Bakr RB (2024) A literature review on pharmacological aspects, docking studies, and synthetic approaches of quinazoline and quinazolinone derivatives. Arch Pharm 357(8):e2400057. https://doi.org/10.1002/ardp.202400057
Acknowledgements
The authors gratefully acknowledge to Najran University, Faculty of Science and Arts at Sharurah, 68342; Sohag University, Egypt; Minia University, Egypt and Tabuk University Faculty of Science, Tabuk 71491.
Author information
Authors and Affiliations
Contributions
All authors wrote the main manuscript text and reviewed the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study has been carried on rats and the authors take personal responsibility for knowingtheir statutory responsibility under the Animal (Scientific Procedures) Act 1986, under the acceptance of Committee for Scientific Research Ethics (CSRE), code no. (CSRE-23-24)-Sohag University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alkorbi, F., Alshareef, S.A., Abdelaziz, M.A. et al. Multicomponent reaction for synthesis, molecular docking, and anti-inflammatory evaluation of novel indole-thiazole hybrid derivatives. Mol Divers (2024). https://doi.org/10.1007/s11030-024-10969-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11030-024-10969-8