Abstract
Objectives The patient centered medical home is now widely supported as a strategy for delivering high quality primary care. The objective of this study was to examine whether children’s primary care experiences nationally have become more aligned with the medical home model over time, and how this may have varied for vulnerable children. Methods This study analyzed data on 289,672 children, aged 0–17 years, of families responding to one of three iterations of National Survey of Children’s Health from 2003, 2007 and 2011–2012. Each year, we assessed indicators of four medical home features (access, continuity, comprehensiveness, and family-centeredness) and a total medical home score for children nationally and for those with a set of social and demographic risk factors. Results Indicators of access and continuity, and total medical home scores fluctuated but improved overall from 2003 to 2012 (7.1, 6.7 and 1.4 % point increases, respectively), while indicators of comprehensiveness and family-centered care measures declined (2.4 and 1.8 % point decreases, respectively). Children with the highest levels of social and demographic risk experienced larger fluctuations in these measures over time. Conclusions for Practice There were improvements in the extent to which children’s primary care experiences aligned with a medical home model, though not linearly or for all component features. Children with more risk factors experienced more volatile changes, suggesting a particular need to attend to the primary care experiences of the most vulnerable children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
There has been growing recognition and investment in recent years into the implementation of the medical home as a model of delivering primary care. Mechanisms are needed to monitor changes in its practice over time. In this study, we examined national trends in indicators of medical home experiences of children from 2003 to 2012. We found that there were some improvements in indicators of access and continuity, but declines in comprehensiveness and family-centered care. Children considered the most vulnerable experienced particular volatility over time.
Introduction
The concept of a medical home is now firmly cemented in the national dialogue regarding health care quality improvement. This is perhaps made most clear by its inclusion in the Patient Protection and Affordable Care Act (ACA) of 2010, with the federal government now having invested over $35 million in promoting its practice [1, 2]. Major physician organizations, including the American Academy of Pediatrics (AAP), have been at the heart of the medical home movement and have issued key policy statements defining this model of primary care and supporting its advancement [1, 3].
There is widespread agreement that the medical home model is an approach to delivering primary care that facilitates partnerships between patients and their providers, with aims to improve efficiency and patient outcomes. In defining the medical home, the AAP emphasized seven features, specifying that care should be: accessible, continuous, comprehensive, coordinated, family-centered, compassionate, and culturally effective [4]. A medical home model is thought to benefit patients, in part, by encouraging an ongoing relationship between patients and providers, and creating an environment that facilitates communication by focusing on the patient and family.
With the widespread promotion of the medical home model comes a growing need to monitor the extent to which patient experiences are increasingly aligned with this model. Many organizations have embraced the approach by the National Committee on Quality Assurance, which mainly measures structural elements within the delivery of services, and providers who apply may achieve medical home “recognition”. Monitoring experiences this way, however, misses practices that have not sought such recognition but still likely deliver some or most features of the medical home. Needed are feasible, national mechanisms for monitoring changes in practice over time in both delivery and receipt of care aligned with a medical home. Such monitoring may help assess if the ACA and the initiatives it funds have had their intended impacts.
Opportunities exist to assess whether patient experiences in primary care are aligning with the medical home model, particularly for children, through nationally representative population surveys. The National Survey of Children’s Health (NSCH) is one of two major surveys (the other being the more narrowly targeted National Survey of Children with Special Health Care Needs) to attempt to more comprehensively measure a range of indicators that reflect features of the medical home model. The NSCH has been conducted three times, and while there have been slight changes in measurement and a substantial change in sampling strategy, a core set of indicators can be used to track patient experiences in primary care over all three iterations.
The purpose of this study is to measure how children’s experiences in health care are aligning with the medical home model and how this has changed over the past decade in the US. Using three cross-sectional iterations of the NSCH conducted over roughly a decade, we examined whether changes occurred in indicators of a child’s medical home experience in four areas: access, continuity, comprehensiveness and family-centered care. We then examined whether changes varied across common socio-demographic subgroups reflective of child vulnerability (based on income, education, race/ethnicity, health insurance status and language) and across combined profiles of these risk factors.
Given the growing number of initiatives and resources invested into expanding the use of the medical home model, it is important to assess the extent to which the model is reaching children and families. By examining nationally representative secular trends in a set of patient experiences that are aligned with this model, we shed some light on the reach of the medical home as it grows over time and, importantly, how it is experienced by important subsets of socio-demographically vulnerable patients.
Methods
Data Source and Sampling
The nationally representative data come from the 2003, 2007 and 2011–2012 (hereafter referred to as just 2012) NSCH surveys conducted by the National Center for Health Statistics and the Federal Maternal and Child Health Bureau as a module of the State and Local Area Integrated Telephone Survey [5–7]. The administration of the 2012 NSCH differs somewhat from the 2003 and 2007 surveys by including a new cell-phone sample, and precautions are noted throughout our paper. More information about the design of each NSCH is available in separate reports [8–10].
Households with at least one child 0–17 years of age were eligible for interview and one child was selected at random. The adult most knowledgeable of the child’s health responded to the interview (a parent in >90 % of cases in each survey). The three iterations contain responses for 289,672 children (n = 102,353 in 2003, n = 91,642 in 2007, and n = 95,677 in 2012) with response rates of 55.3, 46.7, and 23.0 % respectively. The response rate for 2012 was also reported separately for the landline (38.2 %) and cell-phone (15.5 %) samples. All survey data are weighted by the National Center for Health Statistics (NCHS) to account for the complex sample design and non-response. Overall, potential biases from non-response, and from separate cell phone and landline samples, are estimated by NCHS to be negligible [11].
Measures
Medical Home Features
Indicators for four of the seven key features of a primary care medical home as described by the AAP were available in all three iterations of the NSCH. Indicators of other medical home features were available in selected years, but we have focused only on those that were consistently measured across all 3 years. The measures selected were informed by the work of Bethell et al. [12], which provided the foundation for the medical home questions in the NSCH. Because the NSCH changed its measurement of the medical home across iterations of the survey, our measures necessarily differ from Bethell et al. original plan: we could use only one question for each medical home feature and we could not include measures of coordination of care or cultural competence.
The four indicators include: (1) whether the child had a personal doctor or nurse (reflecting the medical home feature of continuity), (2) whether the child had at least one preventive visit in the past year (access), (3) whether the child received all needed medical care in the past year (comprehensiveness), and (4) whether the doctor “always” spent enough time with the child (family-centered care). We created a total medical home score equal to the proportion of the four features that were experienced (i.e. one of four features yielded a score of 25 %, and four of four features, 100 %).
Vulnerability
Five common risk factors were studied as measures of social and demographic vulnerability in our analyses. Their selection was based on the access to care models developed by Anderson and Aday [13, 14], and previous work supports their inclusion as major risk factors for poor health care experiences [15–18]. They include: (1) poverty status (above vs. below 200 % of the federal poverty level), (2) parent education (high school graduate vs. less than high school), (3) race (white vs. non-white), (4) health insurance coverage (yes/no), and (5) household language (English vs. other).
To summarize the risk factors a child experiences and their collective association with experiencing the medical home indicators, the risk factors were combined into an index of vulnerability (or “risk profile”) that is a simple count of the co-occurring risk factors (ranging from zero to five). Similar risk profiles have been used in prior work to study and summarize disparities in child health and health care [19–23], and we have used the same set of risk factors in a risk profile in our previous research on primary care [24, 25].
Analysis
Analyses were computed using Stata13. Survey (“svy”) procedures were invoked for all analyses to account for the complex survey design using weights provided in each of the three iterations of the NSCH. Because of differences in sampling design between the 2012 and earlier versions of the NSCH, we could not test differences across years using regression because we could not account for design effect differences.
To compare all 3 years, we analyzed each survey year separately to correctly calculate the estimates and 95 % confidence intervals, accounting for the design effect in each year. Within a given survey year, we compared medical home indicators across sub-populations using Chi squared techniques. But to compare these estimates across years, we reported changes as statistically significant where confidence intervals did not overlap.
When confidence intervals do not overlap, the difference between groups will be statistically significant at p < 0.05. This approach is widely used and highly conservative [26, 27], meaning that non-overlapping confidence intervals are a very strict test of significance. Where results were significant, arrows indicate the direction of change.
We also examine whether changes in the indicators of medical home across years varied among children considered more or less vulnerable based on risk profile. To do this, we compared estimates for a given indicator at each year and for each level of the risk profile (0, 1, 2 and 3+ risk factors). We present a set of graphs in Figs. 1 and 2, and statistically significance is noted where confidence intervals do not overlap.
Results
Table 1 shows that from 2003 to 2012, more children were in families that were lower-income, less educated, non-white, and non-English speaking, suggesting a higher potential risk for poor health care experiences. On the other hand, there was a decrease in the proportion of children who were uninsured during the same period. Overall, children were slightly more likely to have higher risk profiles in 2012 (e.g., the proportion of children with at least three risk factors increased from 13.0 to 15.6 %).
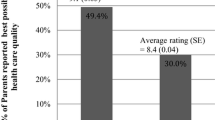
Table 2 shows that within each year of the survey, disparities existed for nearly every indicator and nearly every subgroup. The largest disparities in the indicators of a medical home were observed between the uninsured and insured. Table 2 further shows that two medical home indicators—having a personal doctor or nurse and a preventive visit—improved for children overall from 2003 to 2012. But the changes were not linear; the indicators increased from 2003 to 2007 and then declined slightly from 2007 to 2012.
Two other medical home indicators—getting all needed medical care and having a doctor who always spends enough time—declined for children overall from 2003 to 2012. The largest decrease in getting all needed care was among the uninsured. The uninsured were also the only subgroup to experience a statistically significant decline in the total medical home score from 2003 to 2012 (decreasing from 63.9 to 59.1 %).
Figures 1 and 2 show that changes over time in the medical home indicators tended to be larger among more vulnerable children. The increase from 2003 to 2012 in having a personal doctor or nurse, for example, was larger among children with a higher number of risk factors (i.e., 20.3 % points for those with 3+ risk factors vs. 4.2 for those with 0 risks). This pattern was less prominent for other indicators.
Changes in medical home features over time by the number of risk factors (risk profile). a Children with a personal doctor or nurse by risk profile. b Children with a preventive visit in the past year by risk profile. c Children that got all needed medical care by risk profile. d Children with a doctor that always spends enough time by risk profile
Discussion
Overall, our study finds that the degree to which the health care experiences of children are aligned with the medical home model has fluctuated over a decade, with some gains and some losses. Indicators of the medical home features of access and continuity improved while indicators of comprehensiveness and family-centered care declined. As a whole, the percentage of medical home features experienced by children improved slightly over time. This is notable considering an increase in the proportion of US children experiencing multiple socio-demographic risk factors for poor care.
We also found that more vulnerable children (i.e., those with more risk factors) saw greater changes over time in medical home indicators than less vulnerable children. This includes both larger increases from 2003 to 2007 and larger declines from 2007 to 2012. This is not surprising given that vulnerable populations are by definition more at-risk. It also suggests that trends in their health care experiences are more volatile (i.e., less stable) and perhaps more affected by external factors that can affect their care, both positively and negatively (including economy, health care workforce or policy).
Uninsured children experienced particular difficulties over the decade. They had an increase in continuity of care from 2003 to 2012, but other indicators either declined or were unchanged, leading to an overall decline in the total medical home score. Our findings confirmed previously reported declines in the proportion of uninsured children nationally [28, 29], but reaffirm that the challenges of being uninsured for obtaining quality health care remain profound. With millions of children expected to remain uninsured over the next decade, especially in states not expanding Medicaid [30], disparities in such medical home indicators will likely remain.
Also of concern is the decline in three of the five medical home measures from 2007 to 2012. While our study did not aim to examine reasons for such changes, it is worth considering that they occurred during the recent economic recession. Not only were many families impacted economically, but there are reports that the economy may have prompted providers to reduce staffing, which may reduce the capacity of providers to meet patient needs [31, 32]. On the other hand, the declines occurred during the first years of the ACA implementation, which we would have expected to have a positive impact. Understanding these external factors is an important next step.
Overall, a major contribution of this study is to assess the medical home for the population of US children using patient experience over time. While our study is different from other ways of assessing the medical home (e.g., counting NCQA medical home recognitions), the patient voice is an important component of assessing health care quality. This approach aligns with the renewed emphasis on patient-centered care and patient-reported outcomes [33–35], since care innovations must ultimately reach the patient.
But there are limitations to the NSCH and our study approach. First, our study documented trends nationally, but did not attempt to explain the observed fluctuations. This is an important next step, particularly as future iterations of the NSCH become available. Second, the use of cross-sectional datasets only allows us to assess association (not causality) and changes in the sample schemes across years did not allow us to use more robust regression analyses. Third, only four medical home indicators were consistent across the surveys, leaving out the coordination of care and cultural competence features of a medical home.
Fifth, there were very slight changes to the ordering and wording of questions, which do not allow us to completely rule out the role of instrumentation biases. None of the adjustments, however, suggests an obvious direction of affect, and the consistency of results across sub-groups suggests that any effects may be minor. Sixth, the use of risk profiles oversimplifies the complexity of associations with the medical home indicators. While the approach ignores important variation, it offers a generalizable assessment of vulnerability that can be used across outcomes.
Finally, a strength of the NSCH is that it offers an ongoing national assessment of medical home indicators for the general population of children. However, future versions of the NSCH should continue to aim for consistency in sampling and measurement, or at least interoperability weighting schemes, especially if considered valuable for monitoring the ACA. Surveys like the NSCH are instrumental for focusing measurements where the medical home is intended to impact: the patient.
Conclusion
Our study finds that children’s health care experiences have become more aligned with the medical home model over a decade, despite an increase in child vulnerability in the same period. And children with multiple sociodemographic risk factors appeared to experience larger changes (both positive and negative) in medical home indicators over time. Uninsured children were particularly at risk, and continued efforts to expand and connect children with insurance coverage may help reduce disparities and stabilize the medical home experiences of vulnerable children over time.
References
US Department of Health and Human Services. (2014). The Affordable Care Act Supports Patient-Centered Medical Homes in Health Centers. Accessed 15 Dec 2014.
Patient Protection and Affordable Care Act. (2010). 42 U.S.C. Public Law, §18001 et seq.
Kellerman, R., & Kirk, L. (2007). Principles of the patient-centered medical home. American Family Physician, 76(6), 774–775.
Medical Home Initiatives for Children with Special Health. (2002). Needs project advisory committee. The medical home. Pediatrics, 110(1), 184–186.
National Survey of Children’s Health. (2003). Maternal and child health bureau in collaboration with the national center for health statistics. 2003 NSCH Stata Indicator Set Prepared by the Data Resource Center for Child and Adolescent Health, Child and Adolescent Health Measurement Initiative. http://www.childhealthdata.org.
National Survey of Children’s Health. (2007). Maternal and child health bureau in collaboration with the national center for health statistics. 2007 NSCH Stata Indicator Set Prepared by the Data Resource Center for Child and Adolescent Health, Child and Adolescent Health Measurement Initiative. http://www.childhealthdata.org.
National Survey of Children’s Health. (2011/12). Maternal and child health bureau in collaboration with the national center for health statistics. 2011/12 NSCH Stata Indicator Set Prepared by the Data Resource Center for Child and Adolescent Health, Child and Adolescent Health Measurement Initiative. http://www.childhealthdata.org.
Blumberg, S., Olson, L., Frankel, M., Osborn, L., Srinath, K., & Giambo, P. (2005). Design and operation of the national survey of children’s health, 2003. Hyattsville, MD: National Center for Health Statistics 2005.
Blumberg, S., Foster, E. B., Frasier, A. M., et al. (2009). Design and operation of the national survey of children’s health, 2007. Hyattsville, MD: National Center for Health Statistics.
Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. (2013). National Survey of Children’s Health. http://www.cdc.gov/nchs/slaits/nsch.htm.
Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. (2013). 2011-2012 National Survey of Children’s Health Frequently Asked Questions. http://www.cdc.gov/nchs/slaits/nsch.htm.
Bethell, C. D., Read, D., & Brockwood, K. (2004). Using existing population-based data sets to measure the American Academy of Pediatrics definition of medical home for all children and children with special health care needs. Pediatrics, 113(5 Suppl), 1529–1537.
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior, 36(1), 1–10.
Aday, L., Fleming, G., & Andersen, R. (1984). Access to medical care in the US: Who has it, who doesn’t?. Chicago, IL: Pluribus Press.
Lay-Yee, R., Milne, B., Davis, P., Pearson, J., & McLay, J. (2015). Determinants and disparities: A simulation approach to the case of child health care. Social Science and Medicine, 128, 202–211.
Flores, G., & Tomany-Korman, S. C. (2008). Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics, 121(2), e286–e298.
Flores, G., Olson, L., & Tomany-Korman, S. C. (2005). Racial and ethnic disparities in early childhood health and health care. Pediatrics, 115(2), e183–e193.
Stevens, G., & Shi, L. (2003). Racial and ethnic disparities in the primary care experiences of children: A review of the literature. Medical Care Research and Review, 60(1), 3–30.
Björkenstam, E., Burström, B., Brännström, L., Vinnerljung, B., Björkenstam, C., & Pebley, A. R. (2015). Cumulative exposure to childhood stressors and subsequent psychological distress. An analysis of US panel data. Social Science and Medicine, 142, 109–117.
Baron-Lee, J., Bonner, B., Knapp, C., Bright, M., & Hinojosa, M. (2015). Factors associated with having a medical home for children at-risk of experiencing negative events: Results from a national study. Maternal and Child Health Journal, 19(10), 2233–2242.
Cheng, E. R., Poehlmann-Tynan, J., Mullahy, J., & Witt, W. P. (2014). Cumulative social risk exposure, infant birth weight, and cognitive delay in infancy. Academic Pediatric, 14(6), 581–588.
Larson, K., Russ, S. A., Crall, J. J., & Halfon, N. (2008). Influence of multiple social risks on children’s health. Pediatrics, 121(2), 337–344.
Stevens, G. (2006). Gradients in the health status and developmental risks of young children: The combined influences of multiple social risk factors. Maternal and Child Health Journal, 10(2), 187–199.
Stevens, G. D., Seid, M., Pickering, T. A., & Tsai, K. Y. (2010). National disparities in the quality of a medical home for children. Maternal and Child Health Journal, 14(4), 580–589.
Stevens, G. D., Seid, M., Mistry, R., & Halfon, N. (2006). Disparities in primary care for vulnerable children: The influence of multiple risk factors. Health Services Research, 41(2), 507–531.
Finch, S., & Cumming, G. (2009). Putting research in context: understanding confidence intervals from one or more studies. Journal of Pediatric Psychology, 34(9), 903–916.
Cumming, G., & Finch, S. (2005). Inference by eye: Confidence intervals and how to read pictures of data. American Psychologist, 60(2), 170–180.
Rudowitz, R., Artiga, S., Arguello, R. (2014). Children’s health coverage: Medicaid, CHIP and the ACA. The Henry J. Kaiser Family Foundation. http://kff.org/health-reform/issue-brief/childrens-health-coverage-medicaid-chip-and-the-aca/. Accessed 15 Dec 2014.
DeNavas-Walt, C., Proctor, B. D., Smith, J. C., & US Census Bureau. (2013). Current population reports, P60-245, income, poverty, and health insurance coverage in the United States: 2012. Washington, DC: U.S. Government Printing Office.
Kenney, G. M., Alker, J., Anderson, N., et al. (2014). A First Look at Children’s Health Insurance Coverage under the ACA in 2014. Health Reform Monitoring Survey. http://hrms.urban.org/briefs/childrens-health-insurance-coverage-under-the-aca-in-2014.html.
American Academy of Pediatrics Pediatric Practice Manager Association. Effect of Economic Recession on Pediatric Practices. (2009). http://www.aap.org/en-us/professional-resources/practice-support/practice-management/Pages/Effect-of-Economic-Recession-on-Pediatric-Practices.aspx.
Burgard, S. (2012). Health, mental health and the great recession. Stanford, CA: Stanford Center on Poverty and Inequality.
Wu, A. W., Snyder, C., Clancy, C. M., & Steinwachs, D. M. (2010). Adding the patient perspective to comparative effectiveness research. Health Affairs (Millwood), 29(10), 1863–1871.
Snyder, C. F., Jensen, R. E., Segal, J. B., & Wu, A. W. (2013). Patient-reported outcomes (PROs): Putting the patient perspective in patient-centered outcomes research. Medical Care, 51(8 Suppl 3), S73–S79.
Ahmed, S., Berzon, R. A., Revicki, D. A., et al. (2012). The use of patient-reported outcomes (PRO) within comparative effectiveness research: Implications for clinical practice and health care policy. Medical Care, 50(12), 1060–1070.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stevens, G.D., Kim, A.Y. National Trends in Indicators of a Medical Home for Children. Matern Child Health J 20, 730–739 (2016). https://doi.org/10.1007/s10995-015-1902-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1902-z